* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download CVCOM COMLEX 2-PE QUICK REFERENCE Start of 14
Survey
Document related concepts
Transcript
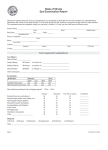
CVCOM COMLEX 2-PE QUICK REFERENCE Start of 14-minute session announced Targeted completion time (TCT) < 1 minute Open wall unit and review: Patient Data Sheet: Circle abnormal BP, pulse, and respirations to be repeated during exam Ancillary provided data: EKGs, laboratory results, etc. Enter the room Stop a few feet inside the door, facing the patient be addressed TCT < 1 minute Ask the patient how he or she prefers to Maintain eye contact; Introduce yourself by name and title Excuse yourself to wash your hands while explaining need to wash before touching the patient Sit on the examination stool History TCT ~ 5 minutes Ask “What brings you in today?”; “What may I do for you today” Allow the story to develop and follow historical clues; Use open-ended questions Maintain eye contact 50% of the time Follow patient comments with humanistic statements about the patient’s work, family, job, ADL’s Fill in the spaces next to the associated letter in the mnemonic as history is obtained Keep a running list of possible diagnoses as they enter the differential Ask symptoms associated to rule in or out each possible diagnosis When you believe the history is complete Summarize the story with the patient Return to blanks in the mnemonic to obtain skipped information Continued Physical Exam TCT < 5 minutes Ask the patient permission to start the examination (examine the patient) Usually best to include cardiac and pulmonary examination with each case; may be short in non cardiopulmonary case Ask if each area encountered would be affected with the suspected diagnosis Skip those areas not affected; include your osteopathic structural examination skills while performing the physical examination Examine in detail the primary absolute organ system affected inspection, auscultation, palpation, percussion, osteopathic structural examination Perform examination of adjacent areas with detail as needed Perform limited examination of distant systems of possible involvement Advise patient of any prohibited examinations (i.e., breast, rectal, or genital) and explain that they would be recommended 2-minute warning: If you have not finished the exam, stop and proceed with the assesssment Assessment: Provide the patient with the proposed diagnosis. TCT < 1 minute This is essentially a differential of the possible diagnoses related to the history, ROS, and physical examination finding’ They should be listed in order of most likely diagnosis Plan: Utilize MOTHRR mnemonic. Consider each component TCT ~ 2 minutes without OMM Medications: Instruct patient on type of medication and how to take it; also list any medications you may wish the patient to stop taking OMM: If appropriate, offer OMM and perform (NO HVLA) and limit to 3 to 5 minutes Testing: Advise patient of labs, imaging, or other testing being ordered; this must be specific to lab types, diagnostic tests, and modalities (PT, OT, home exercise program) Holistic/Humanistic Advise patient of PRICE, work restrictions, diet changes, smoking cessation, preventive medicine counseling (safe sex, condom us, immunizations) Express concern over the condition. Offer to involve family members. Ask them if they can complete the proposed treatment plan Referrals: Advise patient if referrals are being made Return: Advise patient of need for admission, or develop a finite follow-up plan for the office and when to go to the ER Ask the patient if he or she has any questions Thank the patient, shaking hands Exit the room SOAP note documentation: 9-minute Begin the SOAP note immediately upon exiting the room DO NOT document any history or examination that should have been completed but that was not. Document: Date and time Chief Complaint S: CC and HPI: Paragraph form History: Bulleted O: Vitals and general survey; any repeated vitals Systems by bulleted headings A(D): Minimum of four diagnoses related to the chief complaint in order of likelihood Notate less likely diagnoses by “rule out” or “doubt” Secondary diagnoses last P: MOTHRR Format Meds: Minimally name the class. Provide name, dose, frequency, and instructions; meds to discontinue as well OMM: Techniques used Testing: Imagining, laboratory, or other testing; be specific Referrals Return plan for office and ER if needed Note any history, examination, or manipulation that should have been taken or performed, but that was not done during the patient encounter. Legible signature Print name if not legible If the end of session is announced at any time before you are finished, immediately stop and put your pencil down.