* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download PowerPoint to accompany
Urethroplasty wikipedia , lookup
Interstitial cystitis wikipedia , lookup
Kidney transplantation wikipedia , lookup
Urinary tract infection wikipedia , lookup
Kidney stone disease wikipedia , lookup
Chronic kidney disease wikipedia , lookup
Autosomal dominant polycystic kidney disease wikipedia , lookup
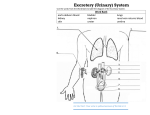
1 Chapter 26 Urinary System Functions: 1. Excretion: removal of waste products from body fluids 2. Elimination: discharge of waste products from body 2 Chapter 26 Urinary System Consists of the • Kidneys: produce urine • Ureters: pathway of urine from kidneys to bladder • Urinary bladder: muscular sac for temporary storage of urine • Urethra: urine removal pathway 3 Location of Kidneys Located on either side of the vertebral column (T12-L3) Superior surface is capped with the adrenal gland. 4 Protection of Kidneys Renal capsule: inner layer of collagen Adipose capsule: thick layer of adipose tissue Renal Fascia: outermost layer of collagen 5 Kidney Structure 6 Kidney Structure 2 layers: 1.Cortex: superficial portion, contains nephrons • Nephron: microscopic, tubular structures that beings urine production 2. Medulla: consists of 6-18 renal pyramids • Renal lobe: renal pyramid + renal cortex • where urine is produced • Renal Pelvis: large chamber which connects the renal lobes to the ureter 7 Functions of the Kidneys • Removal of metabolic wastes from the blood and excretion to the outside of the body • Regulation of blood pressure, calcium ion absorption, and the volume, composition, and pH of the blood 8 Renal Blood Vessels 9 Renal Blood Vessels 10 Renal Blood Vessels • Kidneys receive 20-25% of total cardiac output •Receives blood from the renal artery segmental arteries interlobar arteries arcuate arteries interlobular arteries afferent arterioles deliver blood to nephrons interlobular veins arcuate veins interlobar veins renal vein 11 Structure of a Nephron 12 Structure of a Nephron •Renal tubule: long pathway that starts at the renal corpuscle •Renal corpuscle: contains a glomerulus, where the capillaries are found, where filtration takes place 13 Pathway of filtration of a Nephron •Blood filters into the afferent arteriole Renal corpuscle (Glomerulus and Bowman’s capsule) Proximal convoluted tubule (where reabsorption of water, ions, organic nutrients) down Renal tubule Loop of Henle ( further reabsorption of water) up Renal tubule Distal convoluted tubule (secretion of acids, drugs, toxins) collecting duct Papillary duct (all excess waste—urine– to minor calyx major calyx ureter 14 Glomerular Capsule 15 stop 16 Juxtaglomerular Apparatus 17 Cortical and Juxtamedullary Nephrons • cortical nephrons • 80% of nephrons • located close to the surface of the kidney • juxtamedullary nephrons • regulate water balance • located near the renal medulla 18 Urine Formation • nephrons remove wastes from the blood and regulate water and electrolyte concentrations • urine is the final product of the processes of: • glomerular filtration • tubular reabsorption • tubular secretion 19 Urine Formation • Glomerular Filtration • substances move from blood to glomerular capsule • Tubular Reabsorption • substances move from renal tubules into blood of peritubular capillaries • glucose, water, urea, proteins, creatine • amino, lactic, citric, and uric acids • phosphate, sulfate, calcium, potassium, and sodium ions • Tubular Secretion • substances move from blood of peritubular capillaries into renal tubules • drugs and ions 20 Urine Composition • about 95% water • usually contains urea, uric acid, and creatinine • may contain trace amounts of amino acids and varying amounts of electrolytes • volume varies with fluid intake and environmental factors 21 Ureters •Leave the kidneys •25-30 cm long •parallel to vertebral column • in pelvic cavity, join urinary bladder 22 Urinary Bladder • hollow, muscular organ located within the pelvic cavity, posterior to the Symphysis pubis •Can hold up to a liter of urine (rugae) 23 Urinary Bladder • the internal floor of the bladder includes a triangular area called the trigone •Internal urethral sphincter: provide control over bladder 24 Urethra • tube that conveys urine from the urinary bladder to the outside of the body • Men: 18-20 cm • Connects to the prostate/ejaculatory ducts • Female: 3-5 cm •External urethral sphincter •UTI •Incontinence 25 Life-Span Changes • kidneys appear scarred and grainy • kidney cells die • by age 80, kidneys have lost a third of their mass • kidney shrinkage due to loss of glomeruli •harder for kidneys to clear certain substances • bladder, ureters, and urethra lose elasticity • bladder holds less urine 26 Formal Lab Write-up DUE • Heading • Name, title (be creative), date • Experiment • STEP BY STEP instructions on what happened • Problem • What are you testing and why? • Observations • What did you see, smell, hear? • Hypothesis • What do you think you will discover after the experiment? • Discussion • What do you know NOW? • Materials • LIST of every tool required • Conclusion • Summary of what happened, what errors occurred, why this experiment was useful 27 28 Matching a. Functional Unit of the Kidney 1. Cortex 2. Bowman’s Capsule 3. Loop of Henle 4. Renal Pelvis 5. Nephron 6. Ureter b. Transports Urine to Bladder c. U-shaped tubule d. Covers the surface of the e. f. g. 7. Hilus 8. Renal Capsule h. kidney Surrounds glomerulus Outer layer of kidney Area on kidney where blood vessels, nerves, lymphatics, and ureters enter/exit Drains major calyx 29 Matching 1. Cortex (F) 2. Bowman’s Capsule (E) 3. Loop of henle (C) 4. Renal Pelvis (H) 5. Nephron (A) a. b. c. d. e. f. g. 6. Ureter (B) 7. Hilus (G) 8. Renal Capsule (F) h. Functional Unit of the Kidney Transports Urine to Bladder U-shaped tubule Covers the surface of the kidney Surrounds glomerulus Outer layer of kidney Area on kidney where blood vessels, nerves, lymphatics, and ureters enter/exit Drains major calyx 30 Short Answer • What are some anatomical differences with the male versus female urinary structures and how do they affect the physiology? 31 Short Answer • What are some anatomical differences with the male versus female urethra and how do they affect the physiology? • Males have longer urethra = fewer UTI’s, less urgency for urination • Ejaculatory/prostate ducts connect to males urethra = urethra doesn’t just carry urine How do the following tests relate to a urinalysis? Leukocytes Nitrites Protein pH Blood Specific Gravity Ketone Bilirubin Glucose 32 Meaning 33 Leukocytes Only found in individuals who are fighting a bacterial/viral infection Nitrites Only found in individuals with significant infections Protein Found in individuals with kidney disease/damage pH If increased ketone levels, there will be a more acidic urine Blood Only present if trauma, UTI, or recent menstruation Specific Gravity Degree of concentration/dilution of urine (amount of excess water) Ketone Positive with excessive lipid breakdown Bilirubin Rare-breakdown of hemoglobin Glucose Excess-hyperglycemia