* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Chapter 15 - Farmasi Unand
Survey
Document related concepts
Transcript
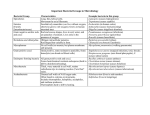
Microbial Mechanisms of Pathogenicity Chapter 15 Pathogenicity - ability to cause disease Virulence - degree of pathogenicity Many properties that determine a microbe’s pathogenicity or virulence are unclear or unknown But, when a microbe overpowers the hosts defenses, disease results! Portals of Entry 1. Mucus Membranes 2. Skin 3. Parentarel 1. Mucus Membranes A. Respiratory Tract • microbes inhaled into mouth or nose in droplets of moisture or dust particles • Easiest and most frequently traveled portal of entry Common Diseases contracted via the Respiratory Tract Common cold Flu Tuberculosis Whooping cough Pneumonia Measles Strep Throat Diphtheria Mucus Membranes B. Gastrointestinal Tract • microbes gain entrance thru contaminated food & water or fingers & hands • most microbes that enter the G.I. Tract are destroyed by HCL & enzymes of stomach or bile & enzymes of small intestine Common diseases contracted via the G.I. Tract Salmonellosis • Salmonella sp. Shigellosis • Shigella sp. Cholera • Vibrio cholorea Ulcers • Helicobacter pylori Botulism • Clostridium botulinum Fecal - Oral Diseases These pathogens enter the G.I. Tract at one end and exit at the other end. Spread by contaminated hands & fingers or contaminated food & water Poor personal hygiene. Mucus Membranes of the Genitourinary System - STD’s Gonorrhea Neisseria gonorrhoeae Syphilis Treponema pallidum Chlamydia Chlamydia trachomatis HIV Herpes Simplex II Mucus Membranes D. Conjunctiva – • mucus membranes that cover the eyeball and lines the eyelid Trachoma • Chlamydia trachomatis 2nd Portal of Entry: Skin Skin - the largest organ of the body. When unbroken is an effective barrier for most microorganisms. Some microbes can gain entrance thru openings in the skin: hair follicles and sweat glands 3rd Portal of Entry: Parentarel Microorganisms are deposited into the tissues below the skin or mucus membranes Punctures injections bites scratches surgery splitting of skin due to swelling or dryness Preferred Portal of Entry Just because a pathogen enters your body it does not mean it’s going to cause disease. pathogens - preferred portal of entry Preferred Portal of Entry Streptococcus pneumoniae • if inhaled can cause pneumonia • if enters the G.I. Tract, no disease Salmonella typhi • if enters the G.I. Tract can cause Typhoid Fever • if on skin, no disease Number of Invading Microbes LD50 - Lethal Dose of a microbes toxin that will kill 50% of experimentally inoculated test animal ID50 - infectious dose required to cause disease in 50% of inoculated test animals • Example: ID50 for Vibrio cholerea 108 cells (100,000,000 cells) • ID50 for Inhalation Anthrax - 5,000 to 10,000 spores ???? How do Bacterial Pathogens penetrate Host Defenses? 1. Adherence - almost all pathogens have a means to attach to host tissue Binding Sites adhesins ligands Adhesins and ligands are usually on Fimbriae Neisseria gonorrhoeae ETEC (Entertoxigenic E. coli) Bordetello pertussis 2. Capsules K. pneumoniae Prevent phagocytosis attachment Streptococcus pneumoniae Klebsiella pneumoniae Haemophilus influenzae Bacillus anthracis Streptococcus mutans Yersinia pestis 3. Enzymes Many pathogens secrete enzymes that contribute to their pathogenicity A. Leukocidins Attack certain types of WBC’s 1. Kills WBC’s which prevents phagocytosis 2. Releases & ruptures lysosomes • lysosomes - contain powerful hydrolytic enzymes which then cause more tissue damage B. Hemolysins - cause the lysis of RBC’s Streptococci 1. Alpha Hemolytic Streptococci - secrete hemolysins that cause the incomplete lysis or RBC’s 2. Beta Hemolytic Streptococci - secrete hemolysins that cause the complete lysis of RBC’s 3. Gamma Hemolytic Streptococci - do not secrete any hemolysins C. Coagulase - cause blood to coagulate Blood clots protect bacteria from phagocytosis from WBC’s and other host defenses Staphylococci - are often coagulase positive • boils • abscesses D. Kinases - enzymes that dissolve blood clots 1. Streptokinase - Streptococci 2. Staphylokinase - Staphylococci Helps to spread bacteria - Bacteremia Streptokinase - used to dissolve blood clots in the Heart (Heart Attacks due