* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download GI Emergencies
Survey
Document related concepts
Transcript
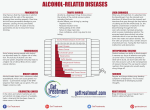
GI Emergencies Core Content Part III Tintinalli Chapters 82-84, 86-87 8 June 2005 GI Emergencies • Hepatic Disorders and Hepatic Failure • Acute and Chronic Pancreatitis • The Liver Transplant Patient Hepatic Disorders and Hepatic Failure • Acute and Chronic Liver Disease • Prevalence of chronic liver disease, cirrhosis and • • • • ESLD steadily increasing Chronic liver disease is 10th leading cause of death among US adults 25,000 deaths yearly=1% all deaths Majority ESLD= alcohol abuse (50%) Increasingly chronic viral hepatitis Epidemiology Hepatitis C • 40% chronic liver dz related to HCV=8-10,000 • • • • • • • deaths yearly By comparison, HIV-related deaths= 14,000 yearly Chronic infection in 85% 70% chronic cases develop chronic liver dz Majority of HCV-infected are 30-49 years old Infection often sub clinical Sxs chronic liver disease/cirrhosis delayed 1020 years Increased risk of HCC Hepatitis C Virus Epidemiology Hepatitis C • Anticipate # of patients with chronic liver dz from HCV to increase sharply over next decades Epidemiology HBV • Effective vaccination has lead to • • • • • decline in prevalence of hepatitis B Still, approximately 140-320,000 new cases yearly 140-320 annual deaths from acute infection Chronic infection occurs in 6-10% 5-6,000 deaths yearly 1-1.25 million Americans with chronic HBV infections Liver tumor from HBV Epidemiology HDV • Hepatitis D virus uncommon • Defective virus-depends on concomitant infection with • • HBV In chronic HBV states, superinfection with HDV results in fulminant liver dz and high mortality Commonly associated with IVDU Epidemiology HAV • Fecal-oral route • 33% Americans have acquired immunity against HAV • • • • secondary to exposure 125-200,000 cases reported annually 100 related deaths Fulminant liver failure is rare Chronic infection does NOT occur Epidemiology Liver dz • LFT abnormalities occur commonly with other acute illnesses – EBV – CMV – HSV – Coxsackie virus • Unlikely to cause clinically evident hepatitis and jaundice in otherwise healthy individuals Epidemiology Liver dz • Alcoholic liver dz and viral hepatitis most acute/chronic cases liver dz • Other causes: – – – – Toxins Idiosyncratic drug reactions Autoimmune Hepatobiliary dzs Causes of Acute Hepatitis • Viral: Hepatitis A, B, C, D, E, CMV • Toxins: – Alcohol – Carbon Tetrachloride – Mushroom poisoning (Ammanita phalloides) • Drugs: – – – – – Acetaminophen Isoniazid Halothane Anesthesia Chlorpromazine Erythromycin Causes of Chronic Hepatitis (>6 months) • Viral: Hepatitis B, C, D • Drugs: – Methyldopa – Amiodarone – Isoniazid • Idiopathic: – Autoimmune features (lupoid hepatitis) – No autoimmune features • Metabolic Liver Disease: – Wilson disease – Alpha-1 antitrypsin deficiency Causes of Chronic Liver Disease and Cirrhosis • • • • Alcohol Hepatitis B and C Drugs: Methyldopa, MTX, Amiodarone Biliary cirrhosis: Primary and Secondary: – – – – – Bile duct strictures Sclerosing cholangitis Biliary atresia Bile duct tumors Cystic Fibrosis Causes of Chronic Liver Disease and Cirrhosis • Chronic hepatic congestion: – Budd-Chiari syndrome – Chronic R sided heart failure – Constrictive pericarditis • Genetic metabolic diseases – – – – Hemachromatosis Wilson’s disease Alpha-1 antitrypsin deficiency Galactosemia Pathophysiology • Hepatobiliary diseases classified according to main • • • • pathologic process involved Hepatocellular Cholestatic Immunologic Infiltrative Clinical Features • Presentation of acute liver disease is variable • Symptoms of hepatocellular necrosis accompanying viral • • hepatitis: anorexia, N/V, low grade fever Cholestatic dz: varying degrees of jaundice, pruritis, clay -colored stools, dark urine Chronic liver dz presents with cirrhosis sxs, portal hypertension: abdominal pain, ascites, GI bleeding, fever, AMS or simply fatigue Historical Features • • • • • • • • • • Sexual behaviors