* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Chemotherapy
Survey
Document related concepts
Human microbiota wikipedia , lookup
Unique properties of hyperthermophilic archaea wikipedia , lookup
Carbapenem-resistant enterobacteriaceae wikipedia , lookup
Bacteriophage wikipedia , lookup
Small intestinal bacterial overgrowth wikipedia , lookup
Neisseria meningitidis wikipedia , lookup
Transcript
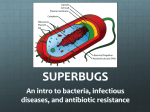
Chemotherapy Chemotherapeutic Agents Definition Chemotherapy is the science that deals with the treatment of disease by means of chemicals (chemotherapeutic agents) that have a specific toxic effect upon the disease-producing microorganisms or that selectively destroy cancerous tissue. Chemotherapeutic agents are: • Antibacterial drugs including antibiotics • Antifungal drugs • Antiviral drugs • Antiprotozoal drugs • Anticancer drugs. Antibiotics (major chemotherapeutic agents) are defined as: Any chemical substances produced by various microorganisms and fungi, having the capacity (in dilute solutions) to inhibit the growth of or to destroy other microorganisms; used chiefly in the treatment of infectious diseases. Some of antibiotics could be used in treatment of cancer diseases. Characteristics of clinically useful Antibiotics •It should have a wide spectrum of activity with the ability to destroy or inhibit different species of pathogenic organisms. • It should be nontoxic to the host and without undesirable side effects. • It should be non-allergenic to the host. • It should not eliminate the normal flora of the host. Characteristics of clinically useful Antibiotics • It should be able to reach the part of the human body where the infection is occurring. • It should be inexpensive . • It should be chemically-stable(have a long shelf-life). • Microbial resistance is uncommon and unlikely to develop. Patient–Drug–Pathogen interaction. In the laboratory the strain of pathogen, the number of infecting organisms, the culture medium, the antibiotic concentration, and the duration of antibiotic exposure can be precisely specified. This precision cannot be obtained in patients since chemotherapy of human disease is complex, as it depends on a complex patient– drug–pathogen interaction. This interaction has six components: Pharmacokinetics (What the patient does to the drug) Pharmacodynamics (What the drug does to the patient) Immunity (What the patient does to pathogen) Sepsis-Infection (What the pathogen does to patient) Resistance (What the pathogen does to the drug) Selective toxicity (What the drug does to the pathogen). Pharmacokinetics To be clinically useful, a chemotherapeutic drug must have both: Selective toxicity against pathogen. Favorable pharmacokinetics. The concentration of the drug in a patient’s body as a function of time is determined by the dose administered & the drug’s pharmacokinetics. Absorption Oral Absorption can be affected by drugs and by food. Aluminum, calcium, and magnesium ions in antacids or dairy products form insoluble chelates with all Tetracyclines and inhibit their absorption. Systemic use of drugs that are poorly absorbed or are destroyed by GI environment requires parenteral administration. If the goal is to attack pathogens in GIT then poor GIT absorption may be an advantage. Pharmacokinetics An antibiotic that is itself nontoxic may have metabolites that are toxic, diminishing its usefulness. For example, Imipenem is hydrolyzed by renal dipeptidase to a metabolite that is inactive against bacteria but is toxic to humans. Co- administration of cilastatin inhibits the renal dipeptidase, which both prevents the formation of the toxic metabolite and decreases Imipenem clearance, prolonging the half-life of the drug. Partitioning Partitioning of some drugs into cells occurs. Macrolides and Flouroquinolones are selectively partitioned into cells which accounts in part for their efficacy against mycoplasma and Chlamydia (intracellular pathogens). The concentrations of chemotherapeutic drugs in plasma, CSF, urine, or ascites fluid can be measured to determine whether sufficient drug is present to inhibit or kill a given pathogen and to ensure that the concentration is not so high as to be toxic to the patient. (e.g. Aminoglycosides)…..TDM Pharmacodynamics In the case of antibiotic chemotherapy, the ideal Pharmacodynamics response is usually obtained; the pharmacological target is not normal human cells but rather a pathogen, parasite, a virus-infected human cell, or a cancerous cell. The less selective the chemotherapeutic drug, the greater the severity of adverse effects. Pharmacodynamics Comparing with other drugs, antibacterial chemotherapeutic drugs are remarkably safe. Toxicity is common mainly in patients who are given inappropriately high doses or who develop high drug levels because of decreased drug clearance. Most antibiotics are renally cleared, so renal failure is a common cause of diminished antibiotic drug clearance Dosage adjustment needed Contraindicated in renal in hepatic impairment impairment 1.Chloramphenicol 2. Clindamycin 3. Erythromycin 4. Clarithromycin 5. Indinavir 6. Metronidazole 7. Tigecycline 1. Nalidixic acid 2. Long acting Sulfonamides 3. Tetracyclines except (Minocycline) 4. Methenamine 5. Cidofovir Adverse effects associated with the use of Antibacterials Allergic reactions. Toxic reactions resulting from inappropriate high doses. Interactions with other drugs. Reactions related to alterations in normal body flora “Superinfection”(e.g. Clindamycin-induced pseudomembranous colitis). Idiosyncratic reactions( due to pharmacogenetics e.g. sulfonamide causing severe RBC hemolysis in people having G6PDH deficiency). Allergic Responses Immediate hypersensitivity reactions (anaphylaxis). Delayed sensitivity reactions (interstitial nephritis). Hapten-mediated serum sickness. Allergic cross-reactions to structurally related antibiotics can occur. Superinfection Many antibiotics alter the enteric microbial flora, particularly if high concentrations reach the colon. Antibiotic-sensitive bacteria are suppressed or killed, thereby removing their inhibitory effects on potentially pathogenic organisms. Overgrowth of pathogenic microbes can then occur. For example, Clostridium difficile is resistant to Clindamycin. Use of such an antibiotic permits the proliferation of C. difficile, which then elaborates its toxin in high concentration. This toxin can cause PMC, which can be fatal if not recognized and treated. Immunity The effectiveness of chemotherapeutic agents is enhanced by adequate immune function; however, some antibiotics suppress immune function. Immunity In the absence of antibiotic therapy, many patients survive infection, even infection by highly virulent pathogens. Thus, immunity may be due to factors such as a high functional reserve of organs or to an enhanced nonspecific Opsonization (the process by which a pathogen is marked for ingestion and destruction by a phagocyte) of pathogens by complement. Immunity In other cases, specific partial immunoglobulin IgG–mediated immunity was produced during prior exposure to the pathogen or a new IgMmediated immunity develops during the course of the infection. Specific immunity can be either cell mediated or antibody mediated & may be enhanced by endogenous cytokines. Exogenously administered cytokines also may prove clinically useful as adjuncts to antibiotic chemotherapy. Sepsis It is a reaction to severe infections in which a variety of mediators are released. Some of these mediators are bacterial metabolic products, while others are cytokines produced by humans during infection. These mediators can induce failure of several organ systems. Cardiac function can be suppressed; acute respiratory distress syndrome can occur; and renal failure is common. Through their ability to cause cell lysis, antibiotics (Beta-lactams or Aminoglycosides )may increase the release of bacterial mediators (e.g. endotoxin). Sepsis Antibiotics also may induce the release of endogenous cytokines, such as interleukin (IL- 1 , IL-6, and TNF from monocytes and IL-4 and IFN- from lymphocytes. These cytokines are important in immunological responses and may contribute to the development of sepsis. Bacterial Resistance • A resistance to an antibiotic can be the result of one or more mechanisms. Alterations in the lipopolysaccharide structure of gram-negative bacilli can affect the uptake of lipophilic drugs. Similarly, changes in porins can affect the uptake of hydrophilic drugs. Once the drug enters the cell, it may be enzymatically inactivated. Some bacteria possess pumps that remove drugs from the bacterial cytosol. The antibiotic also may be ineffective as a result of mutation of genes coding for the target site (e.g., penicillin-binding proteins, DNA gyrase, or ribosomal proteins). Cell membrane Bacterial resistance Acquired resistance, is a result of the following: Spontaneous, random chromosomal mutations: These mutations are commonly due to a change in either a structural protein receptor for an antibiotic or a protein involved in drug transport. Bacterial Resistance Extrachromosomal transfer of drug-resistant genes Transformation is transfer of naked DNA between cells of the same species. Transduction via R plasmids is asexual transfer of plasmid DNA in a bacterial virus between bacteria of the same species. Conjugation is the passage of genes from bacteria to bacteria via direct contact through a sex pilus or bridge. Conjugation occurs primarily in gram-negative bacilli, and it is the principal mechanism of acquired resistance among enterobacteria. Transpositions occur as a result of movement or “jumping” of transposons (stretches of DNA containing insertion sequences at each end) from plasmid to plasmid or from plasmid to chromosome and back. Selective targeting (Selective toxicity) • The goal of chemotherapeutic agents is selective toxicity, i.e. inhibiting pathways or targets that are critical for pathogen or cancer cell survival and replication at concentrations of drug lower than those required to affect host pathways. Selectivity can be realized by 1. Targets (metabolic pathways, enzymes, genes) unique to the pathogen or cancer cell that are not present in the host. One attractive target for antibacterial drugs is the bacterial Peptidoglycan cell wall. This structure is both biochemically unique and essential for the survival of growing bacteria. (Beta-lactams antibiotics inhibit transpeptidase enzymes that catalyze the final cross-linking step in Peptidoglycan synthesis). Selectivity Fungi present two unique targets (cell wall and ergosterol) that are exploited by antifungal drugs: Echinocandins inhibit beta-(1, 3)-D-Glucan, essential component of fungal cell wall. Azoles inhibit ergosterol biosynthesis in fungal cells changing their permeability and cause cell death Selectivity 2. Targets in the pathogen or cancer cell that are similar but not identical to those in the host. Many organisms have metabolic pathways similar to those of human but, because of evolutionary divergence, possess distinct enzyme or receptor isoform. Drugs can have quantitatively different binding specificities based on these biochemical differences. Selectivity Example: Inhibitors of dihydrofolate reductase( DHFR) DHFR is a crucial enzyme in the synthesis of purines & pyramidines building blocks of DNA. Human, bacteria, and protozoa all utilize DHFR in DNA synthesis, but the DHFR isoforms are genetically and structurally distinct and can therefore be targeted by different drugs. Methotrexate powerfully inhibits DHFR in human as well as bacterial and protozoal cells & this drug’s low selectivity produce high toxicity in man. In contrast, Trimethoprim selectively inhibit bacterial DHFR and Pyrimethamine selectively inhibits the malarial DHFR. Lethal vs Inhibitory effects of Antibiotics Antibiotics can be classified according to their effects on the molecular biology of bacteria. Ribosomal inhibitors (Macrolides). Cell wall disrupters (beta -lactams). DNA disturbers (Flouroquinolones). Metabolic poisons (trimethoprim-sulfamethoxazole) Classification Antibiotics also can be classified : Bacteristatic (inhibitory) Bactericidal (lethal). Bactericidal Effects (Irreversible) These effects are the result of the disruption of the cell wall or membrane. Cell lysis may occur when water diffuses into the highosmolarity bacterial cytosol through the antibiotic-induced holes in the membrane, causing the bacteria to swell and burst. Cidal effects also can occur as a consequence of inhibition of bacterial DNA replication or transcription. A cidal drug may prove to be merely static if an inappropriately low dose or short treatment course is prescribed. A static drug may be cidal if given in high doses for prolonged courses to exquisitely sensitive pathogens. Static Effects (Reversible) For example, inhibition of folate synthesis interferes with methylation, a biochemical synthetic process. Reversal of this static effect can occur when the antibiotic concentration falls or if a compensatory increase in the synthesis of the inhibited enzymes occurs. The place of a drug along this spectrum will depend on both the pharmacological properties of the drug and such clinical factors as immune system function, drug concentration in tissue, and duration of therapy. Bactericidal Antibiotics Concentration -dependent Aminoglycosides Bacitracin Quinolones Bacteriostatic Antibiotics Time- dependent Beta-Lactams Isoniazid Metronidazole Rifampicin Vancomycin Pyrazinamide Tigecycline Tetracyclines Chloramphenicol Clindamycin Macrolides Oxazolidinones Sulfonamides Trimethoprim 1. Drug may be static against one organism and cidal against another. 2. Concentration-dependent cidal agents have a rate of killing that increases with drug concentration, while time-dependent cidal agents exhibit constant rate of killing independent of drug concentration. Selection of Antibiotics Factors taken into consideration: The identity of the infecting organism. Drug sensitivity of the infecting organism Host factors (site of the infection, status of host defenses). Empiric therapy prior to completion of lab. tests: it may be necessary to begin treatment in patients with serious infections before the lab results. Host Factors Host defenses (immune system and phagocytic cells). Site of infection: to be effective an antibiotic must be present in the site of infection in a level greater than MIC endocarditis, meningitis. Age (infants and elderly highly vulnerable to drug toxicity). Pregnancy and lactation. Previous allergic reactions. Genetic factors (hemolysis in patients with G-6PD deficiency if given sulfonamides). Combination Chemotherapy Combination chemotherapy is recommended for chronic infections (tuberculosis, AIDS ) and most anticancer drug regimens. There are several reasons to administer multiple drugs simultaneously in a combination chemotherapy regimen: The use of multiple drugs with different mechanisms of action targets multiple steps in microbial or cancer cell growth leading to the maximal possible rate of cell killing. Combination Chemotherapy The use of combinations of drugs that target different pathways or molecules in pathogen or cancer cell makes it more difficult for resistance to develop. The use of lower doses of synergistically acting drugs in the combination can reduce drug-induce adverse effects. This is especially important in antimicrobial chemotherapy, where synergistic activity ofdrug combinations has been clearly demonstrated. Combination Chemotherapy Because many anticancer drugs have different dose-limiting adverse effects, it is often possible to give each drug to its maximally tolerated