* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download How to prescribe antibiotics: maybe it’s not as simple as
Gastroenteritis wikipedia , lookup
Bacterial cell structure wikipedia , lookup
Human microbiota wikipedia , lookup
Triclocarban wikipedia , lookup
Traveler's diarrhea wikipedia , lookup
Disinfectant wikipedia , lookup
Infection control wikipedia , lookup
Clostridium difficile infection wikipedia , lookup
Neonatal infection wikipedia , lookup
Staphylococcus aureus wikipedia , lookup
Urinary tract infection wikipedia , lookup
Bacterial morphological plasticity wikipedia , lookup
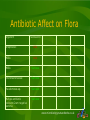
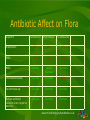
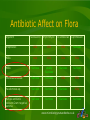
Microbiology Nuts & Bolts Session 4 Dr David Garner Consultant Microbiologist www.microbiologynutsandbolts.co.uk Aims & Objectives • To discuss 3 common clinical scenarios from a microbiology perspective • To understand how to interpret basic microbiology results • To consider the benefits and potential pitfalls of prescribing antibiotics • To look to the future of microbiology and how this will impact primary care www.microbiologynutsandbolts.co.uk Case 1 www.microbiologynutsandbolts.co.uk Mary • 70 years old • Presents with cough, increasing shortness of breath, increasingly purulent sputum • Past Medical History – Hypertension, Type 2 Diabetes, Chronic Obstructive Pulmonary Disease • On examination – Temperature 37.5 oC – Crepitations at the right base – B.P. 140/85, H.R. 98 bpm How should Mary be managed? www.microbiologynutsandbolts.co.uk Questions to ask yourself… • • • • • • • What urgent care does she need? Does she have an infection? What is the likely source of infection? What are the likely causes of the infection? Does she need secondary care? Does she need further investigation? Does she require antibiotic treatment? www.microbiologynutsandbolts.co.uk Differential Diagnosis British Thoracic Society Guidelines for Community Acquired Pneumonia (CAP) •Cough PLUS one other respiratory tract symptom – Shortness of breath – Purulent sputum – Chest pain Exacerbation of COPD • Shortness of breath • Purulent sputum • Amount of sputum •New focal chest signs – – – – Reduced expansion Bronchial breathing Dull percussion Vocal resonance •Systemic symptoms – Fever, sweats, shivers, aches & pains •No other explanation www.microbiologynutsandbolts.co.uk • • • • Diagnosed with Exacerbation of COPD Sputum Prescribed Amoxicillin PO Planned Chest X-ray if not improving www.microbiologynutsandbolts.co.uk How to interpret a sputum result? • Appearance – Mucoid, Salivary, Purulent, Blood Stained… • Microscopy – Gram’s stain, Ziehl Nielsen (ZN) stain… • Culture – Is the organism consistent with the clinical picture? www.microbiologynutsandbolts.co.uk Appearance of sputum • Salivary – Spit not phlegm, risk of contamination • Mucoid – Upper respiratory tract specimen, no evidence of inflammation – Beware neutropaenic patients • Purulent – Pus, indicates inflammation not infection • Blood stained – May indicate infection but not pathognomic www.microbiologynutsandbolts.co.uk Causes of Respiratory Infections Community Acquired Pneumonia • Viruses: – – – – RSV Influenza Parainfluenza Adenovirus – – – – – – – – S. pneumoniae H. influenzae S. aureus M. pneumonia C. pneumoniae L. pneumophila P. aeruginosa (if COPD) M. tuberculosis • Bacteria: Exacerbation of COPD • Viruses: – – – – – RSV Rhinovirus Influenza Parainfluenza Adenovirus – – – – S. pneumoniae H. influenzae S. aureus M. catarrhalis • Bacteria: www.microbiologynutsandbolts.co.uk Culture: classification of bacteria Gram’s Stain Positive Cocci No Stain Uptake Negative Bacilli Cocci Bacilli Acid Fast Bacilli Non-culturable www.microbiologynutsandbolts.co.uk Causes of LRTI usually originate in the upper respiratory tract Culture: how is sputum processed? • Plated to mixture of selective and non-selective agar depending on clinical details – E.g. Cystic Fibrosis = B. cepacia agar • Incubated for 48 hours before reporting • Sensitivities take a further 24-48 hours • Total time 48-96 hours after receipt. www.microbiologynutsandbolts.co.uk Community Normal Flora www.microbiologynutsandbolts.co.uk What happens when patients are given antibiotics? www.microbiologynutsandbolts.co.uk Antibiotics Change Normal Flora www.microbiologynutsandbolts.co.uk Back to Mary… • Sputum – Purulent – Culture Heavy Growth of Moraxella catarrhalis • Resistant