* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Slajd 1 - Zakład Farmakologii Klinicznej w Poznaniu
Survey
Document related concepts
Saturated fat and cardiovascular disease wikipedia , lookup
Cardiovascular disease wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Remote ischemic conditioning wikipedia , lookup
Coronary artery disease wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Transcript
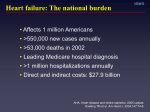
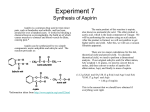
Recommendations for the pharmacological treatment of atherosclerotic cardiovascular disease based on clinical trials Zofia Oko-Sarnowska Department of Clinical Pharmacology Differences between chronic and acute atherosclerotic plaques Chronic(stable)plaque Acute(unstable)plaque Little lipide core Thick fibrous cap A low inflammatory cells migration A low MMP content Big lipide core Thin fibrous cap A high inflammatory cells migration A high MMP content Pharmacological methods of stabilization of atherosclerotic plaque APA VPI TNFαA ACE-I MMPI BB STATIN Proven effect Potencial effect ARBs AP Stabilisation of atherosclerotic plaque Influence on outside risk factor of transition from chronic to acute atherosclerosis -reduction of sudden change of blood pressure -reduction of vasospastic reaction -reduction of inflammatory process Direct influence on atherosclerotic plaque - decrease volume of lipid core - reduction of inflammatory process in situ - reduction of MMP concentration Classes of recommendations Class I Evidence and/or general agreement that a given diagnostic procedure/treatment is beneficial, useful, and effective Conflicting evidence and/or a divergence of opinion about the usefulness/efficacy of the treatment or procedure Class IIa Weight of evidence/opinion is in favour of usefullness/efficacy Class IIb Usefullness/efficacy is less well established by evidence/opinion Class II Class III Evidence or general agreement that the treatment or procedure is not useful/effective and in some cases may be harmful Levels of evidence Level of evidence A Data derived from multiple randomized clinical trials or metaanalyses Level of evidence B Data derived from a single randomized clinical trial or large non-randomized studies Level of evidence C Consensus of opinion of the experts and/or small studies, retrospective studies, registries Pharmacological methods of stabilization of atherosclerotic plaque APA VPI TNFαA ACE-I MMPI BB STATIN Proven effect ARBs AP Angiotensin converting enzyme inhibitors in cardiovacular disease Heart failure (HF) Asymptomatic left ventricular systolic dysfunction (LVSD) Diatolic failure Acute myocardial infarction (AMI) Hypertension (HT) Secondary prevention and high-risk of cardiovascular disease Indication for ACE-I Heart failure: CONSENSUS, SAVE, VheFT-II SOLVD Prevention, SOLVD Treatment LVSD after MI (EF<40%) Trial ACE-I n NNT Mortality reduction (RRR) SAVE kaptopril 2231 42 19% AIRE ramipril 2006 57 27% TRACE trandolapril 2606 76 22% AIREX ramipril 603 114 36% Use of ACE-I in heart failure Setting/indication Class Level All patients with symptomatic HF and reduced LVEF, NYHA II-IV I A LVSD with/without symptoms after MI I A LVSD (EF < 40-45%) without symptoms, no previous MI I A Diastolic HF IIa C Use of ACE-I in myocardial infarction Setting/indication Class AMI, first 24h risk (HF, LVD, no reperfusion, large MI Level ISIS 4, GISSI-3, CCS-1, CONSENSUS-2, SMILE High I A All IIa A patients Evolving AMI (>24h), Post MI Clinical HF, asymptomatic LVD (EF<45%) Diabetes patients or other high risk SAVE, AIRE, TRACE, I A I A Use of ACE-I in hypertension Setting/indication Class Level Trial STOP-2, UKPDS, PROGRESS To control blood pressure I A Patients with HF, LVSD, diabetics, previous MI or stroke, high coronary disease risk I A CAPPP, ABCD, PROGRESS Use of ACE-I in secondary prevention and high-risk of cardiovacular disease Setting/indication High-risk patients (evidence of cardiovascular disease or diabetes and