* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download C. Trachomatis
Survey
Document related concepts
Transcript
STD
Sexually Transmitted disease
Sexually Transmitted and Sexually
Transmissible Microorganisms
Transmitted in Adults Predominantly by Sexual Intercourse
Bacteria
• Neisseria gonorrhoeae
• Chlamydia trachomatis
• Treponema pallidum
• Haemophilus ducreyi
• Calymmatobacterium granulomatis(Klebsiella granulomatis)
• Ureaplasma urealyticum
• Viruses
• HIV (types 1 and2 )
• Human T-cell lymphotropic virus type I
• Herpes simplex virus type 2
• Human papillomavirus (multiple genotypes)
• Hepatitis Bvirus
• Molluscum contagiosum virus
• Othera
• Trichomonas vaginalis
• Phthirus pubis
Sexual Transmission Repeatedly Described but Not
Well Defined or Not the Predominant Mode
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
Bacteria
Mycoplasma hominis
Mycoplasma genitalium
Gardnerella vaginalis and other vaginal bacteria
Group B Streptococcus
Helicobacter cinaedi
Helicobacter fennelliae
Viruses
Cytomegalovirus
Human T-cell lymphotropic virus type II
Hepatitis C, D )?(viruses
Herpes simplex virus type 1
Epstein-Barr virus)?)
Human herpesvirus type 8
Othera
Candida albicans
Sarcoptes scabiei
Transmitted by Sexual Contact
Involving Oral-Fecal Exposure
• Bacteria
• Shigella spp.
• Campylobacter spp.
• Viruses
• Hepatitis A virus
• Othera
• Giardia lamblia
• Entamoeba histolytica
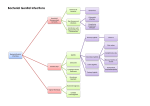
Major STD Syndromes and Sexually Transmitted
males
Urethritis:
•
•
•
•
•
•
•
•
•
Neisseria gonorrhoea
Chlamydia trachomatis
Mycoplasma genitalium
Ureaplasma urealyticum
subspecies urealyticum?
Trichomonas vaginalis
HSV
perhaps adenovirus
Coliform bacteria can cause urethritis
in men who practice insertive anal
intercourse.
Epididymitis
•
•
C. trachomatis
N. gonorrhoeae
Urethritis in Men
• Urethritis in men produces urethral discharge, dysuria, or
both, usually without frequency of urination.
• Until recently ,C. trachomatis caused ~30–40% of cases of
nongonococcal urethritis (NGU); however, the proportion of
cases due to this organism may have declined in some
populations served by effective chlamydial-control
programs, and older men with urethritis appear less likely to
have chlamydial infection.
• HSV and T. vaginalis each cause a small proportion of NGU
cases
• Recently, multiple studies have consistently implicated M.
genitalium as a probable cause of many Chlamydia-negative
cases.
Urethritis in Men
• Fewer studies than in the past have
implicated Ureaplasma ;the
ureaplasmas have been
differentiated into U. urealyticum
and U. parvum ,and a few studies
suggest that U. urealyticum—is
associated with NGU.
Urethritis in Men
• bacteria can cause urethritis in men The
initial diagnosis of urethritis in men
currently includes specific tests only for
N. gonorrhoeae and C. trachomatis. The
following summarizes the approach to the
patient with suspected urethritis:
Establish the presence
of urethritis
• If proximal-to-distal "milking" of the
urethra does not express a purulent or
mucopurulent discharge, even after the
patient has not voided for several hours
(or preferably overnight), a Gram'sstained smear of overt discharge or of an
anterior urethral specimen obtained by
passage of a small urethrogenital swab 2–3
cm into the urethra usually reveals 5
neutrophils per 1000x field in areas
containing cells; in gonococcal infection,
such a smear usually reveals gram-negative
intracellular diplococci as well.
Establish the presence
of urethritis
• Alternatively, the centrifuged sediment of
the first 20–30 mL of voided urine—
ideally collected as the first morning
specimen—can be examined for
inflammatory cells, either by microscopy
showing 10 leukocytes per high-power field
• Patients with symptoms who lack objective
evidence of urethritis may have functional
rather than organic problems and generally
do not benefit from repeated
Evaluate for complications or
alternative diagnoses.