dose and thereby achieve increased overall cell killing. The concept of combination chemotherapy is being redefined as new treatments become available. In the future, immunotherapies, hormone therapies, and biotherapies will become increasingly integrated into combination chemotherapy regimens (Protein therapeutics). Combination Chemotherapy The combination of two bactericidal drugs can be synergistic (greater than the sum of the effects of each drug alone). The combination of two Bacteristatic drugs can also be synergistic, but in most cases it can result in additive effects Disadvantages of combination chemotherapy (Unfavorable) Bacteristatic and bactericidal effects are also important to consider when antibiotics are used clinically in combination. The combination of Bacteriostatic drug with bactericidal drug can result in Antagonistic effects. Disadvantages of combination For example: The Bacteristatic drug (Tetracycline) inhibits protein synthesis and thereby retards cell growth and division. The action of this drug antagonizes the effect of cell wall synthesis inhibitor (penicillin), which requires bacterial growth in order to be effective. Clinical example: pneumococcal meningitis treated by penicillin and tetracycline ? Prophylactic Chemotherapeutic (Chemoprophylaxis) Antimicrobial and anticancer drugs are used to treat overt diseases. These drugs can also be used to prevent diseases from occurring (prophylaxis), both before a potential exposure and after a known exposure. The potential benefit of chemoprophylaxis must always be weighed against the risk of creating drug-resistant pathogens or cancer cells and the potential for toxicity due to chemoprophylactic agent. Prophylaxis Antimicrobial prophylaxis is frequently used in high-risk patients to prevent infection. Travelers to malaria-infested areas often take prophylactic antimalarial agent (Mefloquine). Chemoprophylaxis can also be used in healthy persons after exposures to certain pathogens. Prophylactic therapy after known or suspected exposure to gonorrhea, syphilis, meningitis, HIV, and others can often prevent diseases Non-surgical prophylaxis Infection Cholera Plague Anthrax Indication Close contact Close contact Suspected exposure Tuberculosis H.influenza infection Meningococcal infection Genital herpes simplex Otitis media UTI Malaria Close contact Close contact Close contact Recurrent infection Recurrent infection Recurrent infection Travelers to endemic area Rheumatic heart disease Benzathine penicillin Rheumatic fever Proper drug Tetracyclines Tetracyclines Ciprofloxacin or Doxycycline INH, Rifampin, PZA Rifampicin Rifampicin Acyclovir Amoxicillin Co-trimoxazole Mefloquine Surgical Prophylaxis Chemoprophylaxis is also used in some types of surgery to prevent wound infections. Antibiotics are usually administered prophylactically during surgical procedures that could release bacteria into the wound site. Surgical Prophylaxis Type of operation Pathogen Proper drug Neurosurgical Staphylococci Cefazolin Head and neck S.aureus Cefazolin Gastroduodenal S.aureus Cefazolin Biliary tract Enterococci Cefazolin Cesarean section Anaerobes Cefazolin Colorectal Anaerobes Cefoxitin, Cefotetan Appendectomy Anaerobes Cefoxitin or Cefazolin + Metronidazole Pharmacology of Pathogens Infections/ Classification: Inhibitors of Folate metabolism: Sulfonamides inhibit dihydropteroate synthetase. Trimethoprim and Pyrimethamine, inhibit dihydrofolate reductase. Pharmacology of bacterial infections: Inhibitors of DNA Replication (Topoisomerase II” DNA gyrase” found mainly in Gram-negative bacteria: (Quinolones) . Inhibitors of Transcription (DNA-dependent RNA polymerase): (Rifampicin). Used mainly in tuberculosis & other infections. Pharmacology of Pathogens Infections/ Classification Inhibitors of Translation (bind to bacterial ribosome and Inhibit protein biosynthesis): Drugs bind to 30 S ribosomal subunit : Aminoglycosides, spectinomycin, and Tetracyclines Drugs bind to 50 S ribosomal subunit: Macrolides, Chloramphenicol, Lincosamines, streptogramins and oxazolidines. They are effective against both Gram-positive and Gramnegative bacteria with a wide clinical uses. Complete inhibition of protein synthesis is not sufficient to kill the bacteria. Therefore, all of them are bacteriostatic, except the Aminoglycosides. They are not selective drugs since they affect mammalian mitochondrial ribosome. Pharmacology of Pathogens Infections/ Classification Inhibitors of bacterial and mycobacterial cell wall synthesis: Inhibitors of Murein monomer synthesis: Cycloserine, Bacitracin and Fosfomycin. Inhibitors of Murein polymerization: Vancomycin, and Teicloplanin Inhibitors of polymer cross-linking: Beta-lactams. Antimycobacterial agents: Isoniazid, Ethambutol and Pyrazinamide. Mechanism of Actions of Antibiotics Inhibitors of Folate metabolism 1. Sulfonamides & sulfones inhibit dihydropteroate synthetase. 2.Trimethoprim& Pyrimethamine, inhibit dihydrofolate reductase . Synthesis and Functions of Folic acid Folate synthesis begins with the formation of dihydropteroic acid from pteridine and PABA; this reaction is catalyzed by dihydropteroate synthetase. Glutamate and dihydropteroic acid condense to form Dihydrofolic acid (DHF). DHF is reduced to THF by dihydrofolate reductase. THF serve as one-carbon donors in numerous reactions necessary for the formation of DNA, RNA, and proteins. Note that bacteria synthesize folate de novo from pteridine & PABA, whereas humans require dietary folate. Folate synthesis and Function Sulfonamides They were the first modern agents to be used in treatment of infections. They are highly selective drugs, because bacterial growth requires activity of the enzyme that is inhibited by the sulfonamides, whereas mammalian cells do not express this enzyme; therefore, the use of these drugs is relatively free of adverse effects (except in neonates). Sulfonamides Despite the selectivity of sulfonamides, the development of resistance to these drugs has resulted in their diminished use. Resistance can develop because of overproduction of the endogenous substrate, PABA, for the enzyme synthetase. Sulfonamides are usually bacteriostatic drugs with broad spectrum. Because of the high incidence of resistance in the bacterial population, these drugs are rarely used as single drug. Instead, they are commonly used in combination with synergistic drug such as Trimethoprim and Pyrimethamine. Pharmacokinetics Absorption: varies from well absorbed (sulfamethoxazole and sulfadiazine) to poorly absorbed (Sulfasalazine). Distribution: they distribute throughout body fluids including cerebrospinal fluid (CSF). The absorbed drugs can displace bilirubin from binding sites on serum albumin leading to kernicterus (Jaundice) in newborns. Elevated concentration of free bilirubin in the blood can lead to brain damage. Pharmacokinetics Metabolism: They are mainly acetylated, and the acetylated metabolite has low solubility in urine leading to crystallization. Excretion: The largest fraction of the acetylated metabolite is excreted in the urine. The acidic urine can reduce its solubility and may precipitate causing crystaluria. Adverse Effects of Sulfonamides Crystaluria: characterized by hematuria and proteinuria; it is treated by large volume of fluids and alkalinization of urine. Newer Sulfonamides (long acting drugs) such as Sulfisoxazole and sulfadoxine are more soluble in urine. Haemolytic anaemia (in persons with G-6-PDH deficiency). Skin sensitization (Stevene-Johnson syndrome or erythema multiform- life threatening reaction).large doses may cause this serious hypersensitivity. Skin condition in which cell death causes the epidermis to separate from the dermis. Therapeutic uses of Sulfonamides Sulfonamides are preferred drugs for treatment of acute uncomplicated urinary tract infections (UTI) caused