* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Pharmacy Prior Authorization Criteria
Survey
Document related concepts
Transcript
SELECT HEALTH
PHARMACY PRIOR AUTHORIZATION
CRITERIA
SEPTEMBER 2016
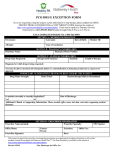
PRIOR AUTHORIZATION PROTOCOL FOR INJECTABLE 5-HYDROXYTRYPTAMINE-3
(5HT3) SEROTONIN RECEPTOR ANTAGONISTS
Formulary Status: Generic Ondansetron or Granisetron Preferred
Aloxi (palonosetron)
Anzemet (dolasetron)
Kytril (granisetron)
Zofran (ondansetron)
Any other newly marketed agent
Criteria for Approval:
The request for the medication is for an Food and Drug Administration (FDA) approved
indication, and/or is used for a medical condition that is supported by the medical compendium
(Micromedex, American Hospital Formulary Service (AHFS), Drug Points , Drug Package
Insert) as defined in the Social Security Act 1927 and/or per the National Comprehensive Cancer
Network (NCCN), the American Society of Clinical Oncology (ASCO), National Cancer
Institute {NCI} (a Division of the U.S. National Institutes of Health) and the Multinational
Association of Supportive Care in Cancer (MASCC) standard of care guidelines for antiemetic
therapy.
•
• Patients receiving an antineoplastic agent =as HIGH or MODERATE emetic risk per the
ASCO Practice guidelines can receive Aloxi® (palonosetron hydrochloride) as a first line
antiemetic agent. (See tables that follow)
For all other patients, if the medication request is for any other 5-hydroxytryptamine-3 (5HT3)
serotonin receptor antagonist other than generic Ondansetron or generic Granisetron, the patient
has a documented (consistent with pharmacy claims data, OR for new members to the health
plan consistent with medical chart history) treatment failure after receiving an adequate trial of
generic Ondansetron or generic Granisetron and/or has another documented medical reason (
intolerance, hypersensitivity, contraindication, etc.) for not utilizing these medications to treat
their medical condition.
•
• Prescribed dosing of the 5HT3 serotonin receptor antagonist is within FDA approved
indications and/or is supported by the medical compendium as defined by the Social Security Act
and/or per the NCCN, ASCO, NCI or MASCC standard of care guidelines.
The medication is recommended and prescribed by a specialist in the field to treat the patient’s
respective medical condition.
•
If all of the above conditions are met, the request will be approved for up to 6 months or as
recommended per FDA approved indications and/or as defined by the medical compendium as
defined above and/or per the NCCN, ASCO, NCI or MASCC standard of care guidelines; if all
of the above criteria are not met, the request is referred to a Medical Director/Clinical reviewer
for medical necessity review.
High
Level
Frequency of Emesis%
>90%
IV Chemotherapy agent
Carmustine, Cisplatin,
Cyclophosphamide ≥1500 mg/m2
Dacarbazine, Dactinomycin,
Moderate
30-90%
Mechlorethamine, Streptozocin
Alemtuzumab, Azacytidine
Belinostat, Bendamustine,
Cabazitaxel, Carboplatin,
Clofarabine,
Cyclophosphamide <1500 mg/m2
Cytarabine >1000 mg/m2
Daunorubicin*, Doxorubicin*
Epirubicin*, Idarubicin*
Ifosfamide, Irinotecan, Oxaliplatin
Low
10-30%
Pralatrexate, Temozolomide
Blinatumomab, Bortezomib,
Carfilzomib,
Cytarabine ≤1000 mg/m2
Dabrafenib, Docetaxel, Eribulin
Etoposide, Fluorouracil,
Gemcitabine, Ibrutinib,
Idelalisib, Ipilimumab, Ixabepilone,
Methotrexate**, Mitomycin
Mitoxantrone, Paclitaxel, Panitumumab,
Pegylated liposomal doxorubicin,
Pemetrexed
Pertuzumab, Romidepsin, Temsirolimus,
Topotecan
Trastuzumab, Ado-trastuzumab
emtansine, Vemurafenib
Minimal
<10%
Vorinostat
Bevacizumab, Bleomycin, Busulfan,
Cetuximab, Cladribine, Fludarabine,
Nivolumab, Obinutuzumab,
Ofatumumab, Pembrolizumab,
Rituximab, Vinblastine, Vincristine,
Vinorelbine
*These anthracyclines, when combined with cyclophosphamide, are now designated as having high emetic risk. **At doses >1
gram, methotrexate has at least moderate emetogenic potential.
Reproduced with updated data from: Basch E, Prestrud A, and Hesketh P, et al. Antiemetics: American Society of Clinical
Oncology Clinical Practice Guideline Update. J Clin Oncol 2011; 29:4189.
Graphic 58756 Version 27.0
Degree of emetogenicity
(incidence)
Oral Antineoplastic Agent*
High (>90%)
Procarbazine
Moderate (30 to 90%)
Altretamine (hexamethylmelamine)
Bosutinib, Busulfan (≥4 mg/day),
Cabozantinib, Ceritinib, Crizotinib, Cyclophosphamide, Imatinib, Lomustine,
Olaparib, Temozolomide,
Tretinoin, Vandetanib
Low (10 to 30%)
Afatinib, Axitinib, Bexarotene, Capecitabine, Dasatinib, Estramustine, Etoposide,
Everolimus, Fludarabine, Ibrutinib, Idelalisib, Lapatinib, Lenalidomide
Lenvatinib, Nilotinib, Palbociclib
Pazopanib, Sunitinib, Tegafur uracil
Thalidomide, Topotecan, Vemurafenib, Vorinostat
Minimal (<10%)
6-Thioguanine, Chlorambucil,
Erlotinib, Gefitinib, Hydroxyurea,
Melphalan (L-phenylalanine mustard),
Methotrexate, Regorafenib, Sorafenib
** Considerable uncertainty prevails for the emetogenic risk of oral agents.
Reproduced with updated data from: Basch E, Prestrud A, and Hesketh P, et al. Antiemetics: American Society of Clinical
Oncology Clinical Practice Guideline Update. J Clin Oncol 2011; 29:4189.
Graphic 58756 Version 27.0
Review Date: 7/2016
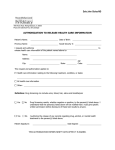
Field Name
Field Description
Prior Authorization Group Desc
Drug(s)
RETINOIDS (DERMATOLOGIC)
Isotretinoin (Amnesteem, Absorica, Claravis, Myorsian, Zenatane) and newly
marketed products
*Medically accepted indications are defined using the following sources: the Food
and Drug Administration (FDA), Micromedex, American Hospital Formulary
Service (AHFS), United States Pharmacopeia Drug Information for the Healthcare
Professional (USP DI) , and the Drug Package Insert).
None
None
None
None
Covered Uses
Exclusion Criteria
Required Medical Information
Age Restrictions
Prescriber Restrictions
Coverage Duration
Other Criteria
If the above conditions are met, the request will be approved for up to a 6 month
duration with generic medication; if the above conditions are not met, the request
will be referred to a Medical Director for medical necessity review
PA CRITERIA FOR APPROVAL:
• Diagnosis of severe recalcitrant nodular acne
AND
• Documented treatment with a therapeutic trial and failure or intolerance to oral
antibiotic therapy first line therapy (e.g. doxycycline, minocycline, tetracycline, and
erythromycin) for at least 4 weeks (28 days) of therapy in the previous 60 days.
NOTE: Clinical reviewer must override criteria when, in his/her professional judgment,
the requested item is medically necessary.
Associated Policy: Prior Authorization of Prescription Drugs 236.200
Review Date: 10/2014
3
Field Name
Field Description
Prior Authorization Group Desc
Drug(s)
ALPHA-1 PROTEINASE INHIBITORS (HUMAN)
Alpha-1 Proteinase Inhibitor (human) (Aralast NP, Glassia, Prolastin®-C,
Zemaira®)
Medically accepted indications are defined using the following sources: the Food and
Drug Administration (FDA), Micromedex, American Hospital Formulary Service
(AHFS), United States Pharmacopeia Drug Information for the Healthcare
Professional (USP DI), and the Drug Package Insert.
None
None
18 years of age or older
Prescriber must be pulmonologist
Covered Uses
Exclusion Criteria
Required Medical Information
Age Restrictions
Prescriber Restrictions
Coverage Duration
The request will be approved for up to a 6 month duration; if all of the above criteria
are not met, the request is referred to a Medical Director for medical necessity review.
Other Criteria
INITIAL AUTHORIZATION:
The member is an adult (≥ 18 y/o) and has a documented diagnosis of a
congenital deficiency of alpha-1 antitrypsin (ATT) [serum level < 11uM or
80mg/dl].
Documentation was submitted indicating the member has undergone genetic
testing for ATT deficiency and is classified as phenotype PiZZ, PiZ(null) or
Pi(null)(null) [NOTE: phenotypes PiMZ or PiMS are not candidates for
treatment with Alpha1-Proteinase Inhibitors].
Documentation was submitted indicating the member does not have selective
IgA deficiency (IgA level < 15 mg/dL) with known antibodies against IgA.
Documentation was submitted (member’s pulmonary function test results)
indicating airflow obstruction by spirometry (eg, FEV1 <80 percent of
predicted)
Documentation was submitted indicating member is non-smoker or ex-smoker
(eg. smoking cessation treatment)
Documentation of the member’s current weight
The Alpha1-Proteinase Inhibitor (human) is being prescribed at an FDA
approved dosage.
If the medication request is for an Alpha1-Proteinase Inhibitor (human) product
other than Prolastin®-C, the patient has a documented medical reason
(intolerance, hypersensitivity, contraindication,treatment failure, etc) for not
using Prolastin®-C to treat their medical condition.
Review Date: 2/2016
PA CRITERIA FOR REAUTHORIZATION:
Documentation of the member’s current weight
Documentation was submitted indicating the member has clinically benefited
from therapy (eg. improved lung function tests {pulmonary function tests}),
alpha-1 antitrypsin serum level maintained above 80 mg/dL, improved quality of
life).
The Alpha1-Proteinase Inhibitor (human) is being prescribed at an FDA
approved dosage.
NOTE: Clinical reviewer/Medical Director must override criteria when, in
his/her professional judgment, the requested item is medically necessary.
4
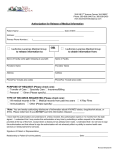
Field Name
Prior Authorization
Group Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber
Restrictions
Coverage Duration
Other Criteria
Field Description
Ampyra
Ampyra (dalfampridine) tablets
Medically accepted indications are defined using the following sources:
the Food and Drug Administration (FDA), Micromedex, American
Hospital Formulary Service (AHFS), United States Pharmacopeia Drug
Information for the Healthcare Professional (USP DI), the Drug Package
Insert (PPI), or disease state specific standard of care guidelines.
History of seizures. Moderate or severe renal impairment (creatinine
clearance ≤ 50mL/minute)
See “other criteria”
Patient must be 18 years of age or older
Prescriber must be a neurologist
If the criteria are met, the request will be approved with a 6 month
duration; if the criteria are not met, the request will be referred to a
clinical reviewer for medical necessity review.
Initial Authorization:
Baseline creatinine clearance (within 60 days of request)
Patient has diagnosis of multiple sclerosis (MS), patient is
ambulatory (baseline 25 foot walk was submitted with request),
AND patient has walking impairment
Documentation was submitted (consistent with pharmacy claims
data, OR for new members to the health plan, consistent with
chart notes) that patient is currently being treated for MS (e.g.
immunomodulator, interferon, immunosuppressive), or
documentation of a medical reason (intolerance, hypersensitivity)
as to why patient is unable to use one of these agents to treat
their medical condition
Drug is being requested at an FDA approved dose
Re-authorization:
Revision/Review
Date 04/2016
Documentation of improvement in 25 foot walk was submitted
with request
Documentation was submitted patient is on MS treatment (e.g.
immunomodulator, interferon, immunosuppressive), or
documentation of a medical reason (intolerance, hypersensitivity)
as to why patient is unable to use one of these agents to treat
their medical condition
Drug is being requested at an FDA approved dose
Medical Director/clinical reviewer must override criteria when, in
his/her professional judgement, the requested item is medically
necessary.
5
Field Name
Field Description
Prior Authorization Group
Anaplastic Lymphoma Kinase (ALK) Tyrosine Inhibitors for Non-Small Cell
Lung Cancer (NSCLC)
Xalkori® (Crizotinib), Zykadia® (Ceritinib), Alecensa™(alectinib)
Medically accepted indications are defined using the following sources: the Food and
Drug Administration (FDA), Micromedex, American Hospital Formulary Service
(AHFS), United States Pharmacopeia Drug Information for the Healthcare
Professional (USP DI) , and the Drug Package Insert), and/or per the National
Comprehensive Cancer Network (NCCN), the American Society of Clinical
Oncology (ASCO).
Drug(s)
Covered Uses
Exclusion Criteria
N/A
Required Medical Information
See “Other Criteria”
Age Restrictions
N/A
Prescriber Restrictions
Prescriber must be an oncologist.
Coverage Duration
If all of the conditions are met, the request will be approved with 6 month duration; if
the above conditions are not met, the request will be referred to a Medical
Director/Clinical Reviewer for medical necessity review.
Other Criteria
Review Date 2/2016
Baseline complete blood count with differential and as recommended by
manufacturer.
Baseline liver function studies including (ALT/AST and total bilirubin)and
as recommended by manufacturer
For treatment of non-small cell lung cancer (NSCLC), documentation of
FISH testing has been provided that the tumors are anaplastic lymphoma
kinase (ALK) positive.
If the request is for Zykadia® or Alecensa™(alectinib) there is a
documented trial of Xalkori® (crizotinib) and were intolerant to crizotinib or
had disease progression while taking it.
The medication is being prescribed by an oncologist at an FDA approved
dosage.
NOTE: Clinical reviewer must override criteria when, in his/her professional judgment,
the requested item is medically necessary.
6
Field Name
Field Description
Prior Authorization Group
ANDROGENIC AGENTS
Drug(s)
ANDROGEL (testosterone) 1.62%
ANDRODERM (testosterone)
TESTIM (testosterone)
AXIRON (testosterone)
ANDROID (testosterone)
ANDROXY (testosterone)
AXIRON (testosterone)
DEPO-TESTOSTERONE (Testosterone Cypionate)
FORTESTA (testosterone)
METHITEST
STRIANT BUCCAL
TESTOPEL IMPLANT (testosterone)
TESTRED (testosterone)
TESTOSTERONE ENANTHATE
TESTOSTERONE CYPIONATE
VOGELXO
Or any newly marketed testosterone agent
Medically accepted indications are defined using the following sources: the Food and
Drug Administration (FDA), Micromedex, American Hospital Formulary Service
(AHFS), United States Pharmacopeia Drug Information for the Healthcare
Professional (USP DI) , and the Drug Package Insert).
Patients that are female
Prescriber must document medical reason for low testosterone, such as
Hypogonadism, copy of laboratory result required, demonstrating low testosterone.
None
None
Covered Uses
Exclusion Criteria
Required Medical Information
Age Restrictions
Prescriber Restrictions
Coverage Duration
If all of the conditions are met, the request will be approved with 3 month duration; if
the above conditions are not met, the request will be referred to a clinical reviewer
for medical necessity review.
For Initial Authorization:
Male patient
Diagnosis of primary hypogonadism (congenital or acquired) or
hypogonadotropic hypogonadism (congenital or acquired)
Documented low testosterone level (s) (copy of laboratory result required)
For Re-Authorization:
Documentation indicating the member has clinically benefited from therapy
Repeat testosterone level (copy of laboratory result required)
Review Date 3/2015
NOTE: Clinical reviewer must override criteria when, in his/her professional judgment,
the requested item is medically necessary.
7
Field Name
Prior Authorization Group
Drug(s)
Field Description
Anti-PD-1 MONOCLONAL ANTIBODIES
Pembrolizumab (Keytruda®) Nivolumab (Opdivo®)
Covered Uses
Medically accepted indications are defined using the following sources: the
Food and Drug Administration (FDA), Micromedex, American Hospital
Formulary Service(AHFS), United States Pharmacopeia Drug Information for
the Healthcare Professional (USP DI) , and the Drug Package Insert), and/or
per the National Comprehensive Cancer Network (NCCN), the American
Society of Clinical Oncology (ASCO).
Exclusion Criteria
N/A
Required Medical Information
See “Other Criteria”
Age Restrictions
N/A
Prescriber Restrictions
Prescriber must be an oncologist.
Coverage Duration
If all of the conditions are met, the request will be approved with 6 month
duration; if the above conditions are not met, the request will be referred to a
Medical Director/Clinical Reviewer for medical necessity review.
Other Criteria
Review Date 2/2016
Baseline liver function studies including (ALT/AST and total bilirubin)
Baseline thyroid function studies
Baseline serum creatinine
For treatment of unresectable or metastatic melanoma, the patient must
have documented treatment failure with a BRAF inhibitor
[vemurafenib or dabrafenib (if BRAF V600 mutation positive)]
For the treatment of Non- Small Cell Lung Cancer (NSCLC), the
patient must have documented treatment failure with a platinum based
chemotherapy regimen
For the treatment of NSCLC with Keytruda, a copy of the FDA
approved test demonstrating tumor expression of PD-L1 was submitted
with request
For treatment of advanced renal cell carcinoma, patient must have
documented trial and failure with anti-angiogenic therapy.
The medication is being prescribed by an oncologist at an FDA
approved dosage
NOTE: Clinical reviewer must override criteria when, in his/her
professional judgment, the requested item is medically necessary.
8
Field Name
Prior Authorization Group
Description
Drugs
Field Description
ANGIOTENSIN II RECEPTOR BLOCKER
FORMULARY STATUS: Formulary, Pays at Point-ofSale (First Line)
Cozaar (losartan) tablets
Hyzaar (losartan/hydrochlorothiazide) tablets
FORMULARY STATUS: Formulary, Requires Step
Therapy (Second Line)
Avalide (irbesartan/hydrochlorothiazide) tablets
Avapro (irbesartan) tablets
Diovan (valsartan) tablets
Diovan-HCT(valsartan/hydrochlorothiazide) tablets
Note: Patient must meet #1 criteria for approval of
initial PA request
FORMULARY STATUS: Non-Formulary, Requires Prior
Authorization (Third Line)
Atacand (candesartan cilexetil) tablets
Atacand HCT (candesartan cilexetil/
hydrochlorothiazide) tablets
Azor (amlodipine besylate/olmesartan medoxomil)
tablets
Benicar (olmesartan medoxomil) tablets
Benicar HCT (olmesartan medoxomil/
hydrochlorothiazide) tablets
Edarbi (azilsartan) Tablets
Edarbyclor (azilsartan/hydrochlorothiazide) Tablets
Entresto (sacubitril-valsartan) Tablets
Exforge (amlodipine besylate/valsartan) tablets
Exforge HCT
(amlodipine/valsartan/hydrochlorothiazide) tablets
Micardis (telmisartan) tablets
Micardis-HCT (telmisartan/hydrochlorothiazide)
tablets
Teveten (eprosartan mesylate) tablets
Tribenzor (olmesartan
medoxomil/amlodipine/hydrochlorothiazide)
Twynsta (telmisartan/amlodipine)
Covered Uses
Note: Patient must meet #1 and #2 criteria for approval
of initial PA request
Medically accepted indications are defined using the
following sources: the Food and Drug Administration
(FDA), Micromedex, American Hospital Formulary Service
(AHFS), United States Pharmacopeia Drug Information for
Exclusion Criteria
Required Medical Information
Age Restrictions
Prescriber Restrictions
Coverage Duration
Other Criteria
the Healthcare Professional (USP DI), the Drug Package
Insert (PPI), or disease state specific standard of care
guidelines.
None
See “other criteria”
None
None
If the criteria are met, the request will be approved with a 12
month duration; if the criteria are not met, the request will
be referred to a clinical reviewer for medical necessity
review.
PA CRITERIA FOR APPROVAL:
1. Documented adequate trial and failure or intolerance
with a first line agent.
2. Documented adequate trial and failure or intolerance
with a second line agent.
Revision/Review Date
04/2016
NOTE: Clinical reviewer must override criteria when, in
his/her professional judgment, the requested item is
medically necessary.
Field Name
Prior Authorization
Group Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber Restrictions
Coverage Duration
Other Criteria
Field Description
ORAL ATYPICAL ANTIPSYCHOTICS
Abilify (Aripiprazole)
Clozaril (Clozapine)
Fanapt (Iloperidone)
Fazaclo (Clozapine)
Geodon (Ziprasidone)
Invega (Paliperidone)
Latuda (Lurasidone)
Risperdal (Risperidone)
Seroquel (Quetiapine)
Seroquel (Quetiapine Extended Release)
Symbyax (Olanzapine/Fluoxetine)
Zyprexa (Olanzapine)
Saphris (Asenapine) **Non-Listed**
Medically accepted indications are defined using the following
sources: the Food and Drug Administration (FDA), Micromedex,
American Hospital Formulary Service (AHFS), United States
Pharmacopeia Drug Information for the Healthcare Professional (USP
DI), the Drug Package Insert (PPI), or disease state specific standard
of care guidelines.
N/A
See “other criteria”
Abilify (Aripiprazole) > 6 years old
Clozaril (Clozapine) > 18 years old
Fanapt (Iloperidone) > 18 years old
Fazaclo (Clozapine) > 18 years old
Geodon (Ziprasidone) > 18 years old
Invega (Paliperidone) > 12 years old
Latuda (Lurasidone) > 18 years old
Risperdal (Risperidone) > 6 years old
Seroquel (Quetiapine) > 10 years old
Seroquel (Quetiapine Extended Release) > 10 years old
Symbyax (Olanzapine/Fluoxetine) > 10 years old
Zyprexa (Olanzapine) > 13 years old
Saphris (Asenapine) > 10 years old
N/A
If the criteria are met, the request will be approved with up to a 12
month duration; if the criteria are not met, the request will be referred
to a clinical reviewer for medical necessity review.
Initial Authorization:
Preferred atypical antipsychotics prescribing in a dose that
exceeds FDA approved limits will require prior
authorization.
For members outside of the stated age range, atypical
antipsychotics may be approved if the prescriber for the initial
Revision/Review Date
07/2016
or current prescription is in one of the following specialties:
psychiatry, developmental pediatric or pediatric neurology.
Documentation of a comprehensive patient evaluation
including baseline monitoring of all of the following:
o Hemoglobin A1c
o Fasting Glucose
o Lipids
If the request is from a pediatrician, approve preferred meds
for 2 months only to allow time for the member to be seen by
one of the approved specialties.
Requests will be considered based on individual
circumstances. Factors to be considered include, but not
limited to:
o Indication for use, previous therapy, previous dose,
concomitant therapy, and side effects of the
increased/higher doses.
Medical Director/clinical reviewer must override criteria when, in
his/her professional judgement, the requested item is medically
necessary.
Field Name
Prior Authorization
Group Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber Restrictions
Coverage Duration
Other Criteria
Revision/Review Date
04/2016
Field Description
Avinza
Avinza® (morphine sulfate) extended-release capsules
Medically accepted indications are defined using the following
sources: the Food and Drug Administration (FDA), Micromedex,
American Hospital Formulary Service (AHFS), United States
Pharmacopeia Drug Information for the Healthcare Professional (USP
DI), the Drug Package Insert (PPI), or disease state specific standard
of care guidelines.
N/A
See “other criteria”
N/A
N/A
If the criteria are met, the request will be approved with up to a 6
month duration; if the criteria are not met, the request will be referred
to a clinical reviewer for medical necessity review.
Initial Authorization:
Diagnosis of moderate to severe pain requiring opioid
analgesic for extended period of time.
AND
Documented trial and failure or intolerance to generic
morphine sulfate extended release tablets.
AND
Documented trial and failure or intolerance to Kadian®.
Medical Director/clinical reviewer must override criteria when, in
his/her professional judgement, the requested item is medically
necessary.
Field Name
Prior Authorization
Group Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber Restrictions
Coverage Duration
Other Criteria
Field Description
Bactroban®
®
Bactroban (mupirocin calcium ointment) Nasal Ointment
Medically accepted indications are defined using the following
sources: the Food and Drug Administration (FDA), Micromedex,
American Hospital Formulary Service (AHFS), United States
Pharmacopeia Drug Information for the Healthcare Professional (USP
DI), the Drug Package Insert (PPI), or disease state specific standard
of care guidelines.
N/A
See “other criteria”
N/A
N/A
If the criteria are met, the request will be approved with a 5 day
duration; if the conditions are not met, the request will be referred
to a Medical Director for medical necessity review.
Revision/Review Date
02/2016
Use is consistent with pre-operative prophylaxis of S. aureus
Medical Director/clinical reviewer must override criteria when, in
his/her professional judgement, the requested item is medically
necessary.
13
Field Name
Prior Authorization
Group Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber Restrictions
Coverage Duration
Other Criteria
Field Description
Banzel®
®
Banzel (rufinamide) tablet and oral suspension
Medically accepted indications are defined using the following
sources: the Food and Drug Administration (FDA), Micromedex,
American Hospital Formulary Service (AHFS), United States
Pharmacopeia Drug Information for the Healthcare Professional (USP
DI), the Drug Package Insert (PPI), or disease state specific standard
of care guidelines.
N/A
See “other criteria”
N/A
N/A
If the conditions are met, the request will be approved with a 12
month duration; if the conditions are not met, the request will be
referred to a Medical Director for medical necessity review.
Diagnosis of Lennox-Gastaut syndrome
AND
Revision/Review Date
02/2016
Patient is currently receiving another anticonvulsant
medication at a therapeutic dosage.
Medical Director/clinical reviewer must override criteria when, in
his/her professional judgement, the requested item is medically
necessary.
14
Field Name
Prior Authorization Group
Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber Restrictions
Coverage Duration
Other Criteria
Field Description
Botulinum Toxins A&B
OnabotulinumtoxinA (Botox®), IncobotulinumtoxinA (Xeomin®),
AbobotulinumtoxinA (Dysport™), RimabotulinumtoxinB (Myobloc®)
Medically accepted indications are defined using the following sources: the Food
and Drug Administration (FDA), Micromedex, American Hospital Formulary
Service(AHFS), United States Pharmacopeia Drug Information for the
HealthcareProfessional (USP DI), the Drug Package Insert (PPI), or disease state
specific standard of care guidelines.
N/A
N/A
N/A
None
If all of the conditions are met, the request will be approved for a 3 month
duration. If the conditions are not met, the request will be sent to a Medical
Director/clinical reviewer for medical necessity review.
**The use of these medications for cosmetic purposes is NOT a covered benefit
under the Medical Assistance program.**
Botox® is the preferred botulinum toxin for pediatric patients, chronic migraine,
overactive bladder and hyperhidrosis.
Xeomin® is the preferred botulinum toxin for spasmodic torticollis (cervical
dystonia), blepharospasm, upper limb spasticity, and any other off labeled
indication that is supported or recommended by the medical compendia and
standard of care guidelines.
For Approval:
The request is for a FDA approved indication, and/or is used for a medical
condition that is supported by the medical compendia and/or per Standard
of Care Guidelines in each respective disease state.
Documentation was submitted, that the patient had an (consistent with
pharmacy claims data) adequate trial (including dates of treatment at
maximum recommended doses of therapy) of standard conventional first
line therapy for their respective disease state (where applicable) as
recommended by the medical compendia and standard of care guidelines
and/or has a documented medical reason (intolerance, hypersensitivity,
contraindication, etc) for not taking standard conventional first line
therapy to treat their medical condition.
If the medication request is for Botulinum toxin type A (Botox®) for
treating Chronic Migraines (≥15 days per month with headache lasting 4
hours a day or longer), the patient has a documented (consistent with
pharmacy claims data) treatment failure after receiving an adequate trial
of beta blockers (e.g. metoprolol, atenolol, nadolol, propranolol, timolol),
tricyclic antidepressants (e.g. amitriptyline), Depakote, and topiramate.
If the medication request is for Botulinum toxin type A (Botox ®) for
treating Overactive Bladder, the patient has a documented treatment
15
Revision/Review Date
11/2015
failure after receiving an adequate trial (consistent with pharmacy claims
data) of at least 2 formulary medications (e.g. oxybutynin)
If the medication is being requested for an off labeled use that is
recommended by the medical compendia, the patient has a documented
trial/failure (including dates) of Xeomin® and/or has a medical reason
(intolerance, hypersensitivity, contraindication, etc.) for not utilizing
Xeomin® to manage their medical condition
Prescribed dosing of medication is within FDA approved guidelines and/or
is supported by the medical compendia as defined by the Social Security
Act and/or per Standard of Care Guidelines in each respective disease
state.
Physician/clinical reviewer must override criteria when, in his/her professional
judgment, the requested item is medically necessary.
16
Field Name
Prior Authorization
Group Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber Restrictions
Coverage Duration
Other Criteria
Field Description
Butrans®
Butrans® (buprenorphine) patches
Medically accepted indications are defined using the following
sources: the Food and Drug Administration (FDA), Micromedex,
American Hospital Formulary Service (AHFS), United States
Pharmacopeia Drug Information for the Healthcare Professional (USP
DI), the Drug Package Insert (PPI), or disease state specific standard
of care guidelines.
N/A
See “other criteria”
N/A
N/A
If the criteria are met, the request will be approved with up to a 6
month duration; if the criteria are not met, the request will be referred
to a Pharmacist for medical necessity review.
Must have moderate to severe chronic pain.
AND
Revision/Review Date
02/2016
Recent trial of or failure to two preferred long-acting
opioids including: morphine sulfate, methadone or
fentanyl patches
Medical Director/clinical reviewer must override criteria when, in
his/her professional judgement, the requested item is medically
necessary.
Field Name
Prior Authorization
Group Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber Restrictions
Coverage Duration
Other Criteria
Field Description
Celebrex®
Celebrex®(celecoxib) capsules
Medically accepted indications are defined using the following sources: the
Food and Drug Administration (FDA), Micromedex, American Hospital
Formulary Service (AHFS), United States Pharmacopeia Drug Information
for the Healthcare Professional (USP DI), the Drug Package Insert (PPI), or
disease state specific standard of care guidelines.
N/A
See “other criteria”
N/A
N/A
If the criteria are met, the request will be approved with up to a 6 month
duration (refer to individual section below for exact duration of
approval); if the criteria are not met, the request will be referred to a clinical
reviewer for medical necessity review.
Initial Authorization:
Anticoagulant Therapy:
Diagnosis of osteoarthritis, rheumatoid arthritis, juvenile rheumatoid
arthritis, or ankylosing spondylitis
and
Current therapy with anticoagulant therapy such as warfarin
If the above conditions are met, the request will be approved with a 3-month
duration; if the above conditions are not met, the request will be referred to a
clinical reviewer for medical necessity review. Re-evaluation of continued
warfarin therapy will be assessed at 3-month intervals for renewal.
Documented Gastrointestinal Disease (GERD, Erosive Esophagitis, Barretts
Esophagus, Zollinger Ellison Disease):
Diagnosis of osteoarthritis, rheumatoid arthritis, juvenile rheumatoid
arthritis, or ankylosing spondylitis
and
Documented gastrointestinal disease of the following conditions:
gastroesophageal reflux disease, erosive esophagitis, Barretts esophagus,
or Zollinger Ellison disease), currently taking either a proton pump
inhibitor or an H2 receptor antagonist.
If the above conditions are met, the request will be approved with a 6 month
duration; if the above conditions are not met, the request will be referred to a
clinical reviewer for medical necessity review.
NSAID Therapy Failure:
Diagnosis of osteoarthritis, rheumatoid arthritis, juvenile rheumatoid
arthritis, or ankylosing spondylitis
and
Documented trial and failure with therapeutic prescription doses or
intolerance to at least two formulary nonsteroidal anti-inflammatory drugs
(NSAIDs).
If the above conditions are met, the request will be approved with a 6-month
duration; if the above conditions are not met, the request will be referred to a
clinical reviewer for medical necessity review.
Familial Adenomatous Polyposis (FAP):
Diagnosis of familial adenomatous polyposis (FAP)
If the above conditions are met, the request will be approved with a 6-month
duration; if the above conditions are not met, the request will be referred to a
clinical reviewer for medical necessity review.
Primary Dysmenorrhea:
Premenopausal female patient
and
Diagnosis of primary dysmenorrhea
and
Documented trial and failure with therapeutic prescription doses or
intolerance to at least two formulary nonsteroidal anti-inflammatory drugs
(NSAIDs).
If the above conditions are met, the request will be approved with a 5 day
duration; if the above conditions are not met, the request will be referred to a
clinical reviewer for medical necessity review.
Acute Pain:
Diagnosis of acute pain
and
Documented trial and failure with therapeutic prescription doses or
intolerance to at least two formulary nonsteroidal anti-inflammatory drugs
(NSAIDs).
If the above conditions are met, the request will be approved with a 5 day
duration; if the above conditions are not met, the request will be referred to a
clinical reviewer for medical necessity review.
Revision/Review Date
04/2016
Medical Director/clinical reviewer must override criteria when, in his/her
professional judgement, the requested item is medically necessary.
Field Name
Prior Authorization Group
Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber Restrictions
Field Description
Cholbam™
Cholbam™ (cholic acid)
Medically accepted indications are defined using the following sources: the Food
and Drug Administration (FDA), Micromedex, American Hospital Formulary Service
(AHFS), United States Pharmacopeia Drug Information for the Healthcare
Professional (USP DI), the Drug Package Insert (PPI), or disease state specific
standard of care guidelines.
N/A
See “other criteria”
N/A
MD is a gastroenterologist OR hepatologist
Coverage Duration
If all of the conditions are met, the request will be approved for a 3 month duration
for the first year of therapy, and then for a 6 month duration after one year of
treatment. If the conditions are not met, the request will be sent to a Medical
Director/clinical reviewer for medical necessity review.
Other Criteria
Initial authorization:
Patient has a confirmed diagnosis of:
Bile acid synthesis disorder due to single enzyme defect (SEDs)
OR
peroxisomal disorders (PDs) including Zellweger spectrum
disorders in patients that exhibit manifestations of liver disease,
steatorrhea or complications from decreased fat soluble vitamin
absorption
Current labs (within 30 days of request) have been submitted for the
following:
ALT/AST
GGT (serum gamma glutamyltransferase)
ALP (Alkaline phosphatase)
Bilirubin
INR
Re-authorization:
Documentation has been submitted indicating clinical benefit/ liver
function has improved since beginning treatment*
* TREATMENT SHOULD BE DISCONTINUED IF LIVER FUNCTION DOES NOT
IMPROVE WITHIN 3 MONTHS OF STARTING TREATMENT, IF COMPLETE BILIARY
OBSTRUCTION DEVELOPS OR CHOLESTASIS
Revision/Review Date
11/2015
Current labs (within 30 days of request) have been submitted for the
following:
ALT/AST
GGT (serum gamma glutamyltransferase)
ALP (Alkaline phosphatase)
Bilirubin
INR
Medical Director/clinical reviewer must override criteria when, in his/her
professional judgement, the requested item is medically necessary.
21
Field Name
Prior Authorization
Group Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber Restrictions
Coverage Duration
Other Criteria
Field Description
CNS STIMULANTS AGE LIMIT
Concerta (Methylphenidate)
Daytrana (Methylphenidate)
Intuniv (Guanfacine)
Quillivant XR (Methylphenidate)
Metadate CD (Methylphenidate)
Metadate ER (Methylphenidate)
Kapvay (Clonidine HCL)
Medically accepted indications are defined using the following
sources: the Food and Drug Administration (FDA), Micromedex,
American Hospital Formulary Service (AHFS), United States
Pharmacopeia Drug Information for the Healthcare Professional (USP
DI), the Drug Package Insert (PPI), or disease state specific standard
of care guidelines.
None
See “other criteria”
Concerta (Methylphenidate) > 6 years old
Daytrana (Methylphenidate) > 6 years old
Intuniv (Guanfacine) > 6 years old
Quillivant XR (Methylphenidate) > 6 years old
Metadate CD (Methylphenidate) > 6 years old
Metadate ER (Methylphenidate) > 6 years old
Kapvay (Clonidine HCL) > 6 years old
None
If the criteria are met, the request will be approved with up to a 12
month duration; if the criteria are not met, the request will be referred
to a clinical reviewer for medical necessity review.
Initial Authorization:
Revision/Review Date
04/2016
Diagnosis of ADHD/ADD as attested to by Prescriber (with
special consideration given to behavioral health specialists)
Adequate trial and failure of behavior modification therapy
(could include parent and/or teacher) as attested to by
Prescriber
Request is for FDA approved dosage
Medical Director/clinical reviewer must override criteria when, in
his/her professional judgement, the requested item is medically
necessary.
Prior Authorization
Group Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber Restrictions
Coverage Duration
Other Criteria
Revision/Review Date
02/2016
Crestor
CRESTOR® (rosuvastatin calcium)
Medically accepted indications are defined using the following
sources: the Food and Drug Administration (FDA), Micromedex,
American Hospital Formulary Service (AHFS), United States
Pharmacopeia Drug Information for the Healthcare Professional
(USP DI), the Drug Package Insert (PPI), or disease state specific
standard of care guidelines.
Patients that are pregnant or breast feeding, or active liver disease or
unexplained persistent elevations of serum transaminases
Documented trial and failure of atorvastatin
Patient must be 8 years of age or older
N/A
If all of the criteria is met, the request will be approved for 12 months.