• A brief history and examination will exclude
epididymitis and systemic complications, such as
disseminated gonococcal infection (DGI) and
Reiter's syndrome.
• Although digital examination of the prostate
gland seldom contributes to the evaluation of
sexually active young men with urethritis.
• men with dysuria who lack evidence of urethritis
as well as sexually inactive men with urethritis
should undergo prostate palpation, urinalysis, and
urine culture to exclude bacterial prostatitis and
cystitis.
Evaluate for gonococcal
chlamydial infection
• An absence of typical gram-negative diplococci on
Gram's-stained smear of urethral exudate
containing inflammatory cells warrants a
preliminary diagnosis of NGU and should lead to
testing of the urethral specimen for C.
trachomatis.
• However, an increasing proportion of men with
symptoms and/or signs of urethritis are
simultaneously assessed for infection with N.
gonorrhoeae and C. trachomatis by "multiplex"
nucleic acid amplification tests (NAATs) of earlymorning first-voided urine.
Evaluate for gonococcal
and chlamydial infection
• Culture or NAAT for N. gonorrhoeae
may be positive when Gram's staining
is negative
• certain strains of N. gonorrhoeae can
result in negative urethral Gram's
stains in up to 30% of cases of
urethritis.
Evaluate for gonococcal
and chlamydial infection
• Results of tests for gonococcal and
chlamydial infection predict the
patient's prognosis
• can guide both the counseling given
to the patient and the management
of the patient's sexual partner(s).
• Treat urethritis promptly, while test
results are pending.
Acute epididymitis
• Acute epididymitis, almost always
unilateral, produces pain, swelling, and
tenderness of the epididymis, with or
without symptoms or signs of
urethritis.
• This condition must be differentiated
from testicular torsion, tumor, and
trauma.
Acute epididymitis
• Torsion, a surgical emergency, usually
occurs in the second or third decade
of life and produces a sudden onset
of pain, elevation of the testicle
within the scrotal sac, rotation of
the epididymis from a posterior to an
anterior position, and absence of
blood flow on Doppler examination or
scan.
Acute epididymitis
• Persistence of symptoms after a
course of therapy for
epididymitis suggests the
possibility of testicular tumor or
of a chronic granulomatous
disease, such as tuberculosis.
Acute epididymitis
• In sexually active men under age 35, acute
epididymitis is caused most frequently by C.
trachomatis and less commonly by N. gonorrhoeae
and is usually associated with overt or subclinical
urethritis.
• Acute epididymitis occurring in older men or
following urinary tract instrumentation is usually
caused by urinary pathogens.
• epididymitis in men who have practiced insertive
rectal intercourse is often caused by
Enterobacteriaceae.
• These men usually have no urethritis but do have
bacteriuria.
Lower genital tract
infections: females
urethritis
• C. trachomatis
• N. gonorrhoeae,
• HSV
Mucopurulent
cervicitis
• C. trachomatis,
• N. gonorrhoeae
• M. genitalium
Vulvitis
Candida albicans
HSV
Vulvovaginitis
C. albicans
T. vaginalis
Bacterial vaginosis
associated bacteria
Urethritis and the Urethral Syndrome
in Women
• C. trachomatis ,N. gonorrhoeae ,and occasionally
HSV cause symptomatic urethritis—known as the
urethral syndrome in women—that is
characterized by "internal" dysuria (usually
without urinary urgency or frequency), pyuria, and
an absence of Escherichia coli and other
uropathogens in urine at counts of 100/mL.
• In contrast, the dysuria associated with vulvar
herpes or vulvovaginal candidiasis (and perhaps
with trichomoniasis) is often described as
"external," being caused by painful contact of
urine with the inflamed or ulcerated labia or
introitus
Urethritis and the Urethral Syndrome
in Women
• Acute onset, association with urinary
urgency or frequency, hematuria, or
suprapubic bladder tenderness suggests
bacterial cystitis.
