* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download TRANSFERSOMES AS A TRANSDERMAL DRUG DELIVERY SYSTEM FOR ENHANCEMENT THE
Survey
Document related concepts
Transcript
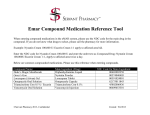
Academic Sciences International Journal of Pharmacy and Pharmaceutical Sciences ISSN- 0975-1491 Vol 5, Issue 4, 2013 Research Article TRANSFERSOMES AS A TRANSDERMAL DRUG DELIVERY SYSTEM FOR ENHANCEMENT THE ANTIFUNGAL ACTIVITY OF NYSTATIN MARWA H. ABDALLAH Department of Pharmaceutics and Industrial Pharmacy, Faculty of Pharmacy, Zagazig University, Zagazig, Egypt. Email: [email protected] Received: 04 Aug 2013, Revised and Accepted: 05 Sep 2013 ABSTRACT Objective: Transdermal drug delivery has made an important contribution to medical practice, but has yet to fully achieve its potential as an alternative to oral delivery and hypodermic injections. Various new technologies have been developed for the transdermal delivery of some important drugs. Physical and chemical means of crossing the lipophilic stratum corneum, the outermost layer of the skin, are being explored. The goal of the present study was to formulate and evaluate the potential use of transfersomal vesicles as a transdermal drug delivery system for poorly soluble drug, Nystatin. Methods: It was investigated by encapsulating the drug in various transfersomal formulations composed of various ratios of Phospholipone H 100, Span 80, Tween 80 and sodium deoxycholate prepared by lipid film hydration by rotary evaporation sonication method. The prepared formulations were characterized for light microscopy, and evaluated for particle shape, entrapment efficiency (EE%), stability, and in vitro skin permeation. Results: The vesicles were spherical in structure as confirmed by Transmission Electron Microscopy. The EE% of nystatin in the vesicles was in the range of 50-70%. The result revealed that Nystatin in all of the formulations was successfully entrapped with uniform drug content. In vitro skin permeation studies were carried by abdominal rabbit skin using a dissolution-dialysis apparatus fabricated in our laboratory. The amount of drug deposited in the skin and the amount permeated were higher in case of transfersomes with an enhancement ratio of 2.59, when compared to liposomes and the commercial product. Conclusion: It is evident from this study that transfersomes are a promising prolonged delivery system for Nystatin and have reasonably good stability characteristics. This research suggests that nystatin loaded transfersomes can be potentially used as a transdermal drug delivery system. Keywords: Nystatin, Transfersomes, Transdermal drug delivery, Phospholipone H 100, Antifungal. INTRODUCTION Transdermal drug delivery systems (TDDS) offer a number of potential advantages over conventional methods such as injectable and oral delivery [1]. However, the major limitation of TDDS is the permeability of the skin, it is permeable to small molecules, lipophilic drugs and highly impermeable to macromolecules and hydrophilic drugs. The main barrier and rate-limiting step for diffusion of drugs across the skin is provided by the outermost layer of the skin, the stratum corneum (SC) [2]. Recent approaches in modulating vesicle compositions have been investigated to develop systems that are capable of carrying drugs and macromolecules to deeper tissues. These approaches have resulted in the design of two novel vesicular carriers, ethosomes and ultraflexible lipid-based elastic vesicles, transfersomes [3]. Transfersomes are ultradeformable vesicles possessing an aqueous core surrounded by the complex lipid bilayer. Interdependency of local composition and shape of the bilayer makes the vesicle both self-regulating and selfoptimizing [4]. Transfersomes have recently been introduced, which are capable of transdermal delivery of low as well as high molecular weight drugs [5]. Transfersomes are specially optimized, ultraflexible lipid supramolecular aggregates, which are able to penetrate the mammalian skin intact and then act as a drug carrier for non-invasive targeted drug delivery and sustained release of therapeutic agents [6]. Each transfersome consists of at least one inner aqueous compartment, which is surrounded by a lipid bilayer with specially tailored properties, due to the incorporation of "edge activators" into the vesicular membrane. Surfactants such as sodium cholate, sodium deoxycholate, Span 80, and Tween 80, have been used as edge activators [7]. Due to their deformability, transfersomes are good candidates for the non-invasive delivery of small, medium, and large sized drugs. Materials commonly used for the preparation of transfersomes are phospholipids (soya phosphatidyl choline, egg phosphatidyl choline), surfactants (Tween 80, sodium cholate) for providing flexibility, alcohol (ethanol, methanol) as a solvent, dye (Rhodamine-123, Nile-red) for confocal scanning laser microscopy (CSLM) and buffering agent (saline phosphate buffer pH 7.4), as a hydrating medium. Transfersomes can deform and pass through narrow constriction (from 5 to 10 times less than their own diameter) without measurable loss. Nystatin (NYS) is a polyene antifungal characterized by a potent broad-spectrum antifungal action including a wide range of pathogenic and non-pathogenic yeasts and fungi. The Nystatin is active against a variety of fungal pathogens including: Candida, Aspergillus, Histoplasma, and Coccidioides and has been used for years to treat Candida at the skin and those for the mouth [8]. The aim of this study is to formulate ultraflexible lipid vesicles for enhanced skin delivery of Nystatin. The system was developed and evaluated for its physicochemical characteristics, such as particle size, entrapment efficiency, stability, and In vitro skin permeation. The compositions of lipid in the transfersomes (cholesterol and surfactants) were evaluated. MATERIALS AND METHODS Materials Nystatin (NYS) was kindly supplied by Delta pharma (Egypt). Phospholipone H 100 (PL), sodium deoxycholate (SDC), Span 80 (SP80) and sodium azide were purchased from Sigma Chemical Co. (St. Louis, USA). Tween 80 (TW80), Chloroform and methanol were purchased from El-Nasr Pharmaceutical Chemical Co., Cairo, Egypt. Methods Preparation of Nystatin loaded transfersomes Transfersomes were prepared by rotary evaporation-sonication method described by (Jain et al.; El-zaafarany et al.) [3,9]. The lipid mixture (500mg) consisted of Phospholipone H 100, edge activator (surfactant) and drug (10 mg/ml) in different ratios was dissolved in an organic solvent mixture consisted of chloroform and methanol (2:1, v/v) then placed in a clean, dry round bottom flask. The organic solvent was carefully evaporated by rotary evaporation (Buchi rotavapor R-3000, Switzerland) under reduced pressure above the lipid transition temperature to form a lipid film on the wall of the flask. The final traces of the solvents were removed by Abdallah et al. Int J Pharm Pharm Sci, Vol 5, Issue 4, 560-567 subjecting the flask to vacuum over night. The dried thin lipid film deposited on the wall of the flask was hydrated with a phosphate buffer solution (pH 6.4) by rotation for 1hr at room temperature at 60 rpm. The resulting vesicles were sonicated for 30 min in a bath sonicator (Model Julabo Labortechnik GMBH- Germany) to reduce the size of the vesicles then stored at 4 oC. Different edge activators in different molar ratios were used for the formulation of transfersomes, the composition of these formulations is shown in Table 1. The liposomes (Phospholipon H 100: cholesterol, 7:3) that act as a control in the present study were prepared by the same method as described above. Characterization of Transfersomes Entrapment Efficiency (EE%) The EE % of transfersomes was determined after separation of the non-entrapped drug. Entrapment efficiency of NYS in transfersomal formulations can be done by Freeze thawing/centrifugation method [10]. 1 ml samples of transfersomal dispersion were frozen for 24 hrs at −20 °C in eppendorff tubes. The frozen samples were removed from the freezer and let to thaw at room temperature, then centrifuged at 14,000 rpm for 50 min at 4 °C. Tranfersomal pellets were re-suspended in PBS (pH 6.4) and then centrifuged again. This washing procedure was repeated two times to ensure that the unentrapped drug was no longer present. The supernatant was separated each time from transfersomal pellets and prepared for the assay of free drug. The drug content was determined spectrophotometrically at 306 nm using PBS (pH 6.4) as a blank [11]. Each result was the mean of three determinations (±SD). The entrapment efficiency was defined as the percentage ratio of the entrapped drug concentration to the total drug concentration and calculated according to the following equation: EE% = Total drug concentration – Free drug concentration X 100 Total drug concentration Differential scanning calorimetry measurements (DSC) The DSC thermograms were recorded on a Schimadzu- DSC 50 differential scanning calorimetry. DSC was carried out for NYS powder as well as for the plain transfersomes and NYS loadedtransfersomes in the ratio of 90:10% (w/w) (PL: EA). The analysis was performed on 40 µl or 1-mg samples sealed in standard aluminium pans. Thermograms were obtained at a temperature range from 0-300 oC and a scanning rate of 10 ◦ C/min under nitrogen atmospher. Phosphate buffer (pH 7.4) was employed as reference [12,13]. In vitro drug release from transfersomes The in-vitro release of NYS bearing transfersomes through an artificial cellophane membrane was determined by a simple dialysis method [14]. The receptor medium was 100 ml PBS (pH 6.4) which was maintained at 37±0.2 ◦ C and constantly stirred at 100 rpm in a thermostatically controlled water bath shaker. An amount of transfersomes pellets equivalent to 