If the conditions are not met, the request will be sent to a Medical
Director/clinical reviewer for medical necessity review.
N/A
Medical Director/clinical reviewer must override criteria when,
in his/her professional judgement, the requested item is medically
necessary.
23
Field Name
Prior Authorization
Group Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber Restrictions
Coverage Duration
Other Criteria
Field Description
Crinone®
Crinone® (micronized progesterone)
Medically accepted indications are defined using the following
sources: the Food and Drug Administration (FDA), Micromedex,
American Hospital Formulary Service (AHFS), United States
Pharmacopeia Drug Information for the Healthcare Professional (USP
DI), the Drug Package Insert (PPI), or disease state specific standard
of care guidelines.
N/A
See “other criteria”
N/A
N/A
If the criterion is met, the request will be approved for 2 boxes (15
single use applicators per box) per 30 days until the end of pregnancy.
If the criterion is not met, the request will be referred to a Clinician for
medical necessity review.
Initial Authorization:
Documented ultrasound of transvaginal cervical length
(TVCL) ≤ 25mm between weeks 17 and 24 of gestation.
AND
Crinone 8% is not being used for infertility.
Revision/Review Date
07/2016
Medical Director/clinical reviewer must override criteria when, in
his/her professional judgement, the requested item is medically
necessary.
Prior Authorization Group Description
Drug(s)
Cystic Fibrosis Agents
Aztreonam lysine (Cayston®), dornase alfa
(Pulmozyme®), tobramycin (Tobi®, Tobi Podhaler®),
ivacaftor (Kalydeco®, Kalydeco Granules®),
Lumacaftor/Ivacaftor (Orkambi®)
Medically accepted indications are defined using the
following sources: the Food and Drug
Administration (FDA), Micromedex, American
Hospital Formulary Service (AHFS), United States
Pharmacopeia Drug Information for the Healthcare
Professional (USP DI), the Drug Package Insert
(PPI), and/or per standard of care guidelines.
See “Other Criteria”
See “Other Criteria”
See “Other Criteria”
MD is pulmonologist
If all of the conditions are met, for Kalydeco® and
Orkambi® the initial request will be 3 months, all
other meds will be approved with a 6-month
duration. Reauthorization for Kalydeco® and
Orkambi® will be 6 months. If all of the criteria are
not met, the request is referred to a Medical
director/clinical reviewer for medical necessity
review.
Covered Uses
Exclusion Criteria
Required Medical Information
Age Restrictions
Prescriber Restrictions
Coverage Duration
Other Criteria
CRITERIA FOR THE USE OF KALYDECO® (IVACAFTOR) IN
THE TREATMENT OF CYSTIC FIBROSIS:
25
The medication is for the treatment of a CF
patient who has an FDA approved
indication for treatment of the patient’s
genotype (there is a FDA cleared CF
mutation test that can be used to determine
genotype if unknown).
Copy of the FDA-cleared CF mutation test
has been provided with request
The patient is 2 years or older.
For patients age 2-6, documentation of the
patient’s weight
The patient is not a homozygous for the
F508del mutation in the cystic fibrosis
transmembrane conductance regulator
(CFTR) gene.
Baseline FEV1 has been submitted with
request (within 90 days of request)
Documentation of current ALT/AST levels
(within 90 days of request). (Ivacaftor is
contraindicated for ALT and AST levels 5
times over upper limit of normal. If ALT
and AST levels are 5 times over the upper
limit of normal or higher, ivacaftor should
not be started until the levels are below this
range.)
The medication is being prescribed at a
dose that is within FDA approved
guidelines.
Continuation of therapy for KALYDECO® (IVACAFTOR):
Documentation has been submitted that
patient has obtained clinical benefit from
medication (i.e. improvement in FEV1,
BMI, decrease in number or frequency of
pulmonary exacerbations, or improvement
in quality of life)
Repeat FEV1 (within 90 days of request)
Repeat ALT/AST (within 90 days of
request) , and results are not 5 times the
upper limit of normal or higher
The medication is being used for an FDA
approved indication at an FDA approved
dose
The prescriber is a pulmonologist
CRITERIA FOR THE USE OF TOBI® (TOBRAMYCIN)
PRODUCTS IN THE TREATMENT OF CYSTIC FIBROSIS:
The medication is being prescribed for the
treatment of a cystic fibrosis patient
colonized with Pseudomonas aeruginosa.
The medication is being prescribed at a
dose that is within FDA approved
guidelines.
CRITERIA FOR THE USE OF PULMOZYME® (DORNASE
ALFA) IN THE TREATMENT OF CYSTIC FIBROSIS:
The medication is not being used as
monotherapy.
The patient is 5 years or older.
The medication is being prescribed at a
dose that is within FDA approved
guidelines.
CRITERIA FOR THE USE OF CAYSTON® (AZTREONAM
LYSINE) IN THE TREATMENT OF CYSTIC FIBROSIS:
The medication is being prescribed for the
treatment of a cystic fibrosis patient
colonized with Pseudomonas aeruginosa.
The medication is being prescribed at a
dose that is within FDA approved
guidelines.
CRITERIA FOR THE USE OF ORKAMBI ®
(LUMACAFTOR/IVACAFTOR) IN THE TREATMENT OF
CYSTIC FIBROSIS:
26
The patient is 12 years of age or older
The patient IS homozygous for the F508del
mutation in the the cystic fibrosis
transmembrane conductance regulator
(CFTR) gene.
Copy of the FDA-cleared CF mutation test
has been provided with request
Baseline FEV1 has been submitted with
request (within 90 days of
request)Documentation of current
ALT/AST and bilirubin levels (within -90
days of request)
The medication is being prescribed at a
dose that is within FDA approved
guidelines.
Continuation of therapy for ORKAMBI ®
(LUMACAFTOR/IVACAFTOR):
Documentation has been submitted that
patient has obtained clinical benefit from
medication (i.e. improvement in FEV1,
BMI, decrease in number or frequency of
pulmonary exacerbations, or improvement
in quality of life)
Repeat FEV1 (within 90 days of request)
Repeat ALT/AST (within 90 days of
request) , and results are not 5 times the
upper limit of normal or higher
The medication is being used for an FDA
approved indication at an FDA approved
dose
The prescriber is a pulmonologist
NOTE: Clinical reviewer/Medical Director must
override criteria when, in his/her professional
judgment, the requested item is medically
necessary.
Review/Revision Date 2/2016
27
Field Name
Prior Authorization
Group Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber Restrictions
Coverage Duration
Other Criteria
Field Description
Daliresp®
Daliresp® (roflumilast) tablets
Medically accepted indications are defined using the following
sources: the Food and Drug Administration (FDA), Micromedex,
American Hospital Formulary Service (AHFS), United States
Pharmacopeia Drug Information for the Healthcare Professional (USP
DI), the Drug Package Insert (PPI), or disease state specific standard
of care guidelines.
N/A
See “other criteria”
N/A
N/A
If the criteria are met, the request will be approved with up to a 12
month duration; if the criteria are not met, the request will be referred
to a clinical reviewer for medical necessity review.
Initial Authorization:
Revision/Review Date
07/2016
Diagnosis of severe chronic obstructive pulmonary disease
associated with chronic bronchitis or a history of exacerbations
Documented trial of three individual first line agents or a
combination product from each of the following classes within
the previous 60 days:
o Long Acting Beta2- Agonists
o Long Acting Anticholinergics
o Inhaled Corticosteroids
o Combination Beta2-Agonist/Anticholinergic
o Combination Beta2- Agonist/Corticosteroid
Medical Director/clinical reviewer must override criteria when, in
his/her professional judgement, the requested item is medically
necessary.
Field Name
Prior Authorization
Group Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber Restrictions
Coverage Duration
Other Criteria
Field Description
®
Danocrine (danazol)
®
Danocrine (danazol) capsules
Medically accepted indications are defined using the following
sources: the Food and Drug Administration (FDA), Micromedex,
American Hospital Formulary Service (AHFS), United States
Pharmacopeia Drug Information for the Healthcare Professional (USP
DI), the Drug Package Insert (PPI), or disease state specific standard
of care guidelines.
N/A
See “other criteria”
N/A
See “other criteria”
If the criteria are met, the request will be approved with a 6 month
duration for generic medication; if the criteria are not met, the
request will be referred to a Medical Director for medical
necessity review.
ENDOMETRIOSIS
Diagnosis of endometriosis
AND
Documented trial and failure, intolerance or documented
medical reason for not using first line therapy of oral
contraceptive therapy.
AND
Prescribing physician is a gynecologist.
FIBROCYSTIC BREAST PAIN DISEASE
Diagnosis of fibrocystic breast disease.
AND
Documented trial and failure, intolerance or documented
medical reason for not using first line therapy of analgesics
including acetaminophen and NSAIDs.
AND
Prescribing physician is a gynecologist.
HEREDITARY ANGIOEDEMA:
Diagnosis of hereditary angioedema.
Revision/Review Date
02/2016
Medical Director/clinical reviewer must override criteria when, in
his/her professional judgement, the requested item is medically
necessary.
29
Field Name
Prior Authorization Group
Description
Drugs
Covered Uses
Exclusion Criteria
Field Description
Daraprim®
Daraprim® (pyrimethamine)
Medically accepted indications are defined using the following sources: the Food
and Drug Administration (FDA), Micromedex, American Hospital Formulary Service
(AHFS), United States Pharmacopeia Drug Information for the Healthcare
Professional (USP DI), the Drug Package Insert (PPI), or disease state specific
standard of care guidelines.
Patients with documented megaloblastic anemia due to folate deficiency.
Required Medical
Information
Age Restrictions
Prescriber Restrictions
Coverage Duration
Other Criteria
Revision/Review Date
11/2015
Patient has diagnosis of toxoplasmosis and is being used in combination
with a sulfonamide.
If diagnosis is prophylaxis of malaria-documentation of a medical reason
has been provided as to why patient is not able to use all other first line
malaria agents, as resistance to pyrimethamine is prevalent worldwide,
and it is not suitable as a prophylactic agent for travelers to most areas.
N/A
Prescriber must be an appropriate specialist or documentation has been provided
that prescriber has consulted with an appropriate specialist (i.e. infectious disease,
OB/GYN)
If all of the conditions are met, the request will be approved for a 2 month
duration. If the conditions are not met, the request will be sent to a Medical
Director/clinical reviewer for medical necessity review.
N/A
Medical Director/clinical reviewer must override criteria when, in his/her
professional judgement, the requested item is medically necessary.
30
Field Name
Prior Authorization
Group Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber Restrictions
Coverage Duration
Other Criteria
Field Description
®
DDAVP
DDAVP® (desmopressin) Tablets & Nasal Spray/Nasal Solution (Rhinal
Tube)
Medically accepted indications are defined using the following sources:
the Food and Drug Administration (FDA), Micromedex, American
Hospital Formulary Service (AHFS), United States Pharmacopeia Drug
Information for the Healthcare Professional (USP DI), the Drug Package
Insert (PPI), or disease state specific standard of care guidelines.
N/A
See “other criteria”
N/A
N/A
If the criteria are met, the request will be approved with a 12 month
duration for generic medication; if the criteria are not met, the request
will be referred to a Medical Director for medical necessity review.
Tablets
Diagnosis of primary nocturnal enuresis in children 6 years of
age and older.
OR
Diagnosis of central cranial (neurogenic) diabetes insipidus.
NOTE: Tablet formulation will process at the point-of-sale for
members ≥6 years old.
Nasal Spray and Rhinal Tube (nasal solution):
Diagnosis of central cranial (neurogenic) diabetes insipidus.
Revision/Review Date
02/2016
Medical Director/clinical reviewer must override criteria when, in
his/her professional judgement, the requested item is medically
necessary.
31
Field Name
Prior Authorization
Group Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber Restrictions
Coverage Duration
Other Criteria
Field Description
Diamox Sequel®
Diamox Sequel® (acetazolamide sustained release) capsules
Medically accepted indications are defined using the following
sources: the Food and Drug Administration (FDA), Micromedex,
American Hospital Formulary Service (AHFS), United States
Pharmacopeia Drug Information for the Healthcare Professional (USP
DI), the Drug Package Insert (PPI), or disease state specific standard
of care guidelines.
N/A
See “other criteria”
N/A
N/A
If the conditions are met, the request will be approved with a 6 month
duration; if the above conditions are not met, the request will be
referred to a Medical Director/clinical reviewer for medical necessity
review.
Initial authorization:
Diagnosis of chronic simple open angle glaucoma, or
secondary glaucoma.
AND
Revision/Review Date
02/2016
Documented trial and failure with therapeutic doses or
intolerance to acetazolamide immediate release tablets.
Medical Director/clinical reviewer must override criteria when, in
his/her professional judgement, the requested item is medically
necessary.
34
Field Name
Prior Authorization
Group Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber
Restrictions
Coverage Duration
Other Criteria
Diclegis
Field Description
®
Diclegis® (doxylamine/pyridoxine HCL)
Medically accepted indications are defined using the following sources:
the Food and Drug Administration (FDA), Micromedex, American
Hospital Formulary Service (AHFS), United States Pharmacopeia Drug
Information for the Healthcare Professional (USP DI), the Drug Package
Insert (PPI), or disease state specific standard of care guidelines.
Member is a male
See “other criteria”
N/A
Prescriber must be an obstetrician/gynecologist
If the above conditions are met, the request will be approved for 6 (six)
months. If the conditions are not met, the request will be sent to a
Medical Director/clinical reviewer for medical necessity review.
Initial authorization:
The indicated diagnosis of nausea and vomiting due to pregnancy.
AND
The member has had an adequate trial and failure with one (1) of
the agents
o Ondansetron, pyridoxine, vitamin B6, metoclopramide
Revision/Review
Date 02/2016
Medical Director/clinical reviewer must override criteria when, in
his/her professional judgement, the requested item is medically
necessary.
36
Field Name
Prior Authorization
Group Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber Restrictions
Coverage Duration
Other Criteria
Field Description
Dostinex®
Dostinex® (cabergoline) tablets
Medically accepted indications are defined using the following
sources: the Food and Drug Administration (FDA), Micromedex,
American Hospital Formulary Service (AHFS), United States
Pharmacopeia Drug Information for the Healthcare Professional (USP
DI), the Drug Package Insert (PPI), or disease state specific standard
of care guidelines.
N/A
See “other criteria”
N/A
N/A
If the conditions are met, the request will be approved with a 6 month
duration; if the above conditions are not met, the request will be
referred to a Medical Director/clinical reviewer for medical necessity
review.
Initial authorization:
Diagnosis of hyperprolactinemia.
AND
Revision/Review Date
02/2016
Documented trial and failure with therapeutic doses or intolerance
to bromocriptine therapy.
Medical Director/clinical reviewer must override criteria when, in
his/her professional judgement, the requested item is medically
necessary.
37
Field Name
Prior Authorization
Group Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber Restrictions
Coverage Duration
Other Criteria
Field Description
Effient®
Effient® (prasugrel) tablets
Medically accepted indications are defined using the following
sources: the Food and Drug Administration (FDA), Micromedex,
American Hospital Formulary Service (AHFS), United States
Pharmacopeia Drug Information for the Healthcare Professional (USP
DI), the Drug Package Insert (PPI), or disease state specific standard
of care guidelines.
N/A
See “other criteria”
N/A
N/A
If the criteria are met, the request will be approved with up to a 12
month duration; if the criteria are not met, the request will be referred
to a clinical reviewer for medical necessity review.
Initial Authorization:
Revision/Review Date
04/2016
Diagnosis of unstable angina or non-ST-elevation myocardial
infarction (NSTEMI), or ST-elevation myocardial infarction
(STEMI)
History of primary or delayed percutaneous coronary
intervention (PCI).
No active pathological bleeding.
No history of transient ischemic attacks or stroke.
Medical Director/clinical reviewer must override criteria when, in
his/her professional judgement, the requested item is medically
necessary.
Field Name
Prior Authorization
Group Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber Restrictions
Coverage Duration
Other Criteria
Field Description
Elidel®
Elidel® (pimecrolimus) cream
Medically accepted indications are defined using the following
sources: the Food and Drug Administration (FDA), Micromedex,
American Hospital Formulary Service (AHFS), United States
Pharmacopeia Drug Information for the Healthcare Professional (USP
DI), the Drug Package Insert (PPI), or disease state specific standard
of care guidelines.
N/A
See “other criteria”
N/A
N/A
If the conditions are met, the request will be approved with a 6 month
duration; if the above conditions are not met, the request will be
referred to a Medical Director/clinical reviewer for medical necessity
review.
Diagnosis of mild to moderate atopic dermatitis in non
immunocompromised patient in whom the use of alternative,
conventional therapy is deemed inadvisable because of potential
risks, or who are not adequately responsive to or intolerant of
alternative conventional therapies.
AND
Revision/Review Date
02/2016
Prescription written by a pediatrician or dermatologist.
Medical Director/clinical reviewer must override criteria when, in
his/her professional judgement, the requested item is medically
necessary.
39
PRIOR AUTHORIZATION CRITERIA
ELMIRON
®
(pentosan polysulfate sodium)
PA Criteria
Criteria Details
Covered Uses
Medically accepted indications are defined using the following sources: the Food and Drug
Administration (FDA), Micromedex, American Hospital Formulary Service (AHFS),
United States Pharmacopeia Drug Information for the Healthcare
Professional (USP DI), and the Drug Package Insert.
Exclusion
Criteria
None
Required
Medical
Information
See “Other Criteria”
Age Restrictions
None
Prescriber
Restrictions
None
Coverage
Duration
Other Criteria
If the criterion is met, the request will be approved with a 6 month duration. If the
criterion is not met, the request will be referred to a Clinician for medical necessity
review.
• Diagnosis of interstitial cystitis
***Please Note: Patients should be evaluated at 3 months and may be continued an
additional 3 months if there has been no improvement and if there are no therapy-limiting
side effects. The risks and benefits of continued use beyond 6 months in patients who
have not responded is not yet known.
NOTE: Clinical reviewer must override criteria when, in his/her professional
judgment, the requested item is medically necessary.
Revision Date 11/2015
40
Field Name
Field Description
Prior Authorization Group
Desc
Drug(s)
Covered Uses
Exclusion Criteria
Required Medical
Information
Age
Restrictions
Prescriber Restrictions
ENDOCRINE AND METABOLIC AGENTS/AGENTS FOR GOUT
Colcrys® (Colchicine)
*Medically accepted indications are defined using the following sources: the Food
and Drug Administration (FDA), Micromedex, American Hospital Formulary
Service (AHFS), United States Pharmacopeia Drug Information for the Healthcare
Professional (USP DI) , and the Drug Package Insert).
None
None
None
None
Coverage Duration
Other Criteria
See Specific Indications
CRITERIA FOR APPROVAL:
Acute gout attack:
Is 17 years of age or older
Has a documented history of therapeutic failure, intolerance, or
contraindication to the following at appropriate doses and frequencies
for the treatment of gout:
NSAIDs or COX-2 Inhibitors
AND
Intra-articular or systemic corticosteroids
If the above conditions are met, the request will be approved with up to three 0.6 mg
tablets (total 1.8mg) for up to 2 week duration; if the above conditions are not met, the
request will be referred to a Pharmacist for medical necessity review.
Chronic gout:
•
Is 17 years of age or older
•
Is being prescribed Colcrys in combination with a uric acid lowering
medication (such as allopurinol, probenecid, Uloric, or Col-Probenecid) recently
started for the prophylaxis of gout attacks.
If the above conditions are met, the request will be approved for a 6 month duration; if
the above conditions are not met, the request will be referred to a clinical reviewer for
medical necessity review.
Familial Mediterranean Fever (FMF):
•
is 4 years of age or older
If the above condition is met, the request will be approved with 6 month duration; if
the above conditions are not met, the request will be referred to a clinical reviewer for
medical necessity review.
NOTE: Clinical reviewer must override criteria when, in his/her professional judgment,
the requested item is medically necessary.
Associated Policy: Prior Authorization of Prescription Drugs 236.200
Review Date: 11/2015
41
Field Name
Prior Authorization
Group Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber Restrictions
Coverage Duration
Other Criteria
Field Description
Entocort EC®
Entocort EC® (budesonide)
Medically accepted indications are defined using the following
sources: the Food and Drug Administration (FDA), Micromedex,
American Hospital Formulary Service (AHFS), United States
Pharmacopeia Drug Information for the Healthcare Professional (USP
DI), the Drug Package Insert (PPI), or disease state specific standard
of care guidelines.
N/A
See “other criteria”
N/A
N/A
If the criteria are met, the request will be approved for up to a 16 week
duration; if the criteria are not met, the request will be referred to a
clinical reviewer for medical necessity review.
Initial Authorization:
Diagnosis of mild to moderate active or remissive Crohn’s
disease involving the ileum and/or the ascending colon.
AND
Prescription written by a gastroenterologist.
AND
Revision/Review Date
07/2016
Documented trial and failure with 16 weeks of therapy at
therapeutic doses of at least two first-line therapies of
sulfasalazine, mesalamine and prednisone.
Medical Director/clinical reviewer must override criteria when, in
his/her professional judgement, the requested item is medically
necessary.
Field Name
Prior Authorization Group
Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical Information
Age Restrictions
Prescriber Restrictions
Coverage Duration
Other Criteria
Revision/Review Date 02/2016
Field Description
Evzio Auto Injector
®
Evzio® (naloxone)
Medically accepted indications are defined using the
following sources: the Food and Drug Administration (FDA),
Micromedex, American Hospital Formulary Service (AHFS),
United States Pharmacopeia Drug Information for the
Healthcare Professional (USP DI), the Drug Package Insert
(PPI), or disease state specific standard of care guidelines.
N/A
See “other criteria”
N/A
N/A
If the above conditions are met, the request will be approved
with a 12 month duration with a quantity limit of four (4) per
year (two (2) boxes – 1.6 ml). If the conditions are not met,
the request will be sent to a Medical Director/clinical
reviewer for medical necessity review.
The indicated diagnosis (including any applicable labs
and /or tests) and medication usage must be supported
by documentation from the patient’s medical records
AND
At risk of suspected opioid overdose (respiratory and/or
CNS depression)
AND
Unable to use/access naloxone vial for injection or
inhalation.
Medical Director/clinical reviewer must override criteria
when, in his/her professional judgement, the requested
item is medically necessary.
43
SELECT HEALTH PRIOR AUTHORIZATION CRITERIA
FARESTON® (toremifene) Tablet: 60mg
FORMULARY STATUS: Formulary
PA CRITERIA FOR APPROVAL:
Postmenopausal woman with the diagnosis of metastatic breast cancer.
AND
Documented intolerance to tamoxifen.
If the above conditions are met, the request will be approved with a 12 month duration; if
the above conditions are not met, the request will be referred to a clinical reviewer for
medical necessity review.
FDA INDICATIONS:
Treatment of metastatic breast cancer in postmenopausal women with estrogen-receptor
(ER)-positive or ER-unknown tumors.
DOSAGE AND ADMINISTRATION:
Dosage is 60 mg once daily, generally continued until disease progression is observed.
BLACK BOX WARNING:
May prolong the QT interval; QTc prolongation is dose-dependent and concentration
dependent. Torsade de pointes, syncope, seizure and/or sudden death may occur. Use is
contraindicated in patients with congenital or acquired long QT syndrome, uncorrected
hypokalemia, or uncorrected hypomagnesemia. Avoid use with other medications
known to prolong the QT interval and with strong CYP3A4 inhibitors.
REFERENCES:
1. Haskell SG. Selective estrogen receptor modulators. South Med J 2003;96(5);469-476.
2. Riggs BL, Hartmann LC. Selective estrogen receptor modulators-mechanism of action
and application to clinical practice. NEJM 2003;348(7):618-629.
3. Parker LM. Sequencing of hormonal therapy in postmenopausal women with metastatic
breast cancer. Clin Ther 2002;24 Suppl C:C43-57.
4. Johnston SR. Endocrine manipulation in advanced breast cancer: recent advances with
SERM therapies. Clin Cancer Res 2001 Dec;7(12 Suppl):4376s-4387s; discussion 4411s4412s.
5. Product Information. Fareston (toremifene). GTx, Inc. October 2014.
6. NCCN Clinical Practice Guidelines in Oncology. Breast Cancer. Version V.1.2010.
Available at www.nccn.org.
7. Pagani, O., et al. Tremifene and Tamoxifen are Equally Effective for Early-Stage Breast
Cancer: First Results of International Breast Cancer Study Group Trials 12-93 and 1493. Annuals of Oncology. 2004. 15: 1749 – 1759.
8. Milla-Santos, A., et al. Phase III Randomized Trial of Toremifene vs. Tomoxifen in
Hormonodependant Advanced Breast Cancer. Breast Cancer Research and Treatment.
January 2001. 65: 119-124.
Revision/Review Date: 11/2015
Associated Policy: Prior Authorization of Prescription Drugs 236.200
NOTE: Clinical reviewer must override criteria when, in his/her professional
judgment, the requested item is medically necessary.
44
PERFORMRx PRIOR AUTHORIZATION CRITERIA
For FUZEON® (Enfuvirtide): 90mg vial
FOR ADULTS:
PA CRITERIA FOR INITIAL APPROVAL:
The patient has documented treatment failure to at least one sensitivity-assisted antiretroviral therapy regimen and at least two
drug regimens that included two different NRTIs and two or more PIs (see table 1), or the patient has a documented medical
reason for not trying two drug regimens that included two different NRTIs and two or more PIs. Refer to Fuzeon Medication
History Form and any other documentation sent by prescriber. Failure may be defined as:
1. Less than a one-log drop in viral load after 12 weeks therapy on a regimen
2. Repeated viral detection in plasma after initial suppression
3. A viral load of > 400 copies/mL after 24 weeks of continued treatment OR > 50 copies/mL after 48 weeks of
continued treatment.
4. A decrease in CD4 count to less than baseline.
3
5. A failure to increase CD4 count by 25 – 50 cells/mm above the baseline count over the first year of therapy.
6. Clinical deterioration: defined as new AIDS-defining illness concurrent with a virological response (greater than a one-log
drop) on current regimen
If the patient is currently taking Stribild, Triumeq, Complera or Atripla, documentation has been submitted indicating the
medical necessity for utilizing Fuzeon in combination with these agents.
Recent (within 30 days or while patient was on current medication regimen) genotype and phenotype testing result was
submitted with request for Fuzeon to determine optimal regimen of at least two sensitive and tolerated anti-retroviral
medications and to eliminate previously ineffective anti-retroviral medications, or there are less than two effective
medications based on sensitivity testing and the patient is at risk for opportunistic infection or death.
Provider is infectious disease or HIV specialist
The patient has a documented adherence level on taking anti-retroviral therapy of greater than 80% and any issue that may
have caused a decrease in adherence in the past (drug or alcohol abuse, difficulty of dosing schedule, etc.) has been
addressed.
Documentation of pretreatment CD4 count and viral RNA was submitted with request.
If all of the above conditions are met, the request will be approved with a 16-week duration; if all of the above criteria are not met, the
request is referred to a Clinical reviewer/Medical Director for medical necessity review.
PA CRITERIA FOR RE-APPROVAL:
Documentation of current background drug therapy was submitted with request (Fuzeon is not recommended as
monotherapy or to be used without optimal oral therapy).
For the initial reauthorization: documentation submitted of a viral load drop of at least a one-log decrease from baseline after 12
weeks of starting therapy for requests to continue therapy beyond 16 weeks, or there is documentation provided that the patient
has documented clinical improvement (i.e. increased CD 4 count) with treatment.
After the initial reauthorization: documentation submitted of current (within the past 30 days) CD 4 count and HIV RNA viral load.
Provider is infectious disease or HIV specialist
If the patient has been on Fuzeon therapy AND there is an increase of at least 2 log in viral load or a 30% decline in CD4 counts
from baseline then current phenotype/genotype testing (within the past 30 days) must be submitted to indicate continued
susceptibility of the HIV virus to Fuzeon.
If all of the above conditions are met, the request will be approved for up to a 6 month duration; if all of the above criteria are not met, the
request is referred to a Medical Director for medical necessity review.
FOR CHILDREN:
PA CRITERIA FOR INITIAL APPROVAL:
Documentation that the patient is pre-pubertal.
The patient has documented treatment failure to at least two drug regimens that included two different NRTIs and two or more
PIs (see table 1), or the patient has a documented medical reason for not trying two drug regimens that included
two different NRTIs and two or more PIs. Refer to Fuzeon Medication History Form and any other documentation sent by
prescriber. Failure may be defined as:
1. For previously naïve patients or those with limited antiretroviral experience: Less than a one-log drop in viral load after 812 weeks therapy on a regimen.
2. For patients with more extensive antiretroviral experience: Less than a one-log drop in viral load after 6 months of
continued treatment.
3. Repeated viral detection in plasma after initial suppression
4. A failure to increase CD4 count by 5% above the baseline or, for children over age of 4 -6 years old, to increase their
3
45 the first year of therapy.
CD4 cell count by at least 50 cells/mm above baseline over
5. Clinical deterioration: defined as progressive neurodevelopemental deterioration (i.e. the presence of two or more of the
following findings documented on repeated assessments: impairment in brain growth, decline of cognitive
function documented by psychometric testing, or clinical motor dysfunction), growth failure (i.e. persistent decline in weightgrowth velocity despite adequate nutritional support and without other explanation), or severe or recurrent
infection or illness (i.e. recurrence or persistence of AIDS-defining conditions or other serious infections).
Recent (within 30 days or request or while patient was on current medication regimen) genotype and phenotype testing
result was submitted with request for Fuzeon to determine optimal regimen of at least two sensitive and tolerated antiretroviral medications and to eliminate previously ineffective anti-retroviral medications, or there are less than two effective
medications based on sensitivity testing and the patient is at risk for opportunistic infection or death.
Provider is infectious disease or HIV specialist
The patient has a documented adherence level on taking anti-retroviral therapy of greater than 80% and any issue that may
have caused a decrease in adherence in the past (difficulty of dosing schedule, etc.) has been addressed.
If the patient is currently taking Stribild, Triumeq, Complera or Atripla, documentation has been submitted indicating the medical
necessity for utilizing Fuzeon in combination with these agents.
If all of the above conditions are met, the request will be approved with a 16-week duration; if all of the above criteria are not met,
the request is referred to a Clinical reviewer/Medical Director for medical necessity review.
PA CRITERIA FOR RE-APPROVAL:
Documentation of current background drug therapy (Fuzeon is not recommended as monotherapy or to be used without
optimal oral therapy).
For the initial reauthorization: documentation submitted of a viral load drop of > 0.7 log decrease from baseline after 12
weeks of starting therapy for requests to continue therapy beyond 16 weeks, or there is documentation provided that the
patient has documented clinical improvement (i.e. increased CD4 count) with treatment.
After the initial reauthorization: documentation submitted of current (within the past 30 days) CD 4 count and HIV RNA viral
load.
Provider is infectious disease or HIV specialist
If the patient has been on Fuzeon therapy AND there is an increase of at least 2 log in viral load or a 30% decline in CD4
counts from baseline then current phenotype/genotype testing (within the past 30 days) must be submitted to indicate
continued susceptibility of the HIV virus to Fuzeon.
If all of the above conditions are met, the request will be approved for up to a 6 month duration; if all of the above criteria are not met,
the request is referred to a Clinical reviewer/Medical Director for medical necessity review.
FDA INDICATION:
Fuzeon is indicated for use in combination with other antiretroviral agents for the treatment of HIV-1 infection in treatment
experienced patients with HIV-1 replication despite ongoing antiretroviral therapy.
DOSAGE AND ADMINISTRATION: The recommended dose of Fuzeon is 90 mg (1mL) twice daily injected subcutaneously into the
upper arm, anterior thigh, or abdomen. In pediatric patients 6 through 16 years of age, the recommended dosage of Fuzeon is
2mg/kg twice daily up to a maximum dose of 90mg twice daily injected subcutaneously into the upper arm, anterior thigh, or abdomen.
Table 1:
NRTI
s
Generic (Retrovir
(Brand; ®
abbreviation)
Zidovudine
; AZT, ZDV)
NNRTIs
Generic (Brand)
®
Nevirapine (Viramune &
®
Viramune XR )
PIs
Generic (Brand)
®
Indinavir (Crixivan )
®
Didanosine (Videx ; ddI)
®
Delavirdine (Rescriptor )
®
Ritonavir (Norvir ) under study
in neonates
®
Nelfinavir (Viracept )
®
Tenofovir disoproxil (Viread )
®
Stavudine (Zerit ; d4T)
®
Lamivudine (Epivir ; 3TC)
®
Abacavir (Ziagen ; ABC)
Abacavir/Lamivudine/Zidovudine
®
(Trizivir )
®
Lamivudine/Zidovudine (Combivir )
®
Emtriva/Viread (Truvada )
®
Telbivudine (Tyzeka )
Revision/Review Date: 2/2016
®
Efavirenz (Sustiva )
®
Etravirine (Intelence )
®
Saquinavir (Invirase -HGC)
Efavirenz + Tenofovir +
®
Emtricitabine (Atripla )
Rilpivirine (Edurant)
Lopinavir + Ritonavir
®
(Kaletra )
®
Atazanivir (Reyataz )
®
Tipranavir (Aptivus )
®
Darunavir (Prezista )
®
Fosamprenavir (Lexiva )
Nelfinavir (Viracept
46
Misc.
Classification
Generic
ENRTY INHIBITORS
Celsentri,(Brand)
Maraviroc
®
(Selzentry )
INTEGRASE INHIBITOR
®
Raltegravir (Isentress )
INTEGRASE INHIBITOR
Elvitegravir, cobicistat,
emtricitabine, tenofovir,
disoproxil fumarate
(Stribild®)
INTEGRASE INHIBITOR
Dolutegravir (Tivicay®)
Field Name
Prior Authorization
Group Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber
Restrictions
Coverage Duration
Other Criteria
Field Description
Agents to Treat Gaucher’s Disease
Cerdelga® (Eliglustat Tartrate), Cerezyme ® (Imiglucerase), Vpriv®
(velaglucerase alfa), Elelyso® (taliglucerase alfa), Zavesca® (miglustat)
Medically accepted indications are defined using the following sources:
the Food and Drug Administration (FDA), Micromedex, American
Hospital Formulary Service (AHFS), United States Pharmacopeia Drug
Information for the Healthcare Professional (USP DI), and the Drug
Package Insert (PPI).
None
See “Other Criteria”
See “Other Criteria”
MD is a specialist in treatment of Gaucher’s Disease (hematologist or
geneticist), or is in consultation with a specialist including
endocrinologists, hematologists, and geneticists.
If all of the conditions are met, the request will be approved with 6month duration. If all of the criteria are not met, the request is referred to
a clinical reviewer for medical necessity review.
Initial Authorization:
Cerezyme®, Vpriv®, or Elelyso® initial authorization:
Patient has a confirmed diagnosis of Gaucher’s disease, type
1 (GD1)
Request is for an FDA approved dose
Zavesca® initial authorization:
Patient has a confirmed diagnosis of Gaucher’s disease, type
1 (GD1)
Documentation has been provided with medical reason why
patient is unable to use Cerezyme®, Vpriv®, or Elelyso® to
manage their medical condition
Request is for an FDA approved dose
Cerdelga® initial authorization:
Patient is 18 years of age or older.
Patient has a confirmed diagnosis of Gaucher’s disease, type
1 (GD1) and is a CYP2D6 extensive metabolizer (EM),
intermediate metabolizer (IM) or poor metabolizer (PM), as
detected by an FDA-approved test.
Patient is not concomitantly taking a moderate or strong
CYP3A inhibitor (e.g. ketoconazole, fluconazole) or a Class
IA or Class III antiarrhythmic.
Patient has no pre-existing cardiac disease or long QT
syndrome.
The patient has a documented (consistent with pharmacy claims
data, OR for new members to the health plan consistent with
medical chart history) adequate trial (including dates and doses)
of Cerezyme®, Vpriv®, or Zavesca®, or has a documented
47
medical reason for not utilizing these therapies to manage their
condition.
Re-Authorization criteria for all agents:
Documentation has been provided that patient has obtained
clinical benefit from medication (e.g. increased platelet count,
improvement in anemia, PFT’s, improvement in radiographic
scans, improved quality of life,)
Request is for an FDA approved dose
Revision/Review
Date 4/2016
Medical Director/clinical reviewer must override criteria when, in
his/her professional judgement, the requested item is medically
necessary.
48
Prior Authorization Group
Description
Drug(s)
Covered Uses
Exclusion Criteria
Required Medical Information
Age Restrictions
Prescriber Restrictions
Coverage Duration
Other Criteria
GONADOTROPIN RELEASING HORMONE AGONISTS (GNRH)
Degarelix Acetate (Firmagon), Goserelin Acetate (Zoladex), Histrelin Acetate
(Supprelin LA, Vantas), Leuprolide Acetate (Lupron, Eligard), Lupron Depot,
Lupron Depot-Ped, Nafarelin (Synarel), Triptorelin Pamoate (Trelstar Depot,
Trelstar LA, Trelstar Mixject), and newly marketed GnRH agonists.
Medically accepted indications are defined using the following sources: the Food and
Drug Administration (FDA), Micromedex, American Hospital Formulary Service
(AHFS), United States Pharmacopeia Drug Information for the Healthcare
Professional (USP DI), the Drug Package Insert (PPI), and/or per the National
Comprehensive Cancer Network (NCCN), the American Society of Clinical
Oncology (ASCO), the American College of Obstetricians and Gynecologists
(ACOG), or the American Academy of Pediatrics (AAP) standard of care guidelines.