by susceptible E. Coli. Combination with Trimethoprim (Cotrimoxazole) is always more effective in UTI. Combination of Sulfadiazine and Pyrimethamine is effective in treatment of toxoplasmosis (parasitic infection). Therapeutic Uses of Sulfonamides Sulfasalazine is used in treatment of ulcerative colitis. It is hydrolyzed by colonic bacteria to sulfapyridine (antibacterial agent) and 5-aminosalicylic acid (anti-inflammatory agent). Sulfamethoxazole is used in treatment of pneumonia, enteritis and urithritis. Sulfamethoxazole-Trimethoprim Combination (Co-Trimoxazole) A synergistic effect is obtained from this combination since these two antibacterial agents act on sequential steps in the pathway of folic acid formation. In order to obtain an optimal ratio of plasma concentration (20/1), needed for the synergistic effect, the two agents must be administered in a ratio of (5 S/1 T). Therapeutic Uses of Co-Trimoxazole UTI: treatment of uncomplicated lower UI with this combined product is highly effective. Bacterial respiratory tract infections (chronic bronchitis, otitis media and pneumonia caused by pneumocystis carinii). GIT infections (Typhoid fever & shigellosis). Adverse Effects of Co-Trimoxazole Similar to sulfonamides. A possible teratogenic effect like all antifolate drugs). Sulfones (Dapsone) They are used in treatment of leprosy and pneumonia caused by pneumocystis carinii. Synergistic effects can be obtained when they combined with Trimethoprim. They produce haemolytic anaemia and methemoglobinemia in patients with G-6-PDH deficiency. Inhibitors of DNA Replication, Transcription and Translation • These processes are generally similar in bacteria and humans. However, there are important differences in biochemistry of bacterial and human central dogma processes, and these differences can be exploited for the development and clinical uses of antibiotics. Three such differences are targeted by some antibacterial drugs: • Topoisomerases, which regulate supercoiling of DNA and mediate segregation of replicated strands of DNA. • RNA polymerases, which transcribe DNA into RNA. • Ribosomes, which translate mRNA into protein. Inhibitors of Topoisomerases: Quinolones • Fluoroquinolones are potentially synthetic broad spectrum antibacterial agents. • They are related to Nalidixic acid, but they have broader spectrum of activity with less frequent development of bacterial resistance. Mechanism of Action of Quinolones (Inhibition of DNA Gyrase) The two strands of double helical DNA must be separated to permit DNA replication or transcription. However, anything that separates the strands results in “overwinding” or excessive positive supercoiling of the DNA in front of separation. To combat this mechanical obstacle, the bacterial enzyme (DNA Gyrase) is responsible for the continuous introduction of negative supercoils into DNA. This is an ATP-dependent reaction that requires that both strands of DNA be cut to permit passage of a segment of DNA through the break; the break is then resealed. DNA Replication Mechanism of Action of Quinolones (Inhibition of DNA Gyrase) The DNA Gyrase of E.coli is composed of two A-subunits and two B-subunits. The Asubunits, which carry out the strand cutting function of the gyrase , are the site of action of (Quinolones). These antibiotics inhibit Gyrase mediated DNA supercoiling at a concentration that correlate well with those required to inhibit bacterial growth. Mechanism of Action of Quinolones (Inhibition of DNA Gyrase) Mammalian cells do not contain DNA Gyrase. However, they do contain a similar type of DNA topoisomerase that removes positive supercoils from eukorytic DNA to prevent its tangling during replication. Quinolones inhibit this type of enzyme only at much higher concentrations. Classification of Quinolones Generation FIRST SECOND THIRD FOURTH Agent Nalidixic acid Enoxacin Norfloxacin Lomefloxacin Ciprofloxacin Ofloxacin Pefloxacin Gatifloxacin Levofloxacin Moxifloxacin Sparfloxacin Trovafloxacin Spectrum Gram Negative Site of infection Urinary tract Gm (+) , (-) Gm(-) P. aeruginos Gm(+)/ chlamyd. Urinary tract Systemic Systemic Gm (+) , (-) Gm (+) , (-) Gm (+) , (-) Atypicals Gm (+) , (-) Atypicals Anaerobes Systemic,UT Systemic,UT Systemic,UT Systemic,UT Systemic, Urinary tract Antibacterial Activities of Quinolones They are highly active against wide range of Gram negative( they have DNA gyrase) and some of the agents have lower activity against Gram-positive (They have Topoisomerase IV). They do not have activity against anaerobes (Except Sparfloxacin and Trovafloxacin). They have activity against Ps.auroginosa (Ciprofloxacin is more potent than Norfloxacin). They have good tissue penetration, which is advantage for deep-seated infections. Pharmacokinetics of Quinolones They are rapidly but variably absorbed with peak concentration achieved in about 2 hours. Food may decrease absorption, and Al- or Mgcontaining antacids inhibit absorption. Bioavailability = 50-95% after oral dose. Elimination half-life = 3-4 hours for ciprofloxacin, and 10-11 hrs for Pefloxacin and others. Metabolism by liver & excretion by bile &/or urine. Some of Quinolones are predominantly excreted by kidneys (Ciprofloxacin, Ofloxacin), while others are predominantly cleared by hepatic system (pefloxacin ) Therapeutic uses of Quinolones UTI (caused by multiple resistant bacteria). Prostatitis (Norfloxacin & ciprofloxacin are used. Sexually transmitted diseases (STD): Quinolones are active in N.gonorrheae, urethritis and cervicitis. They are ineffective against Treponema Pallidum(Syphilis). Respiratory tract infections: They are effective in bacterial bronchitis (Hemophilus ,& enteric Gram-negative).They are more active than the standard therapy against S.pneumoniae. Therapeutic uses of Quinolones Bacterial enteric infections: Shigellosis, Salmonellosis, traveler’s diarrhea, and biliary tract infections. Bacterial endocarditis and meningitis: Ciprofloxacin is more effective than synergistic active combination of aminoglycosides and Beta- Lactams in treatment of pseudomonal endocarditis Skin & soft tissues infections: Ciprofloxacin is used. Adverse Effects of Quinolones GIT symptoms: N.V., abdominal discomfort and anorexia. CNS reactions: mild headache, dizziness, followed by sleep disturbances or mood alteration. Seizures are reported in small number of patients (mechanism is associated with the ability of these drugs to inhibit the specific binding of the inhibitory neurotransmitters GABA” to synaptic membrane). Hypersensitivity: (skin rashes followed by pruritis). Photosensitivity: Only halogenated derivatives (Sparfloxacin and lomefloxacin ) can produce this effect. Adverse Effects of Quinolones Arthropathy (Cartilage damage and tendon rupture): Because of the potentiality for this toxicity in growing children, these drugs should not be used in Children. Laboratory tests abnormalities: Abnormal laboratory values associated with the Quinolones include: eosinophilia, leukopenia, neutropenia & elevation of liver enzymes. Adverse Effects of Quinolones Second generation Flouroquinolones (ciprofloxacin) interact with Theophylline by decreasing its clearance, which leads to Theophylline toxicity. Co-administration of thioridazine (antipsychotic agent) with ciprofloxacin increases the risk of Cardiotoxicity. Inhibitors of Transcription: Rifamycin derivatives Rifampicin and Rifabutin are two semisynthetic derivatives of naturally occurring Rifamycin B. Although Rifampicin can be used for prophylaxis of meningitis and for treatment of some other bacterial infections, its major use is in treatment of TB and other mycobacterial infections. Antibacterial activity of Rifampicin It is a large lipid-soluble molecule that is bactericidal for microorganisms such as staphylococcus aureus, Neisseria meningitides, Haemophilus influenzae, Mycobacterial