one other risk factor Class I Level Trial A QUIET, PEACE, HOPE, EUROPA ONTAGET Hope study Enrolled 9297 men and women age > 55 years old Indications: 1. confirmed arterial disease (CHD, peripheral arterial disease, stroke 2. Diabetes and one other risk factor (hypertension, cigarette smoking, micoalbuminuria or dyslipidaemia) Randomisation to ACE-I (ramipril 2,5-10mg) or placebo Follow-up: 5 years Hope study Results: Primary end-point: death from cardiovascular causes, MI or stroke Ramipril Placebo 14% 17,8% NNT 26,3 RRR 22% Secondary end-points SCD 26% Stroke 32% Need for revascularisation 20% Dabetic complications 16% Onset of new diabetes 34% Trials in low risk patients n=13655 AP without HF Perindopril 8mg/d Reduction of: cardiovascular mortality, MI, SCD RRR= 20% NNT = 50/4,2years PEACE Trandolapril 2-4mg/d EUROPA n=8290 CAD + EF> 40% Reduction of cardiovascular mortality, non fatal MI, need for revascularisation (NS) Use of ACE-I to prevent sudden death In patients with asymptomatic LV dysfunction, moderate and advanced HF treatement with ACE-I resulted in a reduction in mortality from sudden cardiac death (SCD) This reduction varied from 20-54% and was statistically significant in some heart failure studies, although SCD was not the primary endpoint in this trials. Priori et al. For the Task Force on Sudden Cardiac Death of the ESC. Eur Heart J 2001; 22: 1374-450 Update on the guidelines for SCD of the ESC. .Eur Heart J 2003; 24: 13-15 Use of ACE-I to prevent sudden death Setting/indication Class Level Patients with HF I A Patients with previous MI I A Patients with dilated cardiomyopathy I B Pharmacological methods of stabilization of atherosclerotic plaque APA VPI TNFαA ACE-I MMPI BB STATIN Proven effect ARBs AP Usefulness of beta-adrenoceptor antagonists in cardiovascular disease CAD HF H DM A CAD – coranry artery disease, HF-heart failure, H - hypertension DM - diabetes, A - arrythmia Use of beta-adrenoceptor antagonists in coronary heart disease Acute myocardial infarction (AMI) Post MI – secondary prevention Acute coronary syndromes NSTEMI Chronic, stable ischaemic heart disease Heart failure (HF) Arrythmias Prevention of sudden cardiac death (SCD) Use of beta-blockers in AMI Setting/indication Class Level For relief of ischaemic pain I B To control hypertension, sinus tachycardia I B Primary prevention of SCD I B Sustained ventricular tachycardia I C Supraventricular tachyarrythmias I C To limit infarct size IIa A All patients without contraindications IIb A I A I.v.administration Oral administration All patients without contraindications Use of beta-blockers in secondary prevention after MI Setting/indication Class Level All patients without contraindication, indefinitely I A To improve survival I A To prevent reinfarction I A Primary prevention of SCD I A To prevent/treat late ventricular arrythmias IIa B Use of beta-blockers in non-STsegment elevation ACS (NSTEMI ACS) Setting/indication Class Level Early benefit, reduction of ischaemia I B Early benefit, prevention MI I B Long-term secondary prevention I B Use of beta-blockers in chronic, stable ischaemic heart disease Setting/indication Class Level To improve survival I A To reduce reinfarction I A To prevent/control ischaemia I A To improve survival I C To reduce reinfarction I B To prevent/control ischaemia I A Previous infarction No previous infarction Usefulness of beta-blockers in CAD based on clinical trials Olson’s meta-analysis 1992 (5 trials with metoprolol) Yusuf’s meta-analysis 1998 (25 randomized studies) Freemantle’s meta-analysis 1999 (82 trials post MI) 23% reduction of overall mortality despite ACE-I and ASA treatment Use of beta-blockers in chronic heart failure Setting/indication Class Level All stable patients, with symptomatic heart failure and reduced LVEF, functional class II-IV (to prolong survival) I A LVSD without symptoms after AMI I A LVSD without symptoms, no previous MI I B Chronic HF with preserved systolic function (to reduce