* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Hemodynamic_Monitoring
Remote ischemic conditioning wikipedia , lookup
Coronary artery disease wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Electrocardiography wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Jatene procedure wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
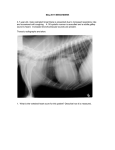
Dextro-Transposition of the great arteries wikipedia , lookup
Hemodynamic Monitoring D. Matamis M.D Papageorgiou Hospital Thessaloniki Greece. Shock or Hypotension may be due to: Decrease in cardiac output • Decrease in preload (hypovolemia - Hemorrhage) • Decrease in contractility (myocardial ischemia) Decrease of the inflow and outflow of blood into the cardiac chambers (obstructive shock) • Pulmonary embolism • HOCM • Valvular stenosis Decrease in peripheral resistances • Distributive shock (sepsis, allergic reactions) Hemodynamic Evaluation Non invasive methods (50%) Κλινικη εμπειρια, Φυσικη εξεταση, ECG, Rx Θωρακος Invasive methods (50%) Προφορτιο, Μεταφορτιο, Συσταλτικοτητα του μυοκαρδιου, Διαστολικη Λειτουργια, Καρδιακη Παροχη Invasive methods PAC Preload Y Cardiac Output Y Afterload Y Systolic Function ? Diastolic Function No Oxygen Delivery Y Oxygen Consumption Y Heart-Lung Interactions Y Intrapulmonary Shunt Y ECHO Y Νo Νo Y Y No No Y No The PAC controversy “The effectiveness of right heart catheterisation in the initial care of critically ill patients.” Connors AF, Speroff T, Dawson NV, et al. JAMA 1996. 276:889-897. 5735 critically ill patients (2184 with PAC) in 15 ICU’s 1008 pairs of patients matched for disease category No benefit Increased mortality (37.5% vs 33.8% without PAC) Greater hospital costs (49,300$ vs 35,700$ without PAC) Longer ICU and hospital stay Therapy related mortality - more aggressive level of care. The PAC controversy A randomized controlled trial of the use of pulmonary-artery catheters in high-risk surgical patients. Sandhham JD et al. N.Engl J Med.2003;348:5-14 From 1990-1999, surgical patients > 60 years old, ASA class risk III-IV. 997 patients in each group. No benefit No difference in mortality or hospital stay. Higher rate of pulmonary embolism in the catheter group(8 vs 0) The PAC controversy “A multicenter study of physicians’ knowledge of the Pulmonary Artery Catheter” Iberti TJ, Fischer EP, Leibowitz AB, et al. JAMA 1990: 264, 2928-32. 31 Q.M.C to 496 I.C.U Physicians practicing in the US and Canada. To quantify the knowledge and ability to interpret derived PAC data. Results. Mean score 20.7(67%), range 6-31(19-100%) Independent of training Frequency of use Frequency of insertion Restrict the use of PAC to individuals with documented competency. The PAC controversy Intensive care physicians’ insufficient knowledge of right heart catheterization at the bedside: Time to act? Gnaegi A, Feihl F, Perret C. Crit. Care Med. 1997:25,213-220. 31 Q.M.C to 535 I.C.U physicians practicing in 86 European I.C.Us. To quantify the knowledge and ability to interpret derived PAC data. Results. Mean score 72.2±14.4% 67.3±14.7% in training, 76.1%±13% postgraduate 50% of the responders did not identify PAOP from a clear chart recording Positive(loose correlation) with frequency of insertion and use. Accreditation policies and teaching practicies concerning this technique need urgent revision. PAC Pulmonary Artery Catheter. Does the problem lie in the users? Squara P, Bennett D, Perret C. Chest 2002: 121.2009-2015. “More than 25 years after the introduction of PAC and despite thousands of scientific publications, our data showed unacceptable variability in treatments and an alarmingly high rate of potentially harmful treatment decisions in participants to three international meetings in Intensive Care Medicine” Comparative studies PAC-ECHO ECHO vs PAC “Evaluation of TEE as diagnostic and therapeutic aid in a critical care setting.” Poelaert JI. Trouerbach J, et al. CHEST 1995.107: 774-779. TEE in 103 patients (66 with PAC, 37 without) offered useful information in 74% of the patients. altered the initial therapy in 44% with PAC. altered the initial therapy in 54% with PAC + Sepsis altered the initial therapy in 41% without PAC. Comparative studies PAC-ECHO “ Value of 2-D ECHO for Determining the Basis of Hemodynamic Compromise in Critically Ill Patients. A Prospective Study.” Sanjiv K, Alexander et al. J. AM. SOC. ECHOCARDIOGR. 1994,7: 598-606 TEE in 49 patients with PAC Agreement between the two methods in 86% of cases. “TEE in the ICU Setting: Luxury or Necessity?” D. Lagonidis, D. Matamis et al. B.J.A 1997. suppl. A46. 