to Amoxicillin & Clarithromycin • Sensitive to Co-amoxiclav & Doxycycline How would you manage Mary now? – Call to Mary, she was feeling much better and finished 7 days of Amoxicillin Should she be given prophylactic antibiotics? www.microbiologynutsandbolts.co.uk Prophylactic Antibiotics Benefits • frequency of exacerbations • Preservation of lung function • use of steroids Potential Drawbacks • Cautions and contraindications – e.g. macrolides and quinolones with myasthenia gravis • Allergies to antibiotics Problem: most studies on antibiotic prophylaxis do not look at long-term consequences – choice for treatment • Side effects of the antibiotic? – e.g. Azithromycin and bone marrow and renal impairment • What monitoring of your patient do you have to do? – e.g. Azithromycin and FBC and U&Es • ↑ Antibiotic resistance www.microbiologynutsandbolts.co.uk Any Questions about Case 1? www.microbiologynutsandbolts.co.uk Case 2 www.microbiologynutsandbolts.co.uk Jack • 45 years old • Presents with small pre-tibial laceration • Ignored for few days now has slightly green slough • Type 2 Diabetic • Normal temperature, heart rate and blood pressure How should Jack be managed? www.microbiologynutsandbolts.co.uk • Wound swab taken • Started empirically PO Flucloxacillin 500mg QDS • Advised to have daily dressing of wound with practice nurse • 48 hours later not much change, switched to Erythromycin • 96 hours after first consultation swab shows: – Mixed faecal flora • Changed to PO Co-amoxiclav 625mg TDS – Wound swab repeated Would you have done anything different? www.microbiologynutsandbolts.co.uk • 1 week later reviewed wound still sloughy • Repeat wound swab – Heavy growth of Pseudomonas sp. sensitive to Ciprofloxacin • Patient changed to PO Ciprofloxacin 500mg BD Would you do anything different? www.microbiologynutsandbolts.co.uk • 2 weeks after initial injury • Wound painful, surrounding erythema and increasingly purulent discharge How are you going to manage Jack now? www.microbiologynutsandbolts.co.uk Culture: how are wound swabs processed? • Cannot do a Gram-stain • Pus is always better! • Mixture of selective and non-selective agar plates • Culture 24-48 hours • Sensitivities 24-48 hours • Swab total time 48-96 hours • A swab cannot diagnose an infection, that is a clinical judgement, it tells you what might be causing the infection www.microbiologynutsandbolts.co.uk How to interpret a wound swab result? • Appearance – Not available • Microscopy – Not available • Culture – Is the organism consistent with the clinical picture? www.microbiologynutsandbolts.co.uk Types & Causes of Bacterial Skin Infections • Ulcers – Staphylococcus aureus, b-haemolytic Streptococcii • Become colonised with bacteria, especially Enterobacteriaceae that DO NOT need treating in most patients • Take samples from “healthy” base after debriding slough • Only treat if increasing pain, erythema or purulent discharge • Cellulitis – Staphylococcus aureus, b-haemolytic Streptococcii www.microbiologynutsandbolts.co.uk Culture: classification of bacteria Gram’s Stain Positive Cocci No Stain Uptake Negative Bacilli Cocci Bacilli Acid Fast Bacilli Non-culturable Skin infections are usually from direct inoculation or haematogenous spread www.microbiologynutsandbolts.co.uk Classification of Grampositive cocci www.microbiologynutsandbolts.co.uk b-haemolytic Streptococci Group Names Flora Clinical A S. pyogenes Mucus membranes? Tonsillitis, cellulitis, septic arthritis, necrotising fasciitis… B S. agalactiae Bowel, genital tract (females) Neonatal sepsis, septic arthritis, infective endocarditis, association with malignancy? C S. S. S. S. Mucus membranes, animals? Tonsillitis, cellulitis, septic arthritis D Enterococcus faecalis Enterococcus faecium Bowel Infective endocarditis, IV catheter associated bacteraemia F “Milleri group” S. intermedius S. anginosus S. constellatus Bowel Empyema (pleural and biliary), bowel inflammation and perforation… G S. dysgalactiae Mucus membranes, bowel? Tonsillitis, cellulitis, septic arthritis, association with malignancy? dysgalactiae equi equisimilis zooepidemicus www.microbiologynutsandbolts.co.uk Community Normal Flora www.microbiologynutsandbolts.co.uk What happens when patients are given antibiotics? www.microbiologynutsandbolts.co.uk Antibiotics Change Normal Flora www.microbiologynutsandbolts.co.uk Antibiotic Affect on Flora Organism Flucloxacillin Streptococci MSSA MRSA