None
None
None
None
If all of the conditions are met, the request will be approved for up to 6 months for
treatment of prostate/breast cancer, endometriosis or central precocious puberty and
up to 3 months or as recommended per FDA approved indications and/or as defined
by the medical compendium as defined above and/or per the NCCN, ASCO, ACOG,
or AAP standard of care guidelines. If the conditions are not met, the request will be
sent to a Medical Director/Clinical Reviewer for medical necessity review.
INITIAL AUTHORIZATION
If the medication request is for the treatment of central precocious puberty
(CPP ) patient may be authorized either Lupron-Depot Ped® OR Supprelin
LA® for the treatment of the condition as long as there is a clinical diagnosis
of CP P with onset of secondary sexual characteristics less than age 8 in
females and age 9 in males and ALL of the following apply to the patient:
Diagnosis is confirmed by a pubertal response to a GnRH stimulation test
and/or measurement of gonadotropins (FSH/LH), and bone age advanced 1
year beyond chronological age.
If basal levels of LH are markedly elevated [e.g. more than 5mlU/ml (where
IU- International units)] in a child with precocious puberty, then a diagnosis of
Gonadotropin Dependent Precocious Puberty (GDPP) can be made without
proceeding to a GnRH stimulation test.
Patients with low or intermediate basal levels of LH should have a GnRH
stimulation test to clarify the diagnosis.
2. There are documented baseline evaluations (including ultrasound, CT, MRI,
and laboratory levels) to rule out a tumor.
For all other indications, if the medication request is for any other GnRH
agonist other than Lupron®, the patient has a documented (consistent with
pharmacy claims data, OR for new members to the health plan consistent
with medical chart history) treatment failure after receiving an adequate trial
(including dates of 3 months or more of therapy) of Lupron® and/or has
49
another documented medical reason (intolerance, hypersensitivity,
contraindication, etc.) for not utilizing Lupron® to treat their medical
condition.
If the diagnosis is HER2 positive breast cancer, and the request is for
Zoladex (goserelin), no prior trial of a GNRH is required for that patient.
If the medication request is for the treatment of advanced prostate cancer
(Stage III or Stage IV) then the patient must be an adult male (≥18 y/o).
If the medication request is for the treatment of a confirmed diagnosis of
endometriosis, the patient is an adult female (≥18 y/o) who does not have
documented Osteoporosis and documentation has been provided that the
patient has had an adequate trial and failure with conservative treatment (i.e.
analgesics, oral contraceptives).
If the medication request is for the treatment of fibroids, the patient is an
adult female (≥18 y/o) and ONE of the following apply to the patient:
The patient is anemic (Hgb < 10.2 g/dl or Hct of < 30%) attributed to
fibroids and the patient has had a one to three month trial of iron therapy
alone which is (consistent with pharmacy claims data, OR for new members
to the health plan consistent with medical chart history) to try and correct the
anemia or there is a medical reason (intolerance, hypersensitivity,
contraindication, etc.) for not using iron alone to manage the anemia.
2. The patient requires the medication to decrease uterine volume as a result
of uterine fibroids to manage symptoms (i.e. pelvic pressure, pelvic
fullness, urinary frequency, nocturia, constipation and/or anemia) and for
shrinkage of size to allow surgical intervention.
If the medication request is for the treatment of endometrial thinning,
documentation was submitted indicating the patient is scheduled for
endometrial ablation for dysfunctional uterine bleeding.
Prescribed dosing of GnRH agonist is within FDA approved indications
and/or is supported by the medical Compendium as defined by the Social
Security Act and/or per the NCCN, ASCO, ACOG or AAP standard of care
guidelines.
The medication is recommended and prescribed by a specialist in the field to
treat the patient’s respective medical condition.
REAUTHORIZATION :
The prescribing physician has provided documentation as to the clinical
benefits of the medication supporting continued treatment, OR the
medication is being continued in accordance with the recommended time as
defined by FDA drug package insert, and/or per recommendations of the
medical compendium as described above, and/or per the NCCN, ASCO,
50
ACOG or AAP standard of care guidelines.
Review Date 2/2016
If the medication reauthorization is for endometriosis ALL of the following
apply to the patient:
If the request is for a continuation of treatment exceeding 6 months, the
patient is receiving or will be prescribed “add back” hormonal therapy
(norethindrone acetate 5 mg daily or conjugated estrogen therapy)
{consistent with pharmacy claims data, OR for new members to the health
plan consistent with medical chart history}, OR if the patient has a
documented medical reason for not being able to take “add back” therapy,
the patient is receiving or is intended to receive anti-osteoporosis therapy
(e.g. alendronate or risedronate) {consistent with pharmacy claims data, OR
for new members to the health plan consistent with medical chart history}.
If the patient received > 6 to 11 months cumulative doses of the GnRH
agonist a Dexa scan was performed and the results were submitted with the
medication request, indicating that the patient does not have documented
Osteoporosis AN D the patient is receiving calcium supplementation (1200
mg /day) and vita min D (400-800 units/day), which is (consistent with
pharmacy claims data, OR for new members to the health plan consistent
with medical chart history).
The patient has not received cumulative doses of the GnRH agonist up to or
greater than 12 months of therapy.
If the medication reauthorization is for fibroids, the patient has not received
cumulative doses of the GnRH agonist up to or greater than 6 months of
therapy, and documentation that the drug is being used prior to surgery.
If the medication reauthorization is for central precocious puberty, the
child is male and < 12 years or female and < 11 years of age OR the child is
male and is > 12 years of age or a female that is > 11 years of age, has an
acceptable documented medical reason to continue treatment, and
documentation of current height and bone age (every 6-12 months).
The medication is recommended and prescribed by a specialist in the field to
treat the member’s respective medical condition
Prescribed dosing of medication is within FDA approved indications and/or
supported by the medical compendium as de fined by the Social Security Act
and/or per the NCCN, ASCO, ACOG or AAP standard of care guidelines.
NOTE: Clinical reviewer must override criteria when, in his/her professional judgment,
the requested item is medically necessary.
51
Field Name
Prior Authorization Group
Drug(s)
Field Description
Growth Hormone
Somatropin (Genotropin, Genotropin MiniQuick,
Humatrope, Norditropin FlexPro, Nutropin AQ, Nutropin
AQ NuSpin, Omnitrope, Saizen, Tev-Tropin), and newly
marketed growth hormone agents.
Covered Uses
Medically accepted indications are defined using the following
sources: the Food and Drug Administration (FDA),
Micromedex, American Hospital Formulary Service (AHFS),
United States Pharmacopeia Drug Information for the
Healthcare Professional (USP DI), the Drug Package Insert
(PPI), or disease state specific standard of care guidelines.
Treatment of idiopathic short stature (ISS)-not a covered benefit
Exclusion Criteria
and will not be approved
Required Medical Information See “other criteria”
Age Restrictions
N/A
MD is an endocrinologist
Prescriber Restrictions
Coverage Duration
If all of the conditions are met, the initial request will be
approved with a 6-month duration, and requests for
reauthorization will be approved for a 12 month duration. If the
conditions are not met, the request will be sent to a Medical
Director/clinical reviewer for medical necessity review.
Other Criteria
1. For patients with growth hormone deficiency states
(adult and pediatric) either the appropriate information,
diagnosis &/or laboratory information has been provided
with the request. This includes Growth Hormone (GH) level
in response to the preferred stimulatory test (i.e. Insulin
Tolerance Test or Glucagon or Arginine) &/or Insulin
Growth Factor 1 level indicative of GH deficiency. In
addition, for pediatric patients, documentation of his or her
growth velocity (below 4.5 cm/year), their height percentile
for age and gender, how far below the standard deviation
(SD) their height is for their age (at least 2 SD below
normal), how far below the SD their height is from their
mid-parent height percentile (at least 2 SD below), and
bone age (at least 2 SD below) the mean for age.
AND
2. If the patient is 17 years of age or older and was
diagnosed with childhood onset growth hormone
deficiency, documentation was provided that indicates
GH therapy is still medically necessary despite a 1-3
month trial off the medication (GH therapy discontinued
for 1-3 months and resulting GH/IGF-1levels are low).
AND
3. If the patient is 17 years of age or older and still
requires GH therapy and is receiving childhood dosing
versus lower adult dosing, appropriate documentation
was provided (i.e. patient has not reached maximum predicted
height or is still having clinical response) documenting the
medical necessity of childhood GH dosing.
AND
4. If the request is not for Humatrope brand growth
52
hormone, the provider submitted a documented medical
reason (i.e. intolerance) why it is medically necessary to
utilize some other brand formulation of growth hormone.
Revision/Review Date
02/2016
Medical Director/clinical reviewer must override criteria
when, in his/her professional judgement, the requested item
is medically necessary.
53
Field Name
Prior Authorization
Group Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber
Restrictions
Coverage Duration
Other Criteria
Hepsera
Field Description
®
Hepsera® (adefovir)
Medically accepted indications are defined using the following sources:
the Food and Drug Administration (FDA), Micromedex, American
Hospital Formulary Service (AHFS), United States Pharmacopeia Drug
Information for the Healthcare Professional (USP DI), the Drug Package
Insert (PPI), or disease state specific standard of care guidelines.
N/A
See “other criteria”
N/A
N/A
If the above conditions are met, the request will be approved with a 12
month duration; If the conditions are not met, the request will be sent to
a Medical Director/clinical reviewer for medical necessity review.
Initial authorization:
Diagnosis of hepatitis B.
AND
Submitted current laboratory values indicating evidence of active
viral replication.
AND
Submitted current laboratory values indicating persistent elevations
in ALT or AST or histologically active disease.
AND
Documented
treatment failure with or contraindication to
Baraclude® (entecavir) therapy.
AND
Patient under the care of a gastroenterologist.
Revision/Review
Date 02/2016
Medical Director/clinical reviewer must override criteria when, in
his/her professional judgement, the requested item is medically
necessary.
54
PRIOR AUTHORIZATION PROTOCOL FOR TREATMENT OF HEREDITARY ANGIOEDEMA
Cinryze
Berinert
Kalbitor
Firazyr
Ruconest
FORMULARY STATUS: Non-Formulary, Require PA
All requests MUST meet the following requirements:
•
Confirmed diagnosis of hereditary angioedema (HAE) with measurement of C1-INH
antigenic level, C1-INH functional level, and C4 level
•
MD must be an immunologist, allergist or hematologist
•
The patient is not taking ACE inhibitors or estrogen replacement
•
Documentation submitted indicates the medication is being prescribed for an FDA
approved indication at FDA approved dose.
For acute treatment:
•
If all of the above conditions are met, the request will be approved for (2) doses with 5 refills.
For prophylaxis treatment:
•
The patient has a history of at least two severe attacks/month with swelling of the face, throat, or
GI tract, and chart notes have been submitted indicating the date and severity of attack.
•
The patient has tried and failed and/or has a documented medical reason (intolerance
or contraindication) for not using danazol, stanozolol, or oxandrolone.
•
If all of the above conditions are met, the request will be approved for three month duration. If
all of the above criteria are not met, the request is referred to a clinical reviewer for medical necessity
review.
Renewal Criteria:
•
Documentation was submitted that the patient has clinically benefited from medication
with reduced attacks.
•
Documentation submitted indicates the medication is being prescribed for an FDA
approved indication at FDA approved dose.
•
Approval duration for acute treatment is 2 doses with 5 refills
•
Approval duration for prophylaxis treatment is 3 months.
If all of the above criteria are not met, the request is referred to a clinical reviewer for medical
necessity review.
References
1. Craig T, Pürsün E, Bork K, Bowen T, Boysen H et al. WAO Guideline for the Management of
Hereditary Angioedema. World Allergy Organization Journal 2012; 5(12): 182-199. WAO Guideline for
the Management of Hereditary Angioedema, WAO Journal, December
2012 http://www.waojournal.org/content/pdf/1939-4551-5-12-182.pdf
2. http://www.haea.org/wp/wp-content/uploads/2013/09/guidelines.pdf
3. http://www.haea.org/professionals/diagnosing-hae/
Revision/Review Date: 11/2015
55
Field Name
Prior Authorization Group Desc
Drug(s)
Covered Uses
Exclusion Criteria
Required Medical Information
Age Restrictions
Prescriber Restrictions
Coverage Duration
Other Criteria
Field Description
HYALURONIC ACID DERIVATIVES
EUFLEXXA is PREFERRED agent
Gel-One
Hyalgan
Monovisc
Orthovisc
Supartz
Synvisc
Synvisc One
Any other newly marketed Hyaluronic Acid derivative
*Medically accepted indications are defined using the following sources: the Food
and Drug Administration (FDA), Micromedex, American Hospital Formulary
Service (AHFS), United States Pharmacopeia Drug Information for the Healthcare
Professional (USP DI), or the Drug Package Insert (PPI).
None
See other criteria
None
None
If all of the criteria is met, the request will be approved for one complete course of treatment
(based on the FDA labeled dose of the drug requested). If all of the criteria is not met, the
request is referred to a Medical Director for medical necessity review.
Initial Authorization:
• A diagnosis of Osteoarthritis (OA)/Degenerative joint disease (DJD) of the knee.
• There is documentation (in claim history or provider statement) that the patient recently (over
the past 4 months) has had adequate trials on simple analgesics (acetaminophen containing
products or topical capsaicin cream) & NSAIDS (including two different prescription strength
NSAIDS) on a continuous basis for 3 months without success or has a medical reason
(intolerance, hypersensitivity, contraindication, etc.) for not being able to utilize simple
analgesic products and NSAIDS.
• Documentation has been provided that a steroid injection has been tried and failed, per
affected knee or patient has a medical reason for not being able to utilize steroid injections.
• If the request is for any other product other than Euflexxa, the patient has a documented
medical reason (intolerance, hypersensitivity, contraindication, etc) for not using Euflexxa to
treat their medical condition.
Reauthorization:
• At least 6 months have elapsed since the previous course of HAD therapy for the treated
knee(s).
• Documentation was submitted that the patient had a response to the treated knee (s) that lasted
for > 6 months to previous HAD therapy, as documented by at least ONE of the following:
Decreased joint pain or stiffness, improved knee range of motion, decrease in midpatellar knee
circumference in millimeters, or synovial effusion absent or volume decreased.
• Documentation was submitted that the patient has a return of symptoms of osteoarthritis, and
has been retreated with NSAIDS and simple analgesics
(acetaminophen containing products or topical capsaicin cream) without success,
or has a medical reason (intolerance, hypersensitivity, contraindication, etc) for not being able to
utilize simple analgesic products and NSAIDS.
• If the request is for any other product other than Euflexxa, the patient has a documented
medical reason (intolerance, hypersensitivity, contraindication, etc) for not using Euflexxa to
treat their medical condition.
If all of the criteria is not met, the request is referred to a Medical Director for medical
necessity review.
Revision/Review Date: 2/2016
56
PRIOR AUTHORIZATION CRITERIA for Ibrance
PREFERRED STATUS: REQUIRES Prior Authorization
Ibrance® (Palbociclib): 75mg, 100mg, 125mg capsules
INITIAL CRITERIA FOR IBRANCE:
Patient is 18 years of age or older
AND
Documentation has been submitted that patient has a diagnosis of estrogen receptor (ER)
positive, human epidermal growth factor receptor 2 (HER2) negative advanced or
(metastatic) breast cancer
AND
Patient is one of the following:
postmenopausal as demonstrated by one of the following: prior bilateral oophorectomy, age
is ≥60 years old, age is < 60 and amenorrheic for 12 months or more in the absence of
chemotherapy, tamoxifen or toremifene, or ovarian suppression (FSH and estradiol in postmenopausal range) and will be using in combination with letrozole
postmenopausal (as described above) who have progressed on endocrine therapy and will be
using in combination with fulvestrant (Faslodex)
premenopausal women who have progressed after receiving a luteinizing hormone-releasing
hormone (LNRH) agonist, and will be using in combination with fulvestrant (Faslodex)
AND
Documentation submitted includes complete blood count with differential (within 30 days of
request).
Prescriber is oncologist.
If all of the above conditions are met, the request will be approved for up to a 2-month duration;
if all of the above criteria are not met, the request is referred to a clinical reviewer for medical
necessity review.
CONTINUATION OF THERAPY FOR IBRANCE:
Repeat complete blood counts with differential were submitted with request (within 30 days of
request).
Documentation submitted indicates that there is no evidence of disease progression on therapy
member has obtained clinical benefit from the medication.
Prescriber is oncologist.
If all of the above conditions are met, the request will be approved for up to a 3-month duration;
if all of the above criteria are not met, the request is referred to a clinical reviewer for medical
necessity review.
NOTE: Medical Director/clinical reviewer must override criteria when, in his/her professional
judgment, the requested itemis medically necessary.
Revision/Review Date: 4/2016
57
PRIOR AUTHORIZATION CRITERIA for Idiopathic Pulmonary Fibrosis
(IPF)
PREFERRED STATUS: REQUIRE Prior Authorization
Ofev® (Nintedanib Esylate): 100mg,150mg capsules
Esbriet® (Pirfenidone): 267mg capsule
INITIAL CRITERIA FOR IDIOPATHIC PULMONARY FIBROSIS:
Patient is 18 years of age or older
Documentation submitted includes patient’s complete medical history/co-morbidities
Confirmed diagnosis of Idiopathic Pulmonary Fibrosis as demonstrated by a High Resolution CT
scan with “honeycombing” or “ground glass opacities” or lung biopsy, and other known causes
of interstitial lung disease have been excluded
MD is a pulmonologist or lung transplant specialist
Pulmonary function test indicate patient has Forced Vital Capacity (%FVC) greater than or equal
to 50% within 30 days of request
Baseline ALT, AST, and bilirubin has been submitted within 30 days of request
Patient does NOT have severe hepatic impairment (Child Pugh C)
If the request is for Ofev, the patient is not currently taking a P-glycoprotein or CYP3A4 inducer
(e.g. rifampin, carbamazepine, phenytoin, St. John’s Wort)
If the request is for Ofev and the patient has history of coronary artery disease, documentation
submitted indicates that the prescriber has consulted with cardiology
If the request is for Esbriet, the patient is not currently taking a strong CYP1A2 inducer (e.g.
carbamazepine, rifampin) or a strong CYP1A inhibitors (e.g. fluvoxamine)
Documentation has been provided that the patient does not smoke
If all of the above conditions are met, the request will be approved for a 3 month duration; if all of the
above criteria are not met, the request is referred to a Medical/clinical reviewer for medical necessity
review.
REAUTHORIZATION CRITERIA FOR IDIOPATHIC PULMONARY FIBROSIS:
MD is a pulmonologist or lung transplant specialist
Repeat ALT, AST and bilirubin within 30 days of request
If the ALT/AST are more than 3-5 times the upper limit of normal, the requested dose is being
reduced based on the manufacturer labeling.
If ALT/AST is more than 5 times the upper limits of normal or increased ALT/AST with
hyperbilirubinemia the medication should be discontinued
Documentation submitted indicates that the member has obtained clinical benefit from the
medication
Documentation has been provided that the patient does not smoke
If all of the above conditions are met, the request will be approved for a 6 month duration; if all of the
above criteria are not met, the request is referred to a Medical Director/clinical reviewer for medical
necessity review.
NOTE: Medical Director/Clinical reviewer must override criteria when, in his/her professional
judgment, the requested item is medically necessary.
Revision/Review Date: 7/2016
Select Health Prior Authorization Criteria for Immunoglobulins (IVIG)
ALL REQUESTS MUST HAVE A CONFIRMED DIAGNOSIS BY A SPECIALIST
FOR ALL INDICATIONS: Patient has documented trial and failure of all other standard of care
therapies as defined per recognized guidelines, or have a documented medical reason why patient is
not able to utilize other standard of care therapy.
IVIG will be considered for the following indications provided the required information is present:
1.
2.
3.
4.
5.
6.
7.
8.
9.
Primary immunodeficiency
Thrombocytopenia purpura, Idiopathic and chronic immune
Kawasaki disease
Chronic B- cell lymphocytic leukemia
Bone marrow transplantation
Pediatric HIV
Multifocal motor neuropathy
Chronic inflammatory demyelinating neuropathy
Guillain-Barre syndrome
If criteria are met, the request will be approved for the duration listed below, if criteria are not met, the
request is referred to a Medical Director/Clinical reviewer for medical necessity review.
Primary immunodeficiency
Congenital agammaglobulinemia
Hypogammaglobulinemia (Common Variable
Immunodeficiency, CVID)
Severe combined immunodeficiency (SCID)
Wiskott-Aldrich syndrome
X-linked agammaglobulinemia or Bruton’s
Hypergammaglobulinemia
X-linked Hyper IgM syndrome
Documentation submitted includes patient’s IgG
level and is below normal level for indication
Clinically significant deficiency of humoral immunity
as evidenced by ONE of the following:
Documented inability to produce an
adequate immunologic response to
specific antigens.
Patient has history of recurrent infections
despite prophylactic antibiotics
Dose does not exceed 400-800mg/kg every 28 days
If criteria is met, approve for 6 months.
Acute : (active bleeding, patients requiring an urgent invasive
procedure, to defer splenectomy, or platelet counts
< 20,000/ul at risk for intra-cerebral hemorrhage or has life
threatening bleeding)
Dose does not exceed 1g/kg daily for up to 2 days,
or 400mg/kg daily for 5 days
Thrombocytopenia purpura, Idiopathic and
chronic immune
Chronic:
Duration of illness of greater than 6 months
Patient has documented trial and failure of
corticosteroids and splenectomy, or has a
documented medical reason why they are not able
to use corticosteroids or patient is at high risk for
post-splenectomy sepsis.
Dose does not exceed 1g/kg daily for up to 2 days,
or 400mg/kg daily for 5 days
If criteria is met, approve for up to 5 days.
59
Kawasaki disease
IVIG is being given with high dose aspirin
Requested dose does not exceed a single 2g/kg dose
or a dose of 400mg/kg for five consecutive days
If criteria is met, approve for up to 5 days.
Chronic B-cell lymphocytic leukemia
Patient’s IgG level has been provided, and is
< 500mg/dL
The patient has history of severe bacterial infections
Dose does not exceed 400mg/kg every 3-4 weeks
If criteria is met, approve for 3 months.
Bone marrow transplantation
Confirmed bone marrow transplant within last 100
days.
Patient’s IgG level has been provided, and is
< 400mg/dL
Dose does not exceed 500mg/kg/wk for the first 100
days post- transplant
If criteria is met, approve for 3 months.
Pediatric HIV
Diagnosis of HIV
Patient is < 13 years of age
Patient’s IgG level has been provided, and is
< 400mg/dL
Clinically significant deficiency of humoral immunity
as evidenced by ONE of the following:
Documented inability to produce an
adequate immunologic response to
specific antigens.
Patient has history of recurrent bacterial
infections despite prophylactic antibiotics
Dose does not exceed 400mg/kg every 28 days
OR
If criteria is met, approve for 3 months.
Multifocal motor neuropathy (MMN)
Duration of symptoms has been at least 1 month
with disability.
Documentation submitted includes nerve
conduction studies were completed to rule out
other possible conditions, and confirms the
diagnosis of MMN.
Dose does not exceed 2g/kg/month. This dose can
be given over two to five days.
If criteria is met, approve for up to 5 days for 3 months.
Chronic inflammatory demyelinating neuropathy
(CIDP)
60
Duration of symptoms has been at least 2 months
with disability.
Documentation submitted includes nerve
conduction studies were completed or nerve biopsy
to rule out other possible conditions, and confirms
the diagnosis of CIDP.
Patient has documented trial and failure of
corticosteroids, or has a documented medical
reason why they are not able to use corticosteroids
to treat the condition.
Dose does not exceed 2g/kg/month. This dose can
be given over two to five days.
If criteria is met, approve for up to 5 days for 3 months.
Guillain-Barre syndrome
Documentation submitted indicates severe disease
with the inability to walk without aid
Onset of symptoms within the last 4 weeks
Dose does not exceed 2g/kg/month
If criteria is met, approve for 3 months.
Any other medically accepted indication
For any other indication, medical recommendation
must have a I, IIa or IIb recommendation, and be
used for a medical condition that is supported by
the medical compendium (Micromedex, American
Hospital Formulary Service, Drug Points, and Drug
Package Insert) as defined in the Social Security Act
1927, and/or per recognized standard of care
guidelines.
Patient has documented trial and failure of all other
standard of care therapies as defined per recognized
guidelines, or has a documented medical reason
why patient is not able to utilize other standard of
care therapy.
If criteria is met, approve for 3 months
Review/Revision Date 11/2015
61
Field Name
Field Description
Prior Authorization Group
Drugs
Injectable Bisphosphonates & Skeletal Related Events
Preferred: Pamidronate disodium (Aredia®), Zoledronic Acid (Zometa
®), Nonpreferred: Denosumab (Xgeva®)
Covered Uses
Exclusion Criteria
The request is for an FDA approved indication or for a medically
accepted indications as defined or as supported by the medical
compendium (Micromedex, American Hospital Formulary Service
(AHFS), United States Pharmacopeia Drug Information for the
Healthcare Professional (USP DI) , Drug Package Insert) as defined in
the Social Security Act 1927, or per the National Comprehensive Cancer
Network (NCCN), the American Society of Clinical Oncology (ASCO),
or the National Institutes of Health (NIH) Consensus Panel standard of
care guidelines.
N/A
Required Medical Information
See “Other Criteria”
Age Restrictions
N/A
Prescriber Restrictions
Prescriber is an oncologist
Coverage Duration
6 months
Other Criteria
The request is for an approved/accepted indication at an
approved dose
Documentation has been provided that patient has a creatinine
clearance > 30mL/min.
If the request is for a brand name agent, the patient has a
documented trial and failure of generic Pamidronate (Aredia)
OR zoledronic acid (Zometa) that is consistent with claims
history, or has a documented medical reason (intolerance,
hypersensitivity, contraindication, etc) for not utilizing one of
these agents to manage their medical condition.
If the request is for denosumab (Xgeva) for treating Giant cell
tumor of bone, documentation has been submitted that the tumor
is unresectable or that surgical resection is likely to result in
morbidity.
If these conditions are not met, the request will be sent to a Medical
Director/clinical reviewer for medical necessity review.
Revision/Review 2/2016
Medical Director/clinical reviewer must override criteria when, in
his/her professional judgement, the requested item is medically
necessary.
62
Field Name
Field Description
Prior Authorization Group
Drug(s)
Covered Uses
KUVAN®
Kuvan® (Sapropterin Dihydrochloride)
*Medically accepted indications are defined using the following sources: the Food
and Drug Administration (FDA), Micromedex, American Hospital Formulary Service
(AHFS), United States Pharmacopeia Drug Information for the Healthcare
Professional (USP DI) , and the Drug Package Insert).
None
See “Other Criteria”
None
Specialist experienced in treating PKU
Exclusion Criteria
Required Medical Information
Age Restrictions
Prescriber Restrictions
Coverage Duration
Other Criteria
Initial: If the criterion is met, the request will be approved for a duration of 1 month;
if the above conditions are not met, the request will be referred to a clinical reviewer
for medical necessity review.
1st Reauthorization: If the criteria is met, the request will be approved for a
duration of 1 month for patients who require a dose increase to 20 mg/kg/day due to
non-responsiveness and for all other patients the request will be approved for a
duration of 3 months; if the above conditions are not met, the request will be referred
to a clinical reviewer/Medical Director for medical necessity review.
2nd Reauthorization and Thereafter: If the criterion is met, the request will be
approved for a duration of 4 months; if the above conditions are not met, the request
will be referred to a clinical reveiwer/Medical Director for medical necessity review.
INITIAL AUTHORIZATION:
• Documentation of a confirmed diagnosis of Phenylketonuria (PKU) by a specialist
experienced in treating PKU
• Documentation of the patient’s baseline blood Phe level. (within 30 days of the
request)
• Documentation consistent with order forms OR receipts (within 30 days of request)
that the patient is currently utilizing a Phe restricted diet with Phe-free medical
products/foods in conjunction with dietician or nutritionist. (Examples include
Phenyl-Free® (phenylalanine free diet powder), Loplex, Periflex, Phlex-10, PKU 2,
PKU 3, XPhe Maxamaid, XPhe Maxamum,)
• Documentation of the patient’s current weight.
• The medication is being prescribed at a dose no greater than the FDA approved
maximum initial dose of 10 mg/kg/day-20mg/kg/day.
PA CRITERIA FOR 1st REAUTHORIZATION:
Patients that were dosed at 20mg/kg/day (initial auth) and did not have a decrease in
Phe level of at least 30% from baseline, are considered NON RESPONDERS and NO
ADDITIONAL TREATMENT will be authorized.
• Documentation of the patient’s current weight.
• Documentation consistent with current order forms OR receipts that the patient is
currently utilizing a Phe restricted diet with Phe-free medical products/foods in
conjunction with dietician or nutritionist. (Examples include Phenyl-Free®
(phenylalanine free diet powder), Loplex, Periflex, Phlex-10, PKU 2, PKU 3, XPhe
Maxamaid, XPhe Maxamum,)
• Documentation of at least two separate blood Phe level results (within 30 days of
request).
63
• The medication is being prescribed at an FDA approved dosage.
PA CRITERIAFOR 2nd REAUTHORIZATIONAND THEREAFTER:
• Documentation of the patient’s current weight.
• Documentation consistent with order forms OR receipts (within 30 days of request)
that the patient is currently utilizing a Phe restricted diet with Phe-free medical
products/foods in conjunction with dietician or nutritionist. (Examples include
Phenyl-Free® (phenylalanine free diet powder), Loplex, Periflex, Phlex-10, PKU 2,
PKU 3, XPhe Maxamaid, XPhe Maxamum, Low-Phe natural foods, Low-protein
specialty foods, Phe-free formula, or Phe-free protein replacement bars, tablets,
capsules, etc.)
• Documentation of at least two separate blood Phe level results (within 60 days of
request).
• The medication is being prescribed at an FDA approved dosage.
If the above conditions are met, the request will be approved for a duration of 4
months; if the above conditions are not met, the request will be referred to a clinical
reviewer/Medical Director for medical necessity review.
Last review 2/2016
NOTE: Clinical reviewer/Medical Director must override criteria when, in his/her
professional judgment, the requested item is medically necessary.
64
Field Name
Field Description
Prior Authorization Group
Drug(s)
Covered Uses
LEMTRADA®
Lemtrada®
Medically accepted indications are defined using the following sources: the Food and
Drug Administration (FDA), Micromedex (DrugPoint or DRUGDEX), American
Hospital Formulary Service (AHFS – accessed via Lexicomp), United States
Pharmacopeia Drug Information for the Healthcare Professional (USP DI), and the
Drug Package Insert.
Patients that are infected with HIV (Human Immunodeficiency Virus)
See “Other Criteria”
Patients must be 17 years age or older
Prescriber must be a neurologist
If all of the criteria are met, the initial request will be approved for 5 vials (60mg).
For continuation of therapy, if all criteria are met, the request will be approved for 3
vials (36mg). If all of the above criteria are not met, the request is referred to a
Clinical Reviewer for medical necessity review.
***Note Lemtrada® is only available through a restricted distribution program that
both patient and physician must be enrolled.
INITIAL AUTHORIZATION:
The patient is ≥ 17 years old with a clinical diagnosis of a relapsing form of
multiple sclerosis.
Documentation of the following lab values have been submitted within 30 days of
Exclusion Criteria
Required Medical Information
Age Restrictions
Prescriber Restrictions
Coverage Duration
Other Criteria
request:
-HIV testing
-Thyroid function tests
-Complete blood count with differential
-Serum creatinine
-Urinalysis with cell counts
-ECG (within 3 months)
-baseline skin exam (for melanoma)
Clinical or diagnostic information was submitted that indicates that that patient
has a documented (consistent with pharmacy claims data OR for new members to
the health plan consistent with medical chart history) treatment failure after
receiving an adequate trial (including dates, doses of 6 months or more of each
therapy) of two of the following: peginterferon Beta- 1A (Plegridy®), glatiramer
acetate (Copaxone®), fingolimod hcl (Gilenya®), or dimethyl fumarate
(Tecfidera®), AND THEN Tysabri®, or has a documented medical reason
(intolerance, hypersensitivity, etc) for not utilizing these therapies for a minimum
of 6 months each to manage their medical condition.
Documentation has been provided that the patient will be taking formulary antiherpetic prophylaxis for a minimum of 60 days beginning day one of treatment.
Lemtrada® is being prescribed at an FDA approved dosage
PA CRITERIA FOR REAUTHORIZATION:
The patient is ≥ 17 years old with a clinical diagnosis of a relapsing form of
multiple sclerosis.
A period of 12 months has elapsed since previous treatment.
Documentation of the following labs values have been submitted with request:
66
- HIV testing (within 30 days of request)
-Thyroid function tests (every 3 months from initial dose)
-Complete blood count with differential (every month from initial dose)
-Serum creatinine (every month from initial dose)
-Urinalysis with cell counts (every month from initial dose)
-ECG (within 3 months)
-annual skin exam (for melanoma)
Review Date 2/2016
Documentation has been provided that the patient will be taking formulary antiherpetic prophylaxis for a minimum of 60 days beginning day one of treatment.
Lemtrada® is being prescribed at an FDA approved dosage
NOTE: Clinical reviewer must override criteria when, in his/her professional judgment,
the requested item is medically necessary.
67
Field Name
Prior Authorization Group
Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber Restrictions
Coverage Duration
Other Criteria
Field Description
Low Molecular Weight Heparins PA Criteria
Arixtra® (fondaparinux), Fragmin® (daltepain), Lovenox®
(enoxaparin) and any newly marketed low molecular weight
heparin agent.
Medically accepted indications are defined using the following sources: the
Food and Drug Administration (FDA), Micromedex, American Hospital
Formulary Service (AHFS), United States Pharmacopeia Drug Information for
the Healthcare Professional (USP DI), the Drug Package Insert (PPI), or disease
state specific standard of care guidelines.
N/A
See “other criteria”
N/A
N/A
If the above conditions are met, the request will be approved:
• For the use in deep vein thrombosis (DVT) and/or pulmonary embolis
(PE) - for up to a 31-day duration (unless greater duration of therapy is
requested and medically necessary then will be approved for up to a 6
month duration).
• For use in pregnant members - for up to a 6 month duration (or up until
the patient’s expected due date, whichever comes first).
• For use in members with cancer - for up to a 6 month duration.
If the conditions are not met, the request will be sent to a Medical
Director/clinical reviewer for medical necessity review.
PA CRITERIA FOR APPROVAL FOR USE IN DEEP VEIN THROMBOSIS
(DVT) AND/OR PULMONARY EMBOLIS (PE):
• The medication is being prescribed for the prevention and/or treatment of
a DVT and/or PE.
• Documentation of the patient’s current weight.
• The medication is being prescribed at a dose that is within FDA approved
guidelines.
• If the request is for a duration of therapy greater than 31 days then a
letter of medical necessity that provides a valid medical reason why the
member cannot be treated with Coumadin or Heparin for long-term
therapy (>31 days) must be submitted.
PA CRITERIA FOR APPROVAL FOR USE IN A PREGNANT MEMBER:
• The medication is being prescribed for the prevention or treatment of a
DVT and/or PE while the member is pregnant.
• Documentation of the patient’s current weight and expected due date
(EDD). If the request is to continue LMWH treatment postpartum then
documentation of the patient’s actual or expected due date and current
weight is required AND THEN up to 6 weeks of additional treatment may
be authorized.
• The medication is being recommended and prescribed by an
obstetrician or a hematologist at a dose that is within FDA approved
guidelines and/or is supported by the medical compendium as
defined by the Social Security Act.
PA CRITERIA FOR APPROVAL FOR USE IN MEMBER WITH CANCER:
• The medication is being prescribed for the prevention or treatment of a
venous thromboembolism (VTE) (a proximal DVT and/or PE) for a
68
member with cancer.
• Documentation of the patient’s current weight.
• The medication is being recommended and prescribed by an
oncologist/hematologist at a dose that is within FDA approved
guidelines and/or is supported by the medical compendium as defined
by the Social Security Act and/or per the National Comprehensive
Cancer Network (NCCN) or American Society of Clinical Oncology
(ASCO) standard of care guidelines.
Revision/Review Date
02/2016
REAUTHORIZATION CRITERIA FOR APPROVAL FOR USE IN MEMBER
WITH CANCER BEYOND SIX MONTHS:
• The medication is being for the prevention and/or treatment of a VTE for a
member with cancer.
• Documentation of the patient’s current weight.
• If the request for a duration of therapy greater than 6 months then a
letter of medical necessity that provides a valid medical reason why
the member needs to continue treatment and cannot be treated with
Coumadin for long-term therapy.
• The medication is being recommended and prescribed by an
oncologist/hematologist at a dose that is within FDA approved
guidelines or is supported by the medical compendium as defined by the
Social Security Act and/or per the National Comprehensive Cancer
Network (NCCN) or American Society of Clinical Oncology (ASCO)
standard of care guidelines.
Medical Director/clinical reviewer must override criteria when, in
his/her professional judgement, the requested item is medically
necessary.
