* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Overdose Prevention with Community Based Naloxone: An …
Neuropharmacology wikipedia , lookup
Compounding wikipedia , lookup
Drug interaction wikipedia , lookup
Polysubstance dependence wikipedia , lookup
Drug design wikipedia , lookup
Adherence (medicine) wikipedia , lookup
Theralizumab wikipedia , lookup
Drug discovery wikipedia , lookup
Pharmaceutical industry wikipedia , lookup
Dextropropoxyphene wikipedia , lookup
Pharmacokinetics wikipedia , lookup
Pharmacogenomics wikipedia , lookup
Prescription costs wikipedia , lookup
Electronic prescribing wikipedia , lookup
Prescription drug prices in the United States wikipedia , lookup
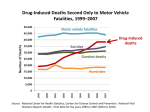
Overdose Prevention with Community Based Naloxone Sharon Stancliff, MD Harm Reduction Coalition Motor vehicle traffic, poisoning, drug poisoning, and unintentional drug poisoning death rates: United States, 1999--2010 Motor vehicle traffic 18 Deaths per 100,000 population 16 Poisoning 14 12 Drug poisoning 10 Unintentional drug poisoning 8 6 4 2 0 1999 2000 2001 2002 2003 2004 2005 2006 2007 2008 2009 2010 NOTES: Drug poisoning deaths are a subset of poisoning deaths. Unintentional drug poisoning deaths are a subset of drug poisoning deaths. SOURCE: CDC/NCHS, National Vital Statistics System; and Warner M, Chen LH, Makuc DM, Anderson RN, Miniño AM. Drug poisoning deaths in the United States, 1980–2008. NCHS data brief, no 81. Hyattsville, MD: National Center for Health Statistics. 2011. http://www.cdc.gov/nchs/data/databriefs/db81.htm. Intercensal populations http://www.cdc.gov/nchs/nvss/bridged_race/data_documentation.htm Number of drug poisoning deaths involving opioid analgesics by opioid analgesic category, heroin and cocaine: United States, 1999--2010 12,000 Natural and semisynthetic opioid analgesic Number of deaths 10,000 Methadone 8,000 6,000 Cocaine 4,000 Heroin 2,000 Synthetic opioid analgesic, excluding methadone 0 1999 2000 2001 2002 2003 2004 2005 2006 2007 2008 2009 2010 NOTES: Opioid analgesic categories are not mutually exclusive. Deaths involving more than one opioid analgesic category shown in this figure are counted multiple times. Natural and semi-synthetic opioid analgesics include morphine, oxycodone and hydrocodone; and synthetic opioid analgesics include fentanyl. SOURCE: CDC/NCHS, National Vital Statistics System; and Warner M, Chen LH, Makuc DM, Anderson RN, Miniño AM. Drug poisoning deaths in the United States, 1980–2008. NCHS data brief, no 81. Hyattsville, MD: National Center for Health Statistics. 2011. http://www.cdc.gov/nchs/data/databriefs/db81.htm Inpatient admissions for heroin use 6 5 Rate Per 100,000 4 16-19 20-23 24-27 3 28-31 32-35 36-39 2 40-43 44-47 48-51 52-55 1 0 1993 1997 2001 2005 2009 Unick, GJ et al, 2013, PLOSONE, in press Opioid overdoses • • • • Overdoses evolve over 1-3 hours There are often bystanders Naloxone is a safe and effective antidote Many overdoses deaths are preventable with prompt recognition and treatment Source: Sporer, K. 2006 Naloxone (Narcan) • Prescribed opioid antagonist which rapidly reverses opioid related sedation and respiratory depression and may cause withdrawal • Overdose victims wake up minutes after administration • Displaces opioids from the receptors for 30-90 minutes • No pleasant psychoactive effects • Routinely used by EMS Naloxone preparations • Injectable – Less expensive: $6.50 per dose – Well-documented efficacy – Requires injection, drawing from a medical vial into a syringe • Intranasal – More expensive: $21.00 per dose – Less well-documented efficacy – Requires assembly of spay device with nasal adaptor and naloxone capsule 7 Models of increasing access to naloxone • Community prescribing/distribution to drug user and/or social networks • Prescribing in outpatient care • Increasing access among first responders • Pharmacy collaborative agreements Legal issues • • • Most states allow for prescription of naloxone to those at risk of overdose Some states have passed legislation to allow for prescribing to anyone potentially at risk of witnessing an overdose (NY, NM, Il, WA, CA, RI, MA, CT) Other jurisdictions have passed local laws or initiated pilot programs Appropriate Settings for Naloxone Assess • Syringe access • Homeless shelters programs • Post-incarceration • HIV programs • Primary care and • Drug treatment other health care – Methadone or settings Suboxone programs • Parent support – Detoxification groups – Residential or outpatient treatment Overdose prevention knowledge • Preventionunderstanding the role of: – mixing drugs – reduced tolerance – using alone • Overdose recognition • Actions – – – – Call 911 Rescue breathing Naloxone administration After-care Reversing an overdose: Program Support • New York, New Mexico and Massachusetts operate state-wide programs supported by State Departments of Public Health • City Health Departments support programs in Baltimore, San