* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Transport in Humans
Survey
Document related concepts
Transcript
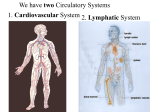
Transport in Humans Pure Biology Chapter 8 Coloured scanning electron micrograph (SEM) of a resin cast of blood vessels supplying the small intestine. Learning Objectives • State the functions of the following components of blood: plasma, red blood cells, white blood cells, platelets • List the different blood groups and all possible combinations for the donor and recipient in blood transfusions. • Relate the structure of arteries, veins and capillaries to their functions. • Identify the main blood vessels to and from the heart, lungs, liver and kidneys. • Describe the structure and function of the heart in terms of muscular contraction and the working of valves. • Outline the cardiac cycle in terms of what happens during systole and diastole. Learning Objectives • Describe the transfer of substances between capillaries and tissue fluid. • Describe coronary heart disease in terms of the occlusion of coronary arteries. • List the possible causes of coronary heart disease. • State the possible preventive measures for coronary heart disease. Why the need for a transport system?? • In simple unicellular organisms, oxygen and nutrients can diffuse through the cell surface membrane and reach all parts of the cell easily. Why the need for a transport system?? • In complex multicellular organisms, simple diffusion cannot bring enough oxygen and food materials to the cells situated deep in the body. Waste products cannot be easily removed as well. • A transport system helps to carry substances from one part of the body to another. Mammalian Transport System Lymphatic system Blood system blood fluid blood vessels heart Structure and Composition of Blood What are the components of blood? Investigation 8.1 • Examine a slide of blood smear using a light microscope. • Make drawings of the different cells observed. Composition of Blood platelet white blood cell (lymphocyte) red blood cells white blood cell (phagocyte) Blood Tissue fluid part 55% blood plasma red blood cells (erythrocytes) cell-like part 45% blood cells (corpuscles) platelets (thrombocytes) white blood cells (leucocytes) lymphocytes phagocytes Blood Plasma • A pale yellowish liquid • About 90% water and 10% mixture of dissolved substances. • The amounts of the various dissolved substances in the blood plasma are kept relatively constant. • Blood plasma transports the dissolved substances and blood cells around the body. Blood Plasma: Dissolved Substances • Soluble proteins: – Fibrinogen and prothrombin: for blood clotting – Antibodies: for fighting diseases • Dissolved minerals (occurring as ions): – Hydrogencarbonates, chlorides, sulfates – Phosphates of calcium, sodium and potassium • Food substances: glucose, amino acids, fats, vitamins • Excretory products: urea, uric acid, creatinine • Hormones (e.g. insulin) Blood Serum • When storing blood, blood-clotting factors (fibrinogen and prothrombin) are removed to prevent the blood from clotting during storage. • Blood plasma with its blood-clotting factors removed is known as blood serum. Blood Tissue fluid part 55% blood plasma red blood cells (erythrocytes) cell-like part 45% blood cells (corpuscles) platelets (thrombocytes) white blood cells (leucocytes) lymphocytes phagocytes Red Blood Cells (Erythrocytes) • Quantity: ≈5 million red blood cells per mm3 of blood. • Produced by the bone marrow. • Lifespan: 3-4 months • Worn-out cells are destroyed in the spleen. • Haemoglobin obtain from destroyed cells are brought to the liver and broken down to form: – bile pigments (excreted as bile) – Iron (stored in liver) Structure and Function of Red Blood Cells Structure Contains haemoglobin Function Haemoglobin combines reversibly with oxygen, enabling red blood cells to transport oxygen from lungs to all cells in the body. Circular, flattened Increases cell’s surface area to volume ratio biconcave disc for faster absorption and release of oxygen. Absence of nucleus Allows cell to contain more haemoglobin Elastic Can turn bell-shaped when squeezing through blood vessels smaller than its diameter. Role of the Bone Marrow • Location: spongy red tissue found in the centre of bones • The marrow of the vertebrae, ribs and pelvis contain stem cells: – Can divide many times to produce different cells • Many blood cells are produced throughout one’s life as the cells have a limited lifespan. – Red blood cells: 120 days – Platelets: 6 days – White blood cells: 1 day or less Blood Tissue fluid part 55% blood plasma red blood cells (erythrocytes) cell-like part 45% blood cells (corpuscles) platelets (thrombocytes) white blood cells (leucocytes) lymphocytes phagocytes White Blood Cells (Leucocytes) • • • • • Quantity: ≈5000-10000 per mm3 of blood Produced by the bone marrow. Lifespan: 1 day or less Size: larger than red blood cells Features: – Colourless: does not contain haemoglobin – Contains nucleus – Can move, change