to obstructed coronary blood vessels) E. Hyaluronidase Breaks down Hyaluronic acid (found in connective tissues) “Spreading Factor” mixed with a drug to help spread the drug thru a body tissue F. Collagenase Breaks down collagen (found in many connective tissues) Clostridium perfringens - Gas Gangrene • uses this to spread thru muscle tissue G. Necrotizing Factor - causes death (necrosis) to tissue cells “Flesh Eating Bacteria” Necrotizing fasciitis Summary of How Bacterial Pathogens Penetrate Host Defenses 1. Adherence 2. Capsule 3. Enzymes • • • • • • • A. leukocidins B. Hemolysins C. Coagulase D. Kinases E. Hyaluronidase F. Collagenase G. Necrotizing Factor 4. Toxins Poisonous substances produced by microorganisms toxins - primary factor - pathogenicity 220 known bacterial toxins • 40% cause disease by damaging the Eukaryotic cell membrane Toxemia • Toxins in the bloodstream 2 Types of Toxins 1. Exotoxins • secreted outside the bacterial cell 2. Endotoxins • part of the outer cell wall of Gram (-) bacteria Exotoxins Mostly seen in Gram (+) Bacteria Most gene that code for exotoxins are located on plasmids or phages 3 Types of Exotoxins 1. Cytotoxins • kill cells 2. Neurotoxins • interfere with normal nerve impulses 3. Enterotoxins • effect cells lining the G.I. Tract Response to Toxins If exposed to exotoxins: antibodies against the toxin (antitoxins) Exotoxins inactivated ( heat, formalin or phenol) no longer cause disease, but stimulate the production of antitoxin • altered exotoxins - Toxoids Toxoids - injected to stimulate the production of antitoxins and provide immunity Example: DPT Vaccine D - Diphtheria • Corynebacterium diphtheriae P - Pertussis • Bordetello pertussis T - Tetanus • Clostridium tetani DPT - Diphtheria Toxoid Pertussis Antigen Tetanus Toxoid Required Immunizations in Illinois 1. Diphtheria 2. Pertussis 3. Tetanus 4. Measles 5. Mumps 6. Rubella Corynebacterium diphtheriae Bordetello pertussis Clostridium tetani Measles virus Mumps virus Rubella virus • German Measles 7. Polio 8. Hib 9. Hepatitis B 10.Chicken Pox Polio virus Haemophilus influenzae Hepatitis B Virus Varicella-zoster virus Type of Vaccines D P T M M R Polio • Salk • Sabin Hib HBV Toxoid Antigen Toxoid Attenuated Attenuated Attenuated IPV – Inactivated Polio virus (Killed) 1953 OPV – Oral Polio vaccine (attenuated) 1964 Conjugated vaccine Recombinant vaccine (antigen) yeast • Capsid produced by genetically engineered yeast Chicken Pox Attenuated Most genes that code for exotoxins - plasmids or phages Lysogenic convergence Diphtheria Cytotoxin inhibits protein synthesis resulting in cell death Pseudomembrane • fibrin, dead tissue, bacterial cells Lysogenic Convergence Scarlet Fever Streptococcus pyogenes • lysogenic convergence prophage • cytotoxin - damages blood capillaries and results in a skin rash • Strep Thoat with a rash Diseases caused by Neurotoxins Botulism • Clostridium botulinum • Gram (+), anaerobic, spore-forming rod, found in soil • works at the neuromuscular junction • prevents impulse from nerve cell to muscle cell • results in muscle paralysis Tetanus (Lock Jaw) Clostridium tetani Gram (+), spore-forming, anaerobic rod neurotoxin acts on nerves, resulting in the inhibition of muscle relaxation tetanospasmin - “spasms” or “Lock Jaw” Diseases caused by Enterotoxins Cholera • Vibrio cholerae • Gram (-) comma shaped rods Cholera toxin Converts ATP into cAMP causes cells to excrete Cl- ions and inhibits absorption of Na+ ions Electrolyte imbalance H2O leaves by osmosis H2O Loss (Diarrhea) Severe cases, 12 - 20 liters of liquid lost in a day Untreated cases - Mortality Rate about 50% Mortality may be reduced to about 1% • administering fluids and electrolytes EHEC (Enterohemorrhagic E. coli) E. coli (0157:H7) enterotoxin causes a hemolytic inflammation of the intestines results in bloody diarrhea • Toxin • • • • • alters the 60S ribosomal subunit inhibits Protein Synthesis Results in cell death lining of intestine is “shed” Bloody Diarrhea (Dysentary) Endotoxins - part of the Gram (-) Bacterial cell wall LPS (Lipopolysaccharides) • O Antigen • Lipid A Lipid A - Toxin portion of the LPS • responsible for Fever that is associated with many Gram (-) Bacterial infections • Gram (-) cells are “digested” endotoxins are released - fever • Antibiotics