69
Field Name
Prior Authorization
Group Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber Restrictions
Coverage Duration
Other Criteria
Revision/Review Date
04/2016
Field Description
Oncology without specific criteria
Oral and Injectable Oncology Medications without medication specific
criteria
Medically accepted indications are defined using the following
sources: the Food and Drug Administration (FDA), Micromedex,
American Hospital Formulary Service (AHFS), United States
Pharmacopeia Drug Information for the Healthcare Professional (USP
DI) , and the Drug Package Insert, and/or per the National
Comprehensive Cancer Network (NCCN
N/A
See “other criteria”
N/A
Prescriber must be an oncologist
If the criteria are met, the request will be approved for up to 6 month
duration; if the criteria are not met, the request will be referred to a
clinical reviewer for medical necessity review.
All of the following criteria must be met:
Requested indication must be supported by NCCN Category 1
or 2A level of evidence. If the request is for a Category 2B
recommendation then medical documentation has been
provided as to why member is unable to utilize a treatment
regimen with a higher level of evidence (e.g. allergic reaction,
contraindication).
Documentation provided of results of genetic testing where
required per drug package insert.
Documentation provided of results of all required laboratory
values and patient specific information (e.g. weight, ALT/AST,
Creatinine Kinase, etc.) when recommended/required per drug
package insert.
The medication is being prescribed at a dose that is within
FDA approved guidelines.
Medical Director/clinical reviewer must override criteria when, in
his/her professional judgement, the requested item is medically
necessary.
70
PRIOR AUTHORIZATION CRITERIA
SPECIALTY BIOLOGICS FOR ANKYLOSING SPONDYLITIS
ENBREL®(etanercept), HUMIRA® (adalimumab) Preferred
CIMZIA® (certolizumab), SIMPONI®(golimumab), REMICADE®(infliximab), Non-Preferred (2nd line)
PA CRITERIA
Covered Uses
Exclusion
Criteria
CRITERIA DETAILS
All medically accepted indications. Medically accepted indications are defined using the
following sources: the Food and Drug Administration (FDA), Micromedex, American
Hospital Formulary Service (AHFS), United States Pharmacopeia Drug Information for the
Healthcare Professional (USP DI, and the Drug Package Insert.
None
Required
Medical
Information
Documentation was submitted indicating that the member was evaluated for active or
latent TB infection (i.e. tuberculin skin test). See “other criteria”
Age Restrictions
The patient is an adult (≥18 y/o) and has documented ankylosing spondylitis
Prescriber
Restrictions
Prescriber must be a rheumatologist or dermatologist.
If all of the above conditions are met, the request will be approved for up to a 6-month
duration; if all of the above criteria are not met, the request is referred to a clinical reviewer
for medical necessity review.
Other Criteria
INITIAL AUTHORIZATION:
The patient has a documented (consistent with pharmacy claims data, OR for new members
to the health plan consistent with medical chart history) adequate trial of or has a
documented medical reason for not taking at least two nonsteroidal anti-inflammatory drugs
(NSAIDS) to manage their medical condition.
The patient has a documented (consistent with pharmacy claims data, OR for new
members to the health plan consistent with medical chart history) adequate trial of or has a
documented medical reason for not taking a cyclo-oxygenase (COX)-2-selective inhibitors
to manage their medical condition.
Documentation was submitted indicating that the member was evaluated for active or
latent TB infection (i.e. tuberculin skin test).
The medication requested has an FDA approved indication for use in patients with
ankylosing spondylitis and is being recommended and prescribed by a rheumatologist at an
FDA approved dosage.
If the request is for a non-preferred agent, documented (consistent with pharmacy claims
data, OR for new members to the health plan consistent with medical chart history)
adequate trial of the preferred biological agents.
RE – AUTHORIZATION:
The medication is being recommended and prescribed by a rheumatologist at an FDAapproved dosage.
The member has been receiving the medication and documentation was provided that the
prescriber has evaluated the member and recommends continuation of therapy.
Documentation submitted indicates that the member has obtained clinical benefit from
the medication.
If all of the above conditions are met, the request will be approved for a 6-month duration
for Remicade requests and for a 12 month duration for requests for all other medications. If
all of the above criteria are not met, the request is referred to a clinical reviewer for medical
necessity review.
Revision/Review Date: NOTE: Clinical reviewer must override criteria when, in his/her professional
6/2015
judgment, the requested item
Coverage
Duration
is medically necessary.
71
PRIOR AUTHORIZATION CRITERIA
SPECIALTY BIOLOGICAL AGENTS FOR CROHN’S DISEASE
®
HUMIRA (adalimumab) Preferred
REMICADE® (infliximab), CIMZIA® (certolizumab), ENTYVIO®(Vedolizumab) Non - Preferred
PA CRITERIA
Covered Uses
Exclusion
Criteria
Required
Medical
Information
Age Restrictions
Prescriber
Restrictions
Coverage
Duration
Other Criteria
CRITERIA DETAILS
All medically accepted indications. Medically accepted indications are defined using the
following sources: the Food and Drug Administration (FDA), Micromedex, American
Hospital Formulary Service (AHFS), United States Pharmacopeia Drug Information for the
Healthcare Professional (USP DI) and the Drug Package Insert.
None
Documentation was submitted indicating that the member was evaluated for active or
latent TB infection (i.e. tuberculin skin test). See “other criteria”
The member is (≥6y/o) and has a documented clinical diagnosis of moderate to
severely active Crohn’s Disease.
None
If the criterion is met, the request will be approved for up to a 6-month duration. If the
criterion is not met, the request will be referred to a clinician for medical necessity review.
INITIAL AUTHORIZATION:
The patient has a documented (consistent with pharmacy claims data, OR for new
members to the health plan consistent with medical chart history) adequate trial (including
dates and doses) at therapeutic doses or has a documented clinically significant medical
reason for not receiving conventional oral therapy (e.g. azathioprine, corticosteroids, 6mercaptopurine) to manage their medical condition.
The medication requested has an FDA approved indication for use in patients with
moderate to severe active Crohn’s disease and is being recommended and prescribed by a
gastroenterologist at an FDA-approved dosage
If the request is for a non-preferred agent, documented (consistent with pharmacy claims
data, OR for new members to the health plan consistent with medical chart history)
adequate trial of the preferred biological agents.
RE – AUTHORIZATION:
The medication is being recommended and prescribed by a gastroenterologist for an FDA
–approved indication at an FDA-approved dosage.
For members who require Humira 40 mg SC weekly, documentation must be submitted
indicating that the member was compliant (consistent with pharmacy claims) with receiving
at least 16 weeks of continuous Humira therapy every other week prior to the request for
weekly dosing of Humira.
If all of the above conditions are met, the request will be approved for a 6-month duration
for Remicade requests and for a 12 month duration for all other medications; if all of the
above criteria are not met, the request is referred to a clinical reviwere for medical necessity
review.
Review Date: 6/2015
NOTE: Clinical reviewer must override criteria when, in his/her professional
judgment, the requested item is medically necessary.
72
PRIOR AUTHORIZATION CRITERIA
SPECIALTY BIOLOGICAL AGENTS FOR POLYARTICULAR JUVENILE IDIOPATHIC ARTHRITIS
ENBREL® (etanercept) HUMIRA® (adalimumab) – Preferred
ACTEMRA® (tocilizumab) ORENCIA® (abatacept) - Nonpreferred
PA CRITERIA
Covered Uses
Exclusion
Criteria
Required
Medical
Information
Age Restrictions
Prescriber
Restrictions
Coverage
Duration
Other Criteria
Review Date: 6/2015
CRITERIA DETAILS
All medically accepted indications. Medically accepted indications are defined using the
following sources: the Food and Drug Administration (FDA), Micromedex, American
Hospital Formulary Service (AHFS), United States Pharmacopeia Drug Information for the
Healthcare Professional (USP DI) and the Drug Package Insert.
None
Documentation was submitted indicating that the member was evaluated for active or
latent TB infection (i.e. tuberculin skin test). See “other criteria”
The member is (≥6y/o) and has a documented clinical diagnosis of moderate to
severely active Crohn’s Disease
None
If the criterion is met, the request will be approved for up to a 6-month duration. If the
criterion is not met, the request is referred to a clinician for medical necessity review.
INITIAL AUTHORIZATION:
The patient has a documented (consistent with pharmacy claims data, OR for new members
to the health plan consistent with medical chart history) adequate trial of or has a
documented medical reason for not taking at least two nonsteroidal anti-inflammatory drugs
(NSAIDS) to manage their medical condition.
The patient has a documented (consistent with pharmacy claims data, OR for new
members to the health plan consistent with medical chart history) adequate trial of or has a
documented medical reason for not taking a cyclo-oxygenase (COX)-2-selective inhibitors
to manage their medical condition.
Documentation was submitted indicating that the member was evaluated for active or
latent TB infection (i.e. tuberculin skin test).
The medication requested has an FDA approved indication for use in patients with
ankylosing spondylitis and is being recommended and prescribed by a rheumatologist at an
FDA approved dosage.
If the request is for a non-preferred agent, documented (consistent with pharmacy claims
data, OR for new members to the health plan consistent with medical chart history)
adequate trial of the preferred biological agents.
RE – AUTHORIZATION:
The medication is being recommended and prescribed by a rheumatologist at an FDAapproved dosage.
The member has been receiving the medication and documentation was provided that the
prescriber has evaluated the member and recommends continuation of therapy.
Documentation submitted indicates that the member has obtained clinical benefit from
the medication.
If all of the above conditions are met, the request will be approved for a 6-month duration
for Remicade requests and for a 12 month duration for requests for all other medications. If
all of the above criteria are not met, the request is referred to a clinical reviewer for medical
necessity review.
NOTE: Clinical reviewer must override criteria when, in his/her professional
judgment, the requested item is medically necessary.
73
PRIOR AUTHORIZATION CRITERIA
SPECIALTY AGENTS FOR PSORIASIS
®
®
ENBREL (etanercept), HUMIRA (adalimumab) Preferred
REMICADE® (infliximab), ENTYVIO® (Vedolizumab), OTEZLA® (Apremilast), COSENTYX®
(Secukinumab), STELARA® (ustekinumab) Nonpreferred
PA CRITERIA
Covered Uses
Exclusion
Criteria
Required
Medical
Information
Age Restrictions
Prescriber
Restrictions
Coverage
Duration
Other Criteria
CRITERIA DETAILS
All medically accepted indications. Medically accepted indications are defined using the
following sources: the Food and Drug Administration (FDA), Micromedex, American
Hospital Formulary Service (AHFS), United States Pharmacopeia Drug Information for the
Healthcare Professional (USP DI) and the Drug Package Insert.
None
See “other criteria”
Member must be >/= 18 years of age
None
If the criterion is met, the initial request will be approved fo r a 6-month duration. For re –
authorization of Remicade requests, an approval of 6 months will be given and for re –
authorization of all other medications, a 12 month duration will be approved. If criterion
is not met, the request will be referred to a Clinician for medical necessity review.
INITIAL AUTHORIZATION:
• The member is an adult (≥18 y/o) and has a documented clinical diagnosis of
moderate to severe plaque psoriasis.
• Documentation that the patient has had (consistent with pharmacy claims data, OR
for new members to the health plan consistent with medical chart history) adequate
trials (including dates and dose s) of at least 3 of the treatment bullet points listed
below:
▪ The use of topical steroids or has a documented medical reason
for not using this therapy to manage their medical condition.
▪ The use of a topical medication [i.e. Dovonex® (calcipotriene),
Tazorac ® (tazorotene), anthralin or a coal tar preparation] that is
indicated for the treatment of psoriasis or has a documented
medical reason for not using any of these therapies to manage
their medical condition.
▪ The use of methotrexate or has a documented medical reason
(e.g. history of liver or kidney disease, pregnancy, severe
cytopenia, alcoholism) for not using this therapy to manage their
medical condition.
▪ The use of cyclosporine or has a documented medical reason for
met, the requestnot
is referred
to atherapy
clinicaltoreviewer
for medical
review.
using this
manage their
medicalnecessity
condition.
▪ The use of Soriatane® (acitretin) or has a documented medical
reason for not using this therapy to manage their medical
condition.
▪ The use of UVB phototherapy or PUVA (psoralen – oral or
topical methoxsalen plus UVA therapy) or has a documented
medical reason (e.g. pregnancy, skin cancer, hypersensitivity due
to preexisting disease state - e.g. systemic lupus erythematus,
cataracts) for not undergoing UVB phototherapy or PUVA to
manage their medical condition.
• Documentation was submitted indicating that the member was evaluated for active or
latent TB infection (i.e. tuberculin skin test).
74
Psoriasis
Other Criteria con’t
• The medication requested has an FDA approved indication for use in patients with
moderate to severe plaque psoriasis and is being recommended or prescribed by a
dermatologist at an FDA-approved dosage.
• If the request is for a non-preferred agent, documented (consistent with pharmacy
claims data, OR for new members to the health plan consistent with medical chart
history) If the request is for a non-preferred agent, documented (consistent with
pharmacy claims data, OR for new members to the health plan consistent with
medical chart history) adequate trial of the preferred biological agents.
RE-AUTHORIZATION:
• The medication is being recommended and prescribed by a dermatologist at an FDAapproved dosage.
• The member has been receiving the medication and documentation was
provided that the prescriber has evaluated the member and recommends
continuation of therapy.
• Documentation submitted indicates that the member has obtained clinical benefit from the
medication.
Review Date: 6/2015
NOTE: Clinical reviewer must override criteria when, in his/her professional
judgment, the requested item is medically necessary.
75
PRIOR AUTHORIZATION CRITERIA
PSORIATIC ARTHRITIS
ENBREL® (etanercept), HUMIRA® (adalimumab) Preferred
CIMZIA® (certolizumab) SIMPONI® (golimumab), REMICADE® (infliximab) OTEZLA® (Apremilast) ,
STELARA® (ustekinumab) Non – Preferred
PA Criteria
Covered Uses
Criteria Details
All medically accepted indications. Medically accepted indications are defined using the
following sources: the Food and Drug Administration (FDA), Micromedex, American
Hospital Formulary Service (AHFS), United States Pharmacopeia Drug Information for
the Healthcare Professional (USP DI) and the Drug Package Insert.
Exclusion
Criteria
None
Required
Medical
Information
Diagnosis of psoriatic arthritis
Age Restrictions
Patient must be 18 years old or older.
Coverage
Duration
If the criterion is met, the request will be approved for up to a 6 -month
duration. If the criterion is not met, the request will be referred to a clinician
for medical necessity review.
Other Criteria
INITIAL AUTHORIZATION:
• The patient has a documented (consistent with pharmacy claims data, OR for new
members to the health plan consistent with medical chart history) adequate trial of 2
g/day for 3 months of sulfasalazine or has a documented medical reason for not taking
sulfasalazine (e.g. predominantly axial symptoms, hepatotoxicity, GI (intolerance) to
manage their medical condition.
• The patient has a documented (consistent with pharmacy claims data, OR for new
members to the health plan consistent with medical chart history) adequate trial (3
months without any improvement at maximum doses) of methotrexate or has another
documented medical reason for not taking methotrexate (e.g. predominantly axial
symptoms, liver toxicity) to manage their medical condition.
• Documentation was submitted indicating that the member was evaluated for active or
latent TB infection (i.e. tuberculin skin test).
• The medication requested has a FDA approved indication for use in patients
with psoriatic arthritis and is being recommended and prescribed by a
rheumatologist or a dermatologist at an FDA-approved dosage.
• If the request is for a non-preferred agent, docum ented (consistent with
pharmacy claims data, OR for new members to the health plan consistent with
medical chart history) If the request is for a non-preferred agent, documented
(consistent with pharmacy claims data, OR for new members to the health plan
consistent with medical chart history) adequate trial of the preferred biological
agents.
RE – AUTHORIZATION:
• The medication is being recommended and prescribed by a rheumatologist or
dermatologist at an FDA- approved dosage.
• The member has been receiving the medication and documentation was
provided that the prescriber has evaluated the member and recommends
continuation of therapy.
• Documentation submitted indicates that the member has obtained clinical
benefit from the medication.
If all of the above conditions are met, the request will be approved fo r a 6-month
76
duration for Remicade requests and for a 12 month duration for all other medications. If
all of the above criteria are not met, the request will be referred to a clinical reviewer for
medical necessity review.
Review Date 6/2015
NOTE: Clinical reviewer must override criteria when, in his/her professional
judgment, the requested item is medically necessary.
77
PRIOR AUTHORIZATION CRITERIA
SYSTEMIC JUVENILE IDIOPATHIC ARTHRITIS
ENBREL® (etanercept), HUMIRA® (adalimumab) Preferred
ACTEMRA® (tocilizumab) , ORENCIA® (abatacept) Non - Preferred
PA Criteria
Criteria Details
Covered Uses
All medically accepted indications. Medically accepted indications are defined
using the following sources: the Food and Drug Administration (FDA),
Micromedex, American Hospital Formulary Service (AHFS), United States
Pharmacopeia Drug Information for the Healthcare Professional (USP DI) and the
Drug Package Insert.
Exclusion
Criteria
None
Required Medical
Information
See “other criteria”
Age Restrictions
Patient is a child </= 17 years old
Prescriber
Restrictions
Rheumatologist or Pediatric Rheumatologist
Coverage
Duration
Other Criteria
If the criterion is met, the request will be approved for a 6-month duration
and re – authorizations will be approved for a 12 month duration. If the
criterion is not met, the request will be referred to a Clinician for medical
necessity review.
INITIAL AUTHORIZATION:
•The patient is a child (< 17 y/o), within the FDA approved age range
for the medication requeste d, and has a documented clinical diagnosis
of systemic juvenile idiopathic arthritis.
• Documentation was submitted indicating that the member was evaluated for
active or latent TB infection (i.e. tuberculin skin test).
• The medication requested has an FDA approved indication for use in patients
with systemic juvenile idiopathic arthritis and is being recommended and
prescribed by a rheumatologist or a pediatric rheumatologist at an FDA - approved
dosage.
RE – AUTHORIZATION:
• The medication is being recommended and prescribed by a rheumatologist or
pediatric rheumatologist at an FDA-approved dosage.
• The member has been receiving the medication and documentation
was provided that the prescriber has evaluated the member and
recommends continuation of therapy.
• Documentation submitted indicates that the member has obtained
clinical benefit from the medication.
Review Date 6/2015
NOTE: Clinical reviewer must override criteria when, in his/her professional
judgment, the requested item is medically necessary.
78
PRIOR AUTHORIZATION CRITERIA
RHEUMATOID ARTHRITIS
ENBREL® (etanercept), HUMIRA® (adalimumab) Perferred
ACTEMRA® (tocilizumab) , ORENCIA® (abatacept), CIMZIA® (certolizumab), KINERET® (anakinra)
SIMPONI® (golimumab), REMICADE® (infliximab,) XELJANZ® (tofacitinib) Non – Preferred
PA Criteria
Covered Uses
Criteria Details
All medically accepted indications. Medically accepted indications are defined using the
following sources: the Food and Drug Administration (FDA), Micromedex, American
Hospital Formulary Service (AHFS), United States Pharmacopeia Drug Information for the
Healthcare Professional (USP DI) and the Drug Package Insert.
Exclusion
Criteria
None
Age Restrictions
Patient is >/= 18 years old
Prescriber
Restrictions
Rheumatologist or Pediatric Rheumatologist
Coverage
Duration
Other Criteria
If the criterion is met for initial authorization, the request will be approved for up to a 6 month duration. For re – authorizations, if the criterion is met, the request will be approved
for a 6 -month duration for Remicade requests and for a 12 month duration for all other
medications. If criterion is not met, the request is referred to a Clinician for medical
necessity review.
INITIAL AUTHORIZATION:
•The patient has a documented clinical diagnosis of rheumatoid arthritis.
• The patient has a documented (consistent with pharmacy claims data, OR for new
members to the health plan consistent with medical chart history) adequate trial
(including dates and doses) of 3 months or more of therapy with methotrexate AND
then leflunomid e (generic Arava®) or another disease -modifying antirheumatic drug
(DMARD) option (i.e. combination therapy consisting of methotrexate + sulfasalazine
or hydroxychloroquine) or has a documented medical reason (e.g. intolerance,
hypersensitivity) for not utilizing any of these therapies to manage their medical
condition.
•Documentation was submitted indicating that the member was evaluated for active or
latent TBuberculin skin test).
•The medication requested has an FDA approved indicatio n for use in patients with
rheumatoid arthritis and is being recommended and prescribed by a rheumatologist
at an FDA -approved dosage.
•If the request is for a non-preferred agent, documented (consistent with pharmacy
claims data, OR for new members to the health plan consistent with medical chart
history) adequate trial of the preferred biological agents.
RE – AUTHORIZATION:
• The member has been receiving the medication and documentation was provided
that a rheumatologist has evaluated the member and recommends continuation of
therapy.
• Documentation submitted indicates that the member has obtained clinical benefit from the
medication.
• For members who require Humira 40 mg SC weekly documentation must be
submitted indicating that the member was compliant (consistent with pharmacy
claims) with receiving at least 16 weeks of continuous Humira therapy every other
week prior to the request for weekly dosing of Humira AND the member has a
medical reason (e.g. intolerance, hypersensitivity, contraindication) for not receiving
concomitant methotrexate.
• The medication is being prescribed for an FDA-approved indication at an FDA-approved
dosage.
79
Review Date
6/2015
NOTE: Clinical reviewer must override criteria when, in his/her professional judgment,
the requested item is medically necessary.
80
PRIOR AUTHORIZATION PRIOR AUTHORIZATION CRITERIA
ULCERATIVE COLITIS
HUMIRA® (adalimumab) Preferred
SIMPONI® (golimumab), REMICADE®(infliximab), ENTYVIO®(Vedolizumab) Non – Preferred
PA Criteria
Covered Uses
Criteria Details
All medically accepted indications. Medically accepted indications are defined using the
following sources: the Food and Drug Administration (FDA), Micromedex, American
Hospital Formulary Service (AHFS), United States Pharmacopeia Drug Information for the
Healthcare Professional (USP DI) and the Drug Package Insert.
Exclusion
Criteria
None
Required
Medical
Information
See “other criteria”
Age Restrictions
The patient is (≥6 y/o) and has moderate to severe active ulcerative colitis.
Prescriber
Restrictions
Rheumatologist or Pediatric Rheumatologist
Other Criteria
INITIAL AUTHORIZATION:
• The patient has a documented (consistent with pharmacy claims data, OR for new
members to the health plan consistent with medical chart history) treatment failure
after receiving an ad equate trial of:
▪ Sulfasalazine (3 to 6 g/day for 3 months), or mesalamine (1.2 to 2.4 g/day
for 3 months), or azathioprine (2 to 2.5 mg/kg/day), or 6-mercaptopurine (1.5
to 2 mg/kg/day), or oral corticosteroids or has a documented medical reason
(GI intolerance, hypersensitivity, etc.) for not taking any of these medications
to treat their medical condition.
• Documentation was submitted indicating that the member was evaluated for active or
latent TB infection (i.e. tuberculin skin test).
• The medication requested has a FDA approved indication for use in patients with
moderate to severe active ulcerative colitis and is being prescribed at an FDAapproved dosage and is recommended or prescribed by a gastroenterologist.
• If the request is for a non-preferred agent, documente(consistent with pharmacy
claims data, OR for new members to the health plan consistent with medical
chart history) adequate trial of the preferred biological agents.
RE – AUTHORIZATION:
• The medication is being recommended and prescribed by gastroent erologist for an
FDA-approved indication at an FDA-approved dosage.
• The member has been receiving the medication and documentation was
provided that the prescriber has evaluated the member and recommends
continuation of therapy.
• Documentation submitted indicates that the member has obtained clinical benefit from the
medication.
Review Date 6/2015
NOTE: Clinical reviewer must override criteria when, in his/her professional
judgment, the requested item is medically necessary
81
PRIOR AUTHORIZATION PRIOR AUTHORIZATION CRITERIA
Specialty Biologic Agents for Non – FDA Approved Medically Accepted Indications
HUMIRA® (adalimumab) Preferred, ENBREL® (etanercept) Preferred
REMICADE®(infliximab), ENTYVIO®(Vedolizumab), ACTEMRA® (tocilizumab), CIMZIA®
(certolizumab), KINERET® (anakinra), ORENCIA® (abatacept), SIMPONI® (golimumab), STELARA®
(ustekinumab) OTEZLA® (Apremilast), COSENTYX® (Secukinumab), XELJANZ® (tofacitinib)
Non - Preferred
PA Criteria
Criteria Details
Covered Uses
The medication is prescribed for a non-FDA approved indication that is
considered a medically accepted use of the medication per the medical compendia
(i.e. Micromedex, DrugPoints, AHFS drug information).
Exclusion
Criteria
None
Required
Medical
Information
See “other criteria”
Prescriber
Restrictions
Coverage
Duration
Other Criteria
Prescribed by a specialist in the field to treat the member’s respective medical condition.
If all criteria is met for initial authorization, the request will be approved for up to a 6
month duration. If all criteria is met for re - authorization, the request will be
approved for an additional 6 months. If criteria is not met, the request will be
referred to a clinician for medical necessity review.
INITIAL AUTHORIZATION:
• The medication is prescribed at a medically accepted dose per the medical compendia.
• Documentation was submitted indicating that the member has a documented
(consistent with pharmacy claims data, OR for new members to the health plan
consistent with medical chart history) adequate trial (including dates, doses of
medications) of all first line medical therapies as recommended by the medical
compendia and standard of care guidelines or has another documented medical
reason (e.g. intolerance, contraindications) for not receiving or trying all first line
medical treatment(s).
• Documentation was submitted indicating that the member was evaluated for active or
latent TB infection (i.e. tuberculin skin test).
• If the request is for a non-preferred agent, documented (consistent with
pharmacy claims data, OR for new members to the health plan consistent with
medical chart history) adequate trial of at least two preferred biological agents
(if possible).
RE - AUTHORIZATION:
• The medication is prescribed at a medically accepted dose per the medical compendia.
• The medication is recommended and prescribed by a specialist in the field to treat the
member’s respective medical condition.
Review Date: 6/2015
• Documentation submitted indicates that the member has obtained clinical benefit from
the medication.
NOTE: Clinical reviewer must override criteria when, in his/her
professional judgment, the requested item is medically necessary.
82
PRIOR AUTHORIZATION CRITERIA for Juxtapid®/Kynamro®
PREFERRED STATUS: Non-Preferred- REQUIRE Prior Authorization
Juxtapid® (lomitapide)
Kynamro® (Mipomersen Sodium)
INITIAL CRITERIA FOR JUXTAPID®/KYNAMRO®:
Patient is 18 year of age or older.
Prescriber must be cardiologist or a specialist in the treatment of lipid disorders.
Documentation submitted includes patient’s complete medical history /co-morbidities.
Patient must have a confirmed diagnosis of familial hypercholesterolemia (FH) with chart notes
or clinical labs including 3 of the following:
Autosomal Dominant Hypercholesterolemia Genetic Testing Reflex Panel (ADHP Panel)
2 fasting lipid panel laboratory reports within the past 12 months with abnormal LDL
cholesterol levels >220
documented strong (first and second degree relatives) family history of high levels of
LDL and/or heart attack and relationship to member
documented chart notes of clinical manifestations of FH such as xanthomas or inflamed
tendons
Documented claim history or chart notes showing consistent therapy (3 months) with
atorvastatin 80mg OR Crestor (Rosuvastatin) 40mg* (*OR documentation has been provided
that patient is of Asian descent in which Crestor 20mg is the max dose) with inadequate
response OR a documented medical reason (e.g. intolerance, hypersensitivity) for not utilizing
one of these therapies to manage their medical condition.
If request indicates that the patient is “statin intolerant”, documentation was provided including
description of the side effects, duration of therapy, “wash out”, re-trial, and then change of
agents.
Documentation submitted includes an attestation that the patient is following a “heart healthy”
diet.
Documentation submitted indicates the patient is a non-smoker or is actively quitting smoking.
If the request is for Juxtapid®, the patient has had an inadequate response or a documented
medical reason (e.g. intolerance, hypersensitivity) for not utilizing Repatha® AND THEN
Kynamro® to manage their medical condition.
If all of the above conditions are met, the request will be approved for a 4 month duration; if all of
the above criteria are not met, the request is referred to a clinical reviewer for medical necessity
review.
REAUTHORIZATION CRITERIA:
Prescriber must be cardiologist or a specialist in the treatment of lipid disorders.
Documentation submitted indicates that the member has obtained clinical benefit from the
medication including repeat fasting lipid panel lab report, and the member has had at least a
50% reduction in LDL.
The patient’s claim history shows consistent therapy (i.e. monthly fills)
If all of the above conditions are met, the request will be approved for a 6 month duration; if all of
the above criteria are not met, the request is referred to a Medical Director/clinical reviewer for
medical necessity review.
NOTE: Medical Director/clinical reviewer must override criteria when, in his/her professional
judgment, the requested items medically necessary.
Revision/Review Date: 4/2016
84
Field Name
Prior Authorization
Group Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber Restrictions
Coverage Duration
Other Criteria
Field Description
Kapvay®
Kapvay® (clonidine) extended-release tablets
Medically accepted indications are defined using the following
sources: the Food and Drug Administration (FDA), Micromedex,
American Hospital Formulary Service (AHFS), United States
Pharmacopeia Drug Information for the Healthcare Professional (USP
DI), the Drug Package Insert (PPI), or disease state specific standard
of care guidelines.
N/A
See “other criteria”
Member must be > 6 years old
N/A
If the criteria are met, the request will be approved with up to a 12
month duration; if the criteria are not met, the request will be referred
to a clinical reviewer for medical necessity review.
Initial Authorization
Documented diagnosis of attention deficit hyperactivity
disorder (ADHD)
At least two month trial of an immediate release clonidine
formulation
Revision/Review Date
04/2016
Medical Director/clinical reviewer must override criteria when, in
his/her professional judgement, the requested item is medically
necessary.
PRIOR AUTHORIZATION CRITERIA
LIDODERM (lidocaine)
PA Criteria
Criteria Details
Covered Uses
Medically accepted indications are defined using the following sources: the Food
and Drug Administration (FDA), Micromedex, American Hospital Formulary
Service (AHFS), United States Pharmacopeia Drug Information for the
Healthcare and the Drug Package Insert.
Exclusion
Criteria
None
Required Medical
Information
See “other criteria”
Age Restrictions
Prescriber
Restrictions
Coverage
Duration
Other Criteria
None
None
If the criterion is met, the request will be approved with a 6 month duration. If the
criterion is not met, the request will be referred to a Clinician for medical
necessity review.
AUTHORIZATION:
Diagnosis of postherpetic neuralgia
AND
Documented trial and failure or intolerance to the following medications:
amitriptyline or nortriptyline and gabapentin
Review Date: 6/2015
NOTE: Clinical reviewer must override criteria when, in his/her professional
judgment, the requested item is medically necessary.
86
Field Name
Prior Authorization
Group Description
Drugs
Field Description
Long Acting Attention Deficit/Hyperactivity Disorder (ADHD)
Medications
Listed
Adderall XR (Dextroamphetamine)
Concerta (methylphenidate ER)
Dexedrine Spansules (dextroamphetamine)
Focalin XR (dexmethylphenidate)
Metadate ER (methylphenidate ER)
Vyvanse (lisdexamfetamine)
Non-Listed
Daytrana (methylphenidate) Patch
Metadate CD (methylphenidate)
Ritalin LA (methylphenidate)
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber Restrictions
Coverage Duration
Medically accepted indications are defined using the following
sources: the Food and Drug Administration (FDA), Micromedex,
American Hospital Formulary Service (AHFS), United States
Pharmacopeia Drug Information for the Healthcare Professional (USP
DI), the Drug Package Insert (PPI), or disease state specific standard
of care guidelines.
None
See “other criteria”
Specific Age Limits:
• Adderall XR (Dextroamphetamine ER) ≥6
• Concerta (methylphenidate ER) ≥6
• Dexedrine Spansule (dextroamphetamine) ≥3 with specific
criteria for those ≥21
• Focalin XR (dexmethylphenidate) ≥6
• Metadate ER (methylphenidate ER) ≥6
• Vyvanse (lisdexamfetamine) ≥6
• Daytrana (methylphenidate) ≥6
• Metadate CD (methylphenidate) ≥6
Ritalin LA (methylphenidate) ≥6
None
If the criteria are met, the request will be approved with up to a 12
month duration; if the criteria are not met, the request will be referred
to a clinical reviewer for medical necessity review.
Other Criteria
Initial Authorization:
Preferred long-acting ADHD medications prescribed in a dose that
exceeds FDA approved limits and/or Select Health daily quantity
limits will require prior authorization.
Requests will be considered base on the individual circumstances.
Things that need to be considered include but are not limited to:
Previous therapy
Previous dose
Side effects of increased/higher once daily doses
Time of day initial dose wears off
Revision/Review Date
04/2016
Medical Director/clinical reviewer must override criteria when, in
his/her professional judgement, the requested item is medically
necessary.
PRIOR AUTHORIZATION CRITERIA
LONG ACTING INJECTABLE ANTIPSYCHOTICS
Risperdal Consta® (risperidone), Invega® Sustenna™ (paliperidone palmitate),
InvegaTrinza™ (paliperidone palmitate), Zyprexa Relprevv® (olanzapine), Abilify Maintena® (aripiprazole)
PA Criteria
Criteria Details
Covered Uses
Medically accepted indications are defined using the following sources: the Food
and Drug Administration (FDA), Micromedex, American Hospital Formulary
Service (AHFS), United States Pharmacopeia Drug Information for the Healthcare
and the Drug Package Insert.
Exclusion
Criteria
Required Medical
Information
Age Restrictions
Coverage
Duration
Other Criteria
None
See “other criteria”
Patients must be >/= 7 years of age
If all initial criteria are met, the request will be approved with a 16-week duration.
If the criterion for re – authorization is met, the request will be approved with a
16-week duration, however for patients stable on a dose (e.g. > 6 months) can be
approved for a 12 month duration. If the criterion is not met, the request will be
referred to a Clinician for medical necessity review.
INITIAL AUTHORIZATION:
The member has a long-term history (>3 months) of two oral anti-psychotic
medications noncompliance AND documentation submitted indicates that the
member had significant clinical decompensation or there is a high risk for
decompensation and functional impairment (e.g. hospitalizations, safety risk)
AND documentation of a drug adherence treatment plan was also submitted that
indicates the member failed the following types of measures to improve
compliance with formulary oral medications and/or a reason for why
any of the following measures were not implemented to improve compliance with
formulary oral medications as clinically applicable:
Psychosocial interventions
Psychoeducational interventions that have a behavioral component and
supportive services.
Provided member with concrete instructions and problem-solving
strategies (i.e. reminders, self – monitoring tools, cues, and
reinforcements).
AND/OR the member has a documented medical reason (i.e. documented
treatment failure to maximum doses and/or has Intolerable side effects or drug
interactions) for not using formulary atypical antipsychotic medication.
Documentation submitted indicates that the medication is being prescribed for an
FDA approved indication.
The patients has documentation submitted (consistent with pharmacy claims
data) of a history of receiving any two oral antipsychotic medication mentioned
above.
If the request is for Invega® Trinza™, the patient has been adequately treated
with Invega® Sustenna® for at least 4 months.
PA CRITERIA FOR REAUTHORIZATION:
Documentation submitted indicates that the medication continues to be
prescribed for its FDA approved indication.
Documentation submitted indicating how the member clinically improved or
stabilized while receiving the medication.
Documentation submitted indicates that the member is tolerating medication.
88
Review Date: 6/2015
NOTE: Clinical reviewer must override criteria when, in his/her professional
judgment, the requested item is medically necessary
89
Field Name
Prior Authorization
Group Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber Restrictions
Coverage Duration
Other Criteria
Field Description
CNS STIMULANTS/AMPHETAMINES
Dexedrine (Dextroamphetamine ER) 5/10/15mg Capsule
Zenzedi (Dextroamphetamine) 5/10mg Tablet
Medically accepted indications are defined using the following
sources: the Food and Drug Administration (FDA), Micromedex,
American Hospital Formulary Service (AHFS), United States
Pharmacopeia Drug Information for the Healthcare Professional (USP
DI), the Drug Package Insert (PPI), or disease state specific standard
of care guidelines.
N/A
See “other criteria”
Member is an adult greater than or equal to 21 years of age.
N/A
If the criteria are met, the request will be approved with up to a 12
month duration; if the criteria are not met, the request will be referred
to a clinical reviewer for medical necessity review.
Initial Authorization:
Revision/Review Date
04/2016
Requests for Dexedrine ER or Zenzedi will be approved if a
documented trial and failure with all formulations of
Methylphenidate in the members claim history is found.
Medical Director/clinical reviewer must override criteria when, in
his/her professional judgement, the requested item is medically
necessary.
Field Name
Prior Authorization
Group Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber Restrictions
Coverage Duration
Other Criteria
Field Description
Lyrica®
Lyrica® (pregabalin) capsule
Medically accepted indications are defined using the following
sources: the Food and Drug Administration (FDA), Micromedex,
American Hospital Formulary Service (AHFS), United States
Pharmacopeia Drug Information for the Healthcare Professional (USP
DI), the Drug Package Insert (PPI), or disease state specific standard
of care guidelines.
N/A
See “other criteria”
N/A
N/A
If the criteria are met, the request will be approved with up to a 12
month duration; if the criteria are not met, the request will be referred
to a clinical reviewer for medical necessity review.
Initial Authorization:
Partial-Onset Seizures
• Documented diagnosis of partial-onset seizures.
• Patient currently receiving another anticonvulsant medication at a
therapeutic dosage.
• Documented trial and failure or intolerance to gabapentin.