2.5 mg drug was placed in the donor compartment. Samples of 4 ml were withdrawn from the receptor compartment at 0.5, 1, 2, 4, 6, 8 and 24 hrs intervals, and immediately replaced with an equal volume of fresh receptor solution. Triplicate experiments were conducted for each study and sink conditions were always maintained through out the experiment. All samples were analyzed for NYS content spectrophotometrically at a wavelength of 306 nm against PBS (pH 6.4) as a blank [15]. Transmission electron microscopy (TEM) The surface appearance and shape of NYS-loaded transfersomes were analyzed by taking TEM photographs using transmission electron microscope (100 CX, Jeol, Tokyo, Japan). The transfersomes were dispersed in water and one drop of the diluted dispersion was placed on a carbon coated grid. The dispersion was left for 2 min, to allow its absorption in the carbon film, and the excess liquid was drawn off with filter paper. Subsequently, a drop of 2% ammonium molybdate was placed on the grid. The excess was removed with distilled water and the samples were examined by TEM [16,17]. In vitro skin permeation studies Preparation of a rabbit skin Abdominal full-thickness skin was obtained from white male rabbits (2-3 kg) obtained from Faculty of Veterinary Medicine, Zagazig University, Egypt. The skin was carefully removed from animals after sacrificing them. The hair was removed from the abdominal skin with the aid of an electric animal clipper and shaver. Care was taken not to damage the skin surface. The fat was removed with the aid of scissor and skin was washed and the excised full thickness rabbit skin samples were stored at 20oC prior to use. The excised full thickness abdominal rabbit skin samples were equilibrated by soaking in buffer solution of pH 6.4 containing 0.02% sodium azide as preservative at 4±1oC for about one hour before beginning of each experiment. In Vitro permeation studies The transfersomal formulation which exhibits the highest EE% was chosen for in vitro permeation studies of NYS through abdominal rabbit skin in comparison to liposomes, plain drug and commercial product (Nystatin ® cream, PHARAONIA).. The in-vitro permeation of NYS from different formulations was determined by using a dissolution-dialysis apparatus, the cell of which is fabricated in our laboratory. The dissolution cell consisted of a hollow glass tube of length [18]. The shaved abdominal rabbit skin was mounted on the receptor compartment with the stratum corneum side facing upwards towards the donor compartment and the dermal side facing downward to the receptor compartment with permeation area of 6.61 cm2. The receptor compartment was then filled with 100 ml of PBS (pH 6.4) containing 0.02% sodium azide as preservative. The temperature of media was maintained at 37±0.5oC. Amounts equivalent to 2.5mg drug of the tested transfersomal formulation were applied to the skin surface. The glass cylinder was attached to the dissolution apparatus by using parafilm and stirred at 100 rpm. 4 ml samples of the solution in the receptor compartment were removed for drug content determination at different time intervals up to 24 hrs and replaced immediately with an equal volume of fresh receptor fluid every time [19]. Samples were analyzed spectrophotometrically at 306 nm using samples collected from permeation of drug free systems as a blank. Triplicate experiments were conducted for each study and the average was taken. The cumulative amount of drug permeated through abdominal rabbit skin per unit area (µg/cm2) was plotted against time (hrs) [11].The permeation parameters of NYS as steadystate transdermal fluxes (JSS), permeability coefficient (Kp) through the abdominal rabbit skin and enhancement ratio (ER) were calculated from the penetration data. The steady-state transdermal fluxes (JSS) of NYS through the abdominal rabbit skin were calculated from the slope of linear portion of the cumulative amount of drug permeated through unit area of the abdominal rabbit skin (ug/cm2) versus time plot. The permeability coefficient (kp) through the abdominal rabbit skin was calculated according to the following equations [3]: Kp = JSS /Cd ER= Kp of test formulation / kp of plain drug Where Cd = the initial drug concentration in the donor compartment (2.5 mg). Skin retention study The ability of transfersomes to help retain the encapsulated drug within the skin (depot-effect) in comparison to liposomes, plain drug and commercial product was investigated by determining the amount of drug retained in the skin samples at the end of permeation studies. After performing the above mentioned in-vitro permeation study for 24 hours, skin mounted on the diffusion cell was removed. The remaining formulation adhering to the skin was scraped with a spatula [20]. The skin was cleaned with cotton piece dipped in saline solution and then gently dried by pressing between two tissue papers to remove any adhering formulation [21]. Subsequently, the cleaned skin sample was mechanically shaked with 100 ml of PBS (pH 6.4) in water shaker bath at 37±0.5oC for 1 hr for complete extraction of the drug. The filtrate was removed and the drug content in the filtrate was determined spectrophotometrically at 306 nm using UV spectrophotometer. 