64 patients. Change in therapy in 23 / 60 patients (38%) What can be assessed with ECHO Preload Systolic function Diastolic function Heart Valves function Pericardial structure-Great vessels Preload Evaluation PAC - PCWP (Pressure) PCWP = LVED Pressure = LVED Volume Tachycardia, MV disease, LV Compliance Lung Hyperinflation(High PEEP,auto PEEP) ECHO - LA, LV Hypovolemia Hypervolemia ECHO > Volume OK (End systolic collapse) ? PAC Preload Evaluation 64 year old woman with History of CAD, Diabetes mellitus, Resp. Pb for 10 yrs Hypercapnic ARF, CXRay bilateral infiltrates, HR=135, MAP=65mmHg, Temperature 39.5. Treatment 40 mg Furosemide, Dobutamine 5mcg/kg/min I.C.U Shock, Intubation, MV, auto PEEP 12 cm H2O. PAC Findings HR= 130, MAP= 60 mmHg, PAP =55/25, PAOP =20mmHg , 16mmHg end expiration, C.O = 6.5lit/min, (a-v)DO2 = 5.8 1. You are happy with the hemodynamic status of the patient 2. You will increase the dose of Dobutamine to increase C.O. 3. You will add Nitroglycerine to decrease PAOP 4. You will ask for an ECHO study Preload Evaluation Preload Evaluation In the post operative period a 42 year old woman with Pulmonary Oedema (clinically, XRay) Heart Rate 140 beats/min, MAP = 85mmHg, ECG=ST depres. Intubation, M.V, PEEP 8cmH2O, FiO2=60% PAC findings Heart rate=140beats/min, SAP=85mmHg, PAOP = 34mmHg C.O = 3.5 lit/min Treatment Dobutamine 8mcg/kg/min, Nitroglycerine 1mcg/kg/min After treatment HR =145 b/min, PAOP = 30mmHg, C.O = 2.5 l/min ECHO to assess LV function and Preload. Preload Evaluation Preload evaluation with ECHO “Non invasive evaluation of pulmonary capillary wedge pressure in patients with acute myocardial infarction by deceleration time of pulmnary venous flow velocity in diastole” Yamamuro A,Yosida K, Hozumi T. JACC 1999:34.90-94 A DTd of <160 ms had 97% sensitivity and 96% specificity for a PCWP of >18 mmHg «The deceleration time of pulmonary venous diastolic flow is more accurate than the pulmonary artery occlusion pressure in predicting left atrial pressure» Kinnaid TD, Thomson CR, Munt BI. JACC 2001:37. 2025-2030 A DTd of <175 ms had 100% sensitivity and 94% specificity for a PLA of >17 mmH Preload evaluation with PVF (DTd) Cardiac Output monitoring “Ideal” CO continuous Monitoring: Minimally invasive, easy to apply: Widely applicable Accurate Real time: beat - to - beat CO Nurse driven Easy data interpretation Bedside management Neonates to adults Early warning of deterioration Evidence of improved outcome Optimum fluid management/drug administration Reduced workload of health care staff Decreased procedural complications (e.g. bolus injections) CO Techniques (non or less invasive) Based on: Echocardiography (TT &TEE) Esophageal Doppler Fick principle & CO2 rebreathing Pulse contour analysis Doppler Echocardiography(1): Principles for CO assessment Assumptions for accurate measurement No rhythm disturbances Accurate cross-sectional area measurement!!! Laminar flow “Flat” velocity profile Parallel angle beam/flow (≤20o) Velocity – diameter at the same site LVOT or AVA (IF No Aortic valvulopathy or HOCM) Esophageal Doppler (EDM): Principles & assumptions for CO monitoring Blood flow velocity of the descending aorta (PW or CW Doppler) Sedated, mech. ventilated pts Flexible probe: Insertion & rotation → Characteristic, clear signal, highest possible peak velocity “Flat” velocity profile (same speed of RBC) Cross – sectional area: Constant during systole (nomogram or direct measurement**) Fixed distribution of blood flow: Aortic arch→ 30%, Descending Aorta → 70% Esophageal Doppler (EDM): Final notes & critical appraisal Safe, easy to learn & set – up & apply (even nurse driven), reproducible results. Real beat to beat CO monitoring in sedated & mech. ventilated pts Monitoring but not diagnostic tool Excellent validity concerning the changes of CO (vs. PAC) Probe displacement: usual source of errors “EDM guided” fluid titration in high risk surgical pts: Evidence for improved outcome (LOS, complications post- op) Pulse contour Cardiac Output (PCCO): Principles, equipment, advantages Arterial waveform: interaction SV/mechanics of arterial tree PCCO methods: estimation of SV by pressure waveform PiCCO®, PulseCO®: Waveform analysis (various arterial models) & indicator dilution technique for calibration FloTrac, Vigileo™: Waveform analysis, no need for calibration Minimally invasive, continuous, real time CO Pulse contour Cardiac Output (PCCO): Flaws & Limitations Aortic Valve disease Arrhythmias Quality of the arterial waveform Frequent & rapid changes in arterial compliance Need for frequent calibrations - every 4h or before important acquisitions Minimally invasive??? Cardiac Output Evaluation The absolute value of C.O. is meaningless.