• Among women with symptoms of acute
bacterial cystitis, costovertebral pain and
tenderness or fever suggests acute
pyelonephritis.
• management of bacterial urinary tract
infection.
Urethritis and the Urethral
Syndrome in Women
• An STI etiology of the urethral syndrome is
suggested by young age,
-more than one current sexual partner.
-a new partner within the past month.
-a partner with urethritis.
- coexisting mucopurulent cervicitis .
• Gonorrhea and chlamydial infection should be
sought by specific tests (nucleic acid
amplification tests =NAATs).
• Among dysuric women with sterile pyuria caused
by infection with N. gonorrhoeae or C.
trachomatis ,appropriate treatment alleviates
dysuria.
Urethritis and the Urethral
Syndrome in Women
• Signs of vulvovaginitis, coupled with symptoms of
external dysuria, suggest vulvar infection (e.g.,
with HSV or Candida albicans
• The finding of a single urinary pathogen, such as
E. coli or Staphylococcus saprophyticus ,at a
concentration of 100/mL in a properly collected
specimen of midstream urine from a dysuric
woman with pyuria indicates probable bacterial
UTI,
• whereas pyuria with <100conventional
uropathogens per milliliter of urine ("sterile"
pyuria) suggests acute urethral syndrome due to
C. trachomatis or N. gonorrhoeae .
Mucopurulent cervicitis
• C. trachomatis,
• N. gonorrhoeae
• M. genitalium
Mucopurulent cervicitis
(MPC)
• MPC in women represents the "silent partner" of
urethritis in men, being equally common and often
caused by the same agents( N. gonorrhoeae ,C.
trachomatis ,or—as shown by case-control
studies—M. genitalium ;)however, MPC is more
difficult than urethritis to recognize.
• As the most common manifestation of these
serious bacterial infections in women.
• MPC can be a harbinger or sign of upper genital
tract infection, also known as pelvic inflammatory
disease (PID)
Mucopurulent cervicitis
(MPC)
• In a prospective study consecutive
patients with MPC [defined on the basis of
yellow endocervical mucopus or
30polymorphonuclear leukocytes
(PMNs)/1000x microscopic field]
• who were seen slightly more than onethird of cervicovaginal specimens tested
for C. trachomatis ,N. gonorrhoeae ,M.
genitalium ,HSV, and T. vaginalis revealed
no identifiable etiology
MG/GC
2%
MG/GC/CT
1%
MG/CT
2%
HSV
5%
GC/CT
7%
MG
8%
No organism
35%
TV
10%
GC
13%
CT
17%
Organisms detected among female STD clinic patients
GC-gonococcus
CT-Chlamydiatrachomatis
MG-Mycoplasma genitalium
TV-Trichomonas vaginalis
HSV-herpes simplex virus
Mucopurulent cervicitis
(MPC)
• The diagnosis of MPC rests on the detection of
yellow mucopurulent discharge from the cervical os
or of increased numbers of PMNs(20) in Gram'sstained or Papanicolaou-stained smears of
endocervical mucus.
• MPC due to C. trachomatis can also produce
edematous cervical and endocervical bleeding upon
gentle swabbing.
• Detection of intracellular gram-negative diplococci
in carefully collected endocervical mucus is quite
specific but 50 %sensitive for gonorrhea.
• cervicitis caused by HSV produces ulcerative lesions
on the epithelium of the exocervix.
Ulcerative lesions of the genitalia
•HSV-1, HSV-2,
•Treponema pallidum,
• Haemophilus ducreyi.
• C. trachomatis(LGV strains)
•Calymmatobacterium granulomatis
Ulcerative lesions of the genitalia
• Genital ulceration reflects a set of important
STIs, most of which sharply increase the risk of
sexual acquisition and shedding of HIV.
• In a study of genital ulcers PCR testing of ulcer
specimens demonstrated
- HSV in 62% of patients.
-Treponema pallidum in 13%.
-Haemophilus ducreyi in 12–20%.