Travel Volume and duration of alcohol use Illicit drug use Consumption of nutritional substances (Vit A) Hx of blood transfusions Needle-stick exposures Herbal remedies Mushroom ingestion Raw oyster consumption Historical Features • • • • Family History: Gilbert’s syndrome Dubin-Johnson/Rotor syndrome Wilson’s dz, hemachromatosis, alpha-1 antitrypsin deficiency Physical Findings • Acute hepatitis findings often limitedmoderate hepatomegaly with TTP • Chronic liver disease: – – – – – – Sallow complexion Appendicular wasting Palmar erythema Distinctive cutaneous spider nevi Parotid gland enlargement Testicular atrophy/gynecomastia • Liver may be enlarged and firm or • Shrunken and nodular in advanced cirrhosis • Splenomegaly, ascites with portal HTN Liver Function Tests • Bilirubin: • Breakdown product of hemoglobin, heme-containing • • • proteins and cytochromes Unconjugated bili poorly soluble anion, bound to albumin Taken in to liver, conjugated, secreted into bile, stool Total serum bili usually < 1.1 and 70% unconjugated Differential Dx of Hyperbilirubinemia • Unconjugated Hyperbilirubinemia >80% indirect: • Overproduction: Hemolysis – Spherocytosis – Autoimmune disorders • Decreased hepatic uptake: – Gilbert’s Sx – Neonatal jaundice – Drug related (Rifampin, contrast agents) • Decreased conjugation: – – – – – Gilbert’s sx Crigler-Najjar sx Neonatal jaundice Hepatocellular dz Drug inhibition-chloramphenecol Differential Dx of Hyperbilirubinemia • Conjugated hyperbilirubinemia > 50% direct • Intrahepatic cholestasis (impaired hepatic secretion) – Familial disorders –Rotor sx, Dubin -Johnson sx, benign recurrent cholestasis – Cholestasis of pregnancy – Drug induced cholestasis (Phenothiazines, OCPs) – Primary biliary cirrhosis – Gram negative sepsis – Post operative • Extrahepatic cholestasis (mechanical obstruction to bile flow) – – – – Common duct gallstones Bacterial cholangitis Tumors Strictures Transaminases • AST derives primarily from liver, also released from heart, smooth muscle, kidney and brain= relatively nonspecific • Meds causing increased AST: – – – – Acetaminophen NSAIDS ACEs Griseofulvin, fluconazole • ALT more specific marker hepatocellular dz • Mild elevations in hundreds/units/liter=ongoing inflammatory hepatocellular damage – Viral hepatitis or subclinical hepatotoxic drugs Transaminases • Values in one thousands suggests acute hepatocellular • • • • • necrosis signifying extensive liver damage=shock liver Value in measuring both enzymes? AST:ALT ratios Ratios>2 common in alcoholic hepatitis AST stimulated by Etoh In acute and chronic viral hepatitis, ratio generally<1 In absence of ongoing Etoh use, mild elevation in AST/ALT with ratio>1 suggests underlying cirrhosis Alkaline Phosphatase • Increased level associated with biliary obstruction and • • • • • cholestasis However mild to moderate elevations accompany virtually all hepatobiliary dz In general, alk phos elevations>4x normal indicate cholestasis rather than hepatocellular process (i.e. hepatitis) Elevations may be nonspecific b/c alk phos derived from bone, placenta, kidneys and leukocytes Specificity increased with GGT (gamma glutamyl transpeptidase) When elevated supports dx of cholestasis Alkaline Phosphatase • GGT, like AST also stimulated by Etoh and drugs= phenobarbital and warfarin • GGT elevated in: – – – – – acute and chronic pancreatitis MI Uremia COPD RA • Isolated elevations in alk phos in absence of hyperbilirubinemia (AP:bilirubin of 1000:1) characteristic of infiltrative or granulomatous dz – – – – Lymphoma Fungal infections Sarcoid TB • Elevated 2-3x adult levels in children Clinical Syndromes • Jaundice = yellow pigmentation to skin, sclera, mucous membranes by elevated bilirubin • Develops w/ overproduction of bili and/or defect in hepatic bili uptake, conjugation or biliary excretion • In absence of underlying or concomitant liver dz hemolysis does NOT result in jaundice Jaundice • In acutely ill or febrile patient, jaundice may be viral hepatitis or bacterial cholangitis • Bacterial