Postherpetic Neuralgia
• Documented diagnosis of postherpetic neuralgia.
• Documented trial and failure or intolerance to gabapentin. Trial
consists of a minimum of 30 days at a dose of at least 1800
mg/day.
Neuropathic Pain Associated with Diabetic Peripheral Neuropathy
• Documented diagnosis of peripheral neuropathy.
Fibromyalgia:
• Documented diagnosis of fibromyalgia.
Trigeminal Neuralgia Pain:
• Documented diagnosis of trigeminal neuralgia.
• Documented trial and failure or intolerance to at least three of the
following: baclofen, carbamazepine, gabapentin, lamotrigine,
oxcarbazepine, phenytoin
Revision/Review Date
04/2016
Medical Director/clinical reviewer must override criteria when, in
his/her professional judgement, the requested item is medically
necessary.
Field Name
Prior Authorization
Group Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber
Restrictions
Coverage Duration
Other Criteria
Field Description
Hydroxyprogesterone Caproate Prior Authorization Criteria
Makena® (hydroxyprogesterone caproate)
Medically accepted indications are defined using the following sources:
the Food and Drug Administration (FDA), Micromedex, American
Hospital Formulary Service (AHFS), United States Pharmacopeia Drug
Information for the Healthcare Professional (USP DI), the Drug Package
Insert (PPI), or disease state specific standard of care guidelines.
Patients pregnant with multiples, history of thrombosis or
thromboembolic disorders, history of breast cancer or other hormone
sensitive cancer, cholestatic jaundice of pregnancy, liver tumors or active
liver disease, or uncontrolled hypertension
See “other criteria”
Patient must be 16 years of age or older
Prescriber must be an obstetrician/gynecologist.
If all of the criteria is met, the request will be approved for up to 21
weeks (5ml for 35 days with 3 refills). If the conditions are not met, the
request will be sent to a Medical Director/clinical reviewer for medical
necessity review.
Initial authorization:
Revision/Review
Date 02/2016
Documentation has been provided that patient has a history of
preterm birth before 37 weeks gestation
Documentation that patient is pregnant with singleton
Documentation that drug is being used for FDA approved
indication (begin treatment between 16 weeks gestation and
continued weekly until week 37 gestation) at an FDA approved
dose.
Medical Director/clinical reviewer must override criteria when, in
his/her professional judgement, the requested item is medically
necessary.
92
Field Name
Prior Authorization
Group Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber Restrictions
Coverage Duration
Other Criteria
Field Description
Mepron®
Mepron® (atovaquone) suspension
Medically accepted indications are defined using the following
sources: the Food and Drug Administration (FDA), Micromedex,
American Hospital Formulary Service (AHFS), United States
Pharmacopeia Drug Information for the Healthcare Professional (USP
DI), the Drug Package Insert (PPI), or disease state specific standard
of care guidelines.
N/A
See “other criteria”
N/A
N/A
If the criteria are met, the request will be approved with up to a 6
month duration; if the criteria are not met, the request will be referred
to a clinical reviewer for medical necessity review.
Initial Authorization:
Diagnosis of Pneumocystis jirovecii pneumonia (PCP) or
diagnosis with the need to prevent PCP infection.
AND
Documented trial and failure with therapeutic doses or
intolerance to trimethoprim- sulfamethoxazole (TMP-SMX) (first
line therapy).
Revision/Review Date
04/2016
Medical Director/clinical reviewer must override criteria when, in
his/her professional judgement, the requested item is medically
necessary.
PRIOR AUTHORIZATION CRITERIA
METANX® ( l-methylfolate with vitamins b6 and b12 capsule)
PA Criteria
Criteria Details
Covered Uses
Medically accepted indications are defined using the following sources: the
Food and Drug Administration (FDA), Micromedex, American Hospital
Formulary Service (AHFS), United States Pharmacopeia Drug Information
for the Healthcare Professional (USP DI, and the Drug Package Insert.
Exclusion
Criteria
None
Required Medical
Information
See “other criteria.”
Age Restrictions
Prescriber
Restrictions
Coverage
Duration
Other Criteria
None
None
If the criterion is met, the request will be approved for a 12 month duration. If
the criterion is not met, the request will be referred to a Clinician for medical
necessity review.
AUTHORIZATION:
• Documentation of dietary management of endothelial dysfunction in
patients with diabetic peripheral neuropathy.
AND
• Trial and failure of or intolerance to therapeutic doses of amitriptyline or
gabapentin.
Review Date: 2/2015
NOTE: Clinical reviewer must override criteria when, in his/her professional
judgment, the requested item is medically necessary.
94
Field Name
Prior Authorization
Group Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber Restrictions
Coverage Duration
Other Criteria
Field Description
Multaq®
Multaq® (dronedarone)
Medically accepted indications are defined using the following
sources: the Food and Drug Administration (FDA), Micromedex,
American Hospital Formulary Service (AHFS), United States
Pharmacopeia Drug Information for the Healthcare Professional (USP
DI), the Drug Package Insert (PPI), or disease state specific standard
of care guidelines.
N/A
See “other criteria”
N/A
Request must be from a cardiologist or electrophysiologist.
If the criteria are met, the request will be approved with up to a 12
month duration; if the criteria are not met, the request will be referred
to a clinical reviewer for medical necessity review.
Initial Authorization:
Revision/Review Date
04/2016
Diagnosis of paroxysmal or persistent arterial fibrillation
(AF) or atrial flutter (AFL) with a recent episode.
Must not have NYHA Class IV heart failure or
symptomatic heart failure with recent decompensation
requiring hospitalization or referral to a specialized heart
failure clinic
Must have at least one of the following associated risk
factor(s):
▪ age > 70
▪ hypertension
▪ diabetes
prior cerebrovascular accident
▪ left atrial diameter ≥50 mm or left ventricular ejection
fraction (LVEF) < 40%
Medical Director/clinical reviewer must override criteria when, in
his/her professional judgement, the requested item is medically
necessary.
Field Name
Prior Authorization
Group Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber
Restrictions
Coverage Duration
Other Criteria
Revision/Review
Date 02/2016
Field Description
SELF INJECTABLE DISEASE MODIFYING
IMMUNOMODULATORS FOR MULTIPLE SCLEROSIS (MS)
Interferon beta-1a (Avonex®, Rebif®), Interferon beta-1b
(Betaseron®, Extavia™), Glatiramer Acetate (Copaxone®,
Glatopa™), Peginterferon beta-1a (Plegridy®)
Medically accepted indications are defined using the following sources:
the Food and Drug Administration (FDA), Micromedex, American
Hospital Formulary Service (AHFS), United States Pharmacopeia Drug
Information for the Healthcare Professional (USP DI), the Drug Package
Insert (PPI), or disease state specific standard of care guidelines.
Patients with primary progressive MS
See “Other Criteria”
Patient must be 18 years of age or older
Prescriber must be a neurologist
If all of the criteria are met, the initial request will be approved for 6
months. For continuation of therapy, if all criteria are met, the request
will be approved for 12 months. If all of the above criteria are not met,
the request is referred to a Medical Director/Clinical Reviewer for
medical necessity review
INITIAL AUTHORIZATION:
The patient is ≥ 18 years old with a clinical diagnosis of a relapsing
form of multiple sclerosis
If the medication request is for Avonex®, Rebif®, Betaseron®,
Extavia® or any other Newly Marketed Self-Injectable DiseaseModifying Immunomodulating MS Agent, the member has a
documented treatment failure to Copaxone® and Plegridy® which is
consistent with pharmacy claims data, OR for new members to the
health plan consistent with medical chart history, indicating they had
received an adequate trial (including dates, doses of 6 months or
more of each therapy) of Copaxone® 40 mg and Plegridy® and/or
has another documented clinically significant medical reason
(intolerance, hypersensitivity, contraindication, etc.) for not taking
Copaxone® 40 mg and Plegridy® for a minimum of 6 months each to
treat their medical condition
The medication is being prescribed by a neurologist at an FDA
approved dose
PA CRITERIA FOR REAUTHORIZATION:
The patient is ≥ 18 years old with a clinical diagnosis of a relapsing
form of multiple sclerosis
Documentation indicating the member has clinically benefited from
therapy
The medication is being prescribed by a neurologist at an FDA
approved dose
Medical Director/clinical reviewer must override criteria when, in
96
his/her professional judgement, the requested item is medically
necessary.
97
Field Name
Prior Authorization Group
Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber Restrictions
Coverage Duration
Other Criteria
Revision/Review Date
11/2015
Field Description
Natpara®
Natpara® (parathyroid hormone)
Medically accepted indications are defined using the following sources: the Food
and Drug Administration (FDA), Micromedex, American Hospital Formulary Service
(AHFS), United States Pharmacopeia Drug Information for the Healthcare
Professional (USP DI), the Drug Package Insert (PPI), or disease state specific
standard of care guidelines.
Patients at risk for osteosarcoma, patients with hypoparathyroidism caused by
calcium-sensing receptor mutations or in patients with acute postsurgical
hypoparathyroidism.
See “other criteria”
Patient is 18 years of age or older
MD is an endocrinologist
If all of the conditions are met, the request will be approved for a 3 month
duration. If the conditions are not met, the request will be sent to a Medical
Director/clinical reviewer for medical necessity review.
Documentation has been submitted that the patient has a diagnosis of
chronic hypoparathyroidism who cannot maintain stable serum and
urinary calcium levels with calcium and vitamin D
Documentation has been submitted (with dates of therapy) that the
patient has had an adequate trial with calcium and vitamin D
Documentation has been submitted that the patient will take Natpara® in
combination with calcium and vitamin D
Patient is NOT currently taking alendronate
Current labs (within 30 days of request) have been submitted for the
following:
Serum calcium (must be above 7.5mg/dL to start therapy)
Vitamin D level (must be adequate to start therapy)
If these conditions are not met, the request will be sent to a Medical
Director/clinical reviewer for medical necessity review.
Medical Director/clinical reviewer must override criteria when, in his/her
professional judgement, the requested item is medically necessary.
98
Field Name
Prior Authorization
Group Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber Restrictions
Coverage Duration
Other Criteria
Field Description
Niaspan®
Niaspan® (niacin)
Medically accepted indications are defined using the following
sources: the Food and Drug Administration (FDA), Micromedex,
American Hospital Formulary Service (AHFS), United States
Pharmacopeia Drug Information for the Healthcare Professional (USP
DI), the Drug Package Insert (PPI), or disease state specific standard
of care guidelines.
N/A
See “other criteria”
N/A
N/A
If the criteria are met, the request will be approved with up to a 12
month duration; if the criteria are not met, the request will be referred
to a clinical reviewer for medical necessity review.
Initial Authorization:
• Diagnosis of hypercholesterolemia or use in prevention of MI or
atherosclerotic disease with a history of high cholesterol.
• Documentation must be submitted that the patient is unable to
tolerate HMG CoA Reductase Inhibitors (Statins).
Revision/Review Date
04/2016
Medical Director/clinical reviewer must override criteria when, in
his/her professional judgement, the requested item is medically
necessary.
Field Name
Prior Authorization
Group Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber Restrictions
Coverage Duration
Other Criteria
Field Description
Non-Preferred/Prior Authorization Required Medications
Criteria
Medically accepted indications are defined using the following
sources: the Food and Drug Administration (FDA), Micromedex,
American Hospital Formulary Service (AHFS), United States
Pharmacopeia Drug Information for the Healthcare Professional (USP
DI), the Drug Package Insert (PPI), or disease state specific standard
of care guidelines.
N/A
See “other criteria”
N/A
N/A
If the criterion is met, the request will approved for up to a 12 month
duration (depending on the diagnosis and usual treatment duration). If
criterion is not met, the request will be referred to a Clinician for
medical necessity review.
Initial Authorization:
Appropriate diagnosis/indication for requested nonpreferred/prior authorization required medication.
Appropriate dose of medication based on age (i.e. pediatric and
elderly populations) and indication.
And patient meets one of the three following criteria:
Revision/Review Date
07/2016
Documented trial and failure or intolerance with up to three
preferred medications used to treat the documented diagnosis.
For medications where there is only one preferred agent, only
that agent must have been ineffective or not tolerated.
No other preferred medication has a medically accepted use for
the patient’s specific diagnosis as referenced in the medical
compendia.
All other preferred medications are contraindicated based on
the patient’s diagnosis, other medical conditions, or other
medication therapy.
Medical Director/clinical reviewer must override criteria when, in
his/her professional judgement, the requested item is medically
necessary.
Field Name
Prior Authorization
Group Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber Restrictions
Coverage Duration
Other Criteria
Revision/Review Date
7/2016
Field Description
Injectable/Specialty Medications Without Specific Prior
Authorization Protocol
Any injectable or specialty medication that does not have criteria
specific to the drug***PLEASE NOTE FOR ONCOLOGY
MEDICATIONS there is either specific criteria or follow the
ONCOLOGY WITHOUT SPECIFIC CRITERIA POLICY***
Medically accepted indications are defined using the following
sources: the Food and Drug Administration (FDA), Micromedex,
American Hospital Formulary Service (AHFS), United States
Pharmacopeia Drug Information for the Healthcare Professional (USP
DI), the Drug Package Insert (PPI), or disease state specific standard
of care guidelines.
N/A
“see other criteria”
N/A
N/A
If all of the conditions are met, requests will be approved for a 6
months. If the conditions are not met, the request will be sent to a
Medical Director/clinical reviewer for medical necessity review.
Documentation has been provided that patient has tried and
failed the formulary or other first line agents as indicated in
covered uses OR a medical reason has been provided as to why
these agents are unable to be used to treat the patient’s
condition (e.g. intolerance, contraindication, etc.)
Dosing is appropriate
Physician/clinical reviewer must override criteria when, in his/her
professional judgment, the requested item is medically necessary.
Field Name
Prior Authorization
Group Description
Drugs
Field Description
OPHTHALMIC ANTIHISTAMINES
FORMULARY STATUS Formulary, Pays at Point-of-Sale
Alaway OTC (ketotifen)
Ketotifen OTC (ketotifen)
Zaditor OTC (ketotifen)
Zyrtec Itchy Eye OTC (ketotifen)
FORMULARY STATUS Formulary, Requires Step Therapy
(Second Line)
Pataday (olopatadine)
Note: Patient must meet #1 & #2 criteria for approval of initial PA
request
FORMULARY STATUS Non-Formulary, Requires Prior
Authorization (Second Line)
Bepreve (bepotastine besilate)
Elestat (epinastine)
Emadine (emedastine)
Optivar (azelastine)
Patanol (olopatadine)
Lastacaft (alcaftadine)
or any newly marketed ophthalmic antihistamine
Note: Patient must meet criteria #1, #2 & #3 for approval of initial
PA request.
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber Restrictions
Coverage Duration
Medically accepted indications are defined using the following
sources: the Food and Drug Administration (FDA), Micromedex,
American Hospital Formulary Service (AHFS), United States
Pharmacopeia Drug Information for the Healthcare Professional (USP
DI), the Drug Package Insert (PPI), or disease state specific standard
of care guidelines.
N/A
See “other criteria”
N/A
N/A
If the above conditions are met, the request will be approved with a 12
month duration. If the criterion is not met, the request will be referred
to a Clinician for medical necessity review.
Other Criteria
Initial Authorization:
Revision/Review Date
07/2016
Documented trial and failure or intolerance to Zaditor OTC,
Alaway OTC, Zyrtec Itchy Eye OTC or Ketotifen OTC (first
line agents) for at least 2 weeks (14 days) of therapy.
Documented trial and failure or intolerance to Pataday (second
line agent) for at least 2 weeks (14 days) of therapy.
Medical Director/clinical reviewer must override criteria when, in
his/her professional judgement, the requested item is medically
necessary.
PRIOR AUTHORIZATION CRITERIA
Opiate Dependence Agents
ZUBSOLV® (buprenorphine HCL/naloxone)
Buprenorphine Tablet
SUBOXONE® (buprenorphine HCL/naloxone)
BUNAVAIL® (buprenorphine HCL/naloxone)
FORMULARY STATUS: Formulary
FORMULARY STATUS: Formulary
FORMULARY STATUS: Formulary
FORMULARY STATUS: Non-Formulary
PA Criteria
Criteria Details
Covered Uses
Medically accepted indications are defined using the following sources: the Food and
Drug Administration (FDA), Micromedex, American Hospital Formulary Service
(AHFS), United States Pharmacopeia Drug Information for the Healthcare Professional
(USP DI), and the Drug Package Insert.
Exclusion
Criteria
None
Required
Medical
Information
See “other criteria”
Patient must be >/= 16 years of age
Age Restrictions
Physician meets all qualifications to prescribe buprenorphine/naloxone (Federal, State, and
Local)
Prescriber
Restrictions
If these criteria are met, then an initial maximum of 3 months of buprenorphine/naloxone (1
month dispensed at a time) or up to a total of 4 weeks of buprenorphine will be authorized,
depending upon the request of the physician. If the criteria are not met, clinical review will
be necessary to determine whether other factors, such as age, co-morbidities, social situation,
or prior treatment considerations, would support medical necessity for the initiation or reinitiation of buprenorphine/naloxone.
Coverage
Duration
AUTHORIZATION:
Other Criteria
Patient is diagnosed with opioid dependence and/or opioid addiction;
The risks of using buprenorphine/naloxone with alcohol or benzodiazepines have been
explained to the patient;
o
No untreated or unstable psychiatric conditions that would interfere with
buprenorphine/naloxone compliance;
No more than one (1) prior attempt to treat opiate addiction with buprenorphine/naloxone
within the prior 12 months (or if an individual has had more than 1 trial in that time frame, an
assessment is completed by a licensed provider indicating the need for buprenorphine);
o
Documentation of referral to or active involvement in formal counseling by a licensed
behavioral health provider (D&A counselor is preferred, but not required). 12-step program
participation, by itself, is not acceptable;
o
Dosing maximum of 16mg/day (for Suboxone or buprenorphine) or 11.4mg/2.8mg/day (for
Zubsolv) is requested. On a case-by-case basis clinical consideration can be given to a
dosage up to 24mg/day (Suboxone/buprenorphine) or 17.1/4.2mg (Zubsolv) on an initial
prescription.
Opiate Dependence Agents Prior Authorization Con’t
103
Other Criteria Con’t RE - AUTHORIZATION:
• Consistent use of buprenorphine/naloxone during the prior 3 months, as verified with
pharmacy data. If inconsistent use is noted upon database search (this would NOT include
changes in buprenorphine/naloxone dosing), then written explanation as to why
buprenorphine/naloxone should be continued despite apparent noncompliance would be
needed;
• Documentation of regular (every one to two months) urine tests that are negative for opiates
since previous authorization;
• Documentation of consistent participation in formal counseling by a licensed behavioral
health provider since previous authorization (D&A counselor is preferred, but not required).
12-step program participation, by itself, is not acceptable;
• Documentation of ongoing behavioral health care for co-existing behavioral health
disorders;
For patients consistently off opiates and taking buprenorphine/naloxone for an extended
period of time and who have successfully completed prescribed formal D&A counseling
programs, documentation of active engagement in “after-care” programs, such as NA or AA
or equivalent, will be accepted instead of the above formal counseling requirement;
Documentation must be provided for renewals after the first year that indicate the
prescriber has reevaluated the patient on an annual basis for a dosage lower than
16mg/day.
Coverage Duration for Re-Authorization:
If these criteria are met, then an additional 6 months of buprenorphine/naloxone will be
authorized (1 month dispensed at a time). If the criteria are not met, psychiatrist review will
be necessary to determine whether other factors would support medical necessity for
continuation of buprenorphine/naloxone.
Review Date: 12/2015
NOTE: Clinical reviewer must override criteria when, in his/her professional
judgment, the requested item is medically necessary.
104
Field Name
Prior Authorization
Group Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber
Restrictions
Coverage Duration
Other Criteria
CHELATING AGENTS
Field Description
FORMULARY STATUS Specialty Tier (PA required)
• Exjade® (Deferasirox) Tablet for Oral Suspension
• Jadenu® (Deferasirox) Tablet
Medically accepted indications are defined using the following sources:
the Food and Drug Administration (FDA), Micromedex, American
Hospital Formulary Service (AHFS), United States Pharmacopeia Drug
Information for the Healthcare Professional (USP DI), the Drug Package
Insert (PPI), or disease state specific standard of care guidelines.
N/A
See “other criteria”
N/A
N/A
If the above conditions are met, the request will be approved with a 6
month duration; if the criteria are not met, the request will be referred to a
clinical reviewer for medical necessity review.
Chronic iron overload due to blood transfusions:
For Pediatric Population:
• Patient must be > 2 years old and < 21 years old
and
• Diagnosis of chronic iron overload due to blood transfusions
and
• Patient receiving blood transfusions on a regular
basis/participating in blood transfusion program
and
• Serum Ferritin concentration is consistently > 1000 mcg/L. If the
serum ferritin levels fall consistently below 500 mcg/L, Exjade
or Jadenu must be discontinued
and
• The medication requested is being prescribed at an FDA
approved dose
For Adult Population: • Patient must be > 21 years old
and
• Diagnosis of chronic iron overload due to blood transfusions
and
• Patient receiving blood transfusions on a regular
basis/participating in blood transfusion program
and
• Serum Ferritin concentration is consistently > 1000 mcg/L. If the
serum ferritin levels fall consistently below 500 mcg/L, Exjade
or Jadenu must be discontinued
and
• Documented patient is unable to use deferoxamine (Desferal)
•
parenterally
and
The medication requested is being prescribed at an FDA
approved dose
Chronic iron overload in non-transfusion dependent thalassemia
Syndromes:
• Patient must be ≥ 10 years old
and
• Diagnosis of thalassemia syndrome
and
• Liver iron content (LIC) by liver biopsy of ≥ 5 mg Fe/g dry
weight
and
• Serum ferritin level on ≥ 2 measurements one month apart of >
300mcg/L
and
• The medication requested is being prescribed at an FDA
approved dose
Revision/Review
Date 07/2016
Medical Director/clinical reviewer must override criteria when, in
his/her professional judgement, the requested item is medically
necessary.
Field Name
Prior Authorization
Group Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber Restrictions
Coverage Duration
Other Criteria
Revision/Review Date
02/2016
Field Description
Oxycontin® Extended Release
Oxycontin® (oxycodone) tablets
Medically accepted indications are defined using the following
sources: the Food and Drug Administration (FDA), Micromedex,
American Hospital Formulary Service (AHFS), United States
Pharmacopeia Drug Information for the Healthcare Professional (USP
DI), the Drug Package Insert (PPI), or disease state specific standard
of care guidelines.
N/A
See “other criteria”
N/A
N/A
If the above conditions are met, the request will be approved with a 6
month duration. If the conditions are not met, the request will be sent
to a Medical Director/clinical reviewer for medical necessity review.
Diagnosis of chronic pain requiring an opioid analgesic
AND
Documented trial and failure or intolerance to sustained-release
morphine sulfate
AND
Documented trial and failure or intolerance to fentanyl
patches).
Medical Director/clinical reviewer must override criteria when, in
his/her professional judgement, the requested item is medically
necessary.
107
PRIOR AUTHORIZATION CRITERIA for PCSK9 Inhibitors
PREFERRED STATUS: REQUIRE Prior Authorization
Repatha® (evolocumab) - Repatha® is PREFERRED AGENT
Praluent® (alirocumab)
INITIAL CRITERIA FOR PCSK9 INHIBITORS:
Requests should not be approved as monotherapy
Diagnosis of Familial Hypercholesterolemia (FH)
Patient is 13 year of age or older.
Prescriber must be cardiologist or a specialist in the treatment of lipid disorders.
Documentation submitted includes patient’s complete medical history /co-morbidities.
For patients with a confirmed diagnosis of familial hypercholesterolemia (FH) with chart
notes or clinical labs including 2 of the following:
Autosomal Dominant Hypercholesterolemia Genetic Testing Reflex Panel
(ADHP Panel)
documented strong (first and second degree relatives) family history of high
levels of LDL and/or heart attack and relationship to member
documented chart notes of clinical manifestations of FH such as xanthomas or
inflamed tendons
Documentation of two fasting lipid panel lab reports within the past 12 months with
abnormal LDL cholesterol levels (>70).
Documented claim history or chart notes showing consistent therapy (3 months) with
atorvastatin 80mg OR Crestor (Rosuvastatin) 40mg (OR documentation has been
provided that patient is of Asian descent in which Crestor 20mg is the max dose) with
inadequate response OR a documented medical reason (e.g. intolerance, hypersensitivity)
for not utilizing one of these therapies to manage their medical condition.
If request indicates that the patient is “statin intolerant”, documentation was provided of
agents tried, including description of the side effects, duration of therapy, “wash out”, retrial, and then change in agents, or change in dose of agents.
Documentation submitted includes an attestation that the patient is following a “heart
healthy” diet.
Documentation submitted indicates the patient is a non-smoker or is actively quitting
smoking.
If request is for Praluent®, documentation of trial and failure or a medical reason has been
provided as to why the member is not able to utilize Repatha® to manage their medical
condition.
108
OR
Diagnosis of atherosclerotic cardiovascular disease (ASCVD)
Requests should not be approved as monotherapy
Patient is 18 year of age or older.
Prescriber must be cardiologist or a specialist in the treatment of lipid disorders.
Documentation submitted includes patient’s complete medical history /co-morbidities.
For patients with a confirmed CLINICAL diagnosis of atherosclerotic cardiovascular
disease (ASCVD) requiring additional lowering of low-density lipoprotein (LDL)
cholesterol :
documentation has been submitted that the patient is receiving and will continue
to receive maximally tolerated doses of statins
Documentation of angiogram or stress test results indicating ASCVD has been
submitted with request.
Patient has history of acute coronary syndromes, history of MI, stable or unstable
angina, coronary or other arterial revascularization, stroke, TIA, or peripheral
arterial disease presumed to be of atherosclerotic origin.
Documentation of two fasting lipid panel lab reports within the past 12 months with
abnormal LDL cholesterol levels (>70).
Documented claim history or chart notes showing consistent therapy (3 months) with
atorvastatin 80mg OR Crestor (Rosuvastatin) 40mg (OR documentation has been
provided that patient is of Asian descent in which Crestor 20mg is the max dose) with
inadequate response OR a documented medical reason (e.g. intolerance, hypersensitivity)
for not utilizing one of these therapies to manage their medical condition.
If request indicates that the patient is “statin intolerant”, documentation was provided of
agents tried, including description of the side effects, duration of therapy, “wash out”, retrial, and then change in agents, or change in dose of agents.
Documentation submitted includes an attestation that the patient is following a “heart
healthy” diet.
Documentation submitted indicates the patient is a non-smoker or is actively quitting
smoking.
If request is for Praluent®, documentation of trial and failure or a medical reason has been
provided as to why the member is not able to utilize Repatha® to manage their medical
condition.
If all of the above conditions are met, the request will be approved for 3 month duration; if all of
the above criteria are not met, the request is referred to a Medical Director/clinical reviewer for
medical necessity review.
109
REAUTHORIZATION CRITERIA FOR PCSK9 INHIBITORS:
Prescriber must be cardiologist or a specialist in the treatment of lipid disorders.
Documentation submitted indicates that the member has obtained clinical benefit from
the medication including repeat fasting lipid panel lab report, and the member has had at
least a 50% reduction in LDL or has achieved goal of <70.
The patient’s claim history shows consistent therapy (i.e. monthly fills)
If all of the above conditions are met, the request will be approved for 6 month duration; if all of
the above criteria are not met, the request is referred to a Medical Director/clinical reviewer for
medical necessity review.
NOTE: Medical Director/clinical reviewer must override criteria when, in his/her
professional judgment, the requested item is medically necessary.
Revision/Review Date: 4/2016
110
Field Name
Prior Authorization
Group Description
Drugs
Field Description
PEDICULICIDES
FORMULARY STATUS Formulary, Pays at Point-of-Sale
Permethrin OTC: Lotion / cream rinse and liquid
Pyrethrins/Piperonyl Butoxide OTC: Shampoo
FORMULARY STATUS Formulary, Requires Step Therapy
(Second Line)
Natroba (spinosad): Topical Suspension
Note: Patient must meet #1 & #2 criteria for approval of initial PA
request
FORMULARY STATUS Non-Formulary, Requires Prior
Authorization (Second Line)
Eurax (crotamiton): Cream and Lotion
Lindane: Shampoo
Lycelle: Gel
Ovide (malathion): Lotion
Sklice (ivermectin): Lotion
or any newly marketed pediculicde
Note: Patient must meet criteria #1, #2 & #3 for approval of initial
PA request.
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber Restrictions
Coverage Duration
Medically accepted indications are defined using the following
sources: the Food and Drug Administration (FDA), Micromedex,
American Hospital Formulary Service (AHFS), United States
Pharmacopeia Drug Information for the Healthcare Professional (USP
DI), the Drug Package Insert (PPI), or disease state specific standard
of care guidelines.
N/A
See “other criteria”
N/A
N/A
If the criterion is met, the request will be approved for initial
authorization. For re – authorization, a maximum of 2 treatments in a
30 day period will be approved. If the criterion is not met, the request
will be referred to a Clinician for medical necessity review.
Other Criteria
Initial Authorization:
Diagnosis of pediculus capitus (head lice and its eggs)
Documented intolerance or hypersensitivity to a first line agent
OR
Documented trial and failure of a first line agent within the
previous 45 days, but no earlier than 7 days after the original
fill.
Documented intolerance or hypersensitivity to a second line
agent
OR
Documented trial and failure of a second line agent within the
previous 45 days, but no earlier than 7 days after the original
fill
Re - Authorization:
Natroba can be approved for a second treatment if live lice are
present 7 days after the initial treatment.
Ovide can be approved for a second treatment if live lice are
present 7-9 days after the initial treatment.
Revision/Review Date
07/2016
Medical Director/clinical reviewer must override criteria when, in
his/her professional judgement, the requested item is medically
necessary.
Field Name
Prior Authorization
Group Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber Restrictions
Coverage Duration
Other Criteria
Field Description
Ponstel®
Ponstel® (mefenamic acid) capsules
Medically accepted indications are defined using the following
sources: the Food and Drug Administration (FDA), Micromedex,
American Hospital Formulary Service (AHFS), United States
Pharmacopeia Drug Information for the Healthcare Professional (USP
DI), the Drug Package Insert (PPI), or disease state specific standard
of care guidelines.
N/A
See “other criteria”
N/A
N/A
If the criteria are met, the request will be approved with up to a 1
month duration; if the criteria are not met, the request will be referred
to a clinical reviewer for medical necessity review.
Initial Authorization:
• Diagnosis of acute, mild-to-moderate pain or primary
dysmenorrhea.
AND
• Documented trial and failure with therapeutic prescription doses
or intolerance to at least three preferred NSAIDs for at least 2
weeks (14 days) of duration for each NSAID.
OR
• Documented trial and failure with therapeutic doses or
intolerance to Celebrex.
Revision/Review Date
04/2016
Medical Director/clinical reviewer must override criteria when, in
his/her professional judgement, the requested item is medically
necessary.
PRIOR AUTHORIZATION CRITERIA
PROTON PUMP INHIBITORS (PPIs)
PRILOSEC (generic omeprazole capsule), PREVACID (lansoprazole SoluTab: 15mg, 30mg ) (For members < 9 years old
only), PROTONIX (pantoprazole tablet: 20m g) – First Line Agents
PREVACID 24HR OTC (lansoprazole capsules), ZEGERID OTC (omeprazole/sodium bicarbonate) – Second Line Agents
ACIPHEX (rabeprazole capsule), DEXILANT (dexlansoprazole capsule), NEXIUM (esomeprazole capsule) (packet for oral
suspension), OMEPRAZOLE OTC (omeprazole tablet), PREVACID (lansoprazole) Capsule,
PREVACID (lansoprazole) SoluTab (Patients 10 years of age and older), PRILOSEC OTC (omeprazole tablet),
PRILOSEC RX (omeprazole packet for oral suspension), PROTONIX (pantoprazole packet for oral suspension for Patients 10
years of age and older), VIMOVO (esomeprazole/naproxen), ZEGERID (omeprazole/sodium bicarbonate capsule and oral
suspension – Third Line Agents
PA Criteria
Criteria Details
Covered Uses
Medically accepted indications are defined using the following sources: the Food
and Drug Administration (FDA), Micromedex, American Hospital Formulary
Service (AHFS), United States Pharmacopeia Drug Information for the Healthcare
Professional (USP DI), and the Drug Package Insert.
Exclusion
Criteria
None
Required Medical
Information
See “other criteria.”
Age Restrictions
Prescriber
Restrictions
Coverage
Duration
Other Criteria
None
See “other criteria”
If the criterion is met, the request will be approved with a 12 month duration
depending on the diagnosis and usual treatment therapy. If the criterion is not met,
the request will be referred to a Clinician for medical necessity review.
AUTHORIZATION:
1. Presumed or documented diagnosis of duodenal ulcer, H.pylori, gastric
ulcer, GERD, erosive esophagitis, or hypersecretory disease.
2. Documented trial and failure or intolerance with omeprazole 20mg or
pantoprazole tablets once daily for a minimum of 3 weeks of therapy
within the previous 60 days.
3. Documented trial and failure or intolerance with Prevacid 24HR
OTC 30mg once daily OR Zegerid OTC 20mg/1100mg once daily
for a minimum of 3 weeks of therapy.
***NOTE: Patient must meet criteria #1 & #2 for approval of initial PA
request for Prevacid 24 hour OTC and Zegerid OTC. For third line agents,
listed, patient must meet criteria #1, #2 & #3 for approval of initial PA
request.***
Doses Greater Than Once Daily After Meeting Criteria For PPI:
1. Confirmed diagnosis of GERD, erosive esophagitis, or hypersecretory
disease OR
2. Evaluation made by gastroenterologist and /or otolaryngologist
recommending higher doses of PPI.
Review Date: 11/2015
NOTE: Clinical reviewer must override criteria when, in his/her professional
judgment, the requested item is medically necessary.
113
PRIOR AUTHORIZATION CRITERIA
PROTOPIC® (tacrolimus)
PA Criteria
Covered Uses
Criteria Details
Medically accepted indications are defined using the following sources: the Food and
Drug Administration (FDA), Micromedex, American Hospital Formulary Service
(AHFS), United States Pharmacopeia Drug Information for the Healthcare Professional
(USP DI), and the Drug Package Insert.
Exclusion
Criteria
None
Required
Medical
Information
See “other criteria”
Age Restrictions
None
Prescriber
Restrictions
Must be written by a family practitioner, pediatrician or dermatologist.
Coverage
Duration
If the criterion is met, the request will be approved with a 6 month duration. If the
criterion is not met, the request will be referred to a Clinician for medical necessity
review.
Other Criteria
AUTHORIZATION:
INDICATIONS
FDA
Diagnosis
of moderate to severe atopic dermatitis in non - immunocompromised
patient in whom the use of alternative, conventional therapy is deemed inadvisable
.
because of potential risks, or who are not adequately responsive to or intolerant of
alternative conventional therapies.
AND
Prescription written by a family practitioner, pediatrician or dermatologist.
BOXED WARNING:
Although a causal relationship has not been established, rare cases of malignancy (e.g., skin
and lymphoma) have been reported in patients treated with other topical calcineurin
inhibitors. Therefore, continuous long-term use of topical calcineurin inhibitors should be
avoided, and application should be limited to areas of involvement with atopic dermatitis.
NOTE: Clinical reviewer must override criteria when, in his/her professional
Review Date: 6/2015 judgment, the requested item is medically necessary.
114
Field Name
Prior Authorization
Group Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber Restrictions
Coverage Duration
Other Criteria
Revision/Review Date
07/2016
Field Description
Pulmicort® Respules (budesonide)
Pulmicort® Respules (budesonide) inhalation suspension
Medically accepted indications are defined using the following
sources: the Food and Drug Administration (FDA), Micromedex,
American Hospital Formulary Service (AHFS), United States
Pharmacopeia Drug Information for the Healthcare Professional (USP
DI), the Drug Package Insert (PPI), or disease state specific standard
of care guidelines.
N/A
See “other criteria”
N/A
N/A
If the above conditions are met, the request will be approved with a 12
month duration. If the conditions are not met, the request will be sent
to a Medical Director/clinical reviewer for medical necessity review.
Diagnosis of chronic asthma for patients of ages 12 months to 8
years will process at the point of sale without prior authorization
required if dosed within appropriate dosing guidelines as follows:
o 0.25mg/2mL once daily
o 0.5mg/2mL once daily or twice daily
o 1.0mg/2mL once daily
A dose of 0.25mg/2mL twice daily will be approved if prescriber
indicates that once daily dosing is not efficacious and determines
that increasing the dose (i.e. 0.5mg/2mL once daily) is not
appropriate for the patient.
All other requests will be referred to a Medical Director/clinical
reviewer for medical necessity review.
Medical Director/clinical reviewer must override criteria when, in
his/her professional judgement, the requested item is medically
necessary.
Field Name
Prior Authorization
Group Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber
Restrictions
Coverage Duration
Other Criteria
Field Description
Pulmonary Arterial Hypertension (PAH) PA Criteria
Adcirca® (tadalafil), Letairis™ (ambrisentan), Revatio® (sildenafil),
Tracleer® (bosentan), Opsumit ® (macitentan), Orenitram™
(Treprostinil Diolamine), Adempas ® (riociguat), Uptravi® (selexipag),
Flolan® (epoprostenol), Remodulin® (Treprostinil), Tyvaso®
(Treprostinil), Ventavis ® (Iloprost) and any other newly marketed
PAH treatment agents.
