* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Document
Survey
Document related concepts
Transcript
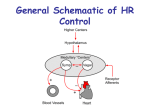
Control of blood pressure Outline • Short term control (baroreceptors) – Location – Types of baroreceptor – Baroreceptor reflex • Other stretch receptors • Long-term control – Renin/ angiotensin/ aldosterone system – Vasopressin – Atrial natiuretic peptide • Response to blood loss (shock) Control of blood pressure • Mean blood pressure is controlled by changing total peripheral resistance and or cardiac output. P = CO x TPR (compare Ohm’s law) – Cardiac output is controlled by sympathetic and para sympathetic nerves which effect: • heart rate • force of contraction – TPR controlled by nervous and chemical means to effect constriction/dilatation of • arterioles and venules Regulation of blood pressure How is pressure “measured”? • Short term – Baroreceptors • Long term – Kidney via renin angiotensin system Location of baroreceptors • Baroreceptors sense stretch and rate of stretch by generating action potentials (voltage spikes) • Located in highly distensible regions of the circulation to maximise sensitivity http://www.cvphysiology.com/Blood Pressure/bp012 baroreceptor anat.gif Baroreceptor output (from single fibres) Rapid increase in mean pressure Rapid decrease in mean pressure Response to pulse pressure From: Introduction to Cardiovascular physiology. J.R. Levick. Arnold 4th edition (2003) Two types of baroreceptor • Type A – High sensitivity – High firing rate • Type C – Lower sensitivity – Lower firing rate – Higher threshold (before firing starts) • Therefore can deal with higher pressures than type A which become “saturated” From “An Introduction to Cardiovascular Physiology” J.R. Levick Response of single baroreceptor fibre to change in pressure From “An Introduction to Cardiovascular Physiology” J.R. Levick Baroreceptor reflex Blood pressure falls Sensors Aortic arch Neural integration Nucleus tractus solitarius Vasoconstriction Effectors Carotid sinus Cardiac inhibition Cardiac stimulation Constriction of veins & arterioles Increased stroke volume Increased peripheral resistance Increased heart rate Increased cardiac output Increased blood pressure Baroreceptor reflex is a feedback loop Example: central heating system Set temperature Read temperature Yes Is temperature too high? No Boiler on Negative feedback Baroreceptor reflex is a feedback loop “Read” pressure Is pressure too high? No Yes Reduce CO Increase CO Reduce TPR Increase TPR Two way negative feedback Positive feedback loop Unstable Set temperature Read temperature No Is temperature too high? Ye Yes s Boiler on Positive feedback Other stretch receptors • Coronary artery baroreceptors – Respond to arterial pressure but more sensitive than carotid and aortic ones • Veno-atrial mechanoreceptors – Respond to changes in central blood volume • Lie down, lift your legs and cause peripheral vasodilatation • Unmyelinated mechanoreceptors – Respond to distension of heart • Ventricular ones during systole; atrial ones during inspiration Location of receptors in and near the heart Nucleus tractus solitarius Cardiac vagal afferents myelinated Cardiac pain unmyelinated Spinal cord Baroreceptors in coronary arteries and aortic arch Sympathetic afferents & unmyelinated nociceptors From “An Introduction to Cardiovascular Physiology” J.R. Levick Other receptors • Heart chemosensors – Cause pain in response to ischaemia • K+, lactic acid, bradykinin, prostaglandins • Arterial chemosensors – Stimulated in response to • Hypoxaemia, hypercapnia*, acidosis, hyperkalaemia** • Regulate breathing • Lung stretch receptors – Cause tachycardia during inspiration *too much CO2 **too much K+ Overview of short-term control mechanisms From: Introduction to Cardiovascular physiology. J.R. Levick. Arnold 4th edition (2003) Long term control of blood pressure • Involves control of blood volume/sodium balance by the kidneys – Hormonal control • Renin-angiotensin-aldosterone system • Antidiuretic hormone (vasopressin) • Atrial natiuretic peptide – Pressure natriuresis Reduced renal blood flow Juxtaglomerular apparatus Renin Angiotensinogen Renin/angiotensin/ aldosterone system Increased blood volume LV filling pressure) Increased pre-load Fluid re-absorption (LV pressure beginning of systole) Sodium retention Increased after-load Angiotensin I Angiotensin II Increased aldosterone secretion Veins vasoconstriction Arteries Vasopressin • Enhances water retention • Causes vasoconstriction • Secretion increased by unloading of aortic Baroreceptors and atrial sensors http://www.cvphysiology.com/Blood%20Pressure/BP016.htm Atrial natiuretic peptide • Increases salt excretion via kidneys – By reducing water reabsorption in the collecting ducts – relaxes renal arterioles – inhibits sodium reabsorption in the distal tubule • Released in response to stimulation of atrial receptors Summary of long term BP control • Cardiac output and BP depend on renal control of extra-cellular fluid volume via: – Pressure natriuresis, (increased renal filtration) – Changes in: • Vasopressin • Aldosterone • Atrial natiuretic peptide All under the control of altered cardiovascular receptor signaling Shock Definition: A pathophysiological disorder characterised by acute failure of the cardiovascular system to perfuse the tissues of the body adequately. Levick J.R. “An Introduction to Cardiovascular Physiology” Symptoms – – – – – – – Cold, clammy skin Muscular weakness Rapid and shallow breathing Rapid and weak pulse Low pulse pressure (and sometimes mean pressure) Reduced urine output Confusion Types of shock – Hypovolaemia • Caused by drop in blood (plasma) volume – e.g. haemorrhage, diarrhoea, vomiting, injury – Septic • Caused by bacterial endotoxins – e.g. salmonella – Cardiogenic • An acute interruption of of cardiac function – e.g. myocarditis (inflammation of the heart muscle) or myocardial infarction – Anaphylactic • Caused by allergic reaction Effect of blood loss • less than 10%, no serious symptoms – e.g. blood transfusion • 20 - 30% blood loss not usually life threatening • greater than 30%, severe drop in BP and, often, death due to impaired cerebral and coronary perfusion Response to moderate blood loss (compensated haemorrhage) • Blood volume falls therefore pulse pressure and stroke volume fall. (Frank-Starling mechanism: reduced LV contractile force) • Cardiopulmonary stretch receptor and baroreceptor activity falls • Arterial chemoreceptor activity increases, due to hypoxia and acidosis rapid breathing release of vasoconstrictors Vasopressin, angiotensin etc. Response to moderate blood loss More serious blood loss can be treated by transfusion to lessen the effects shown here Uncompensated shock If compensation is not sufficient, organ failure occurs due to inadequate perfusion • Heart • Kidney • Brain