561 Abdallah et al. Int J Pharm Pharm Sci, Vol 5, Issue 4, 560-567 Statistical analysis Data were expressed as mean ± SD. The results were statistically analyzed by analysis of variance ANOVA test; P values less than 0.05 (P<0.05) were considered as significant. Microbiological assay of Nystatin Antifungal activity of different formulations was carried out by cup plate test. The cup plate method depends upon diffusion of antifungal from a vertical cylinder through a solidified agar layer in a petri dish or plate to an extent such that growth of added microorganism is prevented entirely in a zone around the cylinder containing antifungal agent [22]. The agar medium was prepared by dissolving 65 gm of sabouraud dextrose agar powder per liter of distilled water and was sterilized using autoclave at 121oC for 20 min. The plates were first sterilized in hot air oven at 160°C for 60 min. Candida albicans suspension (100 μl) was introduced into each plate and 40 ml of sterile sabouraud dextrose agar was poured into each plate. The plates were agitated carefully to allow for both an even distribution of the agar in the plates and a homogenous mixing of the agar with the test organism. The plates were allowed to harden. In each plate, four cups, each 6 mm in diameter were bored in the medium with cork borer. In each plate, 100ul of each formulation was placed in one of the cups and the plates incubated at 25°C for 24 hrs [23]. The entire operation was carried out under aseptic conditions and the mean inhibition zone was calculated. The antifungal efficacy of NYS-loaded transfersomes prepared from PL: SP80 (90:10) compared to liposomes and the commercial product was determined by performing agar-cup diffusion assay. The zones of growth inhibition were measured for all the tested samples. Each type of the samples was tested in triplicate. The inhibition zone of growth of Candida albicans was measured in mm after 24 hrs and the mean inhibition zone was then calculated. RESULT AND DISCUSSION The conventional rotary evaporation sonication method was used to prepare the transfersomal formulations. Formulations were prepared by using different types and concentration of EA. Nystatin entrapment efficiency in transfersomes 1. Effect of phospholipid: edge activator ratio The EE% increased significantly (P<0.05) with increasing EA concentration from 2.5 to 10% (w/w) for transfersomes prepared using SP80, SDC, and TW80, Further increase in EA concentration to 15 then 25% (w/w) showed a significant decrease in EE% (P<0.05), Table 1. The ratio 90:10% (w/w) showed optimum EE%, Table 1. Upon incorporation of EA in low concentration, growth in vesicle size occurred [24], whereas, further increase in the content of edge activator may have led to pore formation in the bilayers. When EA concentration exceeded 15%, mixed micelles coexisted with the transfersomes, with the consequence of lower drug entrapment due to the rigidity and smaller size of mixed micelles [3,9]. Patel et al. reported that, the effect of phospholipids and EA ratio in the lipid components of vesicles on the entrapment efficiency of lipophilic drug, curcumin, the efficiency decreased with increasing surfactant concentration [25]. 2. Effect of types of edge activator Table 1 demonstrates the effect of EA types on the EE% of different transfersomal formulations. The transfersomal formulation (SP804) showed the highest EE% (80.71%±1.11) followed by TW80-4 (74.24% ±0.71 and finally SDC-4 (69.78%±1.54). These results are related to the HLB values of these edge activators. They are 4.3, 15, and 16 for Span 80, Tween 80 and sodium deoxycholate, respectively. Based on these HLB values, the affinity for lipids was expected to be in the order of SP80 > TW80 > SDC. This consideration explains the higher EE% encountered with SP80 and compared to TW80, and SDC. The entrapment efficiency of the SP80 formulation was high because of the increase in the ratio of lipid volume in the vesicles as compared to the encapsulated aqueous volume [25]. 