cholangitis associated with elevations in alk phos • Subacute jaundice w/o prior liver dz likely infiltrative dz or slowly obstructing extrahepatic tumor (ie head of pancreas) Cirrhosis • Fibrous scarring mixed with hepatocellular regeneration in response to sustained insult – – – – Inflammatory Congestive Metabolic Toxic • Functional anatomy replaced w/ scar tissue • Portal HTN develops… • Complications from ESLD emerge Gastroesophogeal Varices and Hemorrhage • Cirrhosis results in progressive increase in resistance to • • • • • portal blood flow through liver Shunting of blood through venous collaterals into systemic circulation Increased blood flow/pressure in these collateral veins promote formation of submucosal varices in gastric fundus and esophagus Varices prone to ulceration/ hemorrhage 25-70% of cirrhotics will have bleeds Acute hemorrhage carries 30-60% mortality rate Esophageal Varices • Hematemesis, hematochezia, and/or melena • Varying HD instability • Complicated by preexisting thrombocytopenia, anemia, • • • coagulopathy DDX less important than aggressive management Priorities – Airway protection – IV access for meds, fluids, blood Caution w/ central lines-coagulopathies Esophageal Varices • Gastric lavage indicated w/ active bleeding to evacuate • • • • stomach and relieve vomiting Vomiting may exacerbate bleeding May provide gross assessment of ongoing blood loss Known GE varices not a contraindication to careful NG placement GI consult for endoscopy=diagnostic and therapeutic Esophageal Varices • Replace blood, fluids • Vasopressin or somatostatin (special order form and GI • • • • • like this) Decrease portal venous blood pressure, by different mechanisms Vasopressin causes splanchnic arteriolar vasoconstriction, reducing portal venous inflow and pressure Somatostatin decreases splanchnic blood flow by causing direct and selective relaxation of mesenteric vascular smooth muscle Vasopressin action is nonspecific Potential cardiac and HD side effects Esophageal Varices • Vasopressin especially hazardous in older folks • May provoke coronary vasospasm leading to • ischemia, MI, arrhythmias CVA, mesenteric, limb ischemia Esophageal Varices • Somatostatin is effective without significant side effects • Limited by short half life 1-2 min • Octreotide (Sandostatin), an analogue of somatostatin also very effective • Minimal HD side effects • Very useful in HD unstable patients who cannot tolerate emergent endoscopy Esophageal Varices • Sengstaken-Blakemore tube • • • • • for balloon tamponade used infrequently High rate of complications Endoscopy/sclerotherapy more readily available Complications: aspiration, esophageal necrosis or rupture Beta blockers, portosystemic shunts or TIPS (transjugular intrahepatic portosystemic shunts) are effective preventative measures for GE varices No role in acute management Ascites & Spontaneous Bacterial Peritonitis • Ascites occurs in hepatic cirrhosis as a result of portal • • • • HTN, impaired renal sodium and water excretion, hypoalbuminemia Most common complication=SBP Yearly risk= 29% SBP may present w/ fever, abdominal pain and tenderness May be relatively silent w/ subacute functional decline and/or worsening baseline encephalopathy SBP • Diagnosed w/ peritoneal fluid by • • • • • • paracentesis Localize fluid collections by U/S Or percussion of dullness in lateral aspects of lower quadrants w/ pt. semirecumbant Avoid areas near surgical scars Lidocaine, 18-20g angiocath Withdraw 10cc Culture results may be improved by processing fluid like a blood cx SBP • Fever, abdominal pain, tenderness • • • • +/- worsening encephalopathy in pt. w/ cirrhosis and ascites Ascitic fluid: – WBC>1000 mm3 – PMNs>250 mm3 Tx: Cefotaxime 2g IV OR Unasyn, Zosyn, ceftriaxone Ofloxacin 400mg po bid – Enterobacteriacae=63% – Streptococcus pneumoniae=15% – Enterococci= 6-10% Hepatic Encephalopathy • In fulminant liver dz • Occurs in response to metabolic insults and cerebral • • edema May be caused by incompletely metabolized prescription