tuberculosis, Chlamydiae and certain viruses. Mechanism of action of Rifampicin Rifampicin binds strongly to β-subunit of bacterial DNA-dependent RNA polymerase and thereby inhibits RNA synthesis. Resistance results from any one of several possible point mutations in rpoβ, the gene for the β- subunit of RNA polymerase. Rifampicin displays high selectivity for bacteria, as mammalian polymerases are inhibited by Rifampicin only at far higher concentrations. Hence, Rifampicin is generally well tolerated, and the incidence of adverse effects is low. Bacterial Transcription Gene expression begins with transcription, which involves the synthesis of single stranded RNA transcripts from DNA template. Transcription is catalyzed by the enzyme RNA polymerase. The process of transcription occurs in 3 stages: Initiation, elongation and termination. The RNA polymerase enzyme differs between bacteria and humans and thus can serve as a selective target for antibacterial action. Pharmacokinetics of Rifampicin Rifampicin is absorbed orally and widely distributed into many tissues and fluids including CSF. It excreted mainly in bile (enterohepatic cycling), but some of its metabolite (deacetylated) appears in urine, sweat, tears causing harmless orange -reddish discoloration. Clinical uses of Rifampicin Indiscriminate use of Rifampicin for minor infections may favor the widespread selection of Rifampicinresistant mycobacterium and thus deprive the drug of most of its usefulness. Clinical uses of Rifampicin It is used to prevent meningococcal disease in individuals who have had close contact with N.meningitidis-infected patients. It is used in combination with Vancomycin and Gentamycin for the treatment of Staphylococcal endocarditis or Osteomylitis. It is used as alternative to INH for the prevention of TB in HIV-positive persons (when there is a resistance to INH). It is usually combined with INH & Pyrazinamide for the initial treatment of TB. It can be used in treatment of tubercular meningitis, since it can penetrate BBB. Adverse effects of Rifampicin Abdominal symptoms (epigastric distress, nausea and vomiting). Hepatotoxicity: Hepatitis from Rifampicin rarely occurs in patients with normal liver function; however, chronic liver disease, alcoholism , old age and drugs(INH) appear to increase the incidence of severe hepatic problems when Rifampicin is given. Flu-like symptoms (fever, chills and myalgia) as an immune-mediated effect with thrombocytopenia. Teratogenicity (it is contraindicated during pregnancy) Unwanted Effects • Potent induction of CYP450 enzymes that leads to the reduction of half-life of many drugs such as digoxin, & oral anticoagulants. It is more complicated in TB therapy in HIV-infected patients receiving protease inhibitors & reverse transcriptase inhibitors. Inhibitors of Bacterial Translation (Ribosomes) Bacterial protein synthesis: Once the mRNA transcripts are synthesized, these transcripts are translated by the bacterial translational machinery. Although the overall process of translation is similar between bacteria and higher organisms, there are a number of pharmacological differences in the details of the mechanisms. Bacterial 70S ribosome Bacterial Translation Protein Biosynthesis 1. • • • Initiation : 1. Activation of amino acids (first a.a. is methionine). (A.A.)1 + ATP (A.A.)1 –AMP activating enzyme • • 2. Formation of Aminoacyl-tRNA complex. (A.A)1-AMP + tRNA (specific) Synthetase • 3. Transcription of genetic information to mRNA. 30 S/50S initiation factor mRNA +(A.A)1-tRNA1 tRNA1-AA (A.A)1-tRNA1 2. Elongations and Translocation: tRNA2-AA2 tRNA1-AA1 peptide synthetase tRNA2-AA2-AA1 Protein 3. Termination : 1.Formation of polyribosomes. 2.Assembly of amino acids into polypeptides. 3.Cleavage of the t-RNA-polypeptide-ribosome complex. Protein Biosynthesis The ribosome of E.coli has a sedimentation coefficient of 70 S and is composed of a 30S subunit and a 50S subunit. The 70S subunit contains two sites that bind tRNAs during translation: the P or “peptidyl” site, which contains the growing peptide chain and the A or “aminoacyl” site (acceptor site) which binds incoming tRNA molecules carrying the various amino acids. 30S subunit is responsible for faithful decoding of the mRNA message. 50S subunit catalyzes peptide bond formation Protein Biosynthesis Translation can be divided into 3 steps: Initiation (the components of the translation system assemble together). Elongation (the addition of amino acids to the carboxyl end of the growing polypeptide chain, as the ribosome moves from the 5’-end to the 3’-end of the mRNA that is being translated. Termination (proteins called release factors recognize the termination codon in the A site and activate discharge of the newly synthesized protein and dissociation of the ribosome-mRNA complex). Considerations Three considerations should apply to these drugs: Translation inhibitors target either 30S or 50S subunit of bacterial ribosome. Complete inhibition of protein synthesis is not sufficient to kill the bacteria. Bacteria can generate a number of responses to various growth-stifling treatments that allow them to remain dormant until the treatment is removed. As a result, most protein inhibitors are bacteriostatic, except aminoglycosides. Selectivity: In addition to their inhibitory effect s on bacterial ribosomes, these drugs can affect mammalian mitochondrial and/or cytosolic ribosomes. Inhibition of host ribosomes is one common mechanism by which these drugs cause adverse effects. For some antibiotics, such as Chloramphenicol, inhibition of mammalian ribosomes represents serious (lethal) toxicity. Certain other antibiotics exhibit little or no inhibition of mammalian ribosomes at clinically relevant concentrations (dose limiting toxicity). Pharmacology of Protein Inhibitors Drugs targeting the 30S ribosome: Aminoglycosides Tetracyclines Spectinomycin Drugs targeting the 50S ribosome: Macrolides Chloramphenicol Lincosamides Streptogramins Oxazolidinones. Aminoglycosides Streptomycin (first one discovered). Neomycin Kanamycin Tobramycin (most widely used) Paromomycin Gentamicin (most widely used) Netlimicin Amikacin (most widely used). Antibacterial Activity Aminoglycosides are used mainly to treat infections caused by Gramnegative bacteria, including Pseudomonas aeruginosa . Pharmacokinetics They have a hexose nucleus, either streptodine or deoxystreptamine to which amino sugars are attached by glycosidic linkages. The amino groups are highly basic and ionized, which can determine many of their pharmacokinetic properties. They are poorly absorbed from GIT and must administered Pareneterally. They are not metabolized, and their excretion by the process of GF. They have limited tissue penetration (accumulate in renal cortex and inner ear). Monitoring of plasma levels is required step in therapy. (2ug/ml for Gentamicin; 10 ug/ml for Amikacin are associated with Nephrotoxicity). Mechanism of Action Aminoglycosides bind to 30S subunit and elicit concentration-dependent effects on protein synthesis. At low concentrations, they induce ribosomes to misread mRNA during elongation, leading to synthesis of proteins containing incorrect amino acids; i.e. aminoglycosides interfere with mRNA decoding function of the 30S subunit. At higher concentrations, aminoglycosides completely inhibit protein synthesis. They stimulate tRNA movement in the opposite direction (reverse translocation); where the ribosomes become trapped at AUG start codons of mRNA. Accumulation of these abnormal initiation complexes stops the translation. Pharmacological Aspects In contrast to other protein inhibitors, AGs are bactericidal. The cell death induced by aminoglycosides is due to: The aminoglycosides-induced misreading leads to synthesis of aberrant proteins that insert into cell membrane causing the