• Today, genital herpes probably represents an
even higher proportion of genital ulcers in the
industrialized countries.
Ulcerative lesions of the genitalia
• In Asia and Africa, chancroid was once considered
the most common type of genital ulcer, followed in
frequency by primary syphilis and then genital
herpes.
• With increased efforts to control chancroid and
syphilis, together with more frequent recurrences
or persistence of genital herpes attributable to
HIV infection, PCR testing of genital ulcers now
clearly implicates genital herpes as the most
common cause of genital ulceration in most
developing countries.
• LGV and donovanosis (granuloma inguinale) continue
to cause genital ulceration in developing countries.
Ulcerative lesions of the genitalia
Other causes of genital ulcer include
• candidiasis and traumatized genital
warts(both readily recognized)
• lesions due to genital involvement by more
widespread dermatoses.
• cutaneous manifestations of systemic
diseases, such as genital mucosal
ulceration in Stevens-Johnson syndrome or
Behçet's disease.
Ulcerative lesions of the genitalia
diagnosis
• Although most genital ulcerations cannot be
diagnosed confidently on clinical grounds alone,
clinical findings plus epidemiologic considerations
can usually guide initial management pending
results of further tests.
• Clinicians should order a rapid serologic test for
syphilis in all cases of genital ulcer.
• a dark-field or direct immunofluorescence test
(or PCR test, where available) for T. pallidum in all
lesions except those highly characteristic of
infection with HSV (i.e., those with herpetic
vesicles).
• All patients presenting with genital ulceration
should be counseled and tested for HIV infection.
Ulcerative lesions of the genitalia
HSV
• Typical vesicles or pustules or a cluster of
painful ulcers preceded by vesiculopustular
lesions suggests genital herpes.
• These typical clinical manifestations make
detection of the virus optional; however,
many patients want confirmation of the
diagnosis, and differentiation of HSV-1
from HSV-2 has prognostic implications,
since the latter causes more frequent
genital recurrences.
Ulcerative lesions of the genitalia
HSV
• Atypical" or clinically trivial ulcers may be
more common manifestations of genital
herpes than classic vesiculopustular
lesions. Specific tests for HSV in such
lesions are therefore indicated.
• HSV infection is best confirmed in the
laboratory by detection of virus, viral
antigen, or viral DNA in scrapings from
lesions.
• HSV DNA detection by PCR, when
available, is the most sensitive laboratory
technique.
Ulcerative lesions of the genitalia
HSV
• Type-specific serologic tests for serum antibody to
HSV-2, now commercially available, may give
negative results, especially when patients present
early with the initial episode of genital erpes or
when HSV-1 is the cause of genital herpes.
Furthermore, a positive test for antibody to HSV-2
does not prove that the current lesions are
herpetic.
• a positive HSV-2 serology does enable the clinician
to tell the patient that he or she has probably had
genital herpes, should learn to recognize symptoms,
should avoid sex during recurrences, and should
consider use of condoms or suppressive antiviral
therapy, both of which can reduce transmission to a
sexual partner .
Ulcerative lesions of the genitalia
Syphilis
• Painless, nontender, indurated ulcers with firm,
nontender inguinal adenopathy suggest primary
syphilis.
• If dark-field examination and a rapid serologic
test for syphilis are initially negative and the
patient will comply with follow-up and sexual
abstinence.
• the performance of two more dark-field
examinations on successive days before treatment
is begun will improve the sensitivity of the
diagnosis of syphilis.
• repeated serologic testing for syphilis 1 or 2
weeks after treatment of seronegative primary
syphilis usually demonstrates seroconversion.
Ulcerative lesions of the genitalia
chancroid
• ulcers are painful and purulent especially if
inguinal lymphadenopathy with fluctuance or
overlying erythema is notedor
• if the patient has recently had a sexual exposure
elsewhere in a chancroid-endemic area (e.g., a
developing country).
• Enlarged, fluctuant lymph nodes should be
aspirated for culture or PCR tests to detect H.
ducreyi as well as for Gram's staining and culture
to rule out the presence of other pyogenic
bacteria.