Medically accepted indications are defined using the following sources:
the Food and Drug Administration (FDA), Micromedex, American
Hospital Formulary Service (AHFS), United States Pharmacopeia Drug
Information for the Healthcare Professional (USP DI), the Drug Package
Insert (PPI), or disease state specific standard of care guidelines.
N/A
See “other criteria”
N/A
Prescriber must be pulmonologist or cardiologist
If all of the above conditions are met, the request will be approved for 6
month duration, with the exception of Orenitram™ or Uptravi® requests.
Orenitram™ and Uptravi® requests will be initially approved for 28 days
(approve Uptravi® for an initial 200mcg bottle of #140 for 28 days,
subsequent refill with Titration Pack for 28 days or documentation that
patient has achieved highest tolerated dose. Orenitram™ requests
should be approved for 28 days using dose the proper tablets required
according to the titration schedule) Once patient has achieved
maintenance dosing, further refills can be approved for 6 month
duration. Patients new to the plan would be approved for 6 months with
documentation patient is stable on dose. If the conditions are not met,
the request will be sent to a Medical Director/clinical reviewer for
medical necessity review.
Initial Authorization:
Documentation of a confirmed diagnosis of pulmonary arterial
hypertension (PAH) World Health Group (WHO Group I), and
functional class.
Medication is being used for an FDA approved functional class.
Documentation that the patient has undergone acute vasoreactivity
testing and whether or not the results were favorable. For those
patients who demonstrated a favorable response to the acute
vasoreactivity testing (defined as a fall in mean pulmonary arterial
pressure [PAPm] of at least 10 mm Hg to < 40 mm Hg with an
116
increased or unchanged cardiac output), then documentation that
his/her pulmonary hypertension has progressed despite maximal
medical treatment with a calcium channel blocker, or documentation
has been provided of medical reason why patient is not able to use a
calcium channel blocker.
Documentation of the patient’s current weight.
The medication is being recommended and prescribed by a
pulmonologist or a cardiologist at a dose that is within FDA approved
guidelines.
If the request is for Revatio® oral suspension, documentation has
been submitted as to why patient is unable to use sildenafil or tablets
(e.g. difficulty swallowing)
If the request is for Opsumit® or Tracleer® the patient must have a
documented trial and failure or intolerance to Letairis™.
If the provider is requesting combination therapy with two agents
then documentation must be submitted as to why patient is unable to
be treated with monotherapy. (e.g. worsening of the symptoms of
dyspnea or fatigue, decline in functional class by at least one class or
in 6-minute walk test (6MWD) by greater than 30 minutes)
If the provider is requesting combination therapy with three agents
then documentation must be submitted of an adequate trial of
therapy with two agents of different mechanism, documentation that
the patient has been compliant with the dual therapy agents, and
documentation that the patient has clinically deteriorated (e.g.
worsening of the symptoms of dyspnea or fatigue, decline in
functional class by at least one class or in 6-minute walk test
(6MWD) by greater than 30 minutes) while on dual therapy.
For Orenitram™ and Uptravi® requests, documentation of current
dosing and titration schedule is required.
If the request is for Uptravi®, and the patient has functional class II,
documentation has been provided that the patient has tried and failed
an adequate trial (3 months) of a phosphodiesterase-5 inhibitor (e.g.
sildenafil) in combination with an endothelin receptor antagonist (e.g.
Letairis) or a medical reason has been submitted why the patient is
not able to use BOTH of these therapies before starting Uptravi®.
If the request is for Uptravi®, and the patient has functional class III,
documentation has been provided that the patient has tried and failed
an adequate trial (3 months) of a phosphodiesterase-5 inhibitor (e.g.
sildenafil) in combination with an endothelin receptor antagonist (e.g.
117
Letairis) AND epoprostenol, or a medical reason has been submitted
why the patient is not able to use ALL of these therapies before
starting Uptravi®.
Re-authorization:
Documentation has been submitted indicating the clinical benefit of
therapy (e.g. improvement in functional class, improvement in 6minute walk test, exercise capacity, or hemodynamics).
If dosing is being increased, documentation of the medical necessity
to increase the dosage is provided.
For Orenitram™ and Uptravi® requests, documentation of current
dosing and titration schedule is required.
The medication is being recommended and prescribed by a
pulmonologist or a cardiologist at a dose that is within FDA approved
guidelines.
Revision/Review
Date 4/2016
Medical Director/clinical reviewer must override criteria when, in
his/her professional judgment, the requested item is medically
necessary.
118
Field Name
Prior Authorization
Group Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber Restrictions
Coverage Duration
Other Criteria
Field Description
Qualaquin®
Qualaquin®(quinine sulfate) capsules
Medically accepted indications are defined using the following
sources: the Food and Drug Administration (FDA), Micromedex,
American Hospital Formulary Service (AHFS), United States
Pharmacopeia Drug Information for the Healthcare Professional (USP
DI), the Drug Package Insert (PPI), or disease state specific standard
of care guidelines.
Treatment or prevention of nocturnal leg cramps, prevention of
malaria, treatment of complicated Plasmodium falciparum malaria
See “other criteria”
N/A
N/A
If the criteria are met, the request will be approved with up to a 7 day
duration; if the criteria are not met, the request will be referred to a
clinical reviewer for medical necessity review.
Initial Authorization:
Revision/Review Date
04/2016
Treatment of uncomplicated Plasmodium falciparum malaria.
Medical Director/clinical reviewer must override criteria when, in
his/her professional judgement, the requested item is medically
necessary.
Field Name
Prior Authorization
Group Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber Restrictions
Coverage Duration
Other Criteria
Revision/Review Date
04/2016
Field Description
Ranexa
Ranexa® (ranolazine) tablet
Medically accepted indications are defined using the following
sources: the Food and Drug Administration (FDA), Micromedex,
American Hospital Formulary Service (AHFS), United States
Pharmacopeia Drug Information for the Healthcare Professional (USP
DI), the Drug Package Insert (PPI), or disease state specific standard
of care guidelines.
N/A
See “other criteria”
N/A
N/A
If the criteria are met, the request will be approved with up to a 12
month duration; if the criteria are not met, the request will be referred
to a clinical reviewer for medical necessity review.
Initial Authorization
• Documented trial and failure, contraindication or
intolerance t o two classes of anti-anginal therapeutic
alternatives (i.e. long acting nitrates, beta-blockers, calcium
channel blockers).
Medical Director/clinical reviewer must override criteria when, in
his/her professional judgement, the requested item is medically
necessary.
Field Name
Prior Authorization
Group Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber Restrictions
Coverage Duration
Other Criteria
Field Description
Restasis®
Restasis® (cyclosporine)
Medically accepted indications are defined using the following
sources: the Food and Drug Administration (FDA), Micromedex,
American Hospital Formulary Service (AHFS), United States
Pharmacopeia Drug Information for the Healthcare Professional (USP
DI), the Drug Package Insert (PPI), or disease state specific standard
of care guidelines.
N/A
See “other criteria”
N/A
Prescriber must be an optometrist, ophthalmologist or rheumatologist.
If the criterion is met, the request will be approved for a one month
supply of the medication with up to a 6 month authorization. If the
criterion is not met, the request will be referred to a Clinician for
medical necessity review.
Initial Authorization:
Revision/Review Date
07/2016
Diagnosis of dry eye syndrome (decreased tear production)
whose lack of tear production is presumed to be suppressed
due to ocular inflammation associated with
keratoconjunctivitis sicca.
AND
Documented trial and failure or intolerance to a therapeutic
trial of artificial tear therapy for a period of 3 months.
Medical Director/clinical reviewer must override criteria when, in
his/her professional judgement, the requested item is medically
necessary.
Field Name
Prior Authorization
Group Description
Drugs
Field Description
Second Generation Antihistamines PA Criteria
FORMULARY STATUS Formulary, Pays at Point-of-Sale (First Line)
ALLEGRA® (fexofenadine) (Only children < 2 years old will pay at
point of sale)
CLARITIN® (loratadine) (generic) tablets, 10 mg orally disintegrating
tablets, oral syrup
ZYRTEC® (cetirizine) (generic) tablets, oral solution
ZYRTEC-D® 12 HOURS (cetirizine/pseudoephedrine) (generic)
CLARITIN-D® 12 HOUR (loratadine/pseudoephedrine) (generic)
CLARITIN-D® 24 HOUR (loratadine/pseudoephedrine) (generic)
FORMULARY STATUS Formulary, Requires Step Therapy (Second
Line)
ALLEGRA® (fexofenadine) (generic) oral suspension and 180 mg
tablets only
ALLEGRA® (fexofenadine)
XYZAL® (levocetirizine) tablets
FORMULARY STATUS Non-Formulary, Requires Prior
Authorization (Third Line)
ALLEGRA® (fexofenadine) 60 mg tablets
ALLEGRA-D® 12 HOUR (fexofenadine/pseudoephedrine)
ALLEGRA-D® 24 HOUR (fexofenadine/pseudoephedrine)
CLARITIN® (loratadine) (generic) 5 mg orally disintegrating tablets
CLARINEX® (desloratadine)
CLARINEX-D® 12 HOUR (desloratadine/pseudoephedrine)
SEMPREX-D (pseudoephedrine/acrivas)
XYZAL® (levocetirizine) oral solution
ZYRTEC® (cetirizine) (generic) chewable tablets, orally disintegrating
tablets, capsules
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber
Restrictions
Coverage Duration
Other Criteria
Medically accepted indications are defined using the following sources:
the Food and Drug Administration (FDA), Micromedex, American
Hospital Formulary Service (AHFS), United States Pharmacopeia Drug
Information for the Healthcare Professional (USP DI), the Drug Package
Insert (PPI), or disease state specific standard of care guidelines.
N/A
See “other criteria”
N/A
N/A
If the above conditions are met, the request will be approved with a 12
month duration; If the conditions are not met, the request will be sent to
a Medical Director/clinical reviewer for medical necessity review.
NOTE: Patient must meet #1, #2, & #3 criteria for approval of PA
123
request.
PA CRITERIA FOR APPROVAL:
1. Diagnosis of seasonal allergic rhinitis with or without nasal
congestion, perennial allergic rhinitis with or without nasal
congestion, or urticaria.
2. Documented trial and failure or intolerance to a first line
loratadine AND cetirizine product for at least 4 weeks (28 days)
of therapy each within the past 12 months or a minimum of 2
weeks of therapy or intolerance to Claritin-D and Zyrtec-D
within the past 12 months.
3. Documented trial and failure or intolerance to fexofenadine or
levocetirizine tablets for at least 4 weeks (28 days) of therapy in
the past 12 months.
Revision/Review
Date 02/2016
Medical Director/clinical reviewer must override criteria when, in
his/her professional judgement, the requested item is medically
necessary.
124
Field Name
Prior Authorization
Group Description
Drugs
Field Description
SEDATIVE HYPNOTICS
FORMULARY STATUS Formulary, Pays at Point-of-Sale (First Line)
• Ambien (zolpidem)
• Sonata (zaleplon)
FORMULARY STATUS: Formulary, Requires Step Therapy (Second
Line)
Lunesta (eszopiclone) tablet
Note: Patient must meet #1 & #2 criteria for approval of initial PA
request
FORMULARY STATUS Non-Formulary, Requires Prior
Authorization (Second Line)
Ambien CR (zolpidem) extended-release tablet
Rozerem (ramelteon) tablet
Edular (zolpidem) sublingual tablet
Intermezzo (zolpidem) sublingual tablet
Zolpimist (zolpidem) oral solution
NOTE: Patient must meet criteria #1, #2 & #3 for approval of initial
PA request.
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber
Restrictions
Coverage Duration
Other Criteria
Medically accepted indications are defined using the following sources:
the Food and Drug Administration (FDA), Micromedex, American
Hospital Formulary Service (AHFS), United States Pharmacopeia Drug
Information for the Healthcare Professional (USP DI), the Drug Package
Insert (PPI), or disease state specific standard of care guidelines.
N/A
See “other criteria”
N/A
N/A
If the criteria are met, the request will be approved with a 12 month
duration; if the criteria are not met, the request will be referred to a
clinical reviewer for medical necessity review.
PA CRITERIA FOR APPROVAL:
1. Diagnosis of insomnia.
2. Documented trial and failure or intolerance to Ambien (zolpidem) or
Sonata (zaleplon) for at least 2 weeks (14 days) of therapy.
3. Documented trial and failure or intolerance to Lunesta (eszopiclone)
for at least 2 weeks (14 days) of therapy.
NOTE: Rozerem can be approved as a first line agent if there is a
history of substance abuse.
Revision/Review
Date 04/2016
Medical Director/clinical reviewer must override criteria when, in
his/her professional judgement, the requested item is medically
necessary.
SEROSTIM PRIOR AUTHORIZATION CRITERIA
SEROSTIM ® (somatropin) Formulary Status: Non-formulary
PA CRITERIA FOR INITIAL APPROVAL FOR HIV RELATED WASTING OR CACHEXIA:
The patient is an adult (≥18 y/o) and has a documented clinical diagnosis of HIV
Prescriber is HIV or infectious disease specialist
The patient is receiving optimal highly active antiretroviral therapy (HAART) as documented by
a recent (with in past 2 months) infectious disease specialist consultation or by recent (with in
past 2 months) laboratory blood analysis indicating plasma HIV RNA of less than 50 copies/ml
Documentation was submitted that indicates that the member does not have cancer (excluding
Kaposi’s sarcoma & Lymphoma)
Documentation was submitted that indicates that the member does not have any
psychiatric disorders, such as anxiety and depression, or documentation was submitted
that the member is receiving treatment for a psychiatric disorder
Documentation was submitted that indicates that the member does not have any active
opportunistic infections (thrush, MAC), diarrhea and GI infections, or that if they have any of
these conditions it is clinically resolved and stabilized with treatment
For male patients, laboratory values were submitted indicating testosterone levels are within
normal limits, or that the patient is receiving testosterone supplementation and documentation was
submitted indicated testosterone levels are within normal limits
The patient is receiving documented nutritional support
Documentation has been provided including patient’s weights, BMI (in kg/m2), and lean body
mass (LBM) by DEXA (baseline and repeat over the last six months)
Documentation provided demonstrates an involuntary weight loss >10% of baseline body
weight associated with either chronic diarrhea (two or more loose stools per day for ≥1
month) or chronic weakness and documented fever for ≥1 month that is not attributable to
a concurrent condition other than HIV infection itself or 2) current weight loss > 5% in a 1mo period or 3) actual BMI (in kg/m2) < 19
The patient has tried a 2 month or more course of therapy with megestrol acetate, dronabinol
or cyproheptadine for appetite stimulation in the past 2 months or has a documented medical
reason for not taking megestrol acetate, dronabinol or cyproheptadine.
The patient has tried a 2 month course of therapy with anabolic steroids (e.g., Oxandrin) in
the past 2 months or has a medical reason for not taking an anabolic steroid.
If all of the above conditions are met, the request will be approved with a 4-week duration; if all
of the above criteria are not met, the request is referred to a Medical Director/clinical reviewer
for medical necessity review.
PA CRITERIA FOR RE-APPROVAL FOR HIV RELATED W ASTING OR CACHEXIA:
Documentation was sent in at the end of 4 weeks of a repeat BIA analysis that shows the
patient’s lean body mass has stabilized or improved
If the last trial of Serostim® was in the distant past and was successful, then evaluate the
patient as naïve
If all of the above conditions are met, the request will be approved for 12 weeks. If all of the above
criteria are not met, the request is referred to a Medical Director/clinical reviewer for medical
necessity review.
PA CRITERIA FOR INITIAL APPROVAL FOR HIV RELATED LIPODYSTROPHYor
HIV ASSOCIATED ADIPOSE REDISTRIBUTION SYNDROME:
The patient is an adult (≥18 y/o) and has a documented clinical diagnosis of HIV.
Documentation that the patient does not have diabetes mellitus and is not receiving any
insulin or insulin-sensitizing agents.
Documentation that the patient is compliant with an unchanged HAART for at least 3
months prior to the initiation of therapy.
Documentation was submitted that indicates that the member does not have an active
infection or malignancy(excludes patients with less than five cutaneous Kaposi’s sarcoma
lesions).
Documentation that the patient does not have untreated or uncontrolled hypertension (i.e.
blood pressure > 140/90 mm Hg).
Prescriber is HIV or infectious disease specialist
A letter of medically necessity documenting the evidence of HIV related lipodystrophy.
The medication is prescribed at a medically accepted dose per the medical compendia (i.e.
Micromedex, DrugPoints and AHFS drug information) as defined by the Social Security
Act or per the standard of care guidelines.
If all of the above conditions are met, the request will be approved with a 12-week duration; if all of
the above criteria are not met, the request is referred to a Medical Director/clinical reviewer for
medical necessity review.
PA CRITERIA FOR RE-APPROVAL FOR HIV RELATED LIPODYSTROPHY or
HIV ASSOCIATED ADIPOSE REDISTRIBUTION SYNDROME:
Duration of therapy does not exceed 9 months.
The prescribing physician has provided documentation as to the clinical
benefits of the medication supporting continued treatment.
The medication is prescribed at a medically accepted dose per the medical compendia (i.e.
Micromedex, DrugPoints and AHFS drug information) as defined by the Social Security Act
or per the standard of care guidelines.
If all of the above conditions are met, the request will be approved with a 24-week duration (9
months total); if all of the above criteria are not met, the request is referred to a Medical
Director/clinical reviewer for medical necessity review.
PA CRITERIA FOR AUTHORIZATION FOR USE IN A NON-FDA APPROVED
MEDICALLY ACCEPTED INDICATION:
The medication is recommended and prescribed by a specialist in the field to treat the
member’s respective medical condition.
The medication is prescribed for a non-FDA approved indication but is considered to be
a medically accepted use of the medication per the medical compendia (i.e. Micromedex,
DrugPoints and AHFS drug information) as defined by the Social Security Act or the
standard of care guidelines.
Documentation was submitted indicating that the member has a documented (consistent with
pharmacy claims data, OR for new members to the health plan consistent with medical chart
history) adequate trial (including dates, doses of medications) of all first line medical therapies as
recommended by the medical compendia and standard care guidelines or has another
documented medical reason (i.e. intolerance, contraindications) for not receiving or trying all
first line medical treatment(s).
The medication is prescribed at a medically accepted dose per the medical compendia as defined
by the Social Security Act or per the standard of care guidelines.
If all of the above conditions are met, the request will be approved for up to a 12-week duration. If all
of the above criteria are not met, the request is referred to a Medical Director/clinical reviewer for
medical necessity review.
PA CRITERIA FOR RE-AUTHORIZATION FOR USE IN A NON-FDA
APPROVED MEDICALLY ACCEPTED INDICATION:
The medication is recommended and prescribed by a specialist in the field to treat the
member’s respective medical condition.
The medication is being prescribed at a medically accepted dose per the medical compendia
(i.e. Micromedex, DrugPoints and AHFS drug information) as defined by the Social
Security Act or per the NCCN or ASCO standard of care guidelines.
The prescribing physician has provided documentation as to the clinical benefits of the
medication supporting continued treatment, OR the medication is being continued in
accordance with the recommended time as defined by FDA drug package insert, or per
recommendations of the medical compendium as described above, or per the standard of
care guidelines.
If all of the above conditions are met, the request will be approved for up to a 12-week duration. If
all of the above criteria are not met, the request is referred to a Medical Director/clinical reviewer
for medical necessity review.
NOTE: Physician review/clinical reviewer must override criteria when, in his/her professional
judgement, the requested item is medically necessary.
Revision/Review Date: 7/2016
SOLIRIS PRIOR AUTHORIZATION CRITERIA
SOLIRIS®(Eculizumab)
Formulary Status: Non-formulary
PA CRITERIA FOR APPROVAL FOR Paraxysmal nocturnal hemoglobinuria
(PNH):
• Patient has a confirmed diagnosis of paroxysmal nocturnal hemoglobinuria
(PNH)
• Documentation was submitted with the following lab results within 30 days of
request: CBC with differential, iron studies (serum iron, total iron binding capacity, and
ferritin), the last pre-transfusion hemoglobin level, a Lactase dehydrogenase (LDH)
level, a PNH type III erythrocyte level proportion of 10% of more, serum creatinine,
AST, and urinalysis
• Documentation submitted indicates that the patient has been vaccinated with the
meningococcal vaccine at least 2 weeks prior to initiation of Soliris therapy and/or
revaccinated according to current medical guidelines for vaccine use
• The medication is being prescribed by a hematologist at an FDA approved dosage.
If all of the above conditions are met, the request will be approved for up to a 6-month
duration; if all of the above criteria are not met, the request is referred to a Medical
Director/clinical reviewer for medical necessity review.
REAUTHORIZATION CRITERIA for PNH:
• For first reauthorization requests: documentation from medical chart was
submitted indicating that a hematologist has evaluated the member and recommends
continuation of therapy due to submitted clinical/diagnostic documentation that
demonstrates that the member has benefited from the medication (e.g. reduced
number of red blood cell transfusions, decreased LDH level, improved hemoglobin
levels, increase in PNH type III erythrocytes, improved fatigue or quality of life)
since beginning therapy with Soliris.
• For additional reauthorization requests beyond 12 months of therapy:
documentation from medical chart was submitted indicating that a hematologist has
evaluated the member and recommends continuation of therapy due to the member
has remained clinically stable while on Soliris (e.g. red blood cell transfusion
requirements have remained the stable or reduced, LDH level remained close to upper
limits of normal, hemoglobin levels remaining stable, PNH type III erythrocytes stable
or improved, low to no fatigue and continues with improved quality of life) while
taking Soliris therapy.
• Documentation was submitted indicating the date of the member’s last
meningococcal vaccine.
• The medication is being prescribed by a hematologist at an FDA approved dosage.
If all of the above conditions are met, the request will be approved for up to a 6-month
duration; if all of the above criteria are not met, the request is referred to a Medical
Director/clinical reviewer for medical necessity review.
PA CRITERIA FOR APPROVAL for Atypical Hemolytic Uremic Syndrome (aHUS)
• Patient has a confirmed diagnosis of aHUS (e.g. genetic testing, chart notes or
labs indicating microangiopathic hemolytic anemia, thrombocytopenia, and acute
kidney injury)
• Documentation provided indicates disease is NOT caused by Shiga toxin E. coli
related hemolytic uremic syndrome (STEC-HUS)
• Documentation submitted indicates that the patient has been vaccinated with the
meningococcal vaccine at least 2 weeks prior to initiation of Soliris therapy and/or
revaccinated according to current medical guidelines for vaccine use
• The medication is being prescribed by a hematologist at an FDA approved
dosage
• Documentation was submitted with the following lab results within 30 days of
request: CBC with differential, a Lactase dehydrogenase (LDH) level, serum
creatinine, AST, and urinalysis
If all of the above conditions are met, the request will be approved for up to a 6-month
duration; if all of the above criteria are not met, the request is referred to a Medical
Director/clinical reviewer for medical necessity review.
REAUTHORIZATION CRITERIA for aHUS:
For first reauthorization requests:
• Documentation from medical chart was submitted indicating that a hematologist
has evaluated the member and recommends continuation of therapy due to submitted
clinical/diagnostic documentation that demonstrates that the member has benefited
from the medication since beginning therapy with Soliris.
• Medication is being prescribed by a hematologist at an FDA approved dosage
For additional reauthorization requests beyond 12 months of therapy:
• Documentation from medical chart was submitted indicating that a hematologist
has evaluated the member and recommends continuation of therapy due to the member
has remained clinically stable while on Soliris
• Documentation was submitted indicating the date of the member’s last
meningococcal vaccine.
• The medication is being prescribed by a hematologist at an FDA approved dosage.
FDA INDICATION:
Soliris is indicated for treatment of adult patients (18 y/o or older) with paroxysmal
nocturnal
hemoglobuinuria (PNH) to reduce hemolysis and for the treatment of patients with
atypical hemolytic uremic syndrome (aHUS) to inhibit complement-mediated
thrombotic microangiopathy.
Soliris is not indicated for the treatment of patients with Shiga toxin E. coli related
hemolytic uremic syndrome (STEC-HUS).
DOSAGE AND ADMINISTRATION:
Dosage Regimen - PNH:
600 mg as an IV infusion over 35 minutes given every 7 days for the first 4 weeks, followed
by:
900 mg IV over 35 minutes for the 5th dose 7 days later then,
900 mg IV over 35 minutes every 14 days thereafter.
Dosage Regimen - aHUS:
For patients ≥ 18 yo:
900 mg as an IV infusion over 35 minutes given every 7 days for the first 4 weeks, followed
by
1200 mg IV over 35 minutes for the 5th dose 7 days later then,
1200 mg IV over 35 minutes every 14 days thereafter.
For patients ≤ 18 yo:
Patient Body
Weight
40 kg and over
Induction
900 mg weekly x
4 doses
Maintenance
1200 mg at week 5; then
1200 mg every 2
weeks
30 kg to less than
40 kg
20 kg to less than
30 kg
10 kg to less than
20 kg
5 kg to less than 10
kg
600 mg weekly x
2 doses
600 mg weekly x
2 doses
600 mg weekly x 1
dose
300 mg weekly x 1
dose
900 mg at week 3; then 900
mg every 2 weeks
600 mg at week 3; then 600
mg every 2 weeks
300 mg at week 2; then 300
mg every 2 weeks
300 mg at week 2; then 300
mg every 3 weeks
Supplemental dose of Soliris after PE/PI (plasmapheresis or plasma exchange; or fresh
frozen plasma infusion):
Type of
Intervention
Plasmapheresis or
plasma exchange
Fresh frozen plasma
infusion
Most Recent
Soliris Dose
Supplemental Soliris Dose
With Each PE/PI Intervention
300 mg
300 mg per each plasmapheresis
or plasma exchange session
600 mg or more
600 mg per each plasmapheresis
or plasma exchange session
300 mg or more
300 mg per each unit of fresh
frozen plasma
Timing of
Supplemental
Soliris Dose
Within 60 minutes
after each
plasmapheresis or
plasma exchange
60 minutes prior to
each 1 unit of fresh
frozen plasma
infusion
REFERENCES:
1. Soliris® prescribing information. Alexion Pharmaceuticals, Inc. 1/2016
2. Hillmen P. Young NS. Schubert J. et al. The complement inhibitor eculizumab in paroxysmal nocturnal
hemoglobinuria. The New England Journal of Medicine. 2006;355:1233-1243.
3. Hill A. Richards SJ. Hillmen P. Recent developments in the understanding and management of paroxysmal
nocturnal haemoglobinuria. British Journal of Haematology. 2007;137:181-192.
4. Parker C. Omine M. Richards S. et al. Diagnosis and management of paroxysmal nocturnal hemoglobinuria.
Blood. 2005;106(12):3699-3709.
5. http://www.nlm.nih.gov/medlineplus/ency/article/003471.htm. For Definition of LDH.
Revision/Review Date: 7/2016
NOTE: Clinical reviewer must override criteria when, in his/her professional judgment, the
requested item is medically necessary.
Field Name
Prior Authorization
Group Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber Restrictions
Coverage Duration
Other Criteria
Field Description
Sporanox®
Sporanox® (itraconazole)
Medically accepted indications are defined using the following
sources: the Food and Drug Administration (FDA), Micromedex,
American Hospital Formulary Service (AHFS), United States
Pharmacopeia Drug Information for the Healthcare Professional (USP
DI), the Drug Package Insert (PPI), or disease state specific standard
of care guidelines.
N/A
See “other criteria”
N/A
N/A
If the criteria are met, the request will be approved with up to a 3
month duration; if the criteria are not met, the request will be referred
to a clinical reviewer for medical necessity review.
Initial Authorization:
• Immunocompromised patient.
OR
• Trial and failure or intolerance to a preferred oral antifungal.
OR
• Following completion of or intolerance to amphotericin B therapy.
OR
• Diagnosis of aspergillosis.
Revision/Review Date
04/2016
Medical Director/clinical reviewer must override criteria when, in
his/her professional judgement, the requested item is medically
necessary.
Field Name
Prior Authorization
Group Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber Restrictions
Coverage Duration
Other Criteria
Field Description
Stadol®
Stadol® (butorphanol) nasal spray
Medically accepted indications are defined using the following
sources: the Food and Drug Administration (FDA), Micromedex,
American Hospital Formulary Service (AHFS), United States
Pharmacopeia Drug Information for the Healthcare Professional (USP
DI), the Drug Package Insert (PPI), or disease state specific standard
of care guidelines.
N/A
See “other criteria”
N/A
N/A
If the criteria are met, the initial authorization request will be approved
for 3 months with generic medication (quantity limit of 1 bottle/30
days), the re – authorization will be approved for 6 months with
generic medication (quantity limit of 1 bottle/30 days); if the criteria
are not met, the request will be referred to a clinical reviewer for
medical necessity review.
Initial Authorization:
PAIN:
Diagnosis of pain
AND
Documented trial and failure with therapeutic doses or
intolerance to at least three oral narcotic medications including:
oxycodone, oxycodone/acetaminophen, hydromorphone,
hydrocodone/acetaminophen, acetaminophen/codeine, and
morphine sulfate (first line therapies).
MIGRAINEHEADACHE:
Diagnosis of pain from migraine headache
AND
Documented trial with therapeutic doses of at least one
recommended migraine preventative therapy (topiramate,
propranolol, timolol, divalproex sodium, amitriptyline,
nortriptyline, and verapamil).
AND
Documented trial and failure with therapeutic doses or
intolerance to abortive therapy including at least one triptan
®
and Migranal (unless contraindicated).
AND
Documented trial and failure with therapeutic doses or
intolerance to at least three oral narcotic medications including:
oxycodone, oxycodone/acetaminophen, hydromorphone,
hydrocodone/acetaminophen, acetaminophen/codeine, and
morphine sulfate.
Re-Authorization:
Patient currently under the care of a neurologist or
pain management specialist.
AND
Documentation submitted by neurologist or pain
management specialist supporting re- evaluation of
patient.
OR
Medical necessity of continued use of medication
Revision/Review Date
04/2016
Medical Director/clinical reviewer must override criteria when, in
his/her professional judgement, the requested item is medically
necessary.
Field Name
Prior Authorization
Group Description
Drugs
Covered Uses
Field Description
Skeletal Muscle Relaxants
Exclusion Criteria
Soma® (carisoprodol)
Medically accepted indications are defined using the following
sources: the Food and Drug Administration (FDA), Micromedex,
American Hospital Formulary Service (AHFS), United States
Pharmacopeia Drug Information for the Healthcare Professional (USP
DI), the Drug Package Insert (PPI), or disease state specific standard
of care guidelines.
N/A
Required Medical
Information
Age Restrictions
Documented trial and failure with NSAID or Cyclobenzaprine in last
90 days
Member is an adult greater than or equal to 18 years of age.
Prescriber Restrictions
Coverage Duration
Other Criteria
N/A
If the criteria are met, the request will be approved with up to a 6
month duration; if the criteria are not met, the request will be referred
to a clinical reviewer for medical necessity review.
Initial Authorization:
A trial of Cyclobenzaprine or an NSAID in the last 90 days is required
prior to approval of Carisoprodol:
o For members that have not tried Cyclobenzaprine or an
NSAID in the last 90 days these preferred alternatives
should be suggested.
o For members that have tried Cyclobenzaprine or an NSAID
in the last 90 days and have received Carisoprodol via step
therapy:
If the provider submits documentation indicating nonabuse with Carisoprodol the request is approved for a
31 day supply (max of 124 tablets for 31 days) for the
duration requested up to a maximum of 6 months.
If the provider does not submit documentation
indicating non-abuse with Carisoprodol the request is
approved for a single fill for a 21 day supply (max of
84 tablets for 21 days) and the provider should be made
aware that continued use of this medication will
require prior authorization and documentation that
there has been a screening by the provider for abuse.
o For members that have tried Cyclobenzaprine or an NSAID
in the last 90 days and have not received Carisoprodol:
If the provider states the member has been screened for
abuse the request can be approved for a 31 day supply
(max of 124 tablets for 31 days) for the duration
requested up to a maximum of 6 months.
If the provider does not state the member has been
screened for abuse the request is approved for a
single fill for a 21 day supply (max of 84 tablets for
21 days) and the provider should be made aware that
continued use of this medication will require prior
authorization and documentation that there has been
a screening by the provider for abuse.
Please note: Continued use of this medication will require prior
authorization and documentation that there has been a screening
by provider for abuse.
Re-Authorization:
Documentation indicating non-abuse with Carisoprodol is required to
be obtained for additional fills once the initial criteria have been met.
Authorization is approved for a one (1) month supply (124 tablets for
31 days) for the duration requested up to a maximum of six (6)
months.
Revision/Review Date
04/2016
Medical Director/clinical reviewer must override criteria when, in
his/her professional judgement, the requested item is medically
necessary.
PRIOR AUTHORIZATION
STIMATE (desmopressin nasal spray)
PA Criteria
Criteria Details
Covered Uses
Medically accepted indications are defined using the following sources: the Food and
Drug Administration (FDA), Micromedex, American Hospital Formulary Service
(AHFS), United States Pharmacopeia Drug Information for the Healthcare Professional
(USP DI), and the Drug Package Insert.
Exclusion
Criteria
None
Required
Medical
Information
See “other criteria”
Age Restrictions
None
Prescriber
Restrictions
None
Coverage
Duration
If criterion is met, the request will be approved for 12 months. If the criterion is not
met, the request will be referred to a Clinician for medical necessity review.
Other Criteria
AUTHORIZATION:
Diagnosis of Hemophilia A with Factor VIII coagulant activity levels greater than 5%.
OR
Diagnosis of mild to moderate classic von W illebrand’s disease (Type 1) with Factor
VIII coagulant activity levels greater than 5%.
NOTE: Clinical reviewer must override criteria when, in his/her professional
Review Date: 11/2015 judgment, the requested item is medically necessary.
129
Field Name
Prior Authorization
Group Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber
Restrictions
Coverage Duration
Other Criteria
Field Description
TOBACCO CESSATION PRODUCTS
FORMULARY STATUS Non-Formulary, Requires Prior
Authorization
• Nicotrol Inhaler
• Nicotrol NS (nasal spray)
Medically accepted indications are defined using the following sources:
the Food and Drug Administration (FDA), Micromedex, American
Hospital Formulary Service (AHFS), United States Pharmacopeia Drug
Information for the Healthcare Professional (USP DI), the Drug Package
Insert (PPI), or disease state specific standard of care guidelines.
N/A
See “other criteria”
N/A
N/A
If criterion is met, approval length for nicotine replacement products
will be for 3 consecutive months (90 days) per rolling 12- month period;
if the criteria are not met, the request will be referred to a clinical
reviewer for medical necessity review.
Initial Authorization:
Revision/Review
Date 04/2016
For approval of non-preferred products (inhaler and nasal spray),
member must have a medical reason for not using the patch, gum
or lozenges (ex. allergic reaction to patch or intolerance to
Chantix, Zyban).
In the event nicotine products, Zyban, or Chantix are deemed
necessary by the provider for 90 additional days, a PA is
required for both preferred and non-preferred products. The
provider must verify that in his or her opinion the patient would
benefit from a second attempt within the 365 day benefit period.
Medical Director/clinical reviewer must override criteria when, in
his/her professional judgement, the requested item is medically
necessary.
Field Name
Prior Authorization
Group Description
Drugs
Field Description
SEROTONIN RECEPTOR AGONISTS (TRIPTANS)
FORMULARY STATUS Formulary, Pays at Point-of-Sale (First Line)
•
•
Imitrex (sumatriptan)
Maxalt & Maxalt- MLT (rizatriptan)
FORMULARY STATUS Non-Formulary, Requires Prior
Authorization (Second Line)
Amerge (naratriptan)
Axert (almotriptan)
Frova (frovatriptan)
Relpax (eletriptan)
Sumavel Dosepro (sumatriptan)
Treximet (sumatriptan/naproxen)
Zecuity sumatriptan)
Zomig (zolmitriptan)
Zomig-ZMT(zolmitriptan)
Zembrace™ SymTouch (sumatriptan)
Any other newly marketed serotonin receptor agonists
(triptans) treatment agents.
Medically accepted indications are defined using the following sources:
the Food and Drug Administration (FDA), Micromedex, American
Hospital Formulary Service (AHFS), United States Pharmacopeia Drug
Information for the Healthcare Professional (USP DI), the Drug Package
Insert (PPI), or disease state specific standard of care guidelines.
N/A
See “other criteria”
•
•
•
•
•
•
•
•
•
•
•
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber
Restrictions
Coverage Duration
Other Criteria
N/A
N/A
Diagnosis of migraine headaches. If the above conditions are met, the
request will be approved with a 12 month duration for quantities not to
exceed 12 tablets per 30 days, 2 injections kits (4 injections) per 30
days, and 6 nasal spray units (1 box) per 30 days; if the criteria are not
met, the request will be referred to a clinical reviewer for medical
necessity review.
Initial Authorization:
1. Diagnosis of migraine headaches.
2. Diagnosis of cluster headaches (sumatriptan injection only).
3. An automatic approval for sumatriptan (generic) or rizatriptan at the
point-of-sale will occur if the quantities prescribed do not exceed 12
tablets per 30 days, 2 injection kits (4 injections) per 30 days, and 6
nasal spray units (1 box) per 30 days.
4. Documented trial and failure at therapeutic doses or intolerance to
sumatriptan or rizatriptan.