drugs, NSAIDs, tylenol, or Etoh Determining baseline mental status often challenging but central to dx Hepatic Encephalopathy • Serum ammonia often elevated • Nonspecific finding • Ammonia may serve as a marker but NOT as an • • • index of encephalopathy Causes of encephalopathy: – GI bleeding – Increased dietary protein – Infection – Sepsis – Drugs (BZDs, opiates or “muscle relaxers”) Remember the pt. may have fallen Admit, give lactulose or neomycin Hepatic Encephalopathy • Staging of Hepatic Encephalopathy • I: General apathy • II: Lethargy, drowsiness, variable • • orientation, asterixis III: Stupor w/ hyperreflexia, extensor plantar reflexes IV: coma Acute and Chronic Pancreatitis • Acute pancreatitis is secondary to cholelithiasis or alcohol abuse in 90% of cases in US • Biliary pancreatitis most female, over age 50, present to community hospitals • Alcoholic pancreatitis most often male b/w 35-45, present to urban EDs • Other causes pancreatitis: – Drugs – Infection – Trauma • Drugs account for >50% of remaining cases after biliary and Etoh excluded Drugs Associated w/ Acute Pancreatitis • • • • • • OCPs Thiazides Lasix Salicylates Calcium Warfarin • • • • • • Acetaminophen Azathioprine Glucocorticoids Rifampin Tetracyclines Isoniazid Pathophysiology • Intracellular activation of digestive enzymes w/ subsequent autodigestion • Activated proteolytic enzymes (trypsins) cause edema, insterstitial hemorrhage, vascular damage and cellular necrosis • May cause remote systemic effects unlike other intrabdominal processes • May cause shock, ARDS Clinical Features • Major symptom is mid-epigastric or LUQ pain • Usually described as boring, radiating to back and flanks, • • • • • chest or lower abdomen Intensity is variable and does not correlate w/ severity of dz Pain exacerbated by supine position Relieved with sitting, knees flexed Colicky pain suggest other etiology N/V, bloating common PE • Low grade fevers, tachycardia, hypotension • 10 percent have respiratory symptoms secondary to • • • atelectasis, pleural effusion-(usually L sided) Abdominal exam-epigastric TTP Peritonitis is late finding- b/c pancreas RP? Maybe decreased BS from ileus PE • Cullen sign-bluish discoloration around • • • • • umbilicus Grey-Turner Sx-bluish discoloration of flanks Signs of hemmorhagic pancreatitis Rare to find these May present in shock Hypotension from third spacing, hemorrhage, cardiac depression, vomiting Diagnosis • • • • • • • • • No pathognomnic syndrome Diagnostic gold standard is pathologic exam of pancreas Lab and radiographic studies helpful but limited diagnostic accuracy Amylase =digestive enzyme to cleave starch into smaller carbohydrates Found in pancreas, salivary glands and numerous other tissues Poor specificity May be normal in actual cases pancreatitis Levels may return to normal after 3 days b/c of short half life even w/ ongoing inflammation Less sensitive after first 36 hours Diagnosis • Lipase=catalyzes breakdown of triglycerides into free • • • • • • fatty acids Predominantly in pancreas Also in gastric/ intestinal mucosa liver Heparin can cause release of endothelial-membrane bound lipase into serum W/in minutes lipase may increase Lipase cleared renally and may be elevated 3x normal in renal failure ½ life=7h –will remain elevated after amylase returns to baseline Diagnosis • Lipase is a better test • Amylase adds little information • Lipase/Amylase ratios, Amylase/Cr ratio not • helpful It is not cost-effective to order amylase or lipase in every patient w/ undifferentiated abdominal pain Radiology • CXR, AXR may be useful in excluding other causes of abd pain • Pancreatic calcification suggestive of dz • Sentinel loop secondary to small bowel ileus, may be present, but not diagnostic • CXR may show elevated hemidiaphragm or pleural effusion Pancreatic Calcifications Radiology • U/S useful for biliary obstruction, GB dz but insensitive for acute pancreatitis-especially nonbiliary causes • CT cannot r/o dz-insensitive in mild/early cases • ERCP not useful in ED but used later if