* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Medial Lateral Anatomy - American Orthopaedic Society for Sports
Survey
Document related concepts
Transcript
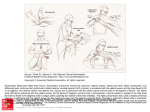
Inside‐out Anatomy and Exposure: Medial and Lateral Anatomy Case‐based Symposium: Management of Meniscus Injuries AOSSM Specialty Day March 5, 2016. Orlando, FL Matthew Matava, M.D. Chief, Sports Medicine Section, Washington University St. Louis, MO I. Patient Positioning Principles o Patient supine with foot of bed flexed 90° in Trendelenburg position preferred o Leg holder around distal thigh to allow varus/varus stress o Contralateral limb abducted (for medial meniscal repair) and flexed in leg holder o Paralysis by anesthesiologist helpful for exposure II. Equipment Headlight for surgical assistant Kocher clamp Needle driver Suture scissors Henning (popliteal) retractor, teaspoon, tablespoon, or pediatric vaginal speculum Cannulated suture guides (single‐ and double‐barrel) in straight and curved options 2‐0 non‐absorbable braided sutures with 10‐inch double‐armed Nitinol needles Meniscal rasp (ball or curved) Kick bucket or basin III. Lateral Meniscal Repair Surface Anatomy and Skin Incision o Surface landmarks a. Lateral joint line b. Lateral collateral ligament c. Lateral epicondyle d. Fibular head o Knee flexed to 90° and a 3 cm vertical incision placed 1/3 above and 2/3 below the lateral joint line o Incision posterior to LCL *Incision should be parallel to the longitudinal axis of the lower extremity with knee extended Deep Anatomy o Subcutaneous dissection down to iliotibial (IT) band o Deep incision between posterior edge of the IT band and anterior edge of biceps femoris short head o “Hockey” stick extension in IT band distally may be needed to facilitate exposure 1 o o o o Fascia posterior to LCL is dissected to level of fibular head Blunt dissection between lateral joint capsule and lateral head of gastrocnemius a. Adhesions may be present between capsule and lateral gastrocnemius *Caution: Perforation of capsule will cause fluid extravasation Common peroneal nerve palpated posterior to biceps femoris but not routinely identified Henning popliteal retractor or spoon placed anterior to lateral gastrocnemius at joint line level to retract the common peroneal nerve posteriorly *Caution: Inferior lateral geniculate artery may be visualized inferiorly and cauterized IV. Medial Meniscal Repair Surface Anatomy and Skin Incision o Surface landmarks a. Medial joint line b. Medial collateral ligament (MCL) c. Medial epicondyle o Knee flexed to 90° and a 3 cm vertical incision placed 1/3 above and 2/3 below the medial joint line o Incision posterior to superficial MCL in‐line with longitudinal axis of knee *Caution: Infrapatellar branch of the saphenous nerve and saphenous vein posterior and inferior to incision Deep Anatomy o Subcutaneous incision through Sartorial (crural) fascia with pes tendons (Sartorius, gracilis, and semitendonosus) reflected posteriorly o Sheath over the direct arm of the semimembranosus is dissected to identify the tendon insertion heading to proximal tibia o Medial head of gastrocnemius deep to and crossing the semimembranosus o Dissection between the inferior surface of semimembranosus and medial head of gastrocnemius *Caution: Deep exposure superior to semimembranosus may result in suture needles passing inferior to popliteal retractor resulting in neurovascular risk o Blunt dissection between the posteromedial capsule and medial gastrocnemius *Caution: Adhesions may be present between capsule and gastrocnemius o Retractor or spoon placed between capsule and gastrocnemius at joint line level V. Suture Repair Technique Positioning and Exposure o Assistant surgeon sits at knee level on side of repair with headlight to facilitate view of needle passage 2 Instrument ‘holster’ (Kocher clamp) clamped at knee level with suture scissors and needle holder contained in finger holes o Kick bucket or basin placed on floor next to seated assistant to drop needles in o Second assistant positioned next to surgeon on side opposite of repair to pass sutures o Knee flexed to 20°‐30° with varus/valgus force applied by surgeon to open the involved compartment o 30° arthroscope placed through either the same or opposite compartment to facilitate viewing while allowing placement of the suture cannula o ‘Pie‐crusting’ of deep MCL with 18‐gauge needle occasionally needed to expose posterior horn of medial meniscus in tight knees Meniscal Suturing o Tear and adjacent synovium braded with meniscal rasp or shaver (without suction) to facilitate fibrovascular healing response o Curved suture cannula brought in from opposite compartment in order to guide needles away from the midline neurovascular structures *Trans‐patellar tendon portal may be useful to pass sutures if the tibial spine blocks cannula passage o Meniscus tear is reduced with the suture cannula, and a 10‐inch suture needle is passed under direct visualization through the meniscus and capsule in a divergent fashion until the needle hits the popliteal retractor o Sutures placed first on the superior meniscal surface to reduce the tear, then on the inferior surface in an alternating pattern o o o The assistant retrieves the needle carefully (Nitinol wire VERY flexible) and the second needle is passed in a similar fashion on the other side of the tear in a vertical mattress configuration *Vertical mattress preferred over horizontal mattress sutures Sutures placed 3‐5 mm apart o Cycle knee multiple times to confirm stability of the repair 3 References Chen N, Martin S, Gill T: Risk to the Lateral Geniculate Artery During Arthroscopic Lateral Meniscal Suture Passage. Arthroscopy. 2007; 23: 642‐646 2. Hoppenfeld S, deBoer P: The Knee, in Hoppenfeld S, deBoer P: Surgical Exposures in Orthopaedics: The Anatomic Approach, ed 2. Philadelphia, PA: JB Lippincott, 1994, pp 467‐476 3. Horner G, Dellon AL: Innervation of the human knee joint and implications for surgery. Clin Orthop. 1994; 301:221‐226 4. Hunter L, Louis D, Ricciardi J, O’Connor G: The saphenous nerve: Its course and importance in medial arthrotomy. Am J Sports Med. 1979; 7:227‐230 5. Jurist K, Greene P, Shirkhoda A: Peroneal nerve dysfunction as a complication of lateral meniscus repair: a case report and anatomic dissection. Arthroscopy.1989; 5: 141‐147 6. LaPrade R, Ly T, Wentorf F, Engebretsen L: The posterolateral attachments of the knee: A qualitative and quantitative morphologic analysis of the fibular collateral ligament, popliteus tendon, popliteofibular ligament, and lateral gastrocnemius tendon. Am J Sports Med. 2003; 31:854‐860 7. McLaughlin J, Noyes F: Arthroscopic meniscus repair: Recommended surgical techniques for complex meniscus tears. Tech Ortho.p 1993; 8:129‐136 8. Medvecky M, Noyes F: Surgical Approaches to the Posteromedial and Posterolateral Aspects of the Knee. J Am Acad Orthop Surg. 2005; 13:121‐128 9. Seebacher J, Inglis A, Marshall J, Warren R: The structure of the posterolateral aspect of the knee. J Bone Joint Surg Am. 1982; 64:536‐541 10. Terry G, LaPrade R: The posterolateral aspect of the knee: Anatomy and surgical approach. Am J Sports Med. 1996; 24:732‐739 11. Watanabe Y, Moriya H, Takahashi K, et al: Functional anatomy of the posterolateral structures of the knee. Arthroscopy. 1993; 9:57‐62 1. 4