3. Effect of vesicle composition Table 1 illustrates the percentages of drug entrapment in different transfersomal formulations in comparison to liposomes. The EE of transfersomes formulations were significantly higher than the liposome formulation (P<0.05). This result might be attributed to interactions between the surfactants and NYS forming a complex and this complex was inserted into the transfersomes bilayers [26]. Fang et al. reported that adding surfactant, sodium stearate to phosphatidylethanolamine vesicles significantly significantly increased the entrapment efficiency of 5-aminolevulinic acid in comparison to liposomes [27]. Higher entrapment efficiency in case of transfersomes has also been reported by Gupta et al. who found that transfersomes revealed significant higher entrapment efficiency in comparison to liposomes and niosomes [28]. Table 1: Composition and entrapment efficiency % of different Nystatin Transfersomal formulations Formulation Composition Drug conc. (mg/ml) Entrapment efficiency %± SD PL:EA (% w/w) SP80-1 97.5:2.5 10 61.98±0.62 SP80-2 95:5 10 66.01±0.68 SP80-3 92.5:7.5 10 70.67±1.56 SP80-4 90:10 10 80.71±1.11 SP80-5 85:15 10 68.16±1.13 SP80-6 80:20 10 62.56±1.49 TW80-1 97.5:2.5 10 60.63±1.26 TW80-2 95:5 10 63.13±1.49 TW80-3 92.5:7.5 10 68.14±1.35 TW80-4 90:10 10 74.24±0.71 TW80-5 85:15 10 65.97±0.63 TW80-6 80:20 10 61.44±1.19 SDC-1 97.5:2.5 10 57.22±0.82 SDC-2 95:5 10 59.62±1.13 SDC-3 92.5:7.5 10 63.80±1.04 SDC-4 90:10 10 69.78±1.54 SDC-5 85:15 10 62.53±1.53 SDC-6 80:20 10 58.52±2.08 Liposomes PL:Chol (7:3) 10 51.85±1.82 SP80-4a 90:10 2.5 50.54±1.84 SP80-4b 90:10 5 71.91±0.52 SP80-4c 90:10 7.5 78.73±0.38 SP80-4d 90:10 15 60.37±0.89 SP80-4e 90:10 20 57.19±2.78 PL: phospholipon H100, EA: edge activator, SDC: sodium deoxycholate, TW80: Tween 80, SP80: Span 80, Chol: cholesterol. Final lipid concentration in all formulations = 5% (w/w). Average of three determinations±standard deviation (SD). 562 Abdallah et al. Int J Pharm Pharm Sci, Vol 5, Issue 4, 560-567 4. Effect of total lipid concentration 5. Effect of drug concentration The effect of total lipid concentration on the EE (expressed as % or ug/g lipids) of NYS transfersomes consisting of PL: Sp80 in 90:10 molar ratio was shown in Fig.1. The EE% of NYS increased significantly (P<0.05) from 56.98±0.79 to 80.71%±1.11 as the total lipid concentration was increased from 100 mg to 500 mg. However, the EE expressed as % µg/g lipids decreased significantly from 56.98±0.79 to 16.39±0.22 % µg/g lipids as the total lipid concentration increased. This means that the amount of lipid taking part in the encapsulation decreased as the lipid concentration increased [29]. Similar observations were obtained by Elzaafarany et al. who reported an optimum lipid concentration for the encapsulation of diclofenac sodium into transfersomes [3]. The entrapment efficiency (%) increased significantly (P<0.05) from 50.53%±1.84 to 80.71%±1.11 as the drug concentration was increased from 2.5 mg/ml to 10mg/ml, respectively, in the transfersomal vesicles (SP80-4), Table 1. However further increase in the drug concentration to 15 mg/ml lead to a significant (P=0.002) decrease in the EE % to 57.19%±2.78. The increased EE% of NYS within the transfersomal vesicles with increasing the drug concentration during the formulation could be due to the saturation of the media with drug that forces the drug to be encapsulated into transfersomal vesicles [30]. When the lipid bilayers became saturated with the drug, any further increase in drug concentration will lead to precipitation [3]. 100 EE% 90 EE % ug/g lipid Entrapment efficiency 80 70 60 50 40 30 20 10 0 100 200 300 400 500 Total lipid concentration (g) Fig. 1: Effect of total lipid concentration on the EE of NYS in transfersomes (SP80-4). 100 SP80-1 SP80-2 SP80-3 SP80-4 SP80-5 SP80-6 90 80 % Drug Released 70 60 50 40 30 20 10 0 0 5 10 15 20 25 30 Time (hrs) Hr Fig. 2: Effect of edge activator concentration on the in-vitro release of NYS transfersomal vesicles. In-vitro drug release studies In vitro studies for the release of NYS from transfersomes prepared from SP80 as edge activators with different PL: EA molar ratios were studied. The release profiles of NYS from different transfersomal formulations were apparently biphasic release processes, where a rapid release was observed during the initial phase (first 2 hrs) results from the release of the surface-adsorbed drug, followed by a sustained release profile for up to 24 hrs (Fig. 2). The release from transfersomal formulations after 24 hrs, first increased with increasing SP80 concentration (from 2.5 to 10%, w/w) in the transfersomal formulations and then decreased by further increasing in the concentration of EA. A possible explanation for lower drug release at low edge activator concentrations may be that the lipid membranes were more ordered and less leaky, which impeded drug release [3]. The maximum release was observed in the formulation containing EA concentration of 10%, because at this concentration the surfactant molecule gets associated with the 563 Abdallah et al. Int J Pharm Pharm Sci, Vol 5, Issue 4, 560-567 phospholipid bilayer resulting in better partitioning of the drug, and resulted in higher drug release from the vesicles [31]. At high edge activator concentrations, the release of the drug was low due to the loss of vesicular structure and formation of rigid mixed micelles [3]. The formulations prepared using the ratio of EA for optimum drug