* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Shorter version LaDoL guidance - Derbyshire Alliance for End of
Survey
Document related concepts
Transcript
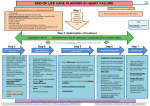
Guidance for the care of patients who are approaching the last days of their lives Patient deteriorating and likely entering last days of life Signs include becoming increasinglybedbound, drowsy, disorientated, weak, dependant and finding it hard to swallow and take medications Decisions MUST HAVE SENIOR RESPONSIBLE CLINICIAN INPUT ALL REVERSIBLE CAUSES MUST HAVE BEEN FIRST CONSIDERED Speak with patient and family Ensure that the patient if able and those close to them are fully involved in the decision making process, have been informed of the current situation, and proposed plan of management. Allow time/opportunity to express the known wishes of the patient and those of the family. (see communication section for further advice) Does patient have any specific wishes Review medication and ensure treatment is appropriate for current situation Prescribe anticipatory drugs Assess need for medically assisted hydration and nutrition Ensure has DNACPR in place Does patient have specialist palliative care needs This might include pain or symptoms that are not easily controlled or support for the patient or those close to them. If yes refer to hospital team Ring 2693 and leave message For urgent referrals bleep 099, 097, 571, 570, or 642 Out of hours advice via hospital switchboard (Request page on-call palliative SPR) Preferred place of care If patient is suitable for discharge, where do they want to be ? Hospital Other Start LADOL patient daily chart Clarify wishes with patient and family, if discharge viable option complete fast track documentation Nurses to speak with family and ensure fully understand plan of care, have opportunity to raise concerns and are aware of carer communication sheet and its uses liaise with discharge team and follow fast track discharge policy and liaise with appropriate services/community partners NB Please refer to palliative care team for assessment of suitability for referral for hospice care NB this document does not replace good clinical decision making for the individual patient it serves as guidance only. Patient assessment/ Care planning After identification that the patient is likely in the last days of life then a more detailed assessment and interaction with the patient and family should take place Areas to be covered include●Specific patient wishes ●Unfinished business ●Place of care ●Family requests ●Review of medication ●Identification of main contact ●Religion and culture ●Preservation of Privacy and dignity ●Issues surrounding mental capacity ●Review of clinical interventions including medically assisted hydration and nutrition, DNACPR status ●Organ donation From the assessment a detailed plan of care is formulated that is tailored and responsive to each individual patients needs and wishes. If patients are no longer able to decide for themselves through lack of capacity or ill health then families need to be asked what they think the patient would have wanted Further guidance on the assessment process can be found on the palliative care tab on ward carts or in the resource file situated in every ward area. Note the GMC guidance (2010) Treatment and care towards the end of life: good practice in decision making provides more detailed advice. Using the LaDoL bundle The LaDoL bundle is based on the recommendations of the Leadership Alliance for the care of dying people "one chance to get it right". It has been designed to help healthcare professionals provide high quality care and support to patients who are thought to be in the last days of their lives. Components ●LaDOL patient daily chart ●Patient guidance booklet ●Palliative care PRN bundle on JAC ●Ward resource file (Nursing) ●Checklists for Health Care Professionals ●Patient relative information leaflet ● Assessment and prescribing guidance on palliative care tab (ward carts) NB To be used in conjunction with usual nursing and medical documentation Underpinning principles Timely identification Patients whose condition undergoes serious change must be identified and assessed promptly. If the change is reversible then, with consideration for the patients wishes, treatment focus should be on maintaining life and wellbeing. Where the change is irreversible then the focus should move towards preserving comfort and dignity. The appropriateness of use of the LADOL bundle is reviewed whenever any change occurs or at least every day. Using the LaDoL bundle UNDERPINNING PRINCIPLES Communication It is essential that patients and those close to them are fully informed in a way that is easily understood, are involved in the planning of care and have the opportunity to discus their concerns, wishes and preferences about care and treatment. There should be regular sensitive communication with those close to the patient, its especially important that any changes in condition or how we are managing care are passed on to the family.Identify where possible who the patient wishes to be informed of any condition changes and ensure their contsct details are checked. All communication and descisions made must be carefully documented. . Carer Support Named nurse for each shift is responsible for ensuring that the patient/family understand the situation, know of any changes to mangement and have had opportunity to voice any concerns/questions. It is important that we enable the patients family to spend time with them and feel part of the care. We need to recognise this as a difficult time for relatives and should assess their needs and signpost to support, such as their GP, health psychology etc. Ensure available written information is offered. Give information about overnight accomodation, open visiting facilities and car parking Carer Communication Sheet At each interaction with the patient check for any new information left on the carer communication sheet, please insure any questions posed there have been answered and discussed with the patients family. Privacy & Dignity Ensuring privacy and dignity is respected is an essential component of care. Where possible a side room should be offered if not possible then this should be explained and documented. All interventions are planned with the individual patient in mind respecting their individual wishes, their situation and their needs. Coordination Every patient must have senior responsible clinician or consultant who is clearly identified on the open ward electronic notice board. An identified named nurse each shift, is named on the daily record sheet You should seek specialist advice if needs are complex and or beyond your limits of competence Ongoing assessment Patient checks are carried out between 1 and 4 hourly, dependant on the needs/wishes of patients and their relatives. Relatives often value time with their loved one but it can be a lonely and frightening time and some families may prefer frequent checks and some may not want disturbing often.(identify and document if any preference). Ensure relatives are aware of how to call for assistance. Each day an assessment must be performed by a Doctor to ensure that the focus of care remain appropriate, if a patients condition has improved then the level of care they are receiving must be considered (document and discuss with the patient and /or their family). Ongoing Assessment At each assessment consider the following interventionsPRIVACY & DIGNITY ●Consider side room - offer if available acknowledge