heart rate) IIa C Acute, compensated heart failure after AMI IIa B Patient stable after acutely decompensated chronic heart failure I A Use of beta-adrenoceptor antagonists in heart failure Waagstein et al. – team from Gőteborg: the pioneers work on application of beta-blockers (metoprolol) in the treatment of HF (1970y) CIBIS I 1994 (bisoprolol). USCP (US Carvedilol Programme) 1996 (carvedilol) Australian/New Zealand Heart Failure Study 1997 (carvedilol) CIBIS II (Cardiac Insufficiency Bisoprolol Study II) 1999 MERIT-HF 1999 (metoprolol CR) COPERNICUS (Carvedilol Prospective Randomised Cumulative Survival Study) 2001 (carvedilol) CAPRICORN (Carvedilol Post-Infarct Survival Control in Left Ventricular Dysfunction) 2001 (carvedilol) Most importent trials in the treatment of HF with beta-blockers Trial Agent N All-cause mortality RRR (%) USCP Carvedilol 451 65 27 CIBIS II Bisoprolol 2647 35 15 MERIT-HF Metoprolol CR 3991 34 13 COPERNICUS Carvedilol 2289 35 27 CV morbidity RRR% Use of beta-adrenoceptor antagonists in heart failure Beta-blockers should be considered for the treatment of all patients (NYHA II-IV) with stable, mild, moderate, and severe heart failure from ischaemic or nonischaemic cardiomyopathies and reduced LVEF on standard treatment, including diuretics, and ACE-I, unless there is a contraindication (Class I, level A) Beta-blocking therapy reduces hospitalisations (all, cardiovascular, and HF), improves the functional class and leads to less worsening of HF. This beneficial effect has been consistently observed in subgroups of different age, gender, functional class, LVEF, and ischaemic or non-ischaemic aetiology (Class I, level A) Use of beta-adrenoceptor antagonists in heart failure In patients with LV systolic dysfunction, with or without symptomatic HF, following an AMI long-term beta-blockade is recommended in addition to ACE inhibition to reduce mortality (Class I, level B) Differences in clinical effects may be present between different beta-blockers in patients with HF. Accordingly, only bisoprolol, carvedilol, metoprolol succinate and nebivolol can be recommended (Class I, level A) Use of beta-adrenoceptor antagonists in diabetes Beta-blockers are particularly effective in decreasing post-infarction mortality and new infarcts in patients with a history of DM. Thus, oral BBs are, in the absence of contraindications, recommended for all diabetic patients with ACS (Class IIa, level B) Furthermore, such patients are more prone to develop heart failure and recent trials have documented the beneficial effects of betablockade in HF patients. Use of beta-blockers in diabetes Selective beta-1-antagonist may be preferred in case of insulin treatment Alpha-1-beta-adrenergic antagonists such as carvedilol may offer additional benefits for patients with peripheral artery disease or substantial insulin resistance. Pharmacological methods of stabilization of atherosclerotic plaque APA VPI TNFαA ACE-I MMPI BB STATIN Proven effect ARBs AP Angiotensin II receptor blockers (ARBs) – angioprotective action? LIFE (losartan vs atenolol): 2002 N=9100; age>55lat Hypertension with LVH Results: Risk reduction of CV death, MI and stroke Risk reduction of fatal nad non-fatal stroke Decrease onset of new diabetes SCOPE – beneficial effect of ARBs in primary prevention of stroke MOSES – beneficial effect of ARBs in secondary prevention of stroke DETAIL (telmisartan vs enalapryl): similar nephroprotecive effects in diabetes VALUE – decrease onset of new diabetes Use of angiotensin II receptor blockers (ARBs) in heart failure ARBs can be used as an alternative to ACE-I in symptomatic patients intolerant to ACE-I to improve morbidity and mortality (Class I, level B) (ELITE II, OPTIMAAL) ARBs and ACE-I seem to have similar efficiacy in CHF on mortality and morbidity (Class IIa, level B). In AMI with signs of HF or LVD ARBs and ACE-I have similar or equivalent effects on mortality (Class I, level B) (CHARM-Added) CHARM Programme 3 component