* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Embryonic Development and Implantation
Survey
Document related concepts
Transcript
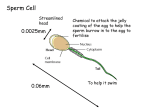
NOTE: This presentation was not made for public use. Please do not use this presentations without my permission and the permission of each of the authors of the photographs, quotes, and other materials that they contain. Thank you, Vicki Hughes Chapter 16: Reproductive System Gonads = primary sex organs (testes and ovaries) Gametes = sex cells (sperm and ova) Roots: Gonad = seed Albu = white Ductus = carrying away Gen = origin Epi = on top of Corp = body Leut = yellow Assignments: OL CH 16 Flashcards treehugger.com Male Anatomy Penis = delivers sperm to vagina Testes = manufactures sperm Epididymis = stores immature sperm Ductus deferens = delivers sperm to penis Seminal vesicle = produces most of fluid carrying sperm Prostrate Gland = secretes milky fluid that activates sperm Bladder Ductus deferens Seminal vesicle Prostate gland Epididymis Spermatogenesis = production of sperm Spermatogenesis occurs in the seminiferous tubules located inside the testes. Immature sperm are stored in the epididymis. Seminiferous tubules http://bio1151.nicerweb.com In the Seminiferous Tubules… 1. Germ cells near the outer wall of the seminiferous tubules of the testis differentiate into stem cells called spermatogonia. 2. Spermatogonia divide by mitosis, and mature into primary spermatocytes. 3. Each primary spermatocyte undergoes meiosis yielding 4 equal-sized spermatids. 4. The spermatids migrate toward the lumen (central opening). 5. Sertoli cells supply nutrients for the spermatids, which mature into motile sperm in the epididymis. Spermatogenesis http://wps.aw.com/bc_martini_eap_4/40/104 69/2680298.cw/content/index.html http://bio1151.nicerweb.com Diseases of the male reproductive system Hydrocele Testicular Cancer Benign Prostrate Hyperplasia Female Anatomy Ovary = location of maturing eggs Fallopian Tubes = provide passage of egg to location for fertilization Uterus = the “womb” where the egg develops into a fetus. Vagina = “birth canal” Oogenesis = production of egg 1. Follicle = saclike structures with one egg each. 2. Oocyte = unfertilized egg 3. FSH = follicle stimulating hormone 4. Ovarian cycle = monthly maturation of a small number of follicles. 5. Produces 2 cells: larger oocyte and smaller polar body. 6. Secondary oocyte grows and bursts from follicle – “ovulation.” 7. Polar body is discarded. http://wps.aw.com/bc_martini_eap_4/40/10 469/2680298.cw/content/index.html http://www.como.wa.edu.au The polar body has no real purpose. Polar body When the body cell undergoes meiosis to produce the egg, ½ of the nuclear material goes into the egg to be fertilized and ½ goes into the polar body. The egg receives the bulk of nutrient rich plasma to provide maximum nutrients in the event of fertilization. The polar body basically “gives up” its plasma and nutrients for the good of the other egg. Diseases of the female reproductive system Endometriosis Ovarian cyst Sexually Transmitted Diseases (STDs) Aids syphilis Gonorrhea Genital Herpes Chlamydia Genital Warts Menstrual Cycle (No Fertilization) Day 1-7 Menstruation (bleeding) Day 8-11 Uterus thickens Day 14 Ovulation Day 18-25 Corpus Luteum fades away Day 26-28 Uterine lining detaches Start over at Day 1 above. Birth Control FEMALE BIRTH CONTROL • Tubal ligation is a surgical procedure in which the uterine tubes are separated. • Tying of the tubes also prevents pregnancy. • Sperm cannot reach the egg and the egg cannot reach the womb. • Hysterectomy is surgical removal of the uterus. Birth Control MALE BIRTH CONTROL • Mature sperm are stored in the epididymides • Vasectomy is a surgical contraceptive procedure whereby the vas deferens are permanently divided, preventing the spermatozoa from leaving the epididymis • Following vasectomy, a man can only ejaculate seminal fluids that are free of sperm cells. Fertilization • Sperm are released into the vagina and move through the cervix into the uterus. • From there sperm move through the fallopian tube to the egg. • Fertilization occurs about 1/3 of the way from the ovary to the uterus. Fertilization • Once a sperm has reached the egg it uses specialized enzymes which break down the egg covering. • The sperm is then absorbed into the egg as the two membranes fuse. Embryonic Development and Implantation Once the egg is fertilized it is called a zygote. Zygote Early Cleavage For the first 0-2 days, the zygote is dividing but not growing. Morula Blastocyst This early division is called early cleavage. Formation of ectoderm, mesoderm and endoderm Gastrula www.msdellasantina.com Embryonic Development and Implantation Early cleavage occurs in the fallopian tube prior to entry into the uterus. www.msdellasantina.com Embryonic Development and Implantation The morula stage is reached in 3 to 4 days. Earlyball Cleavage TheZygote morula is a solid of 16 or more cells. Formation of ectoderm, mesoderm and endoderm Morula Blastocyst Gastrula www.msdellasantina.com Embryonic Development and Implantation The morula enters the uterine cavity, remaining there for 4 to 5 days as it continues to divide into 100 cells or more. www.msdellasantina.com Embryonic Development and Implantation As mitosis continues, a cavity forms within the mass of cells. This hollow ball stage is called a blastocyst, and the