Francisco, Seattle, New York City • Connecticut, Washington, New Mexico, New York, have passed Good Samaritan laws to encourage calling 911 (NM, WA, NY, CT IL Overdose prevention programs: US MMWR report based on survey of programs known to the Harm Reduction Coalition • As of 2010, there were 48 known programs, representing 188 community-based sites in 15 states and DC. CDC MMWR February 17, 2012 http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6106a1.htm Survey completed by Eliza Wheeler [email protected] Overdose fatality prevention programs that distribute naloxone: USA, 2010 2010 survey of programs known to the Harm Reduction Coalition • 189 local programs in 16 states ranging from state-funded to underground 1996 - 2010: • 53,339 individuals have received kits • 10,194 overdose reversals reported CDC MMWR February 17, 2012 http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6106a1.htm naloxone: USA, 2010 Implementation in NYS Agencies register and use their own resources 0ver 80 so far • Syringe exchange/syringe access sites • Hospitals • Drug Treatment: Methadone, detox, 28 day and Therapeutic Community • HIV programs • Homeless shelters • Primary care Prescribing to those at risk • Project Lazarus, North Carolina: A multifaceted OD prevention program including provision of naloxone to chronic pain patients • Operation OpioidSafe, Ft Bragg: replicated aspects of Project Lazarus including naloxone • Brason, Replication of Project Lazarus comprehensive community based model to reduce opioid medication overdoses among active duty soldiers determined to be at risk within select US military bases by implementing the naloxone rescue component as Standard Operating Procedure APHA 2011 Potential Indications/Populations 1. Patient release after emergency medical care involving opioid poisoning/intoxication 2. Suspected history of illicit or nonmedical opioid use 3. High-dose opioid prescription (> 50 mg of morphine equivalence/day) 4. Any methadone prescription to opioid naïve patient Any opioid prescription and … 5. smoking/COPD/emphysema/asthma or other respiratory illness or obstruction 6. renal dysfunction, hepatic disease 7. known or suspected concurrent alcohol use 8. concurrent benzodiazepine prescription 9. concurrent SSRI or TCA anti-depressant prescription 10. Prisoner released from custody 11. Release from opioid detoxification or mandatory abstinence program 12. Voluntary request from patient 13. Patients in methadone or buprenorphine detox/maintenance (for addiction or pain) 14. Patient may have difficulty accessing emergency medical services (distance, remoteness) source + more info at projectlazarus.org 15. Other (specify): _______________________________________ Pharmacy Collaboration NEW NEWS! Collaborative Drug Therapy Agreement for Naloxone Medication in Opioid Overdose Reversal I, __________________, MD, a licensed health care provider authorized to prescribe medication in the State of Washington, delegate prescriptive authority to _______________________ Pharmacy and the pharmacists listed below to initiate drug therapy for the treatment or prophylaxis of opioid overdose according to the protocol that follows. The protocol provides written guidelines for the pharmacists to dispense medication in accordance with the laws (RCW 18.64.011) and regulations (WAC 246‐ 863‐100) of the State of Washington. The pharmacists shall document all drug therapy initiated under this protocol. As the authorizing prescriber, I or authorized staff under my supervision will be available to review the drug therapy initiated by the pharmacists. This protocol will be in effect for two years unless rescinded earlier in writing to the Washington State Board of Pharmacy by either party. Any modification of the protocol shall be treated as a new protocol and filed with the Washington State Board of Pharmacy. Creative strategies for preventing overdose: Massachusetts Source: Four Tales of Overdose Survival, Massachusetts Bureau of Substance Abuse Services, SA1069, 2009 Source: Four Tales of Overdose Survival, Massachusetts Bureau of Substance Abuse Services, SA1069, 2009 Source: Four Tales of Overdose Survival http://www.maclearinghouse.com/PDFs/SubstanceAbuse/SA1069.pdf Source: Four Tales of Overdose Survival, Massachusetts Bureau of Substance Abuse Services, SA1069, 2009 Source: Four Tales of Overdose Survival, Massachusetts Bureau of Substance Abuse Services, SA1069, 2009 Role of EMS Patients receiving naloxone, not being transported to ER: deaths known to medical examiner • 998 patients refused transport: none within 12 hours • 552 patients refused transport: none within 48 hours • 2241 patients discharged by EMS over 10 yrs: 3 died (0.13%) of potential rebound overdose Limitations: some medical evaluation, varying doses of naloxone; all SKOOP responders instructed to call EMS • San Diego: Vilke Acad Emerg Med 2003; San Antonio: Wampler Prehosp Emerg Care 2011; Copenhagen: Rudolph