its shape and squeeze through walls of capillaries 2 Kinds of Leucocytes • Lymphocytes – Nucleus: large, round – Cytoplasm: non-granular, small amounts – Shape: round – Movement: limited – Function: produce antibodies to protect body from disease-causing microorganisms 2 Kinds of Leucocytes • Phagocytes – – – – – Nucleus: lobed Cytoplasm: granular Shape: irregular Movement: can be fast Function: ingests (take in and digest) foreign particles such as bacteria Blood Tissue fluid part 55% blood plasma red blood cells (erythrocytes) cell-like part 45% blood cells (corpuscles) platelets (thrombocytes) white blood cells (leucocytes) lymphocytes phagocytes Blood Platelets (Thrombocytes) • • • • Not true cells Membrane-bound fragments of cytoplasm From bone marrow cells Involved in blood clotting Blood Groups • The understanding of blood groups is important in blood transfusion. • If the wrong blood group is being put into a person, red blood cells from the donor will clump together. This is known as agglutination. • The clumps will block up small blood vessels and prevent the flow of blood, causing death. Agglutination of Red Blood Cells • Surface of all red blood cells contain antigens. These special proteins are the same on all cells. • Blood plasma contains natural antibodies which are always present in blood. • A person’s blood group is based on the types of antigens and antibodies present in the blood. • When both antigen and antibody of the same type are present, agglutination occurs. Blood Groups B B B Blood group A Blood group AB A B A A A A Blood group B B B Blood group O A Antigens and Antibodies in Blood Groups Mixing Blood Groups Functions of the Blood transport function protective function • food substances • blood clotting • excretory products • phagocytosis • hormones • antibody production • heat • oxygen Transport Function of the Blood The following are carried in solution in blood plasma: • Digested food: – Transported from blood capillaries in the small intestine to all parts of the body • Excretory products: – Nitrogenous waste – urea, uric acid, creatinine, removed from the body as blood flows through the kidneys – Carbon dioxide from cell respiration enters the blood as hydrogencarbonate ions, and converted to carbon dioxide in the lungs and expelled when we exhale Transport Function of the Blood The following are carried in solution in blood plasma: • Hormones – Transported from production glands to the parts of the body which require them • Heat – Produced in respiring body tissues – Main heat production is in the muscles and liver – Blood distributes the heat throughout the body, maintaining a uniform body temperature Gas Exchange in the Body O 2 CO2 alveolus (in lung) O2 CO2 HCO3- O2 (oxyhaemoglobin) veins arteries capillaries HCO3- O2 (oxyhaemoglobin) C6H12O6 + 6O2 6CO2 + 6H2O + energy Tissue cells Transport of Oxygen in the Blood • As blood passes through the lungs, oxygen diffuses from the alveoli into the blood. • Oxygen combines reversibly with haemoglobin to form an unstable compound, oxyhaemoglobin, which is bright red in colour. • Blood transports oxyhaemoglobin to all tissues of the body. • As blood passes through tissues with low oxygen concentration, the oxyhaemoglobin releases its oxygen, which diffuses into the cells. Transport of Oxygen in the Blood O2 haemoglobin (purplish-red) oxyhaemoglobin (bright red) O2 Carbon Monoxide Poisoning • If carbon monoxide enters the blood, it combines more readily with haemoglobin. • Carboxyhaemoglobin is formed, which is bright pink. • This compound does not readily give up its carbon monoxide. • Haemoglobin is unavailable to transport oxygen. • Blood cannot transport oxygen, leading to death. • Carbon monoxide is found in car exhaust fumes. Human Adaptation to High Altitudes • At high altitudes, oxygen concentration in the atmosphere is low. • Body produces more red blood cells, thus increasing the haemoglobin content per unit volume of blood. • More oxygen can be transported to tissue cells per unit time. • This is known as acclimatisation. Human Adaptation to High Altitudes • Long-distance runners often train at high altitudes for several months before a race. – Amount of haemoglobin in the blood increases – When running the race at lower altitudes, their bodies can carry oxygen more efficiently. – Runners can run for longer periods. Protective Function: Blood Clotting • Also known as blood coagulation. • Blood exposed to air will form a clot • Function of the clot: – Seal the wound and prevent excessive loss of blood – Prevent foreign particles from entering the blood • Some people suffer from haemophilia, a hereditary disease, where their blood-clotting mechanism is impaired. The person can bleed to death with slight injuries. The Blood Clotting Process damaged tissue and platelets produce thrombokinase (enzyme) prothrombin (inactive) thrombokinase thrombin (active) calcium ions thrombin fibrinogen insoluble fibrin threads, form mesh to trap blood cells The Blood Clotting Process • In undamaged blood vessels, the blood does not clot due to the presence of heparin. • Heparin is produced in the liver. • When thrombokinase is released, it neutralizes the action of heparin so that clotting can take place. Protective Function: Phagocytosis When bacteria enters the blood: • phagocyte will engulf the bacteria and enclose them • phagocyte ingests the bacteria • bacteria is digested in the phagocyte • Some phagocytes may get killed. These cells, together with dead bacteria, form pus. Protective Function: Phagocytosis bacteria bacteria ingested into cytoplasm phagocyte engulfing bacteria Protective Function: Antibody Production When disease-causing organisms (pathogens) enter the blood: • pathogens stimulate lymphocytes to produce antibodies which destroy bacteria by: – attaching to them and causing their surface membrane to rupture – causing bacteria to agglutinate so they can be easily ingested by phagocytes – neutralize harmful toxins produces by bacteria – attaching to viruses and making them unable to bind to a host cell. Protective Function: Antibody Production • Antibodies can stay in the blood for a long time after overcoming the disease. • The person then becomes immune or resistant to the infection. • In immunisation: – dead bacteria are injected into the blood – antibodies are formed – the person is temporarily immune from disease Organ Transplant and Tissue Rejection • In a tissue or organ transplant, the transplanted organ may be treated as a foreign body by the recipient’s immune system. • The recipient’s lymphocyte may produce antibodies to destroy the transplanted organ. • Doctors must be careful to obtain transplants from suitable donors to avoid rejection. • There will be no rejection if the transplanted tissue / organ came from the same person. Organ Transplant and Tissue Rejection To prevent tissue rejection: • a tissue match is necessary – tissues from both donor and recipient must be as genetically close as possible • take immunosuppressive drugs which inhibit the responses of the recipient’s immune system – recipient’s resistance to other infections is reduced – recipient must take drugs for the rest of his life Mammalian Transport System Lymphatic system Blood system blood (fluid) blood vessels heart circulatory system The Circulatory System • Function: to transport substances from one part of the body to another. • 2 types of systems: – open system: found in insects, where blood flows freely through tissues and bathes them – closed system: found in vertebrates, where blood is contained in blood vessels Components of the Human Circulatory heart System vein Components: • Heart • Blood vessels: artery blood flowing back to the heart veins a capillary network links arteries and veins capillaries venules arterioles arterioles blood flowing from the heart arteries – – – – – Arteries Arterioles Capillaries Venules Veins The Circulatory System – Heart • A muscular pump • Function: keep blood circulating throughout the body • When relaxed: it fills up with blood • When contracted: blood is squeezed out with a great force The Circulatory System – Blood Vessels Arteries • Blood vessels that carry blood away from the heart • Branches to form arterioles Arterioles • Arteries branch to form arterioles • Branches to form capillaries The Circulatory System – Blood Vessels Blood capillaries • Microscopic blood vessels found between tissue cells Venules • When leaving an organ / tissue, capillaries unite to form venules Veins • Venules join together to form veins • Carry blood back to the heart The Circulatory System – Blood Vessels arterioles venules vein artery capillaries Blood Vessels – Arteries • Function: Receives blood directly from the heart structure function Thick, elastic Withstand high blood pressure of the blood as it is walls forced out of the heart. The wall is much thicker in arteries nearest the heart. Elastic walls Constricts and dilates Enables artery wall to stretch and recoil, pushing the blood in spurts along the artery. This gives rise to the pulse. Achieved through contraction and relaxation of muscles in the arterial wall. When it constricts: lumen becomes narrower, less blood flows through per unit time. When it dilates: lumen becomes wider, more blood flows through per unit time. Blood Vessels - Arteries • Most arteries carry oxygenated blood from the heart to other parts of the body. – Exception: the pulmonary artery carries deoxygenated blood from the heart to the lungs. external layer (connective tissue) middle layer (smooth muscle and elastic fibres) endothelium lumen wavy elastic band Blood Vessels – Capillaries • Function: Food substances diffuse out, while waste materials diffuse into capillaries structure Walls made up of a single layer of flattened cells (endothelium) Endothelium is partially permeable Repeated branching function Microscopic capillaries can be found between the cells of almost all tissues. Quick diffusion of substances into and out of capillaries Provide large surface area for