formation of membrane pores, which allow the drugs to flood the cell and stop protein synthesis completely. As a result, the damage to the membrane cannot be repaired, and leakage of ions and larger molecules leads to cell death. Aminoglycosides act synergistically with Beta-lactam antibiotics; thereby this combination is commonly used in severe infections. The inhibition of cell wall synthesis (by beta-lactams) increases the entry of aminoglycosides into the bacteria. Single daily doses of Aminoglycosides are as effective as and no more toxic than multiple daily doses. Single daily dosing may be less nephrotoxic and ototoxic than more frequent dosing. Since Aminoglycosides uptake across proximal renal cortical tubular cells and inner ear are saturable. The magnitude of rapid killing effect and duration of the postantibiotic effects of aminoglycosides are proportional to the peak concentration at the site of infection; i.e. the higher the peak concentration, the more pronounced these effects. Giving aminoglycosides as single daily dose results in higher peak tissue concentration than if the total daily doses were divided and given more frequently. Mechanism of Resistance The clinically most common, is the plasmidencoded production of transferase enzyme or enzymes that inactivate aminoglycosides by adenylation, acetylation or phosphorylation. Both amino and hydroxyl groups may be subject to the enzymes attack (The metabolites formed have reduced or no antibacterial activities). Alteration in permeation or transport of AGs. Receptor on 30 S ribosomal subunit may be altered or deleted as a result of chromosomal mutation. Therapeutic Uses Gentamicin, Amikacin and Tobramycin: They are used in serious infections due to aerobic Gram-negative bacilli including Pseudomonas aeruginosa. They are used in treatment (with penicillins) of serious infections (bacterial endocarditis). Streptomycin: It is used in treatment of plague and multiple drug-resistant TB. Neomycin: It is used in empirical treatment of superficial infections of skin. Netlimicin: It is usually reserved for bacteria resistant to other aminoglycosides. Adverse Effects Ototoxicity (manifesting as either auditory or vestibular damage). The aminoglycosides can accumulate in the perilymph and endolymph of the inner ear, and at high concentrations, to damage highly sensitive hair cells. , these antibiotics may cause the following disturbances when they are administered for one month or longer: (Impairment of hearing” deafness” and disturbance of equilibration). Nephrotoxicity can be manifested as a result of drug accumulation in proximal tubular cells Neuromuscular blockade; at very high concentrations, aminoglycosides can produce NM blockade, potentially causing respiratory paralysis. This effect is thought to result from drug competition with calcium at presynaptic sites, leading to reduction in Ach release, failure of the postsynaptic end-plate to depolarize, and muscle paralysis. Tetracyclines and Glycylcyclines Chlortetracycline Tetracycline Oxytetracycline Demeclocycline Methacycline Doxycycline Minocycline (more lipophilic drug). Tigecycline(Glycylcyclines derivative). Tetracyclines Tetracyclines are broad-spectrum, bacteristatic antibiotics that are used widely in treatment of infections. There are minor differences in clinical efficacy of Tetracyclines that are related largely to the pharmacokinetical properties. Mechanism of Action Tetracyclines bind reversibly to the 30S subunit and inhibit protein synthesis by blocking the binding of aminoacyl- tRNA to the A site on the mRNA-ribosome complex. This action prevents the addition of further amino acids to the nascent peptide. The high selectivity of Tetracyclines derives from active accumulation of these drugs in bacteria but not in mammalian cells. Mechanism of Action Tetracyclines enter Gram-negative bacteria by passive diffusion through porin proteins in the outer membrane, followed by active transport across the inner cytoplasmic membrane. Uptake into Gram-positive bacteria occurs similarly via the energydependent transport system. In contrast, mammalian cells lack the active transport system found in bacteria. Mechanism of Resistance Plasmid-encoded Efflux pumps represent the most important mechanism in Tetracyclines-resistant bacteria. Production of proteins that interfere with the binding of tetracycline to the ribosome. Enzymatic inactivation of Tetracyclines. Antibacterial Activity The Tetracyclines possess a wide range of antimicrobial activity against aerobic and anaerobic Gram-positive and Gram-negative bacteria. They also are effective against some microorganisms such as Rickettsiae, Mycoplasma, Chlamydia and Plasmodium. Tetracyclines are bacteriostatic drugs. Pharmacokinetics Most of the Tetracyclines are incompletely and irregularly absorbed from GIT. The % of an oral dose is absorbed: • Chlortetracycline (oral) 30% • Demeclocycline (oral) 60-80% • Doxycycline (oral & paraenteral) 95% • Minocycline (oral) 100% Absorption of Tetracyclines is impaired by the concurrent ingestion of food(dairy products) or medications(antacids) containing calcium & divalent or trivalent cations. The mechanism responsible for the decreased absorption appears to be chelation of these cations and Tetracyclines (as chelating agents). Pharmacokinetics Tetracyclines distribute widely throughout the body and into tissues and secretions including prostate. They accumulate in the liver, spleen, bone marrow and in bone and enamel of the teeth. Tetracycline cross the placenta and enter the fetal circulation. Relatively high concentration is found in breast milk. Pharmacokinetics Absorbed Tetracyclines are excreted mainly in the bile and urine, with the urine (G.F.) being the primary route for most tetracycline except Doxycycline. The renal clearance of Tetracyclines ranges (10-90% ml/min): Oxytetracycline 90 ml/min. Chlortetracycline 30 ml/min. Minocycline 9 ml/min. (Longer half life) Doxycycline can be used in renally compromised patients, because it is preferentially excreted via the bile. Therapeutic uses Rickettsial infections (e.g. Rocky Mountain spotted fever is characterized by fever, chills, and aches in bones and joints). Mycoplasma infections (pneumonia , common in people who live in close contact. Chlamydial infections (non-gonococcal urethritis, pelvic inflammatory disease, pneumonia, hepatitis). Therapeutic Uses Bacillary infections ( Brucellosis and Cholera) caused by brucella species and vibrio cholera. ( Doxycycline is preferred). Spirochetal infections (Lyme disease) transmitted by bite of infected ticks, results in skin lesion, headache, &fever followed by meniningoencephalitis and arthritis. (Single dose of Doxycycline can prevent the development of the disease.) UTIs (Tetracyclines are useless in UTIs caused by Proteus and Pseudomonas). Therapeutic Uses Acne: benefits have been produced by small doses by inhibiting proproni bacteria, which reside in sebaceous follicles and metabolize lipids to irritating FFAs, causing skin irritation & gland Inflammation . (Minocycline is used). Demeclocycline inhibits renal action of ADH and is used in patients with ADH-secreting tumors. Adverse Effects Gastrointestinal disturbances (epigastria burning, abdominal discomfort, nausea and vomiting). Overgrowth of Candida in vagina or Staphylococci in GIT may occur. PMC caused by overgrowth of clost. difficle (few cases). Adverse Effects Photosensitivity: Demeclocycline, Doxycycline may produce mild to severe reactions in the skin of treated patients exposed to sunlight. This effect appears to be as a result from the absorption of UV radiation by the drug following their accumulation in the skin. The activated drug then emits energy at a lower frequency that damage skin tissue leading to erythema. Adverse Effects Permanent staining of developing teeth (Brownish discoloration) , hypoplasia of the teeth, and retardation of bone growth can occur if Tetracyclines are given after 4th month of gestation or to children less than 8 years of age. When given over long periods, use of these drugs can result in a negative nitrogen balance, which may lead to elevated blood urea nitrogen (BUN) “ Nephrotoxicity”. Adverse Effects Hepatic toxicity develops in pregnant women receiving high doses, especially if they were experiencing pyelonephritis. Expired Tetracyclines also cause Hepatotoxicity. Vestibular problems (dizziness, nausea and vomiting) occur with Minocycline or doxycycline which concentrates in the ear and affects function. Tigecycline It has a very broad spectrum. Many tetracycline-resistant strains are susceptible to Tigecycline. Methicillin-resistant staphylococci, Vancomycin-resistant staphylococci, penicillin-resistant streptococci, Vancomycin-resistant enterococci, multidrug resistant enterobacteriaceae, atypical bacteria such as Rickettsiae, Chlamydia, and rapidly growing mycobacteria. Its tissue and intracellular penetration is excellent; consequently its volume of distribution is large. Elimination is primarily biliary. Tigecycline In addition to the tetracycline's adverse effects, tigecycline's chief adverse effect is nausea and occasionally vomiting. Tigecycline is approved for I.V. treatment of skin and skin-structure infections, abdominal infections and community-acquired pneumonia. Antibacterial drugs targeting the 50 S subunit (Macrolides and Ketolides) Macrolides are named for their large lactone rings. Attached to these rings are one or more deoxy sugars. Erythromycin (14 member lactone ring) Clarithromycin (14 member lactone ring) Azithromycin ( 15 member lactone ring) Telithromycin (ketolides with 14 lactone ring). Macrolides Macrolides They are proven to be especially important in the treatment of pulmonary infections, including Legionnaires’ disease. These drugs display excellent lung tissue penetration and they have intracellular activity against legionella and other microorganisms Mechanism of Action Macrolides are bacteriostatic agents that inhibit protein synthesis by binding reversibly to the 50S ribosomal subunits of sensitive bacteria. They appear to inhibit the translocation step wherein the newly synthesized peptidyl tRNA molecule moves from acceptor (A) site on the ribosome to peptidyl (P) or donor site. Alternatively, Macrolides may bind and cause a conformational change that terminates protein synthesis by indirectly interfering with transpeptidation and translocation. Mechanism of Resistance Efflux of drug by active pump mechanism (e.g. Staphylococci, streptococci). Production of methylase enzyme that modifies the ribosomal target, leading to decreased drug binding. Hydrolysis of Macrolides by esterases produced by enterobacteriaceae. Erythromycin Antibacterial activity: Erythromycin is effective against Grampositive organism, in addition to the Mycoplasma, Chlamydia, Rickettsiae, Helicobacter & certain mycobacterium. Pharmacokinetics Erythromycin base is destroyed by acid, and must be administered with enteric coating. Stearates and esters are acid-resistant and well absorbed (Esteolate is the best). The absorbed drug is distributed widely except cerebrospinal fluid. it can cross the placental barriers. These drugs are excreted mainly in the bile (50X higher than blood). Clinical Uses They are the drugs of choice in the followings: Corynebacterial infections (Diphtheria, Sepsis). Chlamydia infections (Respiratory, Genital). Mycoplasma infections (Pneumonia). They are most useful alternative to Penicillins in Gram-positive infections that are sensitive to Penicillins (when there is allergy). Adverse Effects G.I.T. disturbances; N.V.D., mild epigastric pain, and diarrhea (as a result of irritating effects on GIT). Liver toxicity: acute cholestatic hepatitis (fever, Jaundice, Impaired liver function) as hypersensitivity reactions( with Esteolate only). Hypersensitivity: fever, eosinophilia and rashes. Inhibition of CYP450 isoenzymes: Erythromycin metabolites can inhibit certain CYP450 isoenzymes in the liver, & thus increase plasma concentration of numerous drugs (oral anticoagulants , digoxin, and theophylline) that are also metabolized by these hepatic enzymes. They can also increase the concentration of terfenadine causing serious cardiac arrhythmias. Clarithromycin It is a derivative of erythromycin, with similar spectrum of activity and clinical uses, but more consistent absorption and longer half life. The spectrum of activity is the same as that of erythromycin comprising most Gram-positive bacteria, Mycoplasma, Chlamydia & some Gram-negative bacteria. Clarithromycin is more acid stable than erythromycin and therefore is better absorbed. Almost complete oral absorption occurs. It is widely distributed throughout the body. It is 80% bound to plasma proteins (alpha-1 acid glycoprotein). Clarithromycin is eliminated both by renal excretion (40%) and hepatic metabolism (60%). Clinical Uses of Clarithromycin 1. Streptococcal Pharyngitis. 2. Sinusitis. 3. Community acquired pneumonia. 4. Atypical pneumonia. 5. Others: Clarithromycin has been used successfully in Combination with Omeprazole for eradication of Helicobacter pylori in PUD. Azithromycin Antibacterial activity: Azithromycin is active against many aerobic & anaerobic Gram-positive bacteria. Because of its ability to cross the outer membrane of some Gram-negative species (Unlike other Macrolides), it inhibits a number of aerobic & anaerobic Gram-negative bacilli (H.influenzae & certain enterobacteriaceae) . Azithromycin is also active against intracellular pathogens such as mycoplasma, Chlamydia and salmonella ( this is due to great penetration of Azithromycin to the phagocytic cells" macrophages and polymorphonuclear leukocytes”). Pharmacokinetics Azithromycin has an enhanced acid stability in the stomach. Absorption is reduced by about 50% by the presence of food in the stomach, and peak serum levels are reduced by antacids containing (Al) or (Mg). The initial decline in plasma levels is due to rapid and extensive distribution of the drug into the tissues including phagocytes. Drug in phagocytes is transported to the sites of infection by chemotactic mechanisms, and is then released, a process, that is enhanced on exposure of the cell membrane to bacteria. Pharmacokinetics It is widely distributed throughout the body. High concentration is found in prostate, pulmonary tissues, gastric mucosa, liver, and gynecological tissues, even 4-5 days after single dose. The terminal elimination phase of Azithromycin is due to hepatic metabolism, & biliary excretion. The t ½ of this phase is about 40-60 hrs. This long t ½ allows once-daily dosing. Therapeutic Uses Upper and lower respiratory tract infections (Pharyngitis, sinusitis, bronchitis, atypical pneumonia). Skin and soft tissues infections. Sexually transmitted diseases (genital Chlamydia infections). (Single dose has been found to be very effective in treating these infections, because single dose of Azithromycin produces high and sustained levels in gynecological tissues up to 96 hours after administration) Eradication of Helicobacter pylori, in combination with antiPUD Telithromycin It is a semisyntheic 14-membered-ring Macrolides (3-keto group is added), with broad spectrum activity. It has a mechanism of action similar to that of Macrolides, but with a higher affinity for the 50S subunit due to its ability to bind additional components of 50S. This higher affinity allows the use of Telithromycin in treating infections due to certain bacteria that are resistant to Macrolides. Telithromycin Oral bioavailability, tissue and intracellular penetration are good. Telithromycin is metabolized in the liver and eliminated by a combination of biliary and