Ulcerative lesions of the genitalia
donovanosis, carcinoma, and other nonvenereal
dermatoses
• When genital ulcers persist beyond the natural
history of initial episodes of herpes (2–3 weeks)
or of chancroid or syphilis (up to 6 weeks) and do
not resolve with syndrome-based antimicrobial
therapy.
• then—in addition to the usual tests for herpes,
syphilis, and chancroid—biopsy is indicated to
exclude donovanosis, carcinoma, and other
nonvenereal dermatoses.
• HIV serology should also be undertaken, since
chronic, persistent genital herpes is common in
AIDS.
Ulcerative lesions of the genitalia
• Usual causes
– Herpes simplex virus (HSV2)
– Treponema pallidum( primary syphilis)
– Haemophilus ducreyi (chancroid)
Ulcerative lesions of the
genitalia
• Usual initial laboratory evaluation
– Dark-field exam, direct FA, or PCR for T.
pallidum
– RPR or VDRL test for syphilis (if negative but
primary syphilis suspected, repeat in 1 week)
– culture, direct FA, ELISA, or PCR for HSV
– consider HSV-2-specific serology.
– In chancroid-endemic area: PCR or culture for
H. ducreyi
Major STD Syndromes and Sexually Transmitted
Intestinal infections
Proctitis
• C. trachomatis ,N. gonorrhoeae ,HSV ,T. pallidum
Proctocolitis or enterocolitis
• Campylobacter spp ,.Shigella spp ,.Entamoeba
histolytica ,other enteric pathogens
Enteritis
• Giardia lamblia
Proctitis, Proctocolitis,
Enterocolitis, and Enteritis
• Sexually acquired proctitis, with inflammation
limited to the rectal mucosa (the distal 10–12 cm),
results from direct rectal inoculation of typical
STD pathogens
• proctocolitis inflammation extending from the
rectum to the colon.
• enterocolitis inflammation involving both the small
and the large bowel.
• enteritis inflammation involving the small bowel
alone.
• proctocolitis ,enterocolitis ,enteritis can result
from ingestion of typical intestinal pathogens
through oral-anal exposure during sexual contact.
Proctitis, Proctocolitis,
Enterocolitis, and Enteritis
• Anorectal pain and mucopurulent, bloody rectal
discharge suggest proctitis or protocolitis.
• Proctitis commonly produces tenesmus (causing
frequent attempts to defecate, but not true
diarrhea) and constipation.
• whereas proctocolitis and enterocolitis more
often cause true diarrhea.
• In all three conditions, anoscopy usually shows
mucosal exudate and easily induced mucosal
bleeding sometimes with petechiae or mucosal
ulcers.
• Exudate should be sampled for Gram's staining
and other microbiologic studies.
proctitis
• Acquisition of HSV ,N. gonorrhoeae ,or C.
Trachomatis during receptive anorectal
intercourse( causes most cases of infectious
proctitis in women and homosexual men).
• Primary and secondary syphilis can also produce
anal or anorectal lesions, with or without
symptoms.
• Gonococcal or chlamydial proctitis typically
involves the most distal rectal mucosa and is
clinically mild, without systemic manifestations.
• primary proctitis due to HSV produce severe
anorectal pain and often cause fever.
Enteritis and
proctocolitis
• Diarrhea and abdominal bloating or cramping pain
without anorectal symptoms and with normal
findings on anoscopy and sigmoidoscopy occur with
inflammation of the small intestine (enteritis) or
with proximal colitis.
• In homosexual men without HIV infection,
enteritis is often attributable to Giardia lamblia .
• Sexually acquired proctocolitis is most often due
to Campylobacter or Shigella spp.
proctocolitis
• Two species initially isolated in association
with intestinal symptoms in homosexual
men are now known as Helicobacter cinaedi
and Helicobacter fennelliae.
• both have subsequently been isolated from
the blood of HIV-infected men with a
syndrome of multifocal dermatitis and
arthritis .
The End