trials comparing candesartan to placebo in patients with symptomatic heart failure CHARM Alternative CHARM Added CHARM Preserved n=2028 n=2548 n=3025 LVEF 40% ACE inhibitor intolerant LVEF 40% ACE inhibitor treated LVEF >40% ACE inhibitor treated/not treated Primary outcome for each trial: CV death or CHF hospitalisation Primary outcome for Overall Programme: All-cause death Pfeffer et al, Lancet 2003 CHARM-Alternative Primary outcome, CV death or CHF % hospitalisation 50 406 (40%) Placebo 40 334 (33%) 30 Candesartan 20 10 HR 0.77 (95% CI 0.67-0.89), p=0.0004 Adjusted HR 0.70, p<0.0001 0 Number at risk 0 Candesartan 1013 Placebo 1015 1 2 929 887 831 798 3 3.5 years 434 122 427 126 Granger et al, Lancet 2003 CHARM-Alternative Conclusions Despite prior intolerance to another inhibitor of the renin-angiotensinaldosterone system, candesartan was well tolerated In patients with symptomatic CHF and ACE inhibitor intolerance, candesartan reduces cardiovascular mortality and morbidity Granger et al, Lancet 2003 CHARM-Added Primary outcome, CV death or CHF % hospitalisation 50 538 (42.3%) 483 (37.9%) Placebo 40 30 Candesartan 20 10 HR 0.85 (95% CI 0.75-0.96), p=0.011 Adjusted HR 0.85, p=0.010 0 Number at risk 0 Candesartan 1276 Placebo 1272 1 2 1176 1136 1063 1013 3 3.5 years 948 457 906 422 McMurray et al, Lancet 2003 CHARM-Added Prespecified subgroups, CV death or CHF hospitalisation Candesartan event/n BetaYes blocker No Recom. Yes dose of No ACE inhib All patients Placebo event/n 223/702 260/574 232/643 251/633 274/711 264/561 275/648 263/624 483/1276 538/1272 p-value for treatment interaction 0.14 0.26 0.6 0.8 1.0 1.2 1.4 Candesartan Hazard Placebo better ratio better McMurray et al, Lancet 2003 CHARM-Added Conclusions Addition of candesartan to an ACE inhibitor (and beta-blocker) leads to a further and clinically important reduction in CV mortality and morbidity in patients with CHF The benefit of candesartan corresponds to a NNT of 23 (for a mean of 3.0 years) to prevent one CV death or a first CHF hospitalisation This benefit is obtained with relatively few adverse effects, although there is an increased risk of hypotension, hyperkalaemia and renal dysfunction McMurray et al, Lancet 2003 CHARM - Low EF trials: baseline characteristics Candesartan n=2289 Mean age (years) Women (%) NYHA class (%) II III IV Mean LVEF (%) Medical history (%) myocardial infarction diabetes hypertension atrial fibrillation Placebo n=2287 65 26 65 26 35 62 3 29 34 62 4 29 59 29 48 26 58 29 50 26 Young et al, Circulation 2004 CHARM - Low EF trials CV death or CHF hospitalisations CV death or CHF hosp (%) 50 Placebo 944 (41.3%) Two year HR 0.77 p<0.001 40 Candesartan 817 (35.7%) One year HR 0.70 p<0.001 30 20 10 Hazard ratio 0.82 (95% CI 0.74 – 0.90), p<0.001 0 Number at risk Candesartan Placebo 0 1 2289 2287 2105 2023 2 1894 1811 3 1382 1333 3.5 yrs 580 548 Young et al, Circulation 2004 CHARM-Low EF Implications Candesartan significantly reduces cardiovascular death, hospital admission for heart failure, and all-cause mortality in patients with CHF and LVEF 40% when added to standard therapies including ACE inhibitors, beta-blockers, and an aldosterone antagonist This approach offers the clinician an opportunity to make additional improvements in the poor prognosis of CHF patients when left ventricular systolic dysfunction is present Young et al, Circulation 2004 CHARM-Overall % 50 CV death or CHF hospitalisation 40 1310 (34.5%) 1150 (30.2%) Placebo 30 Candesartan 20 10 HR 0.84 (95% CI 0.77-0.91), p<0.0001 Adjusted HR 0.82, p<0.0001 0 0 Number at risk Candesartan 3803 Placebo 3796 1 2 3 3563 3464 3271 3170 2215 2157 3.5 years 761 743 Pfeffer et al, Lancet 2003 CHARM-Overall Conclusions Treatment of a broad spectrum of patients with symptomatic CHF with candesartan resulted in a: 9% reduction in all cause deaths (p=0.055, covariate adj. p=0.032) 12% reduction in CV mortality (p=0.012) 21% reduction in CHF hosp. (p<0.0001) 16% reduction in CV deaths