release (90:10%, w/w) was selected to show the effect of type of edge activator on the release profiles of the drug (Fig. 3). The % amount of drug released after 24 hrs were 70.56%±0.43, 64.72%±2.16 and 59.29%±2.67 for SP80-4, SDC-4 and TW80-4 transfersomes, respectively. The significant increase in the drug release in case of SP80 as edge activator could be attributed to the lipophilic nature of Nystatin. The results are in agreement with Jain et al. who reported that the release of dexamethasone from transfersomes was in the order: SP80> SDC> TW80 [9]. Examination of transfersomes by transmission electron microscopy The electron micrographs of SP80-4 are shown in Fig.4. They show the outline and core of the well-identified spherical vesicles confirming the vesicular characteristics, displaying the retention of sealed vesicular structure. The vesicles are smaller unilamellar vesicles with a more homogenous size distribution. 100 SP80-4 90 SDC-4 % Amount of Drug Released 80 TW80-4 70 60 50 40 30 20 10 0 0 5 10 Time (Hr) 15 20 25 30 Fig. 3: Effect of type of edge activator on the in-vitro release of NYS transfersomal vesicles. Fig. 4: Transmission electron micrographs of transfersomes (SP80-4). Differential Scanning Calorimetry (DSC) DSC thermograms of Nystatin, plain (drug-free) transfersomes of the molar ratio PL:SP 80 (90:10) molar ratio as well as Nystatin-loaded transfersomes of the same molar ratio, are illustrated in Fig. 5. DSC thermogram of Nystatin powder showed endotherm at 160 oC. The DSC thermogram of plain transfersomes (drug free) showed disappearance of the melting endotherm of Nystatin and appearance of 2 distinct endotherms at 88.73 oC and 53.47 oC. DSC thermogram of Nystatin-loaded transfersomes composed PL: SP80 (90:10) molar ratio also showed disappearance of the melting endotherm of Nystatin, the intensity of the endotherms markedly increased, and the major endotherms shifted from 88.73 oC to 80.36 oC and from 53.47 oC to 48.48 oC indicating good interaction of all components. These results indicated that, the entrapped Nystatin associated with lipid bilayers interacted to a large extent with them. Absence of the melting endotherm of Nystatin and shifting of the lipid bilayer components endotherm suggested significant interaction of Nystatin with bilayers [13, 32]. The interaction of Nystatin with bilayers leading to enhanced entrapment of the drug. 564 Abdallah et al. Int J Pharm Pharm Sci, Vol 5, Issue 4, 560-567 Fig. 5: DSC thermogram of Nystatin (A), plain (drug-free) transfersomes (B) and Nystatin loaded Sp80 transfersomes (C). In vitro skin permeation study Fig. 6 illustrates the permeation profiles of NYS (plain drug), commercial product, NYS-loaded transfersomes (SP80-4, Tw80-4, SDS-4) and liposomes over 24 hrs. The cumulative amount of NYS permeated through the abdominal rabbit skin in all vesicle formulations was significantly (P<0.05) higher than the plain drug. The amount of NYS permeated through skin from transfersomal formulations was significantly (P<0.05) higher than that permeated from liposomal formulation. Transfersomes have shown to be successful in the delivery of drugs into the skin, because they are composed of phospholipid and surfactants. Also, they can squeeze through the pores in the stratum corneum (SC) of the skin [26]. They can also adsorb onto or fuse with the stratum corneum, and the intact vesicle can penetrate into and through the intact skin. Moreover, surfactants are enhancers that solubilize the lipophilic compound; they also have the potential to solubilize the lipid within the SC. Surfactants swell the SC, interact with the intercellular keratin, and fluidize the SC lipids to create channels that allow increased drug delivery [26]. The amount of NYS permeated from different transfersomal formulations with different types of EA are found in the following order: SP80> SDC> TW80. The higher the skin permeation of NYS from SP80-4 may be related to the lipophilic nature of the drug. Table (2) demonstrates the steady-state transdermal fluxes (JSS) and permeability coefficient (Kp) values of NYS permeated through the abdominal rabbit skin from different formulations. The steady state flux values were significantly higher (P=0.003) incase of different transfersomal formulations compared to liposomes, plain drug and commercial product. The increased in (JSS) suggesting that, the permeation of NYS increased with the addition of edge activators. Drug skin retention after 24 hrs of diffusion studies of different formulations was compared and the results are recorded in (Table 2). The maximum percents drug retained were noticed with the transfersomal formulations compared with liposomes, plain drug and commercial product. The higher drug skin retention in case of transfersomes may be due to the creation of reservoir effect for drug in the skin due to deposition of other components of transfersomes with drug into the skin and there by increasing the drug retention capacity into the skin [21]. This gave an understanding that transfersomes could not only prolong the penetration of drug molecules but also helped to localize the drug in the skin. According to the amount of drug permeated and deposited in skin, steady state flux (Jss) and permeability coefficient (Kp), SP80-4 was found superior to liposmes, plain drug and commercial product. Cumulative amount of durg permeated (ug/cm 2) 250 SP80-4 SDC-4 TW80-4 Liposomes Commercial Product Plain Drug 200 150 100 50 0 0 5 10 15 20 25 30 Time (Hr) Fig. 6: % cumulative Nystatin permeated through skin from different transfersomal formulations in comparison to commercial product. 