exchange of substances. Blood pressure lowers, slowing down the flow of blood and giving more time for the exchange of substances Blood Vessels - Capillaries single layer of endothelial cells Blood Vessels – Veins • Function: transports blood to the heart structure function thinner, less elastic walls Low blood pressure, where blood flows slowly and smoothly. presence of valves Internal valves prevent backflow of blood. Known as semi-lunar valves due to their half-moon shape. large lumen Lowers blood pressure to allow blood to flow slowly • Movement of blood is assisted by the action of skeletal muscles on the veins. – Exercising the muscles increases the pressure exerted on the veins Blood Vessels - Veins • Most veins carry deoxygenated blood from other parts of the body to the heart. – Exception: the pulmonary vein carries oxygenated blood from the lungs to the heart. external layer (connective tissue) middle layer (smooth muscle and elastic fibres) endothelium lumen Flow of Blood in Blood Vessels Blood Circulation in Vertebrates • In a double circulation, blood passes through the heart twice in one complete circuit. pulmonary circulation Double Circulation in Mammals systemic circulation – Pulmonary circulation – Systemic circulation systemic circulation • Blood flows from the heart to the lungs, and then back to the heart. • Blood goes from the heart to lungs via the pulmonary artery. • Blood returns to the heart from the lungs via the pulmonary vein. pulmonary circulation Double Circulation – Pulmonary Circulation systemic circulation • It is the circulation of blood around the body. • Oxygenated blood leaves the left side of the heart and is distributed by arteries to all parts of the body (except the lungs). • Veins carry deoxygenated blood from all parts of the body to the right side of the heart. pulmonary circulation Double Circulation – Systemic Circulation Double Circulation – Advantages • Blood entering the lungs is at a lower pressure compared to blood leaving the heart. – Blood can flow more slowly through the lungs – More time for blood to absorb oxygen before returning to the heart • Heart can pump the blood at high pressure to the rest of the body. – Distributes oxygenated blood to the body tissues more quickly – Maintain high metabolic rate in mammals The Heart – Structure External structure: • Surrounded by a pericardium, which is made up of two layers of membrane – Inner membrane: in contact with the heart – Between the two membranes: fluid to help reduce friction when the heart is beating The Heart – Structure Internal structure: • 4 chambers: – Upper chambers: atria (singular: atrium) – Lower chambers: ventricles • Divided down the middle into left and right halves by a muscular wall called the median septum – Prevents the mixing of deoxygenated blood and oxygenated blood superior vena cava aortic arch pulmonary arch pulmonary artery pulmonary vein right atrium left atrium semi-lunar valves inferior vena cava chordae tendineae right ventricle median septum bicuspid valve left ventricle Route of the Blood in the Heart 1. Return of deoxygenated blood from the rest of the body to the heart • • • Blood from the head, neck and arms enter via the superior vena cava Blood from the other parts of the body (except lungs) enter via the inferior vena cava Enters the right atrium Route of the Blood in the Heart 2. Right atrium contracts: blood goes into the right ventricle • • Tricuspid valve opens (consists of 3 flaps, attached to the walls by chordae tendinae) Pressure in the right atrium is higher than the pressure in the right ventricle. Route of the Blood in the Heart 3. Right ventricle contracts: • • • • • Blood pressure in right ventricle causes the tricuspid valve to close, preventing backflow of blood into the atrium. Chordae tendinae prevent valve flaps from reverting into the atrium. Blood leaves right ventricle via the pulmonary arch Pulmonary arch divides into two pulmonary arteries, one to each lung. Semi-lunar valves in pulmonary arch prevent backflow of blood into the right ventricle. Route of the Blood in the Heart 4. Blood enters the lungs: • • Blood is slowed down by the branching of the artery into a capillary network. Gaseous exchange occurs 5. Oxygenated blood from the lungs return to the heart: • • Blood enter via the pulmonary vein Blood enters the left atrium Route of the Blood in the Heart 6. Left atrium contracts, blood goes into the left ventricle: • • Bicuspid valve opens (consists of 2 flaps) Pressure in the left ventricle is lower than the pressure in the left atrium. Route of the Blood in the Heart 7. Left ventricle contracts: • • • Bicuspid valve closes Blood leaves left ventricle via the aortic arch Semi-lunar valves in aortic arch prevent backflow of blood into the left ventricle. Route of the Blood in the Heart 8. Blood in aorta is distributed to the rest of the body (except lungs): • • • Aortic arch have branches to direct the blood to specific areas of the body Blood entering the aorta is at a very high pressure