or CHF hosp. (p<0.0001) Pfeffer et al, Lancet 2003 Use of angiotensin II receptor blockers (ARBs) in heart failure ARBs can be considered in combination with ACE-I in patients who remain symptomatic, to reduce mortality (Class IIa, level B) and hospital admissions for HF (Class I, level A) Concerns raised by initial studies about a potential negative interaction between ARBs and beta-blockers have not been confirmed by recent studies in post-MI or CHF (Class I, level A) Pharmacological methods of stabilization of atherosclerotic plaque APA VPI TNFαA ACE-I MMPI BB STATIN Proven effect ARBs AP Benefits of statin therapy Angioprotective effect Secondary prevention of CVE Dyslipidaemia therapy Significance of Scandinavian Simvastatin Survival Study (4S) 1993 Simvastatin (10-40mg/d) vs placebo Patients (n=4444) with CAD/post MI and total cholesterol concentrations 5,5-8mmol/L Prospective, randomized, double-blind, multicenter study Aim of study: to establish the benfit of simvastatin therapy on cardiovascular morbidity and overall mortality. Significance of Scandinavian Simvastatin Survival Study (4S) Results: significant reduction of relative risk Simvastatin vs placebo RRR Overall mortality 33% CV death 42% Serious cardiovascular events (AMI, SCD, cardiovascular death) 34% Need for revascularisation 37% Cost of hospitalisation 32% Beneficial effect was observed also in patients with diabetes and in elderly Pravastatin trials LIPID 1995y CARE 1996y. Patients with CAD/MI pravastatin 40mg/d vs placebo N=9014 Results: reduction of RR CV death ovarall mortality reinfarction CABG Stroke 25% 22% 29% 22% 19% Patients post MI pravastatin 40mg/d vs placebo N=4159 Results: reduction of RR CV death reinfarction CABG PTCA Stroke TIA 24% 25% 26% 23% 32% 27% Beneficial effects of statin despite normal lipidogram? HPS (Heart Protection Study) 2002 British multicenter study (55 hospitals) N=20536 patients (40-80 years old) with CAD or AO or after Stroke/TIA or Diabetes (type 2) Total cholesterol concentration > 135mg% Follow-up: 5 years Arms of study: simvastatin vs placebo simvastatin vs antioxidants antioxidants vs placebo placebo vs placebo HPS (Heart Protection Study) Results: No effects on CV events after antioxidants administration (Vit. C 250mg/d, vit. E 600mg/d, beta-caroten 20mg/d) Simvastatin therapy was associated with significant risk reduction of: CV death 18% all-cause death 13% overall death, MI, stroke, need for revascularisation 24% What LDL concentration is optimal? In the Pravastatin or Atorvastatin Evaluation and Infection Therapy (PROVE-IT) trial, standard statin therapy (pravastatin 40mg/d) was compared with intensive therapy (atorvastatin 80mg/d) Patients (n=4162) within 10 days of an ACS Mean follow-up 24 months Results: more intensive therapy (achived mean LDL 1,6mmol/L) was associated with a significant 16% risk reduction in CVE, compred with standard therapy (mean LDL 2,5mmol/l Intensive vs standard statin therapy Treat to New Targets Trial (TNT) Comparision of intensive statin therapy (atorvastain 80mg/d) and standard statin therapy (atorvastain 10mg/d) Patients (n=10001) with stable CAD Results: Mean LDL Ch SCE Atorvastatin 10mg/d Atorvastatin 80mg/d 101mg/dL 77mg/dL 10,9% 8,7% (RRR=22%) Pharmacological methods of stabilization of atherosclerotic plaque APA VPI TNFαA ACE-I MMPI BB STATIN Proven effect ARBs AP The use of aniplatelet agents in patients with atherosclerotic cardiovasular disease ESC Expert Consensus Document European Heart Journal 2004;25, 166-181 Sixth American College of Chest Physicians (ACCP) Consensus Conference on Antithrombotic Therapy Chest 2001; 119: 39S-63S Antithrombotic Trialists’ (ATT) Collaboration BMJ 2002; 324: 71-86 Antiplatelet drugs that may prevent atherothrombosis Approximately 20 different agents have been shown to inhibit platelet aggregation through different mechanisms of action However, inhibition of platelet aggreagation does not necessarily translate into prevention of