* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Step into the void: Vestibular deficits in children with hearing loss
Survey
Document related concepts
Transcript
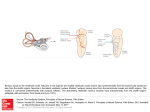
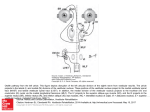
Step into the void: Vestibular deficits in children with hearing loss Genevieve DelRosario, MHS, PA-C University of Kansas Medical Center Kansas City, Kansas Objectives Review vestibular physiology and pathophysiology Discuss the evaluation of a child’s vestibular status Be able to develop a plan for a child with vestibular dysfunction Vestibular system: A “sixth sense” Allows us to know where we are in space Orient selves with respect to gravity Unifying system that allows us to process information from other senses Where does our sense of balance come from? Eyes Sensors in joints, muscles, and feet Balance organs in the ears Vestibular system Vestibular ocular system – Responsible for visual stabilization Vestibular spinal system – Maintains orientation of the body in space – Contributes to the postural tone necessary for the acquisition of motor development milestones Development of the vestibular system Very old in evolutionary terms Emerges early in embryonic development – Prior to vision and hearing Peak developmental time is 6-12 months Continues development through childhood http://www.qmw.ac.uk/~ugha014/vestibular%20stuff/vestibular3.html http://www.qmw.ac.uk/~ugha014/vestibular%20stuff/vestibular3.html Prevalence of vestibular dysfunction* 20-70% of children with hearing loss Higher in profound HL vs. severe Continuum of severity – Mild loss to vestibular areflexia * Angeli 2003. What happens in deaf/HOH children? Semicircular canals may be absent Hair cells may be damaged, absent, or reduced Nerve damage Enlarged vestibular aqueduct ??? Will a deaf child’s vestibular system get better? ……Maybe. Better or worse? In general, balance improves as you age – Vestibular maturation continues through adolescence Vestibular deficits in deaf/HOH may worsen – Small study showed progressive gross motor and balance difficulties1 – Contradicted by other studies2 1. Rine et al 2000. 2. Siegel et al 1991. How does it feel? http://www.theraider.net/films/crusade/making_4_postproduction.php How does it feel (adult perspective)? – Headache – Feeling of ear fullness – Imbalance to the point of being unable to walk – Bouncing and blurring of vision (oscillopsia) – Inability to tolerate head movement – Difficulty walking in the dark – Feel unsteady; actual unsteadiness while moving – Lightheadedness – Severe fatigue In severe cases, symptoms such as oscillopsia and problems with walking in the dark are not going to go away. www.vestibular.org Oscillopia www.dizziness-and-balance.com Signs of poor vestibular function Low muscle tone Delayed loss of primitive reflexes Delayed gross motor milestones Developmental delays Seizures Nystagmus Easy fatiguability Reflux Signs of poor vestibular function Low muscle tone – Delay in holding head up – “Snuggly” baby – “Floppy baby” – Arching of back Signs of poor vestibular function Delayed disappearance of newborn reflexes – Moro – ATNR: Asymmetric tonic next response – Usually disappear by 6-7 months http://www.frisbee.li/webobtimierte-bilder/abb1.jpg Signs of poor vestibular function Delayed motor milestones – Average deaf child walks at 14 months – Average child with Usher’s Type 1 walks at 20 mos – Delays sitting, crawling, climbing steps, hopping… – Speech delays What do older children look like? Clumsy Unable to walk on a balance beam Problems standing with feet together and eyes closed (Romberg test) Love spinning, merry-go-rounds, water activities Weak VOR Challenges with reading – Gaze instability causes problems with acuity* Braswell & Rine 2006. www.fotosearch.com My deaf child is a late walker…does that mean she has vestibular problems? No, but it’s a red flag! Consider also: Vision problems Global developmental delay Autistic spectrum disorder Just taking her sweet time! Tests of vestibular function Eye tracking tests Positional/positioning tests – Dix-Hallpike – Supine Rotational tests – Rotary chair testing is gold standard Causes of poor vestibular function Postnatal acquired cases – Meningitis – Labyrinthitis Some forms of syndromic deafness Labyrinthine dysplasia Ototoxicity Conditions associated with CHL and poor balance Usher’s Syndrome (Type 1) Waardenburg Syndrome Pendred syndrome ESPN mutation CHARGE Syndrome Brachio-oto-renal syndrome ….and more! Usher’s Syndrome Autosomal recessive syndrome Hearing loss, vision loss, and variable vestibular dysfunction – Visual loss is due to retinitis pigmentosa Three types Usher’s syndrome Type 1 – – – – – Born profoundly deaf Vision loss typically noted by age 10 Absent vestibular function 3-6/100,000 individuals ~ 5% of deaf individuals Type 2 – Moderate to severe hearing loss – Vision loss typically begins after teen years – Normal vestibular function Type 3 – Born with normal hearing, varying rate of loss – Night blindness during puberty – Normal or near-normal vestibular function Retinitis pigmentosa <> Retinitis pigmentosa http://www.blindness.org/content.asp?id=45 Waardenburg Syndrome http://www.werathah.com/deafness/waardenburg.htm Pendred Syndrome CHARGE Syndrome Coloboma of the eye Heart defects Atresia of