Quantities Greater Than Allowed Per 30 Days:
If the patient requires doses greater than the set limits after meeting
approval, the request will be referred to a Medical Director for medical
necessity review.
Revision/Review
Date 04/2016
Medical Director/clinical reviewer must override criteria when, in
his/her professional judgement, the requested item is medically
necessary.
Field Name
Prior Authorization
Group Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber Restrictions
Coverage Duration
Other Criteria
Field Description
Transderm-Scop®
Transderm-Scop® (scopolamine)
Medically accepted indications are defined using the following
sources: the Food and Drug Administration (FDA), Micromedex,
American Hospital Formulary Service (AHFS), United States
Pharmacopeia Drug Information for the Healthcare Professional (USP
DI), the Drug Package Insert (PPI), or disease state specific standard
of care guidelines.
N/A
See “other criteria”
N/A
N/A
If the criteria are met, the request will be approved for the treatment of
motion sickness for a one (1) month duration and for the treatment of
sialorrhea for a 12 month duration; if the criteria are not met, the
request will be referred to a clinical reviewer for medical necessity
review.
Initial Authorization:
Motion Sickness
Diagnosis of nausea and vomiting associated with motion
sickness or recovery from anesthesia.
AND
Documented trial and failure at therapeutic doses, intolerance
or contraindication to meclizine, diphenhydramine and
dimenhydrinate.
Sialorrhea
Documented trial and failure at therapeutic doses, intolerance
or contraindication to glycopyrrolate.
Revision/Review Date
07/2016
Medical Director/clinical reviewer must override criteria when, in
his/her professional judgement, the requested item is medically
necessary.
PRIOR AUTHORIZATION
ULORIC (febuxostat tablet)
PA Criteria
Criteria Details
Covered Uses
Medically accepted indications are defined using the following sources: the Food and
Drug Administration (FDA), Micromedex, American Hospital Formulary Service
(AHFS), United States Pharmacopeia Drug Information for the Healthcare Professional
(USP DI), and the Drug Package Insert.
Exclusion
Criteria
None
Required
Medical
Information
See “other criteria”
Age Restrictions
None
Prescriber
Restrictions
None
Coverage
Duration
Other Criteria
If criterion is met, the request will be approved with a 12 month duration. If criterion is
not met, the request will be referred to a Clinician for medical necessity review.
AUTHORIZATION:
Trial and failure of maximized doses of allopurinol. Up to 800mg of allopurinol per day
should have been attempted prior to treatment with febuxostat (depending on renal status).
Review Date: 11/2015 NOTE: Clinical reviewer must override criteria when, in his/her professional
judgment, the requested item is medically necessary.
132
Field Name
Prior Authorization
Group Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber Restrictions
Coverage Duration
Other Criteria
Field Description
Vicoprofen®
Vicoprofen® (hydrocodone/ibuprofen) tablets
Medically accepted indications are defined using the following
sources: the Food and Drug Administration (FDA), Micromedex,
American Hospital Formulary Service (AHFS), United States
Pharmacopeia Drug Information for the Healthcare Professional (USP
DI), the Drug Package Insert (PPI), or disease state specific standard
of care guidelines.
N/A
See “other criteria”
N/A
N/A
If the criteria are met, the request will be approved with up to a 3
month duration; if the criteria are not met, the request will be referred
to a clinical reviewer for medical necessity review.
Initial Authorization:
Diagnosis of acute pain.
AND
Documented trial and failure or intolerance to at least three of the
following medications: oxycodone/acetaminophen,
hydrocodone/acetaminophen, acetaminophen/codeine, morphine,
and hydromorphone.
Revision/Review Date
04/2016
Medical Director/clinical reviewer must override criteria when, in
his/her professional judgement, the requested item is medically
necessary.
Field Name
Prior Authorization
Group Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber
Restrictions
Coverage Duration
Other Criteria
Field Description
WEIGHT LOSS MEDICATIONS
Adipex-P (phentermine)
Alli (orlistat)
Bontril PDL (phendimetrazine) tablets
Bontril Slow-Release (phendimetrazine) capsules
Desoxyn (methamphetamine)
Didrex (benzphetamine)
Ionamin (phentermine) capsules
Qsymia (phentermine/topiramate)
Saxenda (liraglutide) injectable pen
Suprenza ODT (phentermine)
Xenical (orlistat)
or any newly marketed weight loss medication
Medically accepted indications are defined using the following sources:
the Food and Drug Administration (FDA), Micromedex, American
Hospital Formulary Service (AHFS), United States Pharmacopeia Drug
Information for the Healthcare Professional (USP DI), the Drug Package
Insert (PPI), or disease state specific standard of care guidelines.
N/A
See “other criteria”
Patient must be at least 18 years old
N/A
If the criteria are met, the request will be approved for a one (1) month
duration; if the criteria are not met, the request will be referred to a
clinical reviewer for medical necessity review.
Initial Authorization:
Obesity in the Absence of Other Risk Factors
Patient must have an initial body mass index (BMI) of 30 kg/m2
or greater.
Prescribing physician must submit documentation of patient’s
starting weight.
Patient must have received nutritional counseling regarding
adherence to dietary guidelines.
Obesity in the Presence of Other Risk Factors:
Patient must have an initial body mass index (BMI) of 27 kg/m2
or greater.
Patient must have a diagnosis of obesity in the presence of other
risk factors (e.g. hypertension, diabetes, dyslipidemia).
Prescribing physician must submit documentation of patient’s
starting weight.
Patient must have received nutritional counseling regarding
adherence to dietary guidelines.
NOTE: If a request for Xenical is approved, refer patient to use Alli at
the equivalent dosing.
NOTE: Requests for Desoxyn and Saxenda also must first have
documented trial and failure at least two other weight loss medications.
Re-Authorization:
Prescribing physician must submit documentation of patient’s
starting weight and current weight.
Demonstrated weight loss on medication, as shown through
documentation of patient’s starting weight (from previous
month) and current weight.
Revision/Review
Date 07/2016
Medical Director/clinical reviewer must override criteria when, in
his/her professional judgement, the requested item is medically
necessary.
Field Name
Prior Authorization
Group Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber Restrictions
Coverage Duration
Other Criteria
Field Description
Xifaxan®
Xifaxan® (rifaximin)
Medically accepted indications are defined using the following
sources: the Food and Drug Administration (FDA), Micromedex,
American Hospital Formulary Service (AHFS), United States
Pharmacopeia Drug Information for the Healthcare Professional (USP
DI), the Drug Package Insert (PPI), or disease state specific standard
of care guidelines.
N/A
See “other criteria”
≥ 18 years of age
N/A
If the criteria are met, for initial authorization, the request will be
approved with a 6 month duration. For re – authorization, the request
will be approved with a 12 month duration; if the criteria are not met,
the request will be referred to a clinical reviewer for medical
necessity review.
Initial Authorization:
Approval as a concurrent first line medication with Lactulose
for the diagnosis of hepatic encephalopathy.
Re-Authorization:
Revision/Review Date
04/2016
Documentation indicating the member has clinically benefited
from therapy.
Medical Director/clinical reviewer must override criteria when, in
his/her professional judgement, the requested item is medically
necessary.
Field Name
Prior Authorization
Group Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber Restrictions
Coverage Duration
Other Criteria
Field Description
Zovirax topical
Zovirax® (acyclovir) 5% cream/ointment
Medically accepted indications are defined using the following
sources: the Food and Drug Administration (FDA), Micromedex,
American Hospital Formulary Service (AHFS), United States
Pharmacopeia Drug Information for the Healthcare Professional (USP
DI), the Drug Package Insert (PPI), or disease state specific standard
of care guidelines.
N/A
See “other criteria”
N/A
N/A
If the criteria are met, the request will be approved with up to a 12
month duration; if the criteria are not met, the request will be referred
to a clinical reviewer for medical necessity review.
Initial Authorization
Zovirax Cream:
Diagnosis of herpes labialis (cold sores).
Documented trial and failure or intolerance to a preferred oral
antiviral, such as acyclovir.
Zovirax Ointment:
Diagnosis of venereal herpes.
Documented trial and failure or intolerance to a preferred oral
antiviral, such as acyclovir.
Revision/Review Date
04/2016
Medical Director/clinical reviewer must override criteria when, in
his/her professional judgement, the requested item is medically
necessary.
Field Name
Prior Authorization
Group Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber Restrictions
Coverage Duration
Other Criteria
Revision/Review Date
04/2016
Field Description
Zyvox
Zyvox® (linezolid)
Medically accepted indications are defined using the following
sources: the Food and Drug Administration (FDA), Micromedex,
American Hospital Formulary Service (AHFS), United States
Pharmacopeia Drug Information for the Healthcare Professional (USP
DI), the Drug Package Insert (PPI), or disease state specific standard
of care guidelines.
N/A
See “other criteria”
N/A
N/A
If the criteria are met, the request will be approved with up to a 1
month duration; if the criteria are not met, the request will be referred
to a clinical reviewer for medical necessity review.
Initial Authorization
Diagnosis of vancomycin-resistant enterococcus faecium infection,
nosocomial pneumonia, complicated skin and skin structure
infection (including diabetic foot infections, without concomitant
osteomyelitis), uncomplicated skin and skin structure infection,
methicillin-resistant Staphylococcus aureus infection, or
community-acquired pneumonia.
And patient meets one of the two following criteria:
Documented history of treatment with Zyvox IV (continuation of
therapy, IV to PO conversion).
Documentation that the infection is susceptible to Zyvox AND the
patient has failed treatment or is contraindicated to treatment with
antibiotics to which the organism is susceptible.
Medical Director/clinical reviewer must override criteria when, in
his/her professional judgement, the requested item is medically
necessary.
PRIOR AUTHORIZATION CRITERIA
ZOFRAN (ondansetron tablets)
PA Criteria
Criteria Details
Covered Uses
Medically accepted indications are defined using the following sources: the Food and
Drug Administration (FDA), Micromedex, American Hospital Formulary Service
(AHFS), United States Pharmacopeia Drug Information for the Healthcare Professional
(USP DI), and the Drug Package Insert.
Exclusion
Criteria
None
Required
Medical
Information
See “other criteria”
Age Restrictions
Prescriber
Restrictions
Coverage
Duration
Other Criteria
None
None
None
For Chemotherapy or Radiation Therapy if criterion is met, the request will be approved
with a quantity limit of 90 tablets/30days (4mg & 8mg) or 50mL/30 days for the duration
of the chemotherapy or radiation, not to exceed 3 months. For Hyperemesis Gravidarum,
if the criterion is met, the request will be approved for the remaining duration of the
pregnancy or the duration requested (whichever is less). If the criterion is not met, the
request will be referred to a Clinician for medical necessity review. If the request is for a
quantity greater than the limits stated above, the request will be referred to a Clinician for
medical necessity review.
AUTHORIZATION:
Chemotherapy or Radiation Therapy:
Current treatment with emetogenic chemotherapy or radiation therapy.
NOTE: An automatic approval at the point-of-sale will occur if the quantities prescribed
do not exceed 90 tablets/30 days (4mg & 8mg) or 50mL/30 days (4mg/5mL).
NOTE: Zofran 24mg tablets are non-preferred. Requests for the 24mg tablets should be
referred to using the 8mg tablets.
Hyperemesis Gravidarum:
• Diagnosis of hyperemesis gravidarum.
• Dosage does not exceed 4-8mg every 6 hours.
NOTE: An automatic approval at the point-of-sale will occur if the quantities prescribed
do not exceed 15 tablets/30 days (4mg & 8mg) or 50mL/30 days (4mg/5mL).
NOTE: Zofran 24mg tablets are non-preferred. Requests for the 24mg tablets should be
referred to using the 8mg tablets.
Review Date: 11/2015 NOTE: Clinical reviewer must override criteria when, in his/her professional
judgment, the requested item is medically necessary.
140
PRIOR AU THORIZATION CRITERI A
ACTH AR H.P. (corticotrophin) Vials: 80u/ml available in 5 ml vials
PA CRITERI A FOR APPROVAL FOR INFANTILE SPASMS ( WEST SYNDROME):
Patient is < 2 years of age
The medication is being prescribed by a neurologist.
Documented trial and failure of Sabril or documented medical reason for why
the patient cannot use Sabril (vigabartin).
Documentation of the patient’s current weight (in kg) and height/length (in cm)
or body surface area (BSA)
If all of the above conditions are met, the request will be approved for one vial for up to a 1
month duration; if all of the above criteria are not met then, the request is referred to the
Clinical reviewer for medical necessity review.
PA CRITERIA FOR APPROVAL FOR MULTIPLE SCLEROSIS:
Documentation was submitted that patient is having acute attack, with neurologic
symptoms and increased disability or impairments in vision, strength or cerebellar
function, and has failed therapy with IV methylprednisolone, or a medical reason has
been submitted why patient is unable to use IV methylprednisolone.
The medication is being prescribed by a neurologist
If all of the above conditions are met, the request will be approved for up to a 1 month duration;
if all of the criteria are not met, the request will be sent to the clinical reviewer for medical
necessity review.
PA CRITERI A FOR ALL OTHER FD A APPROVED CONDITIONS AND
INDICATIONS:
Documented trial and failure of IV methylprednisolone AND oral
prednisone, or documented medical reason for why the patient cannot use
these therapies for treatment
AND
Documentation was provided that ALL other standard therapies have been used to treat the
member’s condition as described in the medical compendium (Micromedex, AHFS, Drug
Points, and package insert) as defined in the Social Security Act and/or per recognized
standard of care guidelines OR there is a documented medical reason (i.e. medical
intolerance, treatment failure, etc.) for why all other standard therapies could not
be used to treat the member’s condition.
AND
Prescriber is a specialist in the condition they are treating.
If all of the above conditions are met, the request will be approved for up to a 1 month
duration, according to standard dosing based on indication. If all of the above criteria
are not met then, the request will be sent to the clinical reviewer for medical necessity
review
Revision/Review Date: 4/2016
NOTE: Clinical review er must override criteria w hen, in his/her professional
judgment, the requested item is medically necessary.
1
141
Prior Authorization Group: Erythropoiesis-Stimulating Agents
Drug(s): Darbepoetin Alfa-Polysorbate 80 (Aranesp®), Epoetin Alfa (Procrit®)
***ARANESP® is preferred agent for Chronic Kidney Disease and for patients receiving chemotherapy
that are 18 years of age or older.*****
Covered Uses: Medically accepted indications are defined using the following sources: the Food and
Drug Administration (FDA), Micromedex, American Hospital Formulary Service (AHFS), United States
Pharmacopeia Drug Information for the Healthcare Professional (USP DI), the Drug Package Insert (PPI).
Criteria:
All lab results must be submitted within 30 days of the request
Hematocrit, Serum ferritin level (normal is greater than 100ng/ml), Transferrin saturation
(TSAT) (normal is greater than 20%), Serum iron, Total Iron Binding Capacity
(TIBC),Vitamin B12 level, Folate level, Glomerular Filtration Rate (GFR) (for chronic
kidney disease anemia), and Erythopoietin level (for HIV related anemia)
****Procrit requires documentation (consistent with pharmacy claims data, OR for new
members to the health plan consistent with medical chart history) of adequate trials and/or has
a documented medical reason (e.g. intolerance or hypersensitivity) for not utilizing ARANESP
when appropriate****
1. Initial approval for anemia of Pre-dialysis chronic kidney disease or anemia due to
chemotherapy:
Hemoglobin less than 10g/dl OR if the member is new to the health plan and was receiving
therapy at the previous health plan the member has a documented (submitted lab result dated
within 30 days of request) hemoglobin <12 g/dL.
If the member has anemia due to Pre-dialysis chronic kidney disease then documentation
must be submitted that the member has a glomerular filtration rate (GFR) less than 60
ml/min/1.73m2 for > 3 months OR meets the criteria for chronic kidney disease as defined
by the National Kidney Foundation.
If the member has low B12 levels and/or Folate levels then documentation submitted that
indicates the member is or will be prescribed appropriate supplementation.
If the member is iron deficient, the member is in the process of receiving either oral or IV
iron supplementation or the treatment plan is to start iron therapy.
The medication is being recommended and/or prescribed at an FDA appropriate dose for
indication.
If the request is for Procrit®, the provider submitted a documented medical reason (i.e.
intolerance) why it is medically necessary to utilize Procrit® (instead of Aranesp®) for the
treatment of CKD anemia and for patients with chemotherapy-induced anemia that are 18
years of age or older.
If all of the above conditions are met, the request will be approved for up to a 3-month duration if the
member is not functionally iron deficient (ferritin concentration is > 100-800 ng/mL and the
transferrin saturation are > 20-55%) and not vitamin B-12 deficient and not folate deficient, OR a
temporary supply of up to 1 month may be authorized if the member is functionally iron deficient
(ferritin concentration < 100 ng/mL and/or percentage transferrin saturation < 20%) and/or vitamin B12 deficient and/or folate deficient; if all of the above criteria are not met, the request is referred to a
Medical Director/Clinical reviewer for medical necessity review.
Reauthorization:
If the member has been receiving therapy and their hemoglobin is less than 12 g/dL and
one of the following apply (if applicable):
143
a) The ordered dose is reduced by 25% of previous dose if the rate of Hgb increase was
greater than 1g/dL over a two week period OR the Hgb is increasing and
approaching 12 g/dL.
b) The ordered dose is increased from the previous dose if the patients Hgb improved
less than 1g/dL over a 4 to 6 week period and iron stores were adequate.
c) An increase in dose does not occur more than once per month (by 25%)
If the member is iron deficient, the member is in the process of receiving either oral or
IV iron supplementation or the treatment plan is to start iron therapy.
If the member was deficient in either B12 or folate and is NOT receiving
supplementation, repeat B12 and Folate labs are required (within 30 days of request).
The medication is being recommended and/or prescribed at an FDA appropriate dose for
indication.
If the request is for Procrit®, the provider submitted a documented medical reason (i.e.
intolerance) why it is medically necessary to utilize Procrit® (instead of Aranesp®) for
the treatment of CKD anemia and for patients with chemotherapy-induced anemia that
are 18 years of age or older.
If all of the above conditions are met, the request will be approved for up to a 3-month duration if the
member is not functionally iron deficient (ferritin concentration is > 100-800 ng/mL and the
transferrin saturation are > 20-55%) and not vitamin B-12 deficient and not folate deficient, OR a
temporary supply of up to 1 month may be authorized if the member is functionally iron deficient
(ferritin concentration < 100 ng/mL and/or percentage transferrin saturation < 20%) and/or vitamin B12 deficient and/or folate deficient; if all of the above criteria are not met, the request is referred to a
Medical Director/Clinical reviewer for medical necessity review.
2. Initial approval for anemia due to Zidovudine-treated HIV infected patients:
Hemoglobin less than 11g/dl OR if the member is new to the health plan and was receiving
therapy at the previous health plan the member has a documented (submitted lab result dated
within 30 days of request) hemoglobin <12 g/dL.
Patient has been receiving a highly reactive antiretroviral therapy (HAART) regimen for the
past 35 days.
Documentation, within 30 days of the request, that the patient has an erythropoietin level <
500 units/mL.
If the member has low B12 levels and/or Folate levels then documentation submitted that
indicates the member is or will be prescribed appropriate supplementation.
If the member is iron deficient, the member is in the process of receiving either oral or IV
iron supplementation or the treatment plan is to start iron therapy.
The medication is being recommended and/or prescribed at an FDA appropriate dose for
indication.
If all of the above conditions are met, the request will be approved for up to a 3-month duration if the
member is not functionally iron deficient (ferritin concentration is > 100-800 ng/mL and the
transferrin saturation are > 20-55%) and not vitamin B-12 deficient and not folate deficient, OR a
temporary supply of up to 1 month may be authorized if the member is functionally iron deficient
(ferritin concentration < 100 ng/mL and/or percentage transferrin saturation < 20%) and/or vitamin B12 deficient and/or folate deficient; if all of the above criteria are not met, the request is referred to a
Medical Director/Clinical reviewer for medical necessity review.
Reauthorization:
If the member has been receiving therapy and their hemoglobin is less than 12 g/dL and
one of the following apply (if applicable):
a) The ordered dose is reduced by 25% of previous dose if the rate of Hgb increase was
greater than 1g/dL over a two week period OR the Hgb is increasing and
approaching 12 g/dL.
b) The ordered dose is increased from the previous dose if the patients Hgb improved
144
less than 1g/dL over a 4 to 6 week period and iron stores were adequate.
c) An increase in dose does not occur more than once per month
If the member is iron deficient, the member is in the process of receiving either oral or
IV iron supplementation or the treatment plan is to start iron therapy.
If the member was deficient in either B12 or folate and is NOT receiving
supplementation, repeat B12 and Folate labs are required (within 30 days of request).
The medication is being recommended and/or prescribed at an FDA appropriate dose for
indication.
If all of the above conditions are met, the request will be approved for up to a 3-month duration if the
member is not functionally iron deficient (ferritin concentration is > 100-800 ng/mL and the
transferrin saturation are > 20-55%) and not vitamin B-12 deficient and not folate deficient, OR a
temporary supply of up to 1 month may be authorized if the member is functionally iron deficient
(ferritin concentration < 100 ng/mL and/or percentage transferrin saturation < 20%) and/or vitamin B12 deficient and/or folate deficient; if all of the above criteria are not met, the request is referred to a
Medical Director/Clinical reviewer for medical necessity review.
3. Initial approval for anemia due to Ribavirin Induced Anemia:
Hemoglobin less than 10g/dl OR if the member is new to the health plan and was receiving
therapy at the previous health plan the member has a documented (submitted lab result dated
within 30 days of request) hemoglobin <12 g/dL.
Patient is currently receiving ribavirin therapy and initiated therapy ≤ 20 weeks ago.
If the member has low B12 levels and/or Folate levels then documentation submitted that
indicates the member is or will be prescribed appropriate supplementation.
If the member is iron deficient, the member is in the process of receiving either oral or IV
iron supplementation or the treatment plan is to start iron therapy.
The medication is being recommended and/or prescribed at an FDA appropriate dose for
indication.
If all of the above conditions are met, the request will be approved for up to a 3-month duration if the
member is not functionally iron deficient (ferritin concentration is > 100-800 ng/mL and the
transferrin saturation are > 20-55%) and not vitamin B-12 deficient and not folate deficient, OR a
temporary supply of up to 1 month may be authorized if the member is functionally iron deficient
(ferritin concentration < 100 ng/mL and/or percentage transferrin saturation < 20%) and/or vitamin B12 deficient and/or folate deficient; if all of the above criteria are not met, the request is referred to a
Medical Director/Clinical reviewer for medical necessity review.
Reauthorization:
If the member has been receiving therapy and their hemoglobin is less than 12 g/dL and
one of the following apply (if applicable):
a) The ordered dose is reduced by 25% of previous dose if the rate of Hgb increase was
greater than 1g/dL over a two week period OR the Hgb is increasing and
approaching 12 g/dL.
b) The ordered dose is increased from the previous dose if the patients Hgb improved
less than 1g/dL over a 4 to 6 week period and iron stores were adequate.
c) An increase in dose does not occur more than once per month.
If the member is iron deficient, the member is in the process of receiving either oral or
IV iron supplementation or the treatment plan is to start iron therapy.
If the member was deficient in either B12 or folate and is NOT receiving
supplementation, repeat B12 and Folate labs are required (within 30 days of request).
The member is currently receiving ribavirin therapy that was initiated ≤ 20 weeks ago,
or if beyond week 20 of ribavirin therapy, documentation submitted indicates a dosage
reduction of ribavirin to 600 mg/day after week 20 but the member still became anemic.
The medication is being recommended and/or prescribed at an FDA appropriate dose for
145
indication.
If all of the above conditions are met, the request will be approved for up to a 3-month duration if the
member is not functionally iron deficient (ferritin concentration is > 100-800 ng/mL and the
transferrin saturation are > 20-55%) and not vitamin B-12 deficient and not folate deficient, OR a
temporary supply of up to 1 month may be authorized if the member is functionally iron deficient
(ferritin concentration < 100 ng/mL and/or percentage transferrin saturation < 20%) and/or vitamin B12 deficient and/or folate deficient; if all of the above criteria are not met, the request is referred to a
Medical Director/Clinical reviewer for medical necessity review.
4. Initial approval for Allogenic Blood Transfusion Surgery Patients:
Hemoglobin less than 13g/dl and greater than 10g/dl.
The patient has normal iron stores and is, or will be, receiving adequate iron
supplementation.
The patient is scheduled for an elective, non-cardiac, nonvascular surgery.
The medication is being recommended and/or prescribed at an FDA appropriate dose for
indication.
If all of the above conditions are met, the request will be approved with a 1-month duration; if all of
the above criteria are not met, the request is referred to a Medical Director/Clinical reviewer for
medical necessity review.
5. Initial approval for anemia due to Other Medically Acceptable Indications:
Hemoglobin less than 11g/dl OR if the member is new to the health plan and was receiving
therapy at the previous health plan the member has a documented (submitted lab result dated
within 30 days of request) hemoglobin <12 g/dL.
If the member has low B12 levels and/or Folate levels then documentation submitted that
indicates the member is or will be prescribed appropriate supplementation.
If the member is iron deficient, the member is in the process of receiving either oral or IV
iron supplementation or the treatment plan is to start iron therapy.
The medication is being recommended and/or prescribed at an FDA appropriate dose for
indication.
If all of the above conditions are met, the request will be approved for up to a 3-month duration if the
member is not functionally iron deficient (ferritin concentration is > 100-800 ng/mL and the
transferrin saturation are > 20-55%) and not vitamin B-12 deficient and not folate deficient, OR a
temporary supply of up to 1 month may be authorized if the member is functionally iron deficient
(ferritin concentration < 100 ng/mL and/or percentage transferrin saturation < 20%) and/or vitamin B12 deficient and/or folate deficient; if all of the above criteria are not met, the request is referred to a
Medical Director/Clinical reviewer for medical necessity review.
Reauthorization:
If the member has been receiving therapy and their hemoglobin is less than 12 g/dL and
one of the following apply (if applicable):
a) The ordered dose is reduced by 25% of previous dose if the rate of Hgb increase was
greater than 1g/dL over a two week period OR the Hgb is increasing and
approaching 12 g/dL.
b) The ordered dose is increased from the previous dose if the patients Hgb improved
less than 1g/dL over a 4 to 6 week period and iron stores were adequate.
c) An increase in dose does not occur more than once per month.
If the member is iron deficient, the member is in the process of receiving either oral or
IV iron supplementation or the treatment plan is to start iron therapy.
If the member was deficient in either B12 or folate and is NOT receiving
146
supplementation, repeat B12 and Folate labs are required (within 30 days of request).
The medication is being recommended and/or prescribed at an FDA appropriate dose for
indication.
If all of the above conditions are met, the request will be approved for up to a 3-month duration if the
member is not functionally iron deficient (ferritin concentration is > 100-800 ng/mL and the
transferrin saturation are > 20-55%) and not vitamin B-12 deficient and not folate deficient, OR a
temporary supply of up to 1 month may be authorized if the member is functionally iron deficient
(ferritin concentration < 100 ng/mL and/or percentage transferrin saturation < 20%) and/or vitamin B12 deficient and/or folate deficient; if all of the above criteria are not met, the request is referred to a
Medical Director/Clinical reviewer for medical necessity review.
Review Date: 4/2016
.
147
PRIOR AUTHORIZATION CRITERIA
EPOGEN® (epoetin alfa): 2,000 units/ml, 3,000 units/ml, 4,000 units/ml, 10,000 units/ml, 20,000
units/ml, 40,000 units/ml
PA Criteria for Approval Administration of Epogen in ESRD Patients Treated at Dialysis Centers.
• Patient is being treated at a dialysis center.
AND
• The necessary lab work (listed below) is documented on the PA form or submitted with request;
-Hemoglobin – last 3 months results (to determine rolling Hgb)
-Hematocrit – last 3 months results (to determine rolling Hct)
-Serum ferritin – within past 2 months
-Transferrin saturation – within past 2 months
-Serum iron – within past 2 months.
-Total Iron Binding Capacity (TIBC) – within past 2 months
-Vitamin B12 and Folate levels – within past 2 months
-History of Epogen usage
If all of the above criteria are not met then the request is referred to a Medical Director/clinical reviewer
for medical necessity review. If all of the above conditions are met, place the patient into one of the
following categories based on diagnosis:
Place the patient into one of the following categories:
-Epogen treatment naïve with normal iron status (Section A)
-Epogen treatment naïve with iron deficiency (Section B)
-Receiving Epogen treatment with normal iron status (Section C)
-Receiving Epogen treatment with iron deficiency (Section D)
Section A: Epogen treatment naïve with normal iron status (TSAT > 20% and Ferritin > 100ng/ml)
• The patient has a hemoglobin <10g/dL and/or hematocrit <33%.
• Epogen dosing is being initiated at 100 units/kg 3 times a week (TIW) or less.
If all of the above conditions are met, the request will be approved with a 3-month duration, if all of
the above criteria are not met, the request is referred to a Medical Director/clinical reviewer for
medical necessity review.
Section B: Epogen treatment naïve with iron deficiency (TSAT < 20% and Ferritin < 100ng/ml)
• The patient has a hemoglobin <10g/dL and/or hematocrit <33%.
• The patient is in the process of receiving iron supplementation (i.e. 25-125 mg IV once weekly or
>200 mg elemental iron orally daily).
• The patient’s Epogen dose is less than or equal to 100 units/kg- 3 times a week (TIW).
If all of the above conditions are met, the request will be approved with a 2-month duration to allow
follow up on outcome of iron supplementation; if all of the above criteria are not met, 50,000 units of
Epogen per month will be authorized and the request is referred to a Medical Director/clinical
148
reviewer for medical necessity review.
Section C: Existing therapy with Epogen with normal iron status (TSAT > 20% and Ferritin >
100ng/ml)
• The patient has a hemoglobin <12g/dL and/or hematocrit <36%
• The patient’s hematocrit increased greater than 8 percentage points in the past month, or Hgb
increased by more than 1g/dl in a two week period, after starting current dose and the Epogen
dose has been reduced by at least 25% compared to the last course of therapy and therapy
withheld for 1-2 weeks.
• If the patient’s Hgb/Hct is below target range after receiving therapy for at least 4 weeks and the
dose is the same as last month or was increased by no more than 25% of the previous dose.
• If the patient’s current Epogen dose was started less than 8 week ago and their hematocrit has
increased by less than 4 percentage points over the past 2 weeks or less than 8 percentage points
over the last 4 weeks and the ordered dose o Epogen is the same as last month or less.
• If the patient’s hemoglobin is in target range (10-12g/dL) and the ordered dose is either reduced
or the same dose as the previous month.
• The ordered dose is not an increase in dosage that is within 4 weeks of last dosage change or
start of therapy with a medical reason being provided for an early increase.
• If the patient’s hemoglobin exceeds 12 g/dl despite dose reduction, the Epogen dose was
withheld until hemoglobin dropped to 12g/dL or less and the ordered Epogen dose was
reduced by 25%.
• If the dose is greater than 300 units/kg TIW, then documentation (within the past 2 months) of
iron maximum supplementation, documentation of patients TSAT >20% and ferritin >100ng/ml
and documentation (within the past 2 months) was submitted from a hematologist recommending
the current dose if all reversible causes for Epogen resistance have been ruled out.
If all of the above conditions are met, the request will be approved with a 3-month duration, if all of
the above criteria are not met then the request is referred to a Medical Director/clinical reviewer for
medical necessity review.
Section D: Existing therapy on Epogen with iron deficiency (TSAT < 20% and Ferritin <
100ng/ml)
• The patient has a hemoglobin <12g/dL and/or hematocrit <36%
• The patient is currently in the process of receiving iron supplementation (i.e. 25-125 mg IV
once weekly or >200 mg elemental iron orally daily).
• The ordered dose is an increase in dosage that is within one-month time of last dosage change
or start of therapy, and a medical reason was provided for an early increase.
• The Epogen dose is less than or equal to 100 units/kg TIW.
If all of the above conditions are met, the request will be approved with a 2-month duration to allow
follow up on outcome of iron supplementation; if all of the above criteria are not met then the
request is referred to a Medical Director/clinical reviewer for medical necessity review.
149
DOSAGE AND ADMINISTRATION:
CKD patients:
General Therapeutic Guidelines in CKD Patients for Epoetin Alfa
Starting dose
(initiate Epogen treatment when the hemoglobin level is
less than 10g/dL)
Adults: 50 to 100 Units/kg TIW
Pediatric: 50 Units/kg TIW
Maximum dose – (with normal Iron stores)
Intravenous administration
300 units/kg TIW†
**Doses greater than maximum doses require hematologist
consultation and recommendation.
Reduce dose by 25% when
Dose should be temporarily withheld when
Increase dose up to 25% of previous dose if:
Maintenance dose
Suggested target hemoglobin
•
†max dose for the treatment of anemia cause by zidovudine
in HIV-infected patients. There are no well-established
maximum doses for the other approved indications.
2) Hgb increases by more than 1 g/dl in 2-week period
Hgb exceeds 12 g/dl and until Hgb falls to 11g/dl. Therapy
should be reinitiated at a dose approximately 25% below
1)
Hgb remains
the previous
dose.< 10 g/dl
AND
2) Hgb increases by less than 1 g/dl after 4 weeks of
therapy
Individualize to achieve and maintain the lowest Hgb level
sufficient to avoid the need for RBC transfusion and not to
exceed 12 g/dl.
10 to 12 gm/dl
Dose adjustment should not be made more frequently than once a month, unless clinically
indicated.
Revision/Review Date: 4/2016
NOTE: Physician/clinical reviewer must override criteria when, in his/her professional judgement, the
requested item is medically necessary.
150
PRIOR AUTHORIZATION CRITERIA
AUBAGIO® (teriflunomide) tablets: 7mg, 14mg
®
GILENYA (fingolimod hcl) capsules: 0.5mg
TECFIDERA® (dimethyl fumarate) capsules: 120mg, 240mg
PA CRITERIA FOR INITIAL APPROVAL:
•
The member is an adult (≥ 18 y/o) member with relapsing/remitting MS (RRMS) or secondary progressive MS (SPMS) with
a relapsing element.
•
If the medication request is for Aubagio and/or any other newly marketed oral MS Agent, the member has a documented
treatment failure to Gilenya OR Tecfidera (see Box 1 in Glossary for definition of treatment failure) which is consistent with
pharmacy claims data, OR for new members to the health plan consistent with medical chart history, indicating they had
received an adequate trial (including dates, doses of 6 months or more of therapy) or has another documented clinically
significant medical reason (intolerance, hypersensitivity, contraindication, etc.) for not taking Gilenya OR Tecfidera for a
minimum of 6 months to treat their medical condition.
•
The medication is being recommended and/or prescribed by a neurologist at an FDA approved dosage.
If all of the above conditions are met, the request will be approved for up to a 6-month duration; if all of the above criteria are not
met, the request is referred to a clinical reviewer for medical necessity review
REAUTHORIZATION CRITERIA:
•
Documentation sent indicates that the member is an adult (≥ 18 y/o) and has one of the following types of MS: RRMS or
SPMS with a relapsing element.
•
Documentation indicating the member has clinically benefited from therapy.
•
The medication was prescribed at an FDA approved dosage.
•
Medication was recommended by a neurologist and/or prescribed by a neurologist.
If all of the above conditions are met, the request will be approved for up to a 12-month duration; if all of the above criteria are
not met, the request is referred to a clinical reviewer for medical necessity review
FDA INDICATIONS:
Aubagio is indicated for the treatment of patients with relapsing forms of multiple sclerosis.
Gilenya is indicated for the treatment of patients with relapsing forms of multiple sclerosis (MS) to reduce the frequency of
clinical exacerbations and to delay the accumulation of physical disability.
Tecfidera is indicated for the treatment of patients with relapsing forms of multiple sclerosis.
DOSAGE AND ADMINISTRATION:
Aubagio: The recommended dose is 7mg or 14mg orally once daily.
Gilenya: The recommended dose is 0.5 mg orally once daily. Doses of higher than 0.5 mg are associated with a greater
incidence of adverse reactions without additional benefits.
Tecfidera: The recommended starting dose 120mg orally twice daily for 7 days. Maintenance dose after 7 days is 240mg orally
twice daily.
BOX 1: TREATMENT FAILURE:
A member may be considered to have failed treatment if any of the following are documented:
1.
Member who has an attack rate (relapse) of more than 1 per year, fails to show a reduction in relapse rate, or
continues to experience attacks (relapses) at a rate similar to that found before starting therapy**
2.
Member who has incomplete recovery (cumulative residual abnormalities sustained for 6 months) from
repeated attacks, particularly as the EDSS score increases. **
3.
Member experiences an annual increase in the EDSS (Expanded Disability Status Scale) of 1 point from a
previous score of 3 to 5.5, or 0.5 point increase from a previous score of 6.0 or greater in the absence of clinical
attacks or other documentation of clinically significant disability progression. **
4.
Member who develops new or recurrent brainstem or spinal cord lesions as seen on MRI. **
5.
Members experiencing relapses affecting multiple neurologic symptoms, and those accumulating residual
impairments in multiple neurologic systems. **
151
6.
Members who have progressive motor, cognitive or sensory impairment sufficient to disrupt their daily activities
irrespective of changes on neurologic examination, provided the influence of depression, medications or superimposed
concurrent disease is ruled out. Examples include: loss of endurance in sustaining activity, forced alterations in activities of
daily living, muddled thinking, impaired concentration and mental processing and fatigue. **
7.