Enterobacteriaceae Pseudomonas sp. Multiple antibiotic resistant Gram-negative bacteria www.microbiologynutsandbolts.co.uk Antibiotic Affect on Flora Organism Flucloxacillin Streptococci Kills MSSA Kills MRSA Survives Enterobacteriaceae Survives Pseudomonas sp. Survives Multiple antibiotic resistant Gram-negative bacteria Survives www.microbiologynutsandbolts.co.uk Antibiotic Affect on Flora Organism Flucloxacillin Streptococci Kills MSSA Kills MRSA Survives Enterobacteriaceae Survives Pseudomonas sp. Survives Multiple antibiotic resistant Gram-negative bacteria Survives Erythromycin www.microbiologynutsandbolts.co.uk Antibiotic Affect on Flora Organism Flucloxacillin Erythromycin Streptococci Kills Kills MSSA Kills Kills MRSA Survives Usually Survives Enterobacteriaceae Survives Survives Pseudomonas sp. Survives Survives Multiple antibiotic resistant Gram-negative bacteria Survives Survives www.microbiologynutsandbolts.co.uk Antibiotic Affect on Flora Organism Flucloxacillin Erythromycin Streptococci Kills Kills MSSA Kills Kills MRSA Survives Usually Survives Enterobacteriaceae Survives Survives Pseudomonas sp. Survives Survives Multiple antibiotic resistant Gram-negative bacteria Survives Survives Co-amoxiclav www.microbiologynutsandbolts.co.uk Antibiotic Affect on Flora Organism Flucloxacillin Erythromycin Co-amoxiclav Streptococci Kills Kills Kills MSSA Kills Kills Kills MRSA Survives Usually Survives Survives Enterobacteriaceae Survives Survives Kills Pseudomonas sp. Survives Survives Survives Multiple antibiotic resistant Gram-negative bacteria Survives Survives Survives www.microbiologynutsandbolts.co.uk Antibiotic Affect on Flora Organism Flucloxacillin Erythromycin Co-amoxiclav Streptococci Kills Kills Kills MSSA Kills Kills Kills MRSA Survives Usually Survives Survives Enterobacteriaceae Survives Survives Kills Pseudomonas sp. Survives Survives Survives Multiple antibiotic resistant Gram-negative bacteria Survives Survives Survives Ciprofloxacin www.microbiologynutsandbolts.co.uk Antibiotic Affect on Flora Organism Flucloxacillin Erythromycin Co-amoxiclav Ciprofloxacin Streptococci Kills Kills Kills Survives MSSA Kills Kills Kills Kills MRSA Survives Usually Survives Survives Survives Enterobacteriaceae Survives Survives Kills Kills Pseudomonas sp. Survives Survives Survives Kills Multiple antibiotic resistant Gram-negative bacteria Survives Survives Survives Survives www.microbiologynutsandbolts.co.uk Back to Jack… • Admitted to secondary care with established infection with MRSA cellulitis • Blood cultures positive for MRSA – 20% mortality – National target ZERO preventable MRSA bacteraemias • Fortunately made a full recovery after treatment with IV Teicoplanin for 2 weeks Did Jack actually have an infection to begin with? Could his later infection have been prevented? www.microbiologynutsandbolts.co.uk Any Questions about Case 2? www.microbiologynutsandbolts.co.uk Case 3 www.microbiologynutsandbolts.co.uk Betty • 87 years old nursing home resident • Presents with confusion and new incontinence • On examination – Temperature 37.5 oC – Crackles throughout precordium – Cardiovascularly stable How should Betty be managed? www.microbiologynutsandbolts.co.uk • Likely urinary tract infection • No systemic signs of evolving sepsis • Treated for simple UTI with 3 days of Trimethoprim www.microbiologynutsandbolts.co.uk • 2 days later not much better • Still no systemic signs of evolving sepsis • Check of recent bloods – eGFR >60ml/min • Urine – Dipstick • Leucocytes ++, Nitrites ++ – MSU (How do you take a proper MSU?) sent to lab • Microscopy How would you manage Betty now? • Started on second line Nitrofurantoin www.microbiologynutsandbolts.co.uk How to interpret a urine result? • Urine dipstick – Poor PPV, Good NPV • Microscopy – White blood cells, red blood cells, epithelial cells • Culture result – Is the organism consistent with the clinical picture? www.microbiologynutsandbolts.co.uk Microscopy of urine • White blood cells – >100 x106/L definitely significant – >10 x106/L significant if properly taken MSU (rare!) • Red Blood Cells – Poor correlation with UTI, used by urologist and renal physicians • Epithelial cells – Indicator of contact with, and therefore contamination from, the perineum www.microbiologynutsandbolts.co.uk Culture: how is urine processed? • Day 1 Automated Microscopy – If values not significant reported as negative – If values significant or specific