cavity is the blastocoel. Early Cleavage Zygote Trophoblast Blastocoel Morula Blastocyst The outer layer of the cells of the blastocyst is called the trophoblast. Formation of ectoderm, mesoderm and endoderm Gastrula www.msdellasantina.com Embryonic Development and Implantation An inner cell mass called the embryoblast will develop. The trophoblast becomes the Early Cleavage fetalZygote portion of the placenta, and the embryoblast becomes the embryo. Formation of ectoderm, mesoderm and endoderm Becomes placenta Becomes embryo Morula Blastocyst Gastrula www.msdellasantina.com Embryonic Development and Implantation Approximately 6 days following ovulation, the blastocyst attaches to the endometrium, usually on the posterior wall. This attachment is called implantation. www.msdellasantina.com During implantation the embryoblast undergoes embryogenesis in which the three primary germ layers - ectoderm, mesoderm and endoderm - are formed. The germ layers give rise to the primary layers of the individual. By the end of two weeks, embryogenesis is complete, and the individual is an embryo. Embryonic Development and Implantation By the end of the 3rd week the human embryo is at the gastrula stage. Zygote Early Cleavage During the gastrula stage one end of the gastrula invaginates (folds into the ball) forming what will Formation of become the gut. ectoderm, Morula Blastocyst Gastrula mesoderm and endoderm www.msdellasantina.com The chorion becomes part of the placenta that houses the growing fetus. The amnionic cavity fills with fluid that cushions the growing fetus. At the beginning of the 5th week, organs, eyes, limbs, and brain are forming. Note: At this stage, all humans have a tail and gills (pharyngeal pouches). This is evidence of our evolutionary ancestry. After the first two months of development, the embryo is called a fetus. Embryo Fetus During the remainder of development there is an enormous increase in size, with weight increasing by a factor of 600. By the end of the first trimester (3 months), sexual differentiation has occurred, the fetus kicks and sucks its thumb; breathing movements bring amniotic fluid in and out of the lungs. By the end of the second trimester, the fetus is 12 inches long, has hair, eyebrows, and eyelashes, and is moving a great deal. The third trimester is a time of maturation of the digestive and respiratory systems. Pregnancy Hormones Three primary hormones Involved in pregnancy: 1. Human chorionic gonadotropin (HCG) 2. Estrogen 3. Progesterone • Following fertilization, HCG is produced by the embryo. • HCG causes corpus luteum to secrete estrogen and progesterone. Estrogen and Progesterone • • • • • stimulate uterine lining to continue development stop the menstrual cycle stimulate the development of mammary glands prevent premature contractions enlarge the reproductive organs Relaxin • relaxes the pelvic ligaments Physicians usually calculate the gestation period, or length of the pregnancy, as 280 days (40 weeks or 10 lunar months) from the last menstrual period (LMP) to the date of confinement, which is the date of delivery of the infant. Parturition refers to the process by which the baby is born. Stages of Parturition Labor occurs in three stages: dilation stage, expulsion stage, and placental stage. • Dilation is the longest stage marked by dilation (widening) of the cervical canal and by effacement (thinning) of the cervix. • Expulsion stage begins when the baby's head enters the vagina and lasts until the baby is entirely expelled. • Placental stage results in expulsion of the placenta, amnion, and other fetal membranes. • Two weeks or so before birth, the fetus "drops"; its head lies against the cervix, which may begin to dilate. cervix • Baby starts the birthing process. When the fetal brain has sufficiently developed, the fetal hypothalamus causes the anterior pituitary to signal the fetal adrenal cortex to release hormones which trigger the uterine contractions that expel the fetus. As the uterus contracts, the baby’s head pushes against the cervix, causing it to dilate. Cervical dilation is the first stage of labor. The amniotic sac may rupture during this stage. This is commonly called “water breaking.” When the cervix has dilated to 10 centimeters, the second stage of labor begins and the baby moves down the vagina. Once the baby is born, the umbilical cord can be cut. The placenta remains in the uterus. The third stage of labor is delivery of the placenta, also called the "afterbirth." Hormonal Control of Lactation The Miracle of Life http://www.pbs.org/wgbh/nova/body/lifegreatest-miracle.html You should now be able to: 1. 2. 3. 4. Distinguish between gonads and gametes. Identify male and female reproductive structures and functions. Describe spermatogenesis and oogenesis. Describe the diseases of the male and female reproductive systems that we studied. 5. Define a polar body. 6. Describe the menstrual cycle without fertilization. 7. Describe types of birth control for males and females. 8. Describe the development of a fetus from fertilization of the egg to implantation in the womb. 9. Describe the steps of parturition. 10. Describe the growth and development of the embryo into a fetus. 11. Discuss the involvement of HCG, estrogen and progesterone during pregnancy. 12. Define gestation and describe how doctors calculate due dates. 13. Describe the hormonal control of lactation. Any questions?