* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download NSAIDs - My UAG!
Pharmacognosy wikipedia , lookup
Pharmacogenomics wikipedia , lookup
Discovery and development of ACE inhibitors wikipedia , lookup
Discovery and development of proton pump inhibitors wikipedia , lookup
Drug interaction wikipedia , lookup
Dextropropoxyphene wikipedia , lookup
Toxicodynamics wikipedia , lookup
Psychopharmacology wikipedia , lookup
Dydrogesterone wikipedia , lookup
Discovery and development of cyclooxygenase 2 inhibitors wikipedia , lookup
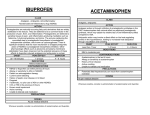
Dr. Eduardo D. Rosas Blum Department of Pharmacology A 5-year-old girl is brought to the emergency department by her parents in a comatose state. Her parents refers that she felt ill recently with high fever. Physical examination: comatose, papilledema, hepatomegaly. A CT Scan reveals cerebral edema. What agent is most likely to be involved in this patient? a) Aspirin b) Acetaminophen c) Codein d) Celecoxib e) Ibuprofen “ Pain is an unpleasant sensory and emotional experience associated with actual or potential tissue damage or described in terms of such damage”. NSAIDs Relief of pain. A major presenting symptoms in common complaints. Suppress the signs and symptoms of inflammation. Exert antipyretic and analgesic effect. Useful in pain related to inflammation. Pharmacokinetics Weak organic acids (nabumetone) Well absorbed Food doesn’t change their bioavailability. Metabolized in phase I and II. Also in CYP3A, CYP2C (part CYP450) Renal, most important route of excretion. (biliary excretion and absorption) 98% Bound to Albumin. Found synovial fluid after repeating doses. Pharmacodynamics Inhibition of biosynthesis of prostaglandins. Inhibition chemotaxis, down-regulation of IL-1, decrease production of free radicals. Decrease sensitivity of vessels to bradykinin and histamine. Gastric irritants, nephrotoxity, hepatotoxicity. Aspirin irreversibly blocks COX. Aspirin® & Salicylates Acetylsalicylic Acid. 400 BC: Greek physician Hippocrates prescribes the bark and leaves of the willow tree (rich salicin) to relieve pain and fever. 1897: Chemist, Felix Hoffmann, at Bayer® in Germany, synthesizes a stable form of ASA powder that relieves his father's rheumatism. The compound later becomes the active ingredient in aspirin named - "a" from acetyl, "spir" from the spirea plant (which yields salicin) and "in," a common suffix for medications. Pharmacokinetics pKa 3.5, rapidly absorbed in the stomach and upper small bowel. Short serum half-life (20 - 25min), peak plasma level 12hrs. Bound to serum albumin 70%. Renal excretion. As Aspirin dose increases the half-life increases. At low doses its elimination follows “first order” kinetics. At high doses, “zero-order” kinetics prevails. Alkalinization of the urine increases the rate of excretion. Mechanism Actions Anti-inflammatory effect Irreversible non-selective COX inhibitor. Inhibits platelet aggregation. Interferes with the mediators of the kallikrein system (bradykinins). Inhibits chemotaxis of PMN leukocytes and macrophages. Mechanism Actions Analgesic effect Probably inhibits pain stimuli at a subcortical site. Antipyretic effect COX inhibition in the CNS, inhibition of IL-1 (released in macrophages). Mechanism Actions Antiplatelet effect Low dose (81mg). Irreversible non-selective COX inhibitor. Inhibits TXA2 synthesis. Effects last 8 – 10 days (platelet’s life). Clinical Uses As analgesic to mild to moderate pain. Combine with opiod analgesics for cancer pain. As anti-inflammatory in rheumatoid arthritis rheumatic, fever and inflammatory joint conditions. Antipyretic, when reducing the fever is desirable. Prophylaxis of ischemic heart disease, to reduce incidence of coronary artery disease. Adverse Effects Gastrointestinal effects. GI upset, Peptic ulcers, upper gastrointestinal bleeding. “Salicylism” Nausea, vomiting, tinnitus, decrease hearing, vertigo, hyperthermia, hyperventilation. Adverse Effects Hepatotoxicity. Elevation of liver enzymes, hepatitis. Hypersensibility (Asthma, Rashes) Renal toxicity (decrease function). Changes in uric acid levels (low doses – high serum levels) Adverse Effects Reyes’s-like syndrome ( Hepatoencephalopathy) highly lethal. Avoid aspirin in children with influenza or chickenpox infections (give Tylenol). Aspirin Overdose Acid-base disturbance. 1st Respiratory Alkalosis (low levels). Direct effect on the CNS respiratory centers and as a compensatory mechanism of a metabolic acidosis. 