Two small coronary arteries emerge from the aortic arch, to bring oxygen and nutrients to the heart muscles The Cardiac Cycle • Two keywords: – Systole: contraction – Diastole: relaxation • 3 stages: – – – – Complete diastole (whole heart) Atrial systole Ventricular systole / Atrial diastole Ventricular diastole (back to complete diastole) The Cardiac Cycle • Complete diastole – – – – Both atria and ventricles are relaxed Right atrium receives blood from vena cavae Left atrium receives blood from pulmonary veins Some blood flows directly into the ventricles pulmonary vein vena cava right atrium right ventricle left atrium left ventricle The Cardiac Cycle • Atrial systole – Atria contract – Blood is forced into the ventricles right ventricle left ventricle The Cardiac Cycle • Ventricular systole / Atrial diastole – Ventricles contract – high pressure in ventricles – Blood flows from left ventricle into the aortic arch, and from right ventricle into the pulmonary arch – Bicuspid and tricuspid valves close, producing a loud ‘LUB’ sound. aortic arch pulmonary arch tricuspid valve bicuspid valve The Cardiac Cycle • Ventricular diastole – Ventricles relax – Drop in blood pressure in ventricles causes semilunar valves in the arches to close – Produce a soft ‘DUB’ sound. – Whole heart is relaxed (complete diastole) right ventricle left ventricle The Heart and Blood Pressure • Definition of blood pressure: – the force that blood exerts on the walls of blood vessels • Measured using a sphygmomanometer • Unit of measurement: mm of mercury The Heart and Blood Pressure • High blood pressure in arteries: – Occurs during ventricular systole when blood is forced into arteries • Decrease in blood pressure: – Occurs during ventricular diastole • Blood pressure varies in different parts of the body. – Highest: near aortic arch – Lowest: vena cava (almost 0 mm mercury) Blood Pressure of a Person • Average blood pressure: 120 (systolic) 80 (diastolic) • High blood pressure: 140/90 or higher – Can occur temporarily after heavy exercise or when a person is angry – Can be persistent, which is unhealthy Pressure Changes in the Heart (Left) ventricular diastole Pressure / mm of mercury ventricular systole pressure in aorta pressure in ventricle atrial diastole Time/s atrial systole pressure in atrium Pressure Changes in the Heart (Right) ventricular diastole Pressure / mm of mercury ventricular systole pressure in ventricle pressure in aorta atrial diastole Time/s atrial systole pressure in atrium Main Arteries of the Body refer to LN Tissue Fluid • Description: colourless liquid • Location: between tissue cells • Function: carry substances in solution between tissue cells and blood capillaries • Formation: – Blood pressure at arterial end of capillaries is high – Blood plasma is forced through capillary walls as tissue fluid. • Other names: intercellular fluid, interstitial fluid Exchange of Substances between Blood and Tissue • Wanted substances: – food substances and oxygen – originate from the arterioles – diffuse from the blood into the tissue fluid • Unwanted waste products: – hydrogencarbonate ions, urea, creatinine – diffuse from cells into tissue fluid, and then through capillary walls into the blood plasma Red Blood Cells in Capillaries • Lumen of the capillary is very narrow, thus red blood cells have to move through the lumen in single file. • Red blood cells may become bell-shaped as they pass through narrow blood capillaries. • Advantages: – Reduce diameter of the cell so that it can pass through easily – Increase surface area to speed up transfer – Reduce rate of blood flow Coronary Heart Disease • Cause: blockage or narrowing of coronary arteries – Arteries lie on the outside of the heart – Carry blood to the muscles in the walls of the heart – Muscle cells are kept alive by the fresh supply of oxygen from the arteries, keeping the heart pumping Coronary Heart Disease • Result: heart attack – Blood flow to a particular part of the heart may be completely blocked – Heart does not receive sufficient oxygen and nutrients – Region of heart muscle dies – Blood is unable to pump blood to various parts of the body Causes of Coronary Heart Disease • Atherosclerosis – Fatty substances (e.g. cholesterol, polysaturated fats) deposited on the inner surface of the coronary arteries. – Lumen of the artery is narrowed – Blood pressure increases – Artery develops rough inner surfaces – Increases the risk of forming a blood clot Causes of Coronary Heart Disease • Coronary thrombosis – Thrombosis: blood clot – Cuts off blood and oxygen supply to the heart muscles – Heart attack occurs Reducing the Risk of Coronary Heart Disease • Proper diet – Replace animal saturated fats with polyunsaturated plant fats: may lower cholesterol – Rich in dietary fibres from green vegetables and fruits • Proper stress management • Avoid smoking – Nicotine increases blood pressure and the risk of coronary thrombosis – Carbon monoxide increases the risk of atherosclerosis • Regular physical exercise