atherothrombosis Antiplatelet drugs that have been successfully tested against placebo in adequately large randomized clinical trials include: * for chronic oral dosing: aspirin, ticlopidine and clopidogrel * for short-term intravenous administration: abciximab, tirofiban and eptifibatide Patients that may benefit from antiplatelet therapy Allocation of high-risk patients to a prolonged course of antiplatelet therapy reduced the combined outcome of nonfatal myocardial infarction, nonfatal stroke or vascular death (serious vascular events-SVA) by about 25% Absolute reductions in the risk of having a SVA: 36/1000 2 years Previous myocardial infarction (MI) 38/1000 1 month Acute myocardial infarction (AMI) 36/1000 2 years Previous stroke/TIA 9/1000 1 month Acute ischaemic stroke 22/1000 2 years Stabile angina (AP), peripheral arterial disease and atrial fibrillation (AF) In each of these high-risk categories, the absolute benefits substentially outweighed the absolute risk of major bleeding complications Clinical trial evidence in patients with ischaemic heart disease Ticlopidine and clopidogrel vs aspirin in patients with AMI non-significantly lower rates of SVA in the aspirinetreated arm In patients with chronic stable angina (AP), aspirin (75mg/d) significantly reduced the occurence of the primary end-point (MI, SCD) by 34% (median duration of follow-up of 50 months) In patients with unstable angina (API) aspirin (751300mg/d in 4 placebo-controlled trials) and ticlopidine have been shown to reduce by~50% the rate of MI and death Clinical trial evidence in patients with ischaemic heart disease Aspirin + Clopidigrel produced additive effects in patients with NSTEMI by reducing the rate of the first primary outcome (a composite of cardiovascular death (CVD), non fatal MI or stroke) by ~20% vs aspirin alone (12months of follow-up) The efficacy and safety of this combined antiplatelet strategy is currently being tested in patients with AMI, a clinical setting where aspirin alone (162,5mg started within 24h of the onset of symptoms) reduced the primary end-piont of CVD by ~23% and non-fatal SVA by ~50% Anitiplatelet therapy in diabetic patients with CAD Aspirin should be given for the same indications and in similar dosages to diabetic and nondiabetic patients (Class IIa, level B) ADP receptor-dependent platelet aggregation inhibitor (clopidogrel) may be considered in diabetic patients with ACS in addition to aspirin (Class IIa, level C) Guidelines on diabetes, pre-diabetes, and cardiovascular disease (ESC and EASD) Eur Heart J 2007: 28, 88-136 Balance of benefits and risks of antiplatelet therapy The absolute benefits of aspirin therapy substantially outweigh the absolute risks of major bleeding [particulary, gastrointestinal (GI)] complications in a variety of clinical settings characterized by moderate to high risk of occlusive vascular events. However, in lowrisk individuals the benfit/risk profile of such a preventive strategy is uncertain. A meta-anlysis of four primary prevention trials suggests that aspirin treatment is safe and worthwhile at coronary event risk ≥ 1,5% per year Recommendations concerning individual antiplatelet agents Aspirin Ticlopidine Clopidogrel Dipyridamol Abciximab, tirofiban, eptifibatide Other antiplatelet drugs ASPIRIN Aspirin once daily is recommended in all clinical conditions in wich antiplatelet prophylaxis has a favourable benefit/risk profile. Because of GI toxicity and its potential impact on compliance, physicians are encouraged to use the lowest dose of aspirin that was shown to be effective in each clinical setting. ASPIRIN The available evidence supports daily dose od aspirin in the range of 75-100 mg for the long term prevention of SVE in high-risk patients (i.e. ≥ 3% per year). In clinical situations where an immediate antithrombotic effect is required (such as in ACS or acute ischaemic stroke), a loading dose of 160 mg should be given at diagnosis (rapid and complete inhibition of TXA2dependent