patient group cultured with direct sensitivities • Day 2 – Reported with identification and sensitivities • Patient groups always cultured – – – – Cancer and haematology Pregnant Urology Children < 5 years old www.microbiologynutsandbolts.co.uk 2 days later • • • • Much more confused, still incontinent Very distressed Vomiting, diarrhoea Urine result – Microscopy >100 x106/L WBC, no epithelial cells – Culture E. coli – Resistant to Amoxicillin, Co-amoxiclav, Trimethoprim, Cephradine, Ciprofloxacin – Sensitive to Nitrofurantoin – Further results to follow How would you manage Betty? What further results are to follow? www.microbiologynutsandbolts.co.uk • Admitted to secondary care for IV antibiotics • Started on Piptazobactam for sepsis, probably UTI • Further result on MSU – E. coli ESBL positive What is an ESBL? What should Betty be treated with? Why didn’t Nitrofurantoin work? www.microbiologynutsandbolts.co.uk Antibiotic dosing in renal failure • Many antibiotics require dose reduction in renal failure • eGFR is not an accurate predictor of renal function • Use Cockcroft Gault equation – Actual body weight or Ideal Body Weight (IBW) if weight > 20% above IBW – Also use IBW for patients with oedema & ascites www.microbiologynutsandbolts.co.uk How might weight effect Betty’s GFR (ml/min) Female, Age 87, Creatinine 75 Weight (kg) eGFR Calculated GFR Variance 45 63 33 -30 50 63 37 -26 55 63 40 -23 60 63 44 -19 65 63 47 -16 70 63 51 -12 75 63 55 -8 80 63 59 -4 www.microbiologynutsandbolts.co.uk How might weight effect Betty’s GFR (ml/min) Female, Age 87, Creatinine 75 Weight (kg) eGFR Calculated GFR Variance 45 63 33 -30 50 63 37 -26 55 63 40 -23 60 63 44 -19 65 63 47 -16 70 63 51 -12 75 63 55 -8 80 63 59 -4 www.microbiologynutsandbolts.co.uk Back to Betty… • Started IV Meropenem 500mg BD • 55kg, Creatinine 77 • Calculated GFR = 39 ml/min www.microbiologynutsandbolts.co.uk 48 hours later • Much improved, diarrhoea and vomiting settled • Bloods – WBC 19 x 109/L – CRP 198 – U&Es – Urea 12, Creat 150 • Blood Culture – Escherichia coli, resistant to Amoxycillin, Co-amoxiclav, Gentamicin, Trimethoprim, Ciprofloxacin, Piptazobactam, Ceftriaxone (ESBL positive) – Sensitive to Meropenem, Amikacin What should we do for Betty now? www.microbiologynutsandbolts.co.uk • Continued IV Meropenem as no oral alternatives • Given 7 days of antibiotics in total for severe UTI? • Made a full recovery and went back to her nursing home Warning – Betty is now known to be colonised with a Antibiotic-resistant E. coli so her future UTIs are likely to be resistant as well (it is part of her normal flora!) www.microbiologynutsandbolts.co.uk Caution: Extended Spectrum Beta-lactamase • Enzyme excreted into periplasmic space which inactivates antimicrobials by cleaving the blactam bond. • Cause resistance to almost all b-lactams including 3rd-generation cephalosporins • Associated with multiple antibiotic resistances • Can be chromosome, plasmid or transposon encoded • Can be constitutive or inducible • Ideally patients with ESBLs should be managed in side-rooms with contact precautions www.microbiologynutsandbolts.co.uk Transfer of antibiotic resistance www.microbiologynutsandbolts.co.uk Caution: Extended Spectrum Beta-lactamase Source: European Centre for Disease Prevention and Control Antimicrobial resistance surveillance in Europe 2011 www.microbiologynutsandbolts.co.uk The Future is Bleak • Increasing numbers of Meropenem resistant Enterobacteriaceae in the UK from overseas – NDM-1 = New Delhi Metallo-beta-lactamase – KPC = Klebsiella pneumoniae carbapenemase • Now starting to see Amikacin resistance as well • Only antibiotic left is Colistin – 60+ years old – Some bacteria are known to be inherently resistant (Proteus sp., Serratia sp.) – May become transferable and then have a real “superbug” for the post-antibiotic era… www.microbiologynutsandbolts.co.uk Conclusions • 3 clinical scenarios showing some of the pitfalls in managing apparently simple infections • Look at microbiology results in order – Appearance, Microscopy and Culture • There are significant benefits to antibiotics but increasingly there are also dangers • Conflict of medicine moving to 1o care but infections moving to 2o care – need for OPAT • The future is looking bleak, we need to try and preserve what we have for as long as we can… www.microbiologynutsandbolts.co.uk Any Questions? Available to buy on www.microbiologynutsandbolts.co.uk