dx is in doubt Necrotizing pancreatitis Ranson Criteria • • • • • • On Admission: Age over 55 Glucose>200 WBCs> 16,000 AST> 200 LDH>350 • • • • • • 48 hours later: Falling hct> 10% Rise in BUN over 5 mg/dl Decreased Ca below 8 Arterial PO2 below 60mmhg Base deficit over 4meq/L Ranson Criteria • • • • • • On Admission: Age over 55 Glucose>200 WBCs> 16,000 SGOT>200 LDH>350 Lipase is not part of Ranson Criteria • • • • • • 48 hours later: Falling hct> 10% Rise in BUN over 5 mg/dl Decreased Ca below 8 Arterial PO2 below 60mmhg Base deficit over 4meq/L Complications • • • • • • • Pancreatic Abscess Pseudocysts Develop 2-3 weeks after onset Pulmonary: pleural effusions, ARDS CV: Myocardial depression Metabolic: Hypocalcemia, hyperglycemia, hyperlipidemia, Coagulopathy, DIC Treatment • • • • • • GI rest Clear fluids may be ok in mild-mod cases IVFs Narcotics, antiemetics No abx-only if secondary infection suspected Admit all but very mild dz Chronic Pancreatitis • Chronic inflammation causes irreversible pancreatic • • • • • • • damage 80% caused by chronic Etoh abuse Remainder are idiopathic Mean ages of onset of dz=42 Death=52 More common in men (like Etoh abuse) Gallstones are not cause of chronic pancreatitis Acute pancreatitis does not progress to chronic dz unless complications like pseudocysts or ductal strictures present Causes of Chronic Pancreatitis • • • • • • • • Alcohol Abuse Hyperparathyroidism Pancreas divisum Ampullary stenosis CF Hereditary Trauma Idiopathic Clinical Features • Abdominal pain • May be absent in 10% cases • In contrast to acute pancreatitis, may be chronically ill • appearing Pancreatic insufficiency – – – – Weight loss Steatorrhea Clubbing Polyuria • Stigmata of chronic liver dz Diagnosis • Acutely, difficult to discern b/c dx based on dz • • • • • • • reversibility Labs may be nonspecific Amylase/lipase may be elevated, but have no prognostic significance May be normal if fibrosis is advanced Glucose tolerance impaired Increased bili and alk phos Pancreatic calcification on AXR present 30% cases-esp w/ alcoholics No gold standard to differentiate acute v. chronic dz Treatment • Supportive care • r/o other dxs or • • complications Long-term goals=pain control, relief of mechanical obstruction, correction of malabsorption Pancreatic extracts improve absorption and relieve pain Treatment • Etoh cessation is essential • 5 year mortality rate 50% in continued alcohol abusers • Imaging for intractable pain to r/o obstruction or • • pseudocyst Other complications=ascites, pleural effusions, splenic vein thrombosis Celiac plexus nerve block performed for long-term pain control Liver Transplant Patient • 7000 liver transplants worldwide • • • • • • each year 4000 performed in US Number or transplants limited by # of donors Before 1980s, 1 year survival rates < 30% Better immunosuppression, surgical techniques and patient selection 1 year survival=87% Post transplant problems high Postoperative Complications • • • • • • • • Bleeding-most occur in first week, so not seen in ED GI bleeding-manage in usual way May signal graft dysfunction May be accompanied by hypoglycemia, profound coagulapathy Portal HTN should have been reversed by transplant Variceal bleeding may indicate portal vein thrombosis High dose steroids predisposed to GI bleeding CMV, HSV, Candidal infections can cause GI bleeding Biliary Complications • Incidence close to 30% • Leaks, strictures (ductal narrowing), obstruction (ductal • • • • • blockage)=80% of biliary complications Leaks occur early=38% in first 30 days 80% w/in first 6 months Early leaks tend to be more severe Present w/ peritonitis, fever, abdominal pain, distention May be masked from immunosuppression Biliary Complications • Labs = leukocytosis, • • • • • hyperbilirubinemia, increased alk phos Doppler U/S Associated with HAT (hepatic artery thrombosis) Tx for biliary leak includes drainage Abx directed against GNs and anaerobes Biliary leak associated w/ high mortality Vascular Complications • • • • • Less common Associated w/ high