* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Bacillus - Cal State LA - Instructional Web Server
Sociality and disease transmission wikipedia , lookup
Vaccination wikipedia , lookup
Germ theory of disease wikipedia , lookup
Globalization and disease wikipedia , lookup
Multiple sclerosis research wikipedia , lookup
Schistosomiasis wikipedia , lookup
Childhood immunizations in the United States wikipedia , lookup
Neonatal infection wikipedia , lookup
African trypanosomiasis wikipedia , lookup
Infection control wikipedia , lookup
Traveler's diarrhea wikipedia , lookup
Bioterrorism wikipedia , lookup
Coccidioidomycosis wikipedia , lookup
Clostridium difficile infection wikipedia , lookup
Hospital-acquired infection wikipedia , lookup
Gastroenteritis wikipedia , lookup
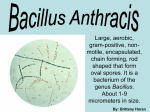
Bacillus Aerobic Gram-Positive Bacilli Bacillus • Large, G(+) rods, square cut ends • Saprophyte in nature; soil, dust • Aerobic, facultative anaerobic • Spore former, survive in environment • Lab presumptive ID by spore stain • Most motile • B. anthracis = non-motile Bacillus: Genera • B. anthracis - “charcoal” carbuncle; major pathogen, anthrax disease • B. cereus – “waxen”, gastroenteritis (rice, meat, vegetable), opportunistic infections • B. subtilis – isolated as contaminant in clinical specimens, opportunistic infections (catheter, prosthesis) Bacillus: Lab Culture • Grows well on ordinary lab media, CBA • Large granular colonies, irregular edge; coarse, dull or frosted-glass texture • B. cereus = hemolytic • B. anthracis = nonhemolytic Bacillus anthracis: Virulence Factors • Capsule resist phagocytosis; lab presumptive ID by stain or DFA (direct fluorescent antibody) test • Exotoxins complex, coded by plasmid; three genes (three proteins, each alone not toxic) – – – – Protective antigen (PA) - bind Lethal factor (LF) - active Edema factor (EF) - active PA combine with LF or EF, binds to host cell receptor, entry into host cell; LF & EF toxic Bacillus anthracis: Two Toxins • Lethal toxin: PA + LF; protease, causes cell death • Edema toxin: PA + EF; increase in cAMP, results in edema • Both toxins: – increase vascular permeability – interferes with phagocytosis Bacillus anthracis: Anthrax • Mainly disease of animals - acquire MO by ingestion or inhalation of spores • Spores extremely resistant, source of infection in soil 2-3 years • Humans acquire anthrax: – Contact animal products (hides, fur, wool, hair) – Less commonly, work in agricultural setting with infected animals • Disease depends on mode of transmission – Skin (cut, abrasion, wound) – Ingestion – Inhalation Cutaneous Anthrax • Most common (95% infections) • Spores enter exposed skin, germinate, multiply • Exotoxin released, rapid development of pustule • Occasionally, MO disseminate - septicemia, death in few days • Vascular injury - edema, hemorrhage, thrombosis • Death - respiratory failure, anoxia by toxin on CNS • Mortality ~20% if untreated Gastrointestinal Anthrax • Ingest spores, inoculated into lesions of mucosa • Ulcers in mouth, esophagus, intestine • GI tract symptoms – nausea, vomiting, malaise • Lead to lymphadenopathy, edema, sepsis • Rapidly progress to systemic disease • High mortality, as anthrax not suspected Inhalation Anthrax (Woolsorter‘s Disease) • Inhale spores by aerosols into RT • Germinate in lungs, multiply, spread to cause fatal septicemia or meningitis • Most serious form of disease • High mortality, as anthrax not suspected • Use as biologic weapon – need to break up spore clumping, aerosolize, so can reach airway • CDC category A Select Biological Agent – Weaponized spores inhaled, easily disseminated – Inhalation anthrax fatal unless treated immediately Bacillus anthracis: Treatment and Prevention • Sensitive to penicillin, but some strains now showing resistance • Ciprofloxacin drug of choice, • Control infection in animals: – Vaccine useful to prevent infection – Bury diseased animals • Short-term PA vaccine available for at high risk individuals, less useful Bacillus cerus: Opportunistic Infections • Ubiquitous, infecton via contaminated soil • Gastroenteritis – two different enterotoxins (emetic, diarrheal) • Cytotoxin - cerolysin, phospholipase) • Eye infection – traumatic injury • Endocarditis – commonly IV drug abuser • Pneumonitis, bacteremia, meningitis immunocompromised patient, neonate, IVcatheter, surgery patient • Resistant to penicillin – combination treatment of clindamycin + gentamycin Food Poisoning: Emetic Form • Contaminated fried or boiled rice, spores survive cooking • Rice not refrigerated, spores germinate, MO release enterotoxin • Intoxication – ingest toxin in rice; toxin not destroyed by reheating rice • Short incubation <6 hr.- vomiting, nausea, abdominal cramps, ±diarrhea (33%) • Last <24 hr. Food Poisoning: Diarrheal Form • Infection – ingest contaminated soup, meat, vegetable, sauce, pudding • Longer incubation >6 hr., MO multiplies, release toxin; diarrhea, nausea, abdominal pain, ±vomiting (25%) • Last >24 hr. • Both forms of food poisoning short, uncomplicated • Symptomatic treatment adequate • Prevent by proper food handling Class Assignment • Textbook Reading: Chapter 16 Aerobic Gram-Positive Bacilli – Bacillus • Key Terms • Learning Assessment Questions Case Study 6 - Bacillus • A 56-year-old female postal worker sought medical care for fever, diarrhea, and vomiting. • She was offered symptomatic treatment and discharged from the community hospital emergency department. • Five days later she returned to the hospital with complaints of chills, dry cough, and pleuritic chest pain. • A chest radiograph showed a small right infiltrate and bilateral effusions but no evidence of a widened mediastinum. Case Study 6 - Bacillus • She was admitted to the hospital, and the next day her respiratory status and pleural effusions worsened. • A computerized tomographic (CT) scan of her chest revealed enlarged mediastinial and cervical lymph nodes. • Pleural fluid and blood was collected for culture and was positive within 10 hours for gram-positive rods in long chains. Case Study - Questions • 1. The clinical impression is that this woman has inhalation anthrax. What tests should be performed to confirm the identification of the isolate? • 2. What are the three primary virulence factors found in B. anthracis? • 3. Describe the mechanisms of action of the toxins produced by B. anthracis. • 4. Describe the two forms of B. cereus food poisoning. What toxin is responsible for each form? Why is the clinical presentation of these two diseases different?