(Hypo, Hyperthermia, Drugs) ICU patients Frequent modifications of Mechanical Ventilation and PEEP, TR, Sedation, General Anesthesia, Surgery, Variations of body temperature in the O.R., Substantial blood losses. SvO2, ScvO2, (a-v)DO2, DO2, VO2. Adequacy of C.O and oxygen transport, quality of tissue oxygenation. Contractility Evaluation Regional (Myocardial ischemia) Correlative study (100 patients) comparing PAC, ECG (12 lead), TEE M. van Daele et al. Circulation.1990. TEE = gold standard in detecting RWMA ECG = Sensitivity = 69% Specificity = 99% PAC = Sensitivity = 25% Specificity = 96% Global PAC Ventricular Work – PCWP (Ventricular Compliance) TEE By Eye, Ejection Fraction, Fract. Shortening. Contractility Evaluation (global systolic function) with PAC 17 y/o male admitted to the ICU with the diagnosis of ARDS due to bilateral pneumonia, fever 39 °C for a week. Upon admission, Bilateral Infiltrates in the CXRay, Temp= 39.4 WBC= 12000, 85%Neutrophils, HR=120 b/min, ECG=NL, MAP=110/55 under 1.2 mcg/kg/min of Noradrenaline. Acute Renal Failure due to Rabdomyolysis(CPK=35000). PAC findings C.O. =10 lit/min, PAOP =18mmHg, (a-v)DO2 = 4.8ml% 1. Do you consider the systolic function normal? 2. Do you consider the systolic function abnormal? 3. You will ask for an ECHO study to assess LV systolic function Contractility Evaluation (global systolic function) with PAC Contractility Evaluation (global systolic function) with PAC -Sepsis -Myocarditis -Dialated Cardiomyopathy Contractility Evaluation (regional systolic function) with PAC Regional systolic function M. Van Daele et al. Circulation 1990 ECHO, ECG 12 leads, PAC ECHO ECG PAC Gold standard Sensitivity. Specificity. 69% 99% 25% 96% TEE transversal axis (T) Diastolic dysfunction Diastolic dysfunction Decrease of the inflow and outflow of blood into the cardiac chambers Pulmonary Embolism Tamponade Valvular stenosis Tumors HOCM Πλεονεκτήματα της Υπερηχοκαρδιογραφίας στήν Οξεία Πνευμονική Εμβολή Ευαισθησια 80% Εξειδικευση 92-100% Οξεια-υποξεια Π.E Μαζικη-υπομαζικη Π.E Καθοδηγηση της Θεραπειας Ανταποκριση στη Θεραπεια Βαθμονομηση του κινδυνου Wood K. CHEST 2002;121:877 Αμεσα ευρήματα Εμμεσα Ευρήματα Διαταση RV/RA Σχεση RV/LV Μετατοπιση του ΜΚΔ Ανεπαρκεια Τριγλωχινος Ταχυτητα ροης του ανεπαρκουντος jet της τριγλωχινας < 3m/sec Case history A 73 –year-old lady admitted to the hospital for surgical repair of hip fracture. Preoperative assessment revealed exertional dyspnea attributed to moderate obesity and reduced physical activity Chest X-Ray: moderate cardiomegaly ECG showed atypical ST segment and T wave abnormalities. In the immediate post- operative period while recovering from regional anaesthesia she developed pulmonary oedema and acute respiratory failure. She was intubated and mechanically ventilated and a PAC was inserted for hemodynamic management. PAC data C.I = 1,9 lit/min/m2, PAP=55/30-42 mmHg, PAOP=28 mmHg. HR =125 b/min, ABP=120/90 mmHg Initial treatment consisted of diuretics (intra-operative fluid balance was 1.5 lit positive), dobutamine, and nitroglycerine, considering that this lady was suffering from congestive heart failure Despite the above treatment, leading to a negative fluid balance of 2,5 lit, the patient did not improve I.C.U ICU PAC data under: sedation (Remifentanyl –Propofol) Dobutamine=8 mcg/kg/min, Nitroglycerine = 1 mcg/kg/min Furosemide 20 mg/hr ABP= 110/85 mmHg, HR = 135 beats /min C.I =1.8 lit/min/m2, PAP = 60/35-45 mmHg, PAOP = 30 Suggestions for therapy changes? mmHg Hypertrophic Cardiomyopathies (HCM) Prevalence 0,2%, 1/500 Inherited autosomal dominant trait Primary sarcomere disorder LVH and Clinical symptoms during any phase of life Elderly patients > 75 years compose as much as 25%. Clinical course – Sudden death – Congestive heart failure Hypertrophic Cardiomyopathies (HCM) Non Obstructive (75%) Hypertrophic Cardiomyopathies (HCM) Obstructive (25%) Ejection Eject Venturi effect - SAM Obstruct Abnormal MV closure Leak MR+++ Tumors Tamponade ECHO unique tool to Diagnose Guide the therapy Quantity (loculated) Quality clear fluid, Thrombi. P.A.C Little diagnostic specificity Equalization of pressures CVP = PCWP Tamponade Conclusion PAC invasive technique but necessary for selected patients (need for SvO2) Echocardiography (TT &TEE) non invasive non expensive in every day practice but special training is necessary Esophageal Doppler non invasive , training is necessary, in the OR Pulse contour analysis: non invasive no special training in every day