Members who have new or enlarging T2 lesions, increase in brain atrophy on MRI, or new T1 Gd enhancing
lesions on MRI accompanied by changes in the ability to perform daily activities.**
** These are members who have a documented treatment failure after receiving a minimum of 6 months each of a self
injectable agent. Diagnostic and/or clinical documentation of treatment failure will be required for the last therapy the
member received. This requires that the member has failed a minimum of 6 months of a self-injectable agent or has a
documented medical reason (i.e. intolerance) for not utilizing each of these therapies for a minimum of 6 months.
Kurtzke Expanded Disability Status Scale (EDSS)
Rating Status
0
1.0
1.5
2.0
2.5
3.0
3.5
Normal Neurological Exam
No Disability, minimal symptoms
No disability, minimal signs in more than one area
Slightly more disability in one area
Slightly greater disability in two areas
Moderate disability in one area but still walking independently
Walking independently but with moderate disability in one area and more than minimal disability in several
others
4.0
Walking without aid, self-sufficient, up and about some12 hours a day despite relatively severe disability; able
to walk without aid or rest some 500 meters
4.5
Walking without aid, up and about much of the day, able to work a full day, may have some limitation of full
activity or require some help, relatively severe disability but able to walk without aid or rest some 300 meters.
5.0
Walking without aid or rest for about 200 meters, disability severe enough to impair full daily activities, can
work a full day without special provisions
5.5
Ambulatory without aid or rest for about 100 meters; disability severe enough to prevent full daily activities
6.0
Intermittent or unilateral constant assistance (cane, crutch, brace) required to walk about 100 meters with or
without resting
6.5
Needs canes, crutches, braces to walk for 20 meters without resting
7.0
Unable to walk beyond five meters even with aid; mostly confined to a wheelchair; wheels self in standard
wheelchair and transfers alone; up and about in wheelchair some 12 hours a day
7.5
Unable to take more than a few steps; restricted to wheelchair; may need aid in transfer; wheels self but
cannot carry on in standard wheelchair a full day; may require motorized wheelchair
8.0
Essentially restricted to bed, chair, or wheelchair, but may be out of bed itself much of the day; retains many
self-care functions; generally has effective use of arms
8.5
Essentially restricted to bed much of day; has some effective use of arms; retains some self-care functions
9.0
Helpless bed patient; can communicate and eat
9.5
Totally helpless bed patient; unable to communicate effectively or eat/swallow
10.0
Death due to MS
Kurtzke JF. Rating neurologic impairment in multiple sclerosis: an expanded disability status scale (EDSS).
Neurology.1983;33:1444-1452.
REFERENCES:
1.
National Multiple Sclerosis Society. Expert Opinion Paper. Medical advisory board of the National MS Society. Treatment
recommendations for physicians. Changing therapy in relapsing multiple sclerosis: Considerations and recommendations of a
task force of the National MS Society.2004. Available at www.nationalmssociety.org/PRC.asp
2.
National Multiple Sclerosis Society. Expert Opinion Paper. Medical advisory board of the National MS Society. Treatment
recommendations for physicians. Disease management consensus statement.2005. Available at
www.nationalmssociety.org/PRC.asp
3.
Cohen BA. Khan O. Jeffery DR. et al. Identifying and treating patients with suboptimal responses. Neurology.2004;
63(Suppl 6):S33-S40.
4.
Cohen JA, Barkhof F, Comi Giancarlo C. et al. Oral Fingolimod or Intramuscular Interferon for Relapsing Multiple Sclerosis.
The New England Journal of Medicine.2010; 362: 402-15.
5.
Kapps L, Antel J, Comi G. Et al. Oral Fingolimod (FTY720) for relapsing Multiple Sclerosis. The New England Journal of
Medicine.2006; 355:1124-40.
6.
Kappos L, Radue EW, O’Connor P, Et al. A Placebo-Controlled Trial of Oral Fingolimod in Relapsing Multiple Sclerosis. The
New England Journal of Medicine. 2010; 362: 387-401.
7.
Kurtzke JF. Rating neurologic impairment in multiple sclerosis: an expanded disability status scale (EDSS).
Neurology.1983;33:1444-1452.
152
8.
Rovaris M. Comi G. Filippi M. MRI markers of destructive pathology in multiple sclerosis-related cognitive
dysfunction.
Journal of the Neurological Sciences.2006; 245:111-116.
9.
Rudick, RA. Lee JC. Simon J. Fisher E. Significance of T2 lesions in multiple sclerosis: A 13-year longitudinal
study. Annals of Neurology.2006;60:236-242.
10. Rieckmann P. Toyka KV. Escalating immunotherapy of multiple sclerosis. New aspects and practical application.
Multiple
Sclerosis Therapy Consensus Group (MSTCG). Journal of Neurology. 2004;251:1329-1339.
11. Leary SM. Porter B. Thompson AJ. Multiple sclerosis: diagnosis and the management of acute relapses.
Postgraduate
Medicine Journal. 2005;81:302-308.
12. Rio J. Nos C. Tintore M. et al. Assessment of different treatment failure criteria in a cohort of RRMS patients
treated with
interferon β: implications for clinical trials. Annals of Neurology. 2002;52:400-406.
13. Gilenya® Prescribing Information. Novartis, Inc. 9/2010
14. Aubagio® Prescribing Information. Genzyme Corp. 9/2012.
15. Tecfidera® Prescribing Information. Biogen Idec Inc. 3/2013.
16. Rosalind C. Kalb, Ph.D., Director, Professional Resource Center, National Multiple Sclerosis Society, “MS
Guidelines” 11
August 2004, personal email (11 August, 2004).
17. Disease modifying therapies in multiple sclerosis: Report of the Therapeutics and Technology, Assessment
Subcommittee of the American Academy of Neurology and the MS Council for Clinical Practice Guidelines.
Neurology. 58(2):169-178, January 22, 2002.
18. Morrow T, Brown J, Smith C, Thrower B. Considerations for the treatment of multiple sclerosis in the managed
care setting.
Formulary 2003; 38 (11).
Revision/Review Date: 11/2015
Associated Policy: Prior Authorization of Medications 236.200
NOTE: Clinical reviewer must override criteria when, in his/her professional judgment, the requested item
is medically necessary.
153
Field Name
Prior Authorization
Group Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber Restrictions
Coverage Duration
Other Criteria
Field Description
Injectable/Infusible Osteoporosis Agents
Boniva® Injection (Ibandronate), Forteo® (teriparatide), Prolia™
(denosumab), Reclast® (zoledronic acid) or any other newly marketed
agent
Medically accepted indications are defined using the following
sources: the Food and Drug Administration (FDA), Micromedex,
American Hospital Formulary Service (AHFS), United States
Pharmacopeia Drug Information for the Healthcare Professional (USP
DI), the Drug Package Insert (PPI), or disease state specific standard
of care guidelines.
N/A
“See other criteria”
N/A
N/A
If all of the conditions are met, requests will be approved for a 1 year.
***FORTEO REQUESTS WILL ONLY BE APPROVED FOR A
TOTAL DURATION OF 24 MONTHS***If the conditions are not
met, the request will be sent to a Medical Director/clinical reviewer
for medical necessity review.
Documentation was submitted indicating patient is
postmenopausal woman or a male patient with a bone mineral
density (BMD) value consistent with osteoporosis (T-scores
equal to or less than –2.5) or has had an osteoporotic fracture,
OR patient is over age of 50 with a T-score between
-1 and -2.5 at the femoral neck or spine and a 10 year hip
fracture probability >3% or a 10 year major osteoporosisrelated fracture probability >20%, based on the US-adapted
WHO absolute fracture risk model
The patient has a documented (consistent with pharmacy
claims) adequate trial of an oral bisphosphonate or has a
medical reason (e.g. intolerance, hypersensitivity,
contraindication, etc.) for not using an oral bisphosphonate
If request is for Forteo (teriparatide) the patient has not
exceeded a total of 24 months of therapy AND one of the
following applies to patient:
patient has documented trial and failure of Boniva
(Ibandronate) injection, Reclast (zoledronic acid) or
Prolia (denosumab) or has a medical reason (e.g.
intolerance, contraindication, etc.) why these therapies
are not suitable to be used
has SEVERE osteoporosis (T-Score -3.5 or below, or
T-Score of -2.5 or below plus a fragility fracture)
Revision/Review Date
7/2016
If diagnosis is Paget’s disease, documentation (within 60 days
of request) was submitted including patient’s serum alkaline
phosphatase level of ≥ two times the upper limit of normal, the
patient is symptomatic OR there is documentation of active
disease
The patient is taking calcium and vitamin D
The medication is FDA approved for indication and is being
requested at an FDA approved dose
Physician/clinical reviewer must override criteria when, in his/her
professional judgment, the requested item is medically necessary.
PRIOR AUTHORIZATION CRITERIA RITUXAN® (rituximab)
PA CRITERIA FOR APPROVAL FOR USE IN RHEUMATOID ARTHRITIS:
• The medication is being recommended and prescribed by a rheumatologist.
• The patient is an adult (≥18 y/o) and has a documented clinical diagnosis of rheumatoid arthritis.
• The patient has a documented (consistent with pharmacy claims data, OR for new members to the health plan
consistent with medical chart history) adequate trial (including dates and doses) of 3 months or more of therapy) of
®
methotrexate AND then leflunomide (generic Arava ) and/or another disease-modifying antirheumatic treatment
option (i.e. combination therapy - methotrexate + sulfasalazine and/or hydroxychloroquine) or has another
documented medical reason (e.g. intolerance, hypersensitivity) for not utilizing any of these therapies to manage their
medical condition.
• The patient has a documented (consistent with pharmacy claims data, OR for new members to the health plan
consistent with medical chart history) adequate trial (including dates, doses) of all preferred biologics indicated for
rheumatoid arthritis, or has documented medical reason (intolerance, hypersensitivity, etc.) for not taking ALL of these
therapies to manage their medical condition.
• Documentation indicating that Rituxan® is being used concurrently with methotrexate.
• Documentation indicating that the patient has been screened for HBV (hepatitis B virus) prior to initiation of
treatment.
• Rituxan® is being prescribed at an FDA approved dosage.
If all of the above conditions are met, the request will be approved for up to a 1 month duration; if all of the above
criteria are not met, the request is referred to a Medical Director/clinical reviewer for medical necessity review.
PA CRITERIA FOR RE-AUTHORIZATION FOR USE IN RHEUMATOID ARTHRITIS
• The member has been receiving Rituxan® and documentation is provided that a rheumatologist has reevaluated the
member and recommends continuation of therapy.
• Documentation was provided indicating that the patient had clinical benefit from receiving Rituxan® therapy.
• At least 16 weeks (4 months) has elapsed since the previous course of Rituxan® therapy.
• Documentation indicating that Rituxan® is being used concurrently with methotrexate.
• Rituxan® is being prescribed at an FDA approved dosage.
If all of the above conditions are met, the request will be approved for up to a 1 month duration; if all of the above
criteria are not met, the request is referred to a Medical Director/clinical reviewer for medical necessity review.
PA CRITERIA FOR INITIAL APPROVAL FOR USE IN NON-HODGKIN’S LYMPHOMA (NHL) AND
CHRONIC LYMPHOCYTIC LEUKEMIA (CLL):
• The medication is being recommended and prescribed by an oncologist.
• If the medication request is for Non-Hodgkin Lymphoma, documentation was submitted of confirmed diagnosis of
CD20-positive B-cell NHL
• If the medication request is for Chronic Lymphocytic Leukemia, documentation was submitted of confirmed
diagnosis of CD20-positive CLL and Rituxan® is being using in concurrently with fludarabine and cyclophosphamide
(FC)
• Documentation indicating that the patient has been screened for HBV (hepatitis B virus) prior to initiation of
treatment.
• Rituxan® is being prescribed at a dose that is within FDA approved guidelines and/or is supported by the
medical compendium as defined by the Social Security Act and/or the National Comprehensive Cancer
Network (NCCN) or American Society of Clinical Oncology (ASCO) standard of care guidelines.
If all of the above conditions are met, the request will be approved for up to a 3 month duration; if all of the above
criteria are not met, the request is referred to a Medical Director/clinical reviewer for medical necessity review.
PA CRITERIA FOR RE-AUTHORIZATION FOR USE IN NON-HODGKIN’S LYMPHOMA (NHL) AND
CHRONIC LYMPHOCYTIC LEUKEMIA (CLL):
• The medication is being recommended and prescribed by an oncologist.
• Rituxan® is being prescribed at a dose that is within FDA approved guidelines and/or is supported by
the medical compendium as defined by the Social Security Act and/or per the NCCN or ASCO standard of
care guidelines.
159
If all of the above conditions are met, the request will be approved for up to a 3 month duration; if all of the above
criteria are not met, the request is referred to a Medical Director/clinical reviewer for medical necessity review.
PA CRITERIA FOR INITIAL APPROVAL FOR USE IN GRANULOMATOSIS WITH
POLYANGIITIS (GPA) (WEGENER’S GRANULOMATOSIS) AND MICROSCOPIC
POLYANGIITIS (MPA):
• The medication is being recommended and prescribed by a rheumatologist.
• The patient is an adult (≥18 y/o) and has a documented clinical diagnosis of granulomatosis with
polyangiitis (GPA) (Wegener’s Granulomatosis) or microscopic polyangiitis (MPA).
• The patient has a documented (consistent with pharmacy claims data, OR for new members to the
health plan consistent with medical chart history) adequate trial (including dates, doses) of glucocorticoid
®
(i.e. prednisone) AND methotrexate, OR glucocorticoid AND cyclophosphamide (Cytoxan ) or
documentation includes a medical reason (intolerance, hypersensitivity, etc.) why patient is not able to use
these therapies to manage their medical condition.
• Documentation indicating that Rituxan® is being used concurrently with glucocorticoids.
• Documentation indicating that the patient has been screened for HBV (hepatitis B virus) prior to initiation of
treatment.
• Rituxan® is being prescribed at an FDA approved dosage.
If all of the above conditions are met, the request will be approved for up to a 1 month duration; if all of the
above criteria are not met, the request is referred to a Medical Director/clinical reviewerfor medical
necessity review.
PA CRITERIA FOR INITIAL AUTHORIZATION FOR USE IN OTHER MEDICALLY ACCEPTED
INDICATIONS
• The medication is prescribed for a non-FDA approved indication but is considered to be a medically
accepted use of the medication per the medical compendia (Micromedex, American Hospital Formulary
Service (AHFS), DrugPoints, the Drug Package Insert as defined in the Social Security Act and/or per the
National Comprehensive Cancer Network (NCCN), the American Society of Clinical Oncology (ASCO) or
the American Academy of Pediatrics (AAP) standard of care guidelines and has a Class I or IIa
recommendation.
• The medication is prescribed at a medically accepted dose per the medical compendia as defined above.
• The medication is recommended and prescribed a specialist in the field to treat the member’s respective medical
condition.
• Documentation indicating that the patient has been screened for HBV (hepatitis B virus) prior to initiation of
treatment.
• Documentation was submitted indicating that the member has a documented (consistent with pharmacy
claims data, OR for new members to the health plan consistent with medical chart history) adequate trial
(including dates, doses of medications) of ALL first line medical therapies as recommended by the medical
compendia and standard care guidelines and/or has another documented medical reason (e.g. intolerance,
contraindications, etc.) for not receiving or trying all first line medical treatment(s).
If all of the above conditions are met, the request will be approved for up to a 3 month duration. If all of the
above criteria are not met, the request is referred to a Medical Director/clinical reviewer for medical
necessity review.
PA CRITERIA FOR RE-AUTHORIZATION FOR USE IN OTHER MEDICALLY ACCEPTED
INDICATIONS
• The medication is prescribed at a medically accepted dose per the medical compendia
The medication is recommended and prescribed a specialist in the field to treat the member’s respective medical
condition.
• Documentation from medical chart was submitted indicating that the member has significantly clinically benefited
from the medication.
If all of the above conditions are met, the request will be approved for up to a 3 month duration. If all of the above
criteria are not met, the request is referred to a Medical Director/clinical reviewer for medical necessity review.
Revision/Review Date: 4/2016
NOTE: Physician/clinical reviewer must override criteria when, in his/her professional judgment, the
requested item is medically necessary.
160
Select Health Prior Authorization Criteria
SYNAGIS® (palivizumab): 50mg vial/100mg vial
Palivizumab Guideline for initiation and discontinuation of therapy
Palivizumab prophylaxis is indicated under the following criteria:
Infants less than 1 year of age at the onset of the RSV season (November 1 st) AND have one of the following indications:
- Born at less than 29 weeks, 0 days gestation
- Born at less than 32 weeks, 0 days gestation AND had chronic lung disease of prematurity defined as greater
than 21% oxygen for at least 28 days after birth
- Born at any gestational age with hemodynamically significant heart disease including
o Cyanotic heart disease in consultation with a pediatric cardiologist
o Acyanotic Heart disease with one of the following
On heart failure medication and expected to require cardiac surgical procedure
Moderate to severe pulmonary hypertension
Infants less than 2 years of age at the onset of the RSV season (November 1 st) AND have one of the following indications:
- Born at less than 32 weeks, 0 days AND had a diagnosis of chronic lung disease of prematurity at birth as defined
above AND had continued need for one of the following respiratory interventions in the 6 months preceding
RSV season:
o Chronic steroids
o Chronic diuretics
o Supplemental Oxygen
Palivizumab prophylaxis can be considered under the following criteria:
Infants less than 1 year or age at the onset of the RSV season (November 1st) AND have one of the following indications:
- Born at any gestational age with pulmonary abnormality or neuromuscular disease that impairs the ability to
clear secretions from the lower airway
Infants less than 2 years of age at the onset of the RSV season (November 1 st) AND have the following indications:
- Born at any gestational age and will be profoundly immunocompromised during the RSV season, including:
o Solid organ or hematopoietic stem cell transplant recipient
o Chemotherapy recipient
- Born at any gestational age and receiving a cardiac transplant
Palivizumab prophylaxis is not indicated based on:
- Diagnosis of cystic fibrosis
- Diagnosis of Down’s syndrome
- Prevention of nosocomial disease.
- Hemodynamically insignificant heart disease including:
o
o
o
o
o
o
Secundum ASD
Small VSD
Pulmonic stenosis
Uncomplicated aortic stenosis
Mild coarctation of the aorta
PDA
197
161
Palivizumab prophylaxis should be discontinued if:
There is hospitalization for breakthrough RSV infection
Revision/Review Date: 11/2015
NOTE: Medical Director/Clinical reviewer must override criteria when, in his/her professional
judgment, the requested item is medically necessary
198
162
Field Name
Prior Authorization
Group Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber
Restrictions
Coverage Duration
Other Criteria
TYSABRI
Field Description
®
Tysabri®
Medically accepted indications are defined using the following sources:
the Food and Drug Administration (FDA), Micromedex, American
Hospital Formulary Service (AHFS), United States Pharmacopeia Drug
Information for the Healthcare Professional (USP DI), the Drug Package
Insert (PPI), or disease state specific standard of care guidelines.
Member does not have a history of progressive multifocal
leukoencephalopathy (PML) or have a compromised immune system.
Documentation consistent with pharmacy claims data was submitted
indicating the patient is not currently using any antineoplastic,
immunosuppressant, or immunomodulating medications
See “Other Criteria”
Patients must be 18 years age or older
See “Other Criteria”
If all of the criteria are met, the initial request for Crohn’s Disease will
be approved for 3 months of treatment. For all other requests and for
continuation of therapy the request will be approved for 6 months of
treatment If all of the above criteria are not met, the request is referred
to a Clinical Reviewer for medical necessity review.
Documentation on request form indicates that the medication is
prescribed is authorized by the TOUCH™ program to prescribe
Tysabri® and that the patient is enrolled in the TOUCH™ program and
has agreed to comply with the requirements for receiving Tysabri®
AND
Tysabri® is being prescribed at an FDA approved dosage.
PA CRITERIA FOR INITIAL AUTHORIZATION FOR USE IN
MULTIPLE SCLEROSIS (MS):
The member has a clinical diagnosis of a relapsing form of multiple
sclerosis.
Clinical or diagnostic information was submitted that indicates that
that patient has a documented (consistent with pharmacy claims data
OR for new members to the health plan consistent with medical
chart history) treatment failure after receiving an adequate trial
(including dates, doses of 6 months or more of each therapy) of two
of the following: peginterferon Beta- 1A (Plegridy®), glatiramer
acetate (Copaxone® 40 mg), fingolimod hcl (Gilenya®) or dimethyl
fumarate (Tecfidera®) or has a some other documented medical
reason (intolerance, hypersensitivity, etc.) for not utilizing two of
these therapies for a minimum of 6 months each to manage their
163
medical condition.
Tysabri® is being prescribed by a neurologist
PA CRITERIA FOR REAUTHORIZATION FOR USE IN
CROHN’S DISEASE:
The member has a documented clinical diagnosis of moderate to
severely active Crohn’s Disease
The patient has a documented (consistent with pharmacy claims
data, OR for new members to the health plan consistent with
medical chart history) adequate trial (including dates and doses) at
therapeutic doses or has some documented clinically significant
medical reason for not receiving oral conventional therapy to
manage their medical condition.
The patient has a documented (consistent with pharmacy claims
data, OR for new members to the health plan consistent with
medical chart history) adequate trial (including dates and doses)
with therapeutic doses of or has some documented clinically
significant medical reason for not receiving Humira®
(adalimumab).
Tysabri® is being prescribed by a gastroenterologist
PA CRITERIA FOR INITIAL AUTHORIZATION FOR USE IN
OTHER MEDICALLY ACCEPTED INDICATIONS
The medication is recommended and prescribed by a specialist in
the field to treat the member’s respective medical condition.
The medication is prescribed at a medically accepted dose per
the medical compendia as defined by the Social Security Act.
PA CRITERIA FOR RE-AUTHORIZATION
The medication is recommended or prescribed by a specialist for
the respective treated disease state.
Diagnostic or clinical documentation was submitted (e.g.
improved disease activity index, quality of life, blood work,
radiographic evidence) that indicates the member has
significantly clinically benefited from receiving Tysabri®
therapy.
Revision/Review
Date 02/2016
Medical Director/clinical reviewer must override criteria when, in
his/her professional judgement, the requested item is medically
necessary.
164
PRIOR AUTHORIZATION
URINARY ANTISPASMODIC AGENTS
FORMULARY STATUS Preferred, Pays at Point-of-Sale (First Line):
DETROL® (tolterodine) Tablets, DITROPAN® (oxybutynin) Tablet & Syrup,, DETROL LA® (tolterodine)
Capsules, SANCTURA® (trospium) Tablet, DITROPAN XL® (oxybutynin) Tablets
FORMULARY STATUS Preferred, Requires Step Therapy (Second Line):
TOVIAZ® (fesoterodine) Tablets
NOTE: Patient must meet #1 criterion to meet step therapy.
FORMULARY STATUS Non-Preferred, Requires Prior Authorization (Third Line):
ENABLEX® (darifenacin) Tablets, SANCTURA XR® (trospium) Capsule, GELNIQUE® (oxybutynin) Gel:
OXYTROL® (oxybutynin) Patch, URISPAS® (flavoxate) Tablet, VESICARE® (solifenacin) Tablets
NOTE: Patient must meet #1 and #2 criteria for approval of PA request.
PA Criteria
Criteria Details
Covered Uses
Medically accepted indications are defined using the following sources: the Food and
Drug Administration (FDA), Micromedex, American Hospital Formulary Service
(AHFS), United States Pharmacopeia Drug Information for the Healthcare Professional
(USP DI), and the Drug Package Insert.
Exclusion
Criteria
None
Required
Medical
Information
See “other criteria”
Age Restrictions
None
Prescriber
Restrictions
None
Coverage
Duration
Other Criteria
If criterion is met, the request will be approved with a 12 month duration. If criterion is
not met, the request will be referred to a Clinician for medical necessity review.
AUTHORIZATION:
Documented trial and failure or intolerance to a first line generic product for at least 4
weeks (28 days) of therapy within the past 3 months.
Documented trial and failure or intolerance to a first and a second line therapy for at
least 4 weeks (28 days) of therapy in the past 6 months each.
Review Date: 11/2015 NOTE: Clinical reviewer must override criteria when, in his/her professional
judgment, the requested item is medically necessary.
165
Field Name
Prior Authorization
Group Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber Restrictions
Coverage Duration
Other Criteria
Field Description
Vancocin®
Vancocin® (vancomycin) capsule
Medically accepted indications are defined using the following
sources: the Food and Drug Administration (FDA), Micromedex,
American Hospital Formulary Service (AHFS), United States
Pharmacopeia Drug Information for the Healthcare Professional (USP
DI), the Drug Package Insert (PPI), or disease state specific standard
of care guidelines.
N/A
See “other criteria”
N/A
N/A
If the criteria are met, the request will be approved for a 10 – 14 day
duration; if the criteria are not met, the request will be referred to a
clinical reviewer for medical necessity review.
Initial Authorization:
Staphylococcal Enterocolitis:
Diagnosis of enterocolitis caused by Staphylococcus aureus.
Pseudomembranous Colitis:
Diagnosis of antibiotic associated pseudomembranous colitis
produced by C. difficile.
AND
For mild-to-moderate infection:
Documented trial and failure with therapeutic doses or intolerance
to metronidazole if mild-to-moderate C. difficile infection (CDI).
For severe infection:
With severe infection, vancomycin is the drug of choice for initial
treatment.
For severe, complicated infection:
Vancomycin administered orally with or without I.V.
metronidazole is the initial regimen of choice for treatment of
severe, complicated CDI.
Considerations for automatic approval:
Member is age 65 or greater
Member has renal dysfunction
Recently discharged from hospital on PO vancomycin
Revision/Review Date
07/2016
Medical Director/clinical reviewer must override criteria when, in
his/her professional judgement, the requested item is medically
necessary.
Field Name
Prior Authorization
Group Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber Restrictions
Coverage Duration
Other Criteria
Field Description
Vfend®
Vfend®(vorizonazole) tablets and oral suspension
Medically accepted indications are defined using the following
sources: the Food and Drug Administration (FDA), Micromedex,
American Hospital Formulary Service (AHFS), United States
Pharmacopeia Drug Information for the Healthcare Professional (USP
DI), the Drug Package Insert (PPI), or disease state specific standard
of care guidelines.
N/A
See “other criteria”
FDA recommends use in patients 12 years of age and older.
N/A
If the above conditions are met, the request will be approved with up
to a 3 month duration depending upon the severity of the infection; if
the above conditions are not met, the request will be referred to a
clinical reviewer for medical necessity review.
.
Initial Authorization:
Revision/Review Date
07/2016
Diagnosis of invasive aspergillosis or a serious fungal infection
caused by Scedosporium apiospermum and Fusarium species.
Medical Director/clinical reviewer must override criteria when, in
his/her professional judgement, the requested item is medically
necessary.
Field Name
Prior Authorization
Group Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber Restrictions
Coverage Duration
Other Criteria
Field Description
VIVITROL®
Naltrexone Intramuscular Injection
Medically accepted indications are defined using the following
sources: the Food and Drug Administration (FDA), Micromedex,
American Hospital Formulary Service (AHFS), United States
Pharmacopeia Drug Information for the Healthcare Professional (USP
DI), the Drug Package Insert (PPI), or disease state specific standard
of care guidelines.
Patients receiving opioid analgesics, patients in acute opioid
withdrawal, patients with a positive urine screen, or patients with acute
hepatitis or liver failure.
See “other criteria”
Patient must be 18 years of age or older
See “Other Criteria”
If all of the conditions are met, the request will be approved with 3month duration. If all of the criteria are not met, the request is referred
to a clinical reviewer for medical necessity review.
Initial Authorization:
OR
Prescriber is, or has consulted with a behavioral health or
licensed Drug and Alcohol (D&A) provider.
Patient must have diagnosis of opioid dependence,
following opioid detoxification
alcohol dependence and documentation has been provided
that patient is able to abstain from alcohol in an outpatient
setting.
Documentation is provided of an initial evaluation by a
D&A provider to recommend level of care.
Documentation is provided of a referral to or participation
in a substance abuse or behavioral health treatment
program or behavioral health counseling by a licensed
D&A provider.
Documentation has been provided that the patient was
screened for depression and risk of suicide. If these
conditions are present, documentation is provided that the
patient was referred for treatment with a behavioral health
provider.
Documentation is provided that the patient is free from
opioids (including tramadol) for a minimum of 7-10 days
before starting therapy, or for alcohol dependence the
patient is not actively drinking.
Re - Authorization:
Documentation submitted includes participation in a substance
abuse or behavioral health counseling, treatment program, or an
Revision/Review Date
07/2016
•
addictions recovery program with a licensed D&A or behavioral
health provider.
Documentation of monthly urine drug screens that are
negative for opiates (specifically including oxycodone and
fentanyl) and also for licit and illicit drugs with the
potential for abuse. ( Lab results are required)
If diagnosis is alcohol dependence, documentation of
monthly blood alcohol (ethyl alcohol) testing is also
required.
Negative pregnancy test (for women, as indicated)
within 30 days of request. If test is positive, request
will be denied and member should be treated with
buprenorphine.
If patient has symptoms of depression or is at risk for
suicide, documentation has been provided that the patient
is being treated by a behavioral health provider.
Medical Director/clinical reviewer must override criteria when, in
his/her professional judgement, the requested item is medically
necessary.
Field Name
Prior Authorization
Group Description
Drugs
Covered Uses
Exclusion Criteria
Required Medical
Information
Age Restrictions
Prescriber
Restrictions
Coverage Duration
Other Criteria
Field Description
WHITE BLOOD CELL STIMULATORS
FORMULARY STATUS Specialty Tier (PA required)
• Zarxio™ (Filgrastim-sndz)
• Neupogen® (Filgrastim)
• Neulasta® (Pegfilgrastim)
• Mozobil® (Plerixafor)
• Leukine® (Sargramostim)
Medically accepted indications are defined using the following sources:
the Food and Drug Administration (FDA), Micromedex, American
Hospital Formulary Service (AHFS), United States Pharmacopeia Drug
Information for the Healthcare Professional (USP DI), the Drug Package
Insert (PPI), or disease state specific standard of care guidelines.
N/A
See “other criteria”
N/A
N/A
The request will be approved for up to 12 weeks. If all of the above
criteria are not met, the request is referred to a Medical Director/clinical
reviewer for medical necessity review.
Initial Authorization:
• For Leukine® requests ONLY: Documentation is submitted of the
patient’s current diagnosis, current bodyweight, body surface area and
absolute neutrophil count (within 30 days of the request).
• For Neulasta® requests ONLY: If the medication request is being
ordered for a patient requiring dose dense chemotherapy (i.e. for a
documented diagnosis of breast cancer) no prior trials of any other white
blood cell stimulator is needed for that patient.
• For Neupogen® requests that are less than 180mcg, Neupogen® can
be approved. For all other requests for Neupogen® or Neulasta®: the
patient has a documented treatment failure {i.e. failure to reach and/or
maintain target ANC, prolonged febrile neutropenia, unplanned
hospitalization, infection requiring prolonged anti-infectives} which is
consistent with pharmacy claims data, with an adequate trial (including
dates, doses of therapy) of Zarxio™ and/or has another documented
medical reason (intolerance, hypersensitivity, or dose dense
chemotherapy, stem cell collection, etc.) for not using Zarxio™ to treat
their medical condition.
• For Mozobil® requests ONLY: documentation must be submitted that
the patient is using Mozobil® in combination with a granulocyte-colony
stimulating factor (G-CSF) agent (i.e. Zarxio™)
• Patients ANC (absolute neutrophil count) has been submitted with
request and prescribed dosing of medication is within FDA approved
dosing.
Revision/Review
Date 07/2016
Medical Director/clinical reviewer must override criteria when, in
his/her professional judgement, the requested item is medically
necessary.
PRIOR AUTHORIZATION CRITERIA FOR XOLAIR
Xolair® (omalizumab): 150 mg lyophilized powder for injection
Formulary Status: Non Formulary
PA CRITERIA FOR INITIAL APPROVAL FOR ASTHMA:
•
The physician who has requested Xolair is pulmonologist or allergist or
documentation (consultation) was submitted with the request indicating that Xolair was
recommended by a pulmonologist or allergist.
•
The patient’s age is > 6 years old and the patient has a > 1 year history of moderateto-severe asthma
•
The patient’s total serum IgE ≥ 30 IU/ml to ≤ 700 IU/ml for patients 12 and older or
IgE ≥ 30 IU/ml to ≤ 1300 IU/ml for patients 6-12 years old, and the prescribed dose is
within approved FDA dosing guidelines for the IgE level and weight
•
The patient has a documented baseline FEV1 < 80% of predicted or FEV1/FVC that
has been reduced by at least 5% of normal for the patient age range (see Table 1 below).
•
The patient has a documented history of one or more of the following: requires daily
use of inhaled short acting B2 agonists, history of daily or continual asthma symptoms,
limited physical activity or activity affected by exacerbations due to asthma, and frequent
(> once per week) nighttime symptoms
•
Documentation that the patient is still having significant symptoms (i.e. hospital
admission, emergency room visits, and/or the severe of asthma exacerbations) while
compliant on a high-dose inhaled corticosteroid with a long-acting B2 agonists + a
leukotriene receptor antagonist or theophylline. If the patient is not utilizing these
therapies, documentation must include a medical reason for not maximizing both high
dose inhaled corticosteroids with long acting bronco dilator medication (e.g. side effects,
intolerance, and hypersensitivity).
•
The patient has a positive documented immediate response on RAST test and/or skin
prick test to at least 1 common allergen (e.g. dermatophagoides farinae, dermatophagoides
pteronyssinus, dog, cat, or cockroach) and there is documented evidence that the positive
skin tested allergen(s) is an asthma trigger either from environmental exposure or from
testing or from attempted allergen immunotherapy
•
Documentation was submitted that the patient has received immunotherapy and
despite this the patient had documented clinical asthma recurrence/persistence precipitated
by the allergen(s) for which the patient is receiving immunotherapy that had resulted in a
hospital admission or emergency room visit, OR if the patient has not received allergy
shots they have a documented medical reason for not taking allergy shots (e.g. severe,
unstable asthma or severe, systemic injection reactions)
•
Documentation was submitted indicating what environmental measures were
attempted to avoid and/or minimize exposure to identified allergen asthma triggers OR a
reason (e.g. unavoidable allergen) for not trying to avoid asthma allergen trigger(s)
•
The patient is not receiving any medication (e.g. Beta Blockers or NSAIDs) that
could cause bronchospasm or cause an asthma exacerbation and if the patient is on a
potential asthma inducing medication, that there is a documented medical reason for
continuing that medication as well as documentation that the medication is not a cause for
worsening asthma or causing any asthma symptoms
If all of the above conditions are met, the request will be approved with a 4-month
duration; if all of the above criteria are not met, the request is referred to a Medical
Director/Clinical Reviewer for medical necessity review.
PA CRITERIA FOR INITIAL APPROVAL FOR CHRONIC IDIOPATHIC
URTICARIA:
•
The physician who has requested Xolair is an allergist, immunologist or dermatologist
or documentation (consultation) was submitted with the request indicating that Xolair was
recommended by a specialist that treats urticaria
•
The patient’s age is > 12 years old.
•
The patient has a documented history of urticaria for at least 3 months
•
The patient remains symptomatic despite adequate trials of TWO formulary H1
antihistamines (1st generation-e.g. hydroxyzine, cyproheptadine and 2nd generation –
loratidine, cetirizine), a formulary H2 antihistamine (e.g. famotidine, ranitidine)and
Montelukast.
•
The patient requires oral steroids to control symptoms
•
The prescribed dose is within approved FDA dosing guidelines
If all of the above conditions are met, the request will be approved with a 4-month
duration; if all of the above criteria are not met, the request is referred to a Medical
Director/Clinical Reviewer for medical necessity review.
PA CRITERIA FOR REAUTHORIZATION AFTER 4 MONTHS OF THERAPY
FOR ASTHMA:
•
Documentation submitted indicates that the member has significantly clinically
benefited from the medication (e.g. patient has marked improvement in pulmonary function
tests such as FEV1 or peak expiratory flow rate, decrease in asthma exacerbations and/or a
decrease in inhaled or oral corticosteroid use since receiving Xolair therapy)
The prescribed dose is within approved FDA dosing guidelines
•
If all of the above conditions are met, the request will be approved with a 6-month
duration; if all of the above criteria are not met, the request is referred to a Medical
Director/Clinical Reviewer for medical necessity review.
PA CRITERIA FOR REAUTHORIZATION AFTER 4 MONTHS OF THERAPY
FOR CHRONIC URTICARIA:
•
Documentation submitted indicates that the member has significantly clinically
benefited from the medication
•
The member has been receiving the medication and documentation was provided that
the prescriber has evaluated the member and recommends continuation of therapy
•
The prescribed dose is within approved FDA dosing guidelines
If all of the above conditions are met, the request will be approved with a 6-month
duration; if all of the above criteria are not met, the request is referred to a Medical
Director/Clinical Reviewer for medical necessity review.
Table 1: Normal FEV1/FVC
Patients Age:
Normal Values:
85 %
8 - 19 y/o
20 - 39 y/o
80 %
40 - 59 y/o
75 %
70 %
60 - 80 y/o
Review Date: 7/2016
Medical Director/Clinical reviewer must override criteria when, in his/her professional
judgment, the requested item is medically necessary.