2nd Metabolic Acidosis (High levels) Depletion of HCO3, accumulation of salicylic acids derivatives, respiratory depression. 3rd Mixed Acidosis (respiratory and metabolic). Drug Interaction Acetazolamine, ammonium chloride enhances aspirin toxicity. EtOH increases GI bleeding. Reduces the activity of spironolactone. Antagonizes the effect of heparin in the platelets. Competes with Penicillin G for renal tubular secretion. Drug Interactions Inhibits the uricosuric effect of sulfinpyrazone and probenecid. Displaces drugs from proteins in serum Oral hypoglycemic agents, methotrexate, other NSAIDs. Nonacetylated Salicylates Mg Choline salicylate, sadium salicylate, salicylsalicylate. Chemically different for aspirin. Reversible platelet inhibition. Effective anti-inflammatory effect, less analgesic effect than aspirin. Can use in patient with asthma, bleeding tendencies or renal dysfunction. Nonselective COX inhibitors Mechanism is similar to aspirin (exceptions) All are: inhibitors of prothrombin synthesis, analgesic, anti-inflammatory, antipyrectic, inhibit platelet aggregation (variations). As a group: cause less gastric irritation (exceptions), nephrotoxicity. PROPIONIC ACID DERIVATIVES Ibuprofen, Naproxen, Fenoprofen. Very similar in mechanism of action and effects (compared to aspirin). More effective as analgesics, and have less adverse effects in the GI tract. Ibuprofen and Fenoprofen half-life of 2 hrs. Naproxen has a longer half-life (13 hrs). Dysmenorrhea. Adverse effects are similar: nephrotoxicity, jaundice, nausea, dyspepsia, edema, rash, pruritus, tinnitus. Interactions and contraindications: same as aspirin. ACETIC ACIDS Indomethacin Most potent inhibitor of prostaglandin synthesis (COX-1) more effective but more toxic than aspirin. Orally absorbed, highly bound to plasma proteins, half-life 2hrs. Metabolized in liver, excreted in bile and urine. Indomethacin High incidence of dose-related toxic effects: GI, severe migraine (20-25%), dizziness, confusion and depression, risk of fluid retention, hyperkalemia and blood dyscrasias. Contraindicated in pregnancy and in patients with psychosis. Indomethacin Uses Treatment of patent ductus arteriosus in premature babies. Acute gouty arthritis, ankylosing spondylitis, osteoarthritis. Pericarditis and pleurisy. Sulindac Is a pro-drug closely related to Indomethacin. It should be converted to the active form of the drug. Indications and toxicity similar to Indomethacin. May inhibit the development of breast, colon and prostate cancer. Suppresses familial intestinal polyposis disease. Tolmetin Approved for treatment of juvenile arthritis. Has a short half-life (60 min.). Fewer GI and CNS side effects than Indomethacin. Rare IgM related TTP. Not often used. Ineffective for gout. Diclofenac Gastrointestinal distress, gastrointestinal bleeding, gastric ulceration. Less frequent than other NSAIDs. Combinations with misoprostol and omeprazol reduce incidence. High doses impairs renal function. Elevates liver enzymes. FENAMATES Meclofenamate, Mefenamic acid. Analgesic, anti-inflammatory properties less effective than aspirin and clearly more toxic. Short half-lives, and should not be used for longer than one week and never in pregnancy and in children. Diarrhea and abdominal pain. Enhances oral anticoagulants. PYRAZOLONE DERIVATIVES Phenylbutazone Withdrawn from the market. Adverse effects of this drug are: agranulocytosis, aplastic anemia, hemolytic anemia, severe gastric irritation, nephrotic syndrome, optic neuritis, deafness, serious allergic reactions, exfoliative dermatitis, hepatic and renal tubular necrosis. PYRAZOLONE DERIVATIVES Oxyphenbutazone: one of the metabolites of phenylbutazone. Apazone.- Similar to phenylbutazone, but less likely to cause agranulocytosis. OXICAM Piroxicam. Half-life of 45 hrs. Once-daily dosing. Delay onset of action. High doses inhibits PMN migration, decrease oxygen radical production, inhibits lymphocyte function (high doses). Used in osteoarthritis, ankylosing spondylitis and rheumatoid arthritis. Adverse effects: GI symptoms, dizziness, tinnitus, headache, rash. Peptic ulcer (9.5 higher) Ketorolac Analgesic, no anti-inflammatory effect (market). Have typical NSAIDs properties. More analgesic efficacy. Can replace morphine in mild to moderate postsurgical pain. VO, IM, IV. Similar toxicities. Renal toxicity common with chronic use. COX-2 Selective Celecoxib, Etoricoxib, Rofecoxib, Valdecoxib, Meloxicam (preferential). Inhibit prostacyclin (COX-2) in sites of inflammation. Do not