the choanae Retardation of growth and/or development Genital and/or urinary abnormalities Ear abnormalities and deafness www.charrgesydnrome.org Brachio-oto-renal syndrome Autosomal dominant Malformation of ear – cochlear hypoplasia – enlargement of the cochlear and vestibular aqueducts – hypoplasia of the lateral semicircular canal Hearing loss Malformations of kidney ESPN Mutation Autosomal recessive mutation Mapped to chromosome 1p36.3 Environmental causes Aminoglycoside antibiotics – Gentamicin, streptomycin, kanamycin, tobramycin, neomycin, amikacin, netilmicin, dihydrostreptomycin, and ribostamycin. Anti-neoplastics – Cisplatin, carboplatin Environmental chemicals – Butyl nitrite, mercury, carbon disulfide, styrene, carbon monoxide, tin, hexane, toluene, lead, trichloroethylene, manganese, xylene, mercury Loop diuretics – Bumetanide, ethacrynic acid, furosemide, and torsemide. Aspirin and quinine products Infections www.vestibular.org Vestibular effects of cochlear implantation Rare cause of permanent damage Common cause of transient damage – 20% in one series1 Anecdotal evidence for improvement Hearing with CI does not make a difference2 1: Vilbert et al 2001. 2. Suarez et all 2007. I think the child I am treating may have vestibular problems. Now what? Evaluation CT of temporal bone Vestibular testing (if possible) Physical, occupational, ? cognitive therapies Genetic appointment – Strongly consider testing for Usher’s mutations Vision evaluation – ?ERG Therapeutic goals Enhance existing vestibular capabilities Strengthen compensatory mechanisms http://www.tradecards.com/articles/thread/thread11.html Compensatory mechanisms Proprioceptive input – Walking barefoot or soft soled shoes Visual input Other sensory systems Therapies for children with poor vestibular systems Swinging Rocking Bouncing/jumping Dancing Skipping Running Hopping Jumping rope Rough and tumble play http://static.flickr.com/49/1 31593782_00522c7610_m.j Other interventions May wear weighted vests, leg weights, etc Consider orthopedic shoes – OR soft soled shoes Offer sensory activities May need extra time to process information www.bright-start.com Does treatment make a difference? Motor development improved post treatment1 – Therapy three times weekly for 12 weeks – Visual and somatosensory function, balance training – Significant improvement in motor development – Insignificant improvement in posturography May improve gaze stability2 – Preliminary study of two individuals 1. Rine et al 2004. 2. Braswell and Rine 2006. Treatment challenges Lack of data – Especially true for infants and toddlers Different causes of balance problems Cautions with poor vestibular function Where visual and proprioceptive information is unreliable – Eg, swimming in the dark Problems with depth perception Tunnel vision can cause problems – Worse in unfamiliar places Implications for future research Vestibular hypofunction in infancy and early childhood poorly understood Need for research on both function and treatment Implications for families Share vestibular information with parents Encourage physical activity Continue to screen older children – Balance – Retinitis pigmentosa Helpful resources What’s going on in there: How the brain and mind develop in the first five years of life. Lise Eliot, PhD. 1999 The out of sync child has fun. Carol Stock Kranowitz & TJ Wylie. 2003. Vestibular disorders organization www.vestibular.org www.boystownhospital.org Genevieve DelRosario [email protected] Department of Pediatrics University of Kansas Medical Center 3901 Rainbow Blvd Kansas City, KS 66160 (913) 588-5908 Angeli S. Value of vestibular testing in young children with sensorineural hearing loss. Arch Otolaryngol Head Neck Surg. 2003;129:478-482. Braswell J, Rine RM. Evidence that vestibular hypofunction affects reading acuity in children. Int J Pediatr Otorhinolaryngol. 2006 Nov; 70(11): 1957-1965. Braswell, J, Rine RM. Preliminary evidence of improved gaze stability following exercise in two children with vestibular hypofunction. Int J Pediatr Otorhinolaryngol. 2006 Nov;70(11):1967-73. Epub 2006 Oct 4 www.chargesyndrome.org www.dizziness-and-balance.com Eliot, L. What’s going on in there: How the brain and mind develop in the first five years of life. Bantam Books, 1999. Rine RM, Braswell J, Fisher D, Joyce K, Kalar K, Shaffer M. Improvement of motor development and postural control following intervention in children with sensorineural hearing loss and vestibular impairment. Int J Pediatr Otorhinolaryngol. 2004 Sep;68(9):1141-8. Rine RM, Cornwall G, Gan K, LoCascio C, OHare T, Robinson E, Rice M. Evidence of progressive delay of motor development in children with sensorineural hearing loss and concurrent vestibular dysfunction. Perceptual and Motor Skills. 90(3 Pt 2): 11-1-12, 2000 June. www.sense.org Siegel JC, Marchetti M, Tecklin JS. Age-related balance changes in hearing-impaired children. Phys Ther. 1991 Mar;71(3):183-9 Suarez H, Angeli S, Suarez A, Rosales B, Carrera X, Alonso R. Balance sensory ogranization in children with profound hearing loss and cochlear implants. Int J Pediatr Otorhinolaryngol. 2007 Feb 1; [Epub ahead of print] www.vestibular.org Vibert D, Hausler R, Kompis M, Visher M. Vestibular function in patients with cochlear implantation. Acta Otolaryngol Suppl. 2001; 545: 29-34.