565 Abdallah et al. Int J Pharm Pharm Sci, Vol 5, Issue 4, 560-567 Table 2: Permeation parameters of Nystatin from different formulations across abdominal rabbit skin Formulation SP40-4 SDC-4 Tw80-4 Liposomes Plain drug Commercial product Jss (µg/cm2. hr) 6.23±1.02 5.88±0.86 5.60±0.73 4.13±0.73 2.40±0.53 2.59±0.59 Kp (cm/hr *10-2) 0.249±1.42 0.235±1.56 0.224±1.59 0.164±0.89 0.096±0.92 0.100±1.34 In vitro Antifungal Activity The optimized transfersomal formulation (SP80-4) was further evaluated for antifungal activity against Candida albicans by cup plate method. The results of zone of inhibition of NYS transfersomal vesicles were compared to the commercial product and liposomal formulation. The zones of inhibition of various formulations are represented graphically (Fig. 7). These results demonstrated that, the antifungal activity of the transfersomes was significantly higher than the liposomes and the commercial product (p<0.05). These transfersomes acts as carriers for drug delivery to the particular site of action, the antifungal activity is created by the drug incorporated into the transfersomal vesicles. This enhanced antifungal activity is due to enhanced ER Percent Drug Deposition 2.59 2.44 2.33 1.72 -----1.06 56.141.32 52.942.00 49.612.00 40.271.98 25.750.23 31.331.62 penetration of transfersomes containing drug through the fungal cell wall and inhibiting the ergo sterol synthesis [33]. It was noted that, there was a non significant increase (P=0.061) in the antifungal activity of NYS loaded transfersomes and liposomes after 24 hrs and 48 hrs while, there was a significant decrease (P=0.021) in the inhibitory zones at 24 hrs and 48 hrs for the commercial product, (Fig.7). This can be explained by the fact that, Candida albicans will be in log phase during 24 hrs and reaches stationary phase at 48 hrs. The longer duration of antifungal activity of transfersomes formulations may be attributed to the slow and prolonged release of the entrapped drug from transfersomal vesicles compared to commercial product. Furthermore, transfersomes act as a reservoir system, similar to a slow release vehicle, enabling more uniform and sustained release of the drug. Fig. 7: Photograph showing the inhibition zones of different formulations of Nystatin after 24hr (A) and 48 hr (B), 1: Plain transfersomes (free drug), 2: Nystatin loaded transfersomes (SP80-4), 3: Liposomes, 4: Commercial product. CONCLUSION Finally, it may be concluded from the study that transfersomes, can increase the transdermal flux, prolong the release, and improve the site specificity of bioactive molecules. Transfersomes may be used as alternative carriers for transdermal drug delivery systems because they interact with solid gel phase SC lipids and thus leading to disruption and fluidization of the SC lipid. Nystatin was successfully incorporated into transfersomes. From this study, it can concluded that transfersomes loaded with Nystatin showed a prolonged action than liposomes and commercial product and it can be developed successfully to improve the antifungal activity. REFERENCES 1. 2. Irfan M, Verma S, Ram A. Preparation and characterization of ibuprofen loaded transferosome as a novel carrier for transdermal drug delivery system. Asian j pharm clin resear. 2012;5(3):162-5. Trommer H, Neubert RHH: Overcoming the stratum corneum. The modulation of skin penetration. A review, Skin Pharmacology and Physiology. 2006;19(2):106-21. 3. 4. 5. 6. 7. 8. El Zaafarany GM, Awad GAS, Holayel SM, Mortada ND. Role of edge activators and surface charge in developing ultradeformable vesicles with enhanced skin delivery. Int J Pharm. 2010;397:164-72. Cevc G, Grbauer D, Schatzlein A, Blume G. Ultraflexible vesicles, transfersomes, have an exteremly low pore penetration resistance ant transport therapeutic amounts of insulin across the intact mammalian skin. Biochem Biophys Acta. 1998;1368(2):201-15. El-Maghraby GM, Williams AC. Vesicular systems for delivering conventional small organic molecules and larger macromolecules to and through human skin. Expert Opin Drug Deliv. 