block “housekeeping” effect of COX-1. Antipyretic, analgesic and antiinflammatory effect. COX-2 Selective Indications Osteoarthritis, rheumatoid arthritis, dysmenorrhea, acute gouty attacks, acute musculoskeletal pain. Still under investigation. Rofecoxib (Vioxx®) Withdrawn from the market. Higher incidence of cardiovascular thrombotic events. Inhibits prostacyclin letting TXA2 act freely and promote platelet aggregation. Acetaminophen Para-aminophenol. Analgesic and antipyretic actions equivalent aspirin. No significant anti-inflammatory effects. No occult bleeding or gastric irritation ,do not inhibit platelet aggregation, or affect prothrombin time. No relationship with Reye’s syndrome. Does not antagonize the effects of uricosuric drugs. Acetaminophen Hepatic toxicity is its major problem. It is the drug of choice for analgesia and fever reduction in patients who cannot tolerate aspirin. Acetaminophen is the active metabolite of Phenacetin. But unlike phenacetin, doesn’t produce renal toxicity or hemolytic anemia and methemoglobinemia Acetaminophen Pharmacokinetics and Toxicity: Acetaminophen is orally absorbed, it is only slightly bound to plasma proteins. In liver is metabolized to acetaminophen glucuronide and sulfate. A minor but highly toxic metabolite builds up when gluthatione is depleted (overdose, hepatic insufficiency). Acetaminophen Large doses of acetaminophen (or in patients with liver disease), may cause severe liver damage and death. The signs of toxicity occur in 12-24: nausea, vomiting, diarrhea, abdominal pain, dizziness and death being caused by severe hepatotoxicity Sometimes associated with acute renal tubular necrosis. Administration of N-acetylcysteine, is a useful antidote. High-Yield Slides. Dr. Rosas Blum NSAIDs • Prototype aspirin. • Ibuprofen, naproxen, indomethacin. • Traditionally NSAIDs are non-selective and inhibit COX-1 and COX -2. Aspirin • The only clinically marketed irreversible inhibitor of COX-1. • Inhibits platelet aggregation. • Analgesia. • Fever reduction. • Anti-inflammatory effects. Salicylates & IBD • Salicylates derivatives are used in intra-gut treatment of IBD. • Oral drug dissociate in colon. • Enema preparations. • Mainly used in Ulcerative colitis than Crohn’s disease. Aspirin • Adverse effects. • • • • • GI Irritation (ulcers, active bleeding) Tinnitus and vertigo (early sign intoxication) Hypersensitivity. Bleeding complications. Platelet inhibition. Acid-base disorder • Mixed. • Metabolic acidosis (aspirin acid). • Respiratory alkalosis. • Stimulatory effect on breathing centers. Reye’s Syndrome • Highly Lethal • Hepatoencephalopathy. • Aspirin and derivatives may be a trigger. • Do not give in children with chickenpox or influenza B infection. Other Non-Selective NSAIDs • Ibuprofen, Naproxen • Analgesic, antipyretic and anti- inflammatory effects. • Not as effective for anti-platelet effects. Selective COX-2 inhibitors • Celecoxib, Rofecoxib. • When don’t what to inhibit COX-1. • Patients with gastric ulcers. • Similar anti-inflammatory effects as conventional NSAIDs. • Vioxx produces heart attacks. Acetaminophen • Does not inhibit COX-1 or COX-2. • Lacks of anti-inflammatory effects. • Excellent analgesic and antipyretic activity. • Mechanism of action unknown. • Acts directly in the CNS to reduce fever. NSAIDs vs Acethaminophen • No antiplatelet action • Not implicated in Reye’s syndrome. • Not bronchospastic. • Minimal GI effects. Acetaminophen overdose • Disastrous. • Mayor cause of liver failure that require liver transplant. (Teenagers and young adults). Acetaminophen Metabolism • Metabolized by liver glucoronyl transferase to • • • form an inactive compound. Minor CYP-dependent pathway produces a Nacetyl-para-benzoquinonimine, a reactive metabolite that is inactivated by glutathione. In serious overdose glutathione becomes depleted, and metabolite damages hepatocytes. EtOH enhances liver toxicity via induction of CYP2E1 enzyme. Acetaminophen overdose • Antidote N-acetylcysteine. • Replenishes glutathione stores. • Most effective when used in the first 12 hrs before liver damage becomes irreversible. A 5-year-old girl is brought to the emergency department by her parents in a comatose state. Her parents refers that she felt ill recently with high fever. Physical examination: comatose, papilledema, hepatomegaly. A CT Scan reveals cerebral edema. What agent is most likely to be involved in this patient? a) Aspirin b) Acetaminophen c) Codein d) Celecoxib e) Ibuprofen [email protected]