urinary routes of excretion. It is administered as a once-daily dose. Telithromycin is indicated for treatment of respiratory tract infections, including communityacquired pneumonia, chronic bronchitis, sinusitis and Pharyngitis. Like erythromycin, Telithromycin is a reversible inhibitor of CYP450 and can be involved in numerous drug-drug interactions. Chloramphenicol • It is a bacteriostatic broad-spectrum antibiotic that is active against both aerobic and anaerobic Gram-positive and negative bacteria. The most highly susceptible organisms include H. influenzae, Neisseria meningitides and some Bacteroides. Chloramphenicol The potential for serious toxicity has limited the systemic use of Chloramphenicol. The drug is still used occasionally in treatment of meningitis and Rickettsial infections, but only when safer alternatives are not available, as in the case of resistance or serious drug allergy. Chloramphenicol binds to 23S fraction of 50S subunit and inhibits peptide bond formation, apparently by occupying a site that interferes with proper positioning of the aminoacyl moiety of tRNA in the A site. Pharmacokinetics Absorption: mainly by Jejunum Distribution: Diffuses to all fluids (including CSF), cross the placenta. Metabolism: Glucuronic acid conjugation by Glucuronide transferase. Excretion: Mainly enterohepatic cycling, and Renal (Fraction). Mechanism of Resistance Resistance is mainly developed as a result of spread of plasmid-encoded acetyltransferases that inactivate the drug. Clinical Uses Because of potential toxicity and bacterial resistance, this drug is almost obsolete, except for the following treatments: Anaerobic infections (brain abscess, intraabdominal abscess caused by Bacteroides fragilis) Bacterial meningitis caused by H.influenzae. Topical treatment of eye infections due to good penetration to ocular tissues and aqueous humor. Adverse Effects The mechanism underlying the toxicity appears to involve inhibition of mitochondrial protein synthesis. Hematological toxicity: Dose related reversible depression of erythropoiesis. Aplastic anemia, a rare but potentially fatal toxicity occurs via an idiopathic mechanism that is unrelated to dose. Baby Gray Syndrome in premature and newborns. Accumulated and toxic level of Chloramphenicol occurs as a result of lacking glucuronic acid conjugation, causing vomiting, flaccidity, hypothermia, gray color respiratory distress and metabolic acidosis. Drug-drug interaction : Chloramphenicol is metabolic inhibitor Lincosamides The major Lincosamide in clinical use is Clindamycin (chlorine substituted derivative of lincomycin (semisynthetic). Antibacterial activity: Many Gram-positive are inhibited by Clindamycin. Clindamycin is highly effective against anaerobic bacteria such as bacteroides. Mechanism of action and Resistance Mechanism of action: Clindamycin inhibits peptide bond formation through interactions with both the A site (like Chloramphenicol) and/or the P site. Mechanism of resistance: Resistance to Clindamycin includes methylation of the binding site on the 50S ribosomal subunit and enzymatic inactivation Pharmacokinetics Clindamycin is absorbed from GIT rapidly and incompletely (Kaopectate interferes with absorption). It penetrates well most tissues including bone. It also concentrates within phagocytic cells, which may offer a therapeutic advantage. It does not penetrate the meninges but pass the placental barrier. It metabolizes in liver, and 90% of the metabolites excreted in the urine. Therapeutic Uses Treatment of serious anaerobic infections (Bacteroides)-mixed infections. It is used in combination with aminoglycosides to treat the penetrating wounds of the abdomen; and infections originating in female GUT (Septic abortion). Treatment of deep seated infections (e.g. Staphylococcal Osteomylitis), because it can penetrate to bones. It has excellent activity topically against Corynebacterium acnes. Adverse Effects Antibiotic-associated colitis is caused by toxigenic Clostridium difficile. This organism is infrequently part of the normal fecal flora but is selected out during administration of oral Clindamycin. It grows to high number in the sigmoid colon and secretes a necrotizing toxin that produces pseudo- membranous colitis (PMC). This potentially fatal complication must be recognized promptly and treated with oral Vancomycin (0.5 gm every 4-6 hours) and/or Metronidazole which is also effective agent. Adverse Effects P.M.C. is characterized by mucosal ulcerations, severe diarrhea, abdominal pain, fever, & mucous and blood in stool. This syndrome may occur several weeks after cessation of drug. For this reason, persons who develop diarrhea during Clindamycin therapy should discontinue use the drug and be closely monitored for Superinfection and colitis. Streptogramins It is a combination of two Streptogramin A (Dalfopristin) and Streptogramin B (quinupristin) in a 30:70 ratio. It is a rapidly bactericidal antibiotic for the most multiple-drug-resistant strains. Mechanism of Action This combined product binds to the P binding site of the 50 S bacterial ribosome, forming stable complex. Thus, they synergistically interrupt protein synthesis. The type A Streptogramin binding causes a conformational change to the 50S subunit, which increases the activity of the type B Streptogramin by a 100-fold. Streptogramin B prevents the elongation of protein chains and causes the release of incomplete peptides. Pharmacokinetics They are rapidly metabolized, with half-lives of less than one hour. It is excreted with its metabolites via biliary system. Therapeutic Uses Its primary use is in the I.V. treatment of infections caused by intracellular Vancomycin-resistant Enterococcus faecium (VRE), since this drug penetrates the macrophages and polymorphonucleocytes easily. The infections caused by VRE include pneumonia, meningitis, and endocarditis. Adverse Effects The principal toxicities are pain at the site of infusion; arthralgia – myalgia syndrome, and hyperbilirubinemia. Because this antibiotic inhibits CYP3A4, concomitant administration with other drugs metabolize by the same CYP450 (Warfarin, diazepam terfenadine, reverse transcriptase inhibitors & cyclosporine) may lead to potential toxicities of these drugs. Linezolid (Oxazolidinones derivative) It was introduce to combat resistant grampositive bacteria, such as Methicillin and Vancomycin—resistant staphylococci, streptococci and enterococci, in addition to Vancomycin-resistant Enterococcus (VRE). It is approved to be used in skin and soft tissues infection and pneumonia caused by the susceptible organisms Mechanism of Action Linezolid appears to work on the first step of protein synthesis, initiation, unlike most other protein synthesis inhibitors, which inhibit elongation.It does so by preventing the formation of the initiation complex, composed of the 30S and 50S subunits of the ribosome, tRNA, and mRNA. Linezolid binds to the 23S portion of the 50S subunit (the center of peptidyl transferase activity), close to the binding sites of Chloramphenicol, lincomycin, and other antibiotics. Pharmacokinetics Linezolid is 100% bioavailable after oral administration and has a half-life of 4-6 hours. It is metabolized by CYP450 yielding two inactive metabolites that are excreted by renal and non-renal systems. Adverse Effects The principal toxicity of Linezolid is hematologicalreversible and mild. Thrombocytopenia, anemia and neutropenia are the most common manifestations in about 3% of treatment courses. Cases of optic and peripheral neuropathy and lactic acidosis have been reported with prolonged therapy of Linezolid. It is neither an inducer nor an inhibitor of CYP450 enzyme but it is a weak, reversible inhibitor of MAO. Enhancement of the pressor effects of symapthomimitics, tyramine-containing foods, and SSRIs were shown to occur.