2009;6(2):149-63. Walve JR, Bakliwal SR, Rane BR, Pawar SP. Transfersomes: A syrrogated carrier for transdermal drug delivery system. Int J App Bio Pharm Tech. 2011; 2(1):204-13. Cevc G, Blume G. Lipid vesicles penetrate into intact skin owing to transdermal osmotic gradient and hydration force. Biochem Biophys Acta 1992; 1104: 226-32. Elosaily GH. Formulation and In-vitro Evaluation of Nystatin Nanoemulsion-Based Gel for Topical Delivery. J Am Sci. 2012; 8(12): 541-8. 566 Abdallah et al. Int J Pharm Pharm Sci, Vol 5, Issue 4, 560-567 9. 10. 11. 12. 13. 14. 15. 16. 17. 18. 19. 20. 21. Jain S, Jain P, Umamaheshwari RB, Jain NK. Transfersomes–a novel vesicular carrier for enhanced transdermal delivery: development, characterization, and performance evaluation. Drug Dev Ind Pharm. 2003;29:1013-26. Mokhtar M, Sammour OA, Hammad MA, Megrab NA. Effect of some formulation parameters on flurbiprofen encapsulation and release rates of niosomes prepared from proniosomes. Int J Pharm. 2008; 361: 104-11. Marzouk MA, Ammar AA, Darwish MK, El-sayed HA. Effect of penetration enhancers on in vitro permeation of Nystatin from topical formulations. Int J Drug Disc. 2012;4(2):153-9. Chanda H, Das P, Chakraborty R, Ghosh A. Development and Evaluation of Liposomes of Fluconazole. J Pharm Biomed Sci. 2011; 5(27):1-9. El-Ridy MS, Badawi AA, Safar MM, Mohsen AM. Niosomes as a novel pharmaceutical formulation encapsulating the hepatoprotective drug silymarin. Int J Pharm Pharm Sci. 2012;4(1):549-59. Mujoriya RZ, Bodla RB. Design and Development of Niosomal Delivery System for Ketoprofen. Adv Life Sci Tech. 2012;3:1-12. Desaia S, Dokeb A, Disouzaa J, Athawalec R. Development and evaluation of antifungal topical niosomal gel formulation. Int J Pharm Pharm Sci. 2011;3(5):224-31. Song YK, Hyun SY, Kim HZT, Kim CK, Oh JM. Transdermal delivery of low molecular weight heparin loaded in flexible liposomes with bioavailability enhancement: comparison with ethosomes. J Microencap. 2011; 28(3):151-8. Marwa HA, Omaima AS, Hanaa AE, Mohammed EA. Design and development of piroxicam-entrapped niosomes as an oral drug delivery system. Int J Adva Pharm Res. 2013; 4(6):1873 – 86. Ibrahim MM, Sammour OA, Hammad MA, Megrab NA. In-vitro evaluation of proniosomes as a drug carrier for flurbiprofen. AAPS PharmSciTech. 2008;9(3):782-90. Singh S, Gajra B, Rawat M, Muthu MS. Enhaced transdermal delivery of ketoprofen from bioadhesive gels. Pak J Pharm Sci. 2009;22 (2):193-8. Agarwal R, Katare OP. Preparation and In Vitro Evaluation of Miconazole Nitrate–Loaded Topical Liposomes. Pharm Tech. 2002;11:48-60. Maurya SD, Aggarwal S, Tilak VK, Dhakar RC, Singh A, Maurya G. Enhanced transdermal delivery of indinavir sulfate via transfersomes. Int J Comp Pharm. 2010; 1(01):1-7. 22. Sabale V, Vora S. Formulation and evaluation of microemulsion-based hydrogel for topical delivery. Int J Pharm Investig. 2012;2(3):140-9. 23. Hashem FH, Shaker DS, Ghorab MK, Nasr M, Ismail A. Formulation, Characterization, and Clinical Evaluation of Microemulsion Containing Clotrimazole for Topical Delivery. AAPS PharmSciTech. 2011; 12(3):879-86. 24. Van den Bergh BAI,Wertz PW, Junginger HE, Bouwstra JA. Elasticity of vesicles assessed by electron spin resonance, electronmicroscopy and extrusion measurements. Int J Pharm. 2001;217: 13-24. 25. Patel R, Singh SK, Singh S, Sheth NR, Gendle R. Development and characterization of curcumin loaded transfersome for transdermal delivery. J Pharm Sci Res. 2009; 1(4):71-80. 26. Duangjit S, Opanasopit P, Rojanarata T, Ngawhirunpat, T. Characterization and InVitro Skin Permeation of MeloxicamLoaded Liposomes versus Transfersomes. J Drug Deliv. 2011; 2(11):1-9. 27. Fang YP, Tsai YH, Wu PC, Huang YB. Comparison of 5aminolevulinic acid-encapsulated liposome versus ethosome for skin delivery for photodynamic therapy. Int J Pharm. 2008; 356(1-2):144-52. 28. Gupta PN, Mishra V, Rawat A, Dubey P, Mahor S, Jain S, Chatterji DP, Vyas SP. Non-invasive vaccine delivery in transfersomes, niosomes and liposomes: a comparative study. Int J Pharm.2005; 293: 73-82. 29. Abu-Zaid SS, El-ghamry HA, Hammad M, Mokhtar M. Effect of some formulation parameters on encapsulation, release profile and biological activity of liposomes containing certain drugs. M J P S. 2003; 19(2):76-89. 30. Balakrishnana P, Shanmugama S, Lee WS, Lee WM, Kima JO, Oha DH, Kim D, Kim JS, Yoo BK, Choi, H, Woo JS, Yong CS. Formulation and in vitro assessment of minoxidil niosomes for enhanced skin delivery. Int J Pharm. 2009; 377:1-8. 31. Gupta A, Aggarwal G, Singla S, Arora R. Transfersomes: A novel vesicular carrier for enhanced transdermal delivery of sertraline: development, characterization, and performance evaluation. Sci Pharm. 2012; 80:1061-80. 32. Hathout RM, Mansour S, Mortada ND, Guinedi AS. Liposomes as an Ocular Delivery System for Acetazolamide: In Vitro and In Vivo Studies. AAPS PharmSciTech. 2007;8(1):5-12. 33. Thomas L, Viswanad V. Formulation and Optimization of Clotrimazole-Loaded Proniosomal Gel Using 32 Factorial Design. Sci Pharm. 2012; 80: 731-48. 567