Rescusitation 2011 Incremental Cost Effectiveness Ratio • ICER = Added cost of intervention divided by increase in Quality adjusted life year • Generally accepted threshold is $50,000/year • Chlamydia screening, Problem drinking screening both < $14,000 • Naloxone provision $438- $14,000 depending on variables used • Coffin 2013, Outcomes per 1 million heroin users Change if naloxone given to 20% of heroin users Baseline OD Increase by 60,000 OD death Decrease by 10,000 Kits to prevent 1 death 164 Cost / QALY gained $400 If naloxone reduces OD risk behaviors OD Decrease by 1,000,000 OD death Decrease by 43,000 Kits to prevent 1 death 36 Cost / QALY gained Cost-saving Opioid Overdose Prevention: Who Gets there first? Richard Cotroneo, Director HIV Education and Training Programs OMD, AIDS Institute NYSDOH • 1,250 EMT staff trained • More than 50 overdose events reversed • Excellent news coverage • No serious adverse events reported Is naloxone distribution decreasing mortality? Observational studies in places with overdose prevention programs find an association with reductions in overdose deaths: • Massachusetts, New York City, San Francisco, Baltimore, Pittsburgh, Chicago More studies are in progress 39 Heroin-related Deaths, San Francisco, 1993-2011 160 140 Naloxone distribution begins, 2003 120 100 Heroin-related deaths 80 60 40 20 0 19931994 19941995 19951996 19961997 19971998 19981999 19992000 20022003 *Data compiled from San Francisco Medical Examiner’s Reports, www.sfgsa.org **no data available for FY 2000-2001 20032004 20042005 20052006 20062007 20072008 20082009 20092010 20102011 The DOPE Project 2003-2012 700 600 500 400 New Enrollments Refills 300 Reversals 200 100 0 2003 2004 2005 2006 2007 2008 2009 2010 2011 2012 Unintentional drug poisoning deaths decreased by 37% in NYC from 2005 to 2010 Number of unintentional drug poisoning deaths 12.3 14 12.9 800 12 10.5 700 9.4 9.3 Number 600 10 7.9 8 500 400 801 838 695 300 6 631 624 200 516 4 2 100 0 0 2005 2006 2007 2008 Year of death Source: NYC OCME & NYC DOHMH- BADUPCT, 2005-2009 Age-adjusted mortality rate per 100,000 New Yorkers 900 Age-adjusted Rate 2009 2010 Cocaine and heroin rates decreased while opioid analgesic rate increased 500 Number 400 300 Heroin Cocaine* Benzodiazepines* Sedatives 200 Opioid Analgesics* Anti-Depressants Methadone 100 Anti-Psychotics 0 2005 * P-Value less than .05; (2005 vs. 2009) 2006 2007 2008 Year Drugs are not mutually exclusive 2009 2010 43 Massachusetts • Massachusetts compared towns by enrollment in Opioid Education and Naloxone Distribution programs determining Adjusted Rate Ratios • Controlled for: city/town population rates of age under 18, male, race/ ethnicity (hispanic, white, black, other), below poverty level, medically supervised inpatient withdrawal treatment, methadone treatment, BSAS-funded buprenorphine treatment, prescriptions to doctor shoppers, and year A. Walley et al Is implementation of bystander overdose education and naloxone distribution associated with lower opioid-related overdose rates in Massachusetts? AMERSA 2011 Results Fatal opioid OD rates were lower in citiestowns: • Where program enrollment reached a density of 150 per 100k population (ARR: 0.74) • Where drug user enrollment was high (ARR:0.78) • Where there were high annual rates of reversals reported (ARR: 0.74) No differences were found in nonfatal opioid OD rates. Federal Support SAMHSA is finalizing an overdose prevention tool kit to be sent to all Outpatient Treatment Programs ONDCP participated in a webinar on the topic with Safe States and CDC 12/12 FDA which held a workshop in collaboration with HHS, NIDA and CDC on increasing access to naloxone 4/12 Italy Rescheduled naloxone as an over the counter medication in 1987 Medication not subject to medical prescription. International Support UN Resolution: Promoting measures to prevent drug, in particular opioid overdose Encourages Member States to include effective drug overdose prevention and treatment elements in national drug policies ... including the use of opioid receptor antagonists such as naloxone; Requests the UNODC & WHO, circulate best practices on drug overdose treatment and emergency response and to provide advice, guidance and capacity-building on preventing mortality from drug overdose Programs without Naloxone Lack of naloxone should not deter overdose prevention education and training • Screening for risk of overdose and giving information: risks, prevention, recognition, calling 911 and rescue breathing CAN HELP SAVE LIVES! • Make OD screening and training a standard of care 49 Conclusions • Many overdoses can be prevented • Ask about risk factors and educate patients • Overdose training consists of a few basic components • Integrate into intake, medical visits and patient care • Drug users, friends, and family can learn to prevent and safely treat overdose • Goals: • Overdose training as standard of care • Naloxone available over the counter 50