morbidity, mortality, graft failure HAT most common-occurs w/in 3 weeks post-transplant Incidence b/w 5-40% Incidence higher in children (26%)-treated w/ anitplatelet agents Vascular Complications • • • • • • Presents w/ increased PT, LFTS Children have more varied presentation May be fever or sepsis Doppler U/S 92% sensitive If U/S not diagnostic but suspicion still highangiography If diagnosed early, immediate thrombectomy and anastomosis revision may preclude need for retransplantation Vascular Complications • Portal vein thrombosis less common= 2-3% of patients • Dx suggested by variceal hemorrhage, massive ascites, other sxs portal HTN • Tx directed towards reducing portosystemic pressure gradient • May need retransplantation Acute Rejection • • • • • Acute rejection usually seen at 7-14 days Incidence =40-80% w/in first posttransplant year After 3 months, incidence declines steadily May be triggered by tapering immunosuppressive agents (have you changed doses of any of your medications lately?) Acute rejection may be subtle presentation – – – – – Fever Liver tenderness Lymphocytosis Eosinophelia Increased LFTs Acute Rejection • Dx only by excluding other causes of graft • • • • dysfunction and bx Perioperative period consider infection, acute biliary obstruction, vascular insufficiency Acute rejection treated w/ high dose glucocorticosteroids w/ rapid taper over 5-7 days Effective in 65-80% Secondary therapy w/ antilymphocyte globulin (OKT3) Chronic Rejection • Occurs in 5-10% of recipients • Major cause of late graft failure • Primary manifestation=persistently • • • cholestatic liver injury pattern (biopsy) Elevated alk phos, bilirubin Associated w/ pruritis Significant loss of hepatic fxn often not evident until late in course of chronic rejection Infection • Account for most death • Most patients have at least one episode • Immunosuppression-induced blunting of inflammatory • response may mask presentation Three major infection periods – <1 month – 1-6 months – >6 months • In first 30 postop days=bacteria and fungi • Immunosuppression at greatest levels, anastamoses at most vulnerable Infection • Most infections <30 days normal • • • • nosocomial agents in post-op patients Opportunistic organisms absent in first month From 1-6 months most infections=viruses EBV from reactivation or donor transmission Or opportunisitic infections Infection • After 6 months, incidence of serious infection declines • Cholangitis most common • High index of suspicion • “Close monitoring is essential, as rapid deterioration can take place while the patient is still in the ED” CMV • • • • • • • Often seen w/ bacterial infections Most common virus affecting patients Occurs b/w 23-85% of all liver transplant patients Despite high incidence and morbidity, rarely fatal unless disseminated Rarely has significant effect on graft survival Generally occurs within first 3 months Peak incidence in first 3-4 weeks CMV • Later CMV occurrence related to increase in • • immunosuppression for tx of prolonged rejection May be primary infection or reactivation Mononucleosis-like syndrome – – – – – Fever Atypical lymphocytosis Thrombocytopenia Neutropenia Mild increase in LFTs • May present w/ pneumonitis • B interstitial infiltrates CMV • CMV pneumonitis may be seen in conjunction w/ PCP • • • • • • pneumonia CMV hepatitis presents similarly to rejection-fever, abdominal pain, hepatomegaly, liver dysfunction Diagnosed by liver bx, but still difficult to distinguish from chronic rejection CMV retinitis-decreased vision, photophobia, floaters, eye pain Signals profound immunosuppression Carries poor prognosis TX: Ganciclovir for 2-4 weeks Question • Which types of hepatitis produce neither an • infection nor a carrier state? Hepatitis A and Hepatitis E Question • What abnormal electrolyte finding is seen in • patients with pancreatitis? Hypocalcemia Question • What is the most common cause of portal HTN worldwide? • Schistomsomiasis Question • What is the most common bloodborne infection • in the US Hepatitis C