platelet aggregation)!!! ASPIRIN No test of platelet function is recommended to assess the antiplatelet effect of aspirin in the individual patient The routine use of proton pump inhibitors or cytoprtotecive agents is not recommended in patients taking daily dose of aspirin in the range of 75-100 mg, because of lack of randomized trials demonstrating the efficiacy of such protective strategies in this setting ASPIRIN Non-steroidal anti-inflammatory drugs (NSAIDs) have been investigated inadequately in terms of their potential cardiovacular effects. Thus, physicians prescibing these drugs to arthritic patients with prior vascular complications should not discontinue treatment with low-dose aspirin Because of potential pharmacodynamic interactions between traditional NSAIDs and aspirin, patients treated with low-dose aspirin requiring NSAID therapy may benfit from the use of selective COX-2 inhibitors. TICLOPIDINE The role of ticlopidine in the present therapeutic armamentarium is uncertain. Now that ticlopidine is available as a generic drug in many countries, its lower cost as compared to clopidogrel is being emphasized within a broad-cost containment strategy. Although there are no large head-to-head comparisions between the two thienopyridines, indirect comparisions are highly suggestive of a lower burden of serious bonemarrow toxicity with clopidogrel as compared to ticlopidine In contrast to clopidogrel, ticlopidine does not have an approved indication for patients with a AMI CLOPIDOGREL Although clopidogrel may be slightly more effecive than aspirin, the size of any additional benefit is statistically uncertain and the drug has not been granted a claim of superiority vs aspirin by regulatory authorities. Clopidogrel, 75mg daily, is an approppriate alternative for high-risk patients with coronary, cerebrovascular or peripheral arterial disease who have a contraindication to low-dose aspirin CLOPIDOGREL The results of the CURE trial have led to approval of a new indication for clopidogrel in patients with NSTEMI ACS A loading dose of 300 mg clopidogrel should be used in this setting followed by 75 mg daily. Revision of the existing guidelines will need a consensus agreement by the experts with respect to timing of percutaneous coronary intervention (PCI), length of clopidogrel treatment, and combination with GPIIb/IIIa anatagonists. DIPYRIDAMOL The combination of low-dose aspirin and extendedrelase dipyridamol (200mg bid) is considered an acceptable option for initial therapy of patients with noncardioembolic cerebral ischaemic events. (ESPS-2 trial) There is no basis to recommend this combination in patients with ischaemic heart disease. Abciximab, eptifibatide and tirofiban The benefit/risk profile of currently available GPIIb/IIIa antagonists is substentially uncertain for patients with ACS who are not routinely scheduled for early revascularisation (GUSTO IV, ACS, PARAGON-B) In contrast, for patients undergoing PCI, intensification of antiplatelet therapy by adding an intravenous GPIIb/IIIa blocker is an appropriate strategy to reduce the risk of procedure-related thrombotic complications. Other antiplatelet drugs Indobufen, triflusal and picotamide are commercially available in a few European countries, based on relatively limited evidence for efficacy and safety. Because of substantial statistical uncertainty surrounding the direct randomized comparisions of these agents vs aspirin and inadequate statistical power of the studies to assess reliably any difference in SVE, the use of indobufen, triflusal and picotamide instead of aspirin is not recommended ACS STEMI without PCI-secondary prevention STATIN ACE-I STEMI ACS ASA BB ACS STEMI post PCI (stent) STATIN clopidogrel BB STEMI ACS ACE-I ASA ACS NSTEMI with or without PCI –secondary prevention STATIN clopidogrel BB NSTEMI ACS ACE-I ASA Stroke/TIA –secondary prevention ACE-I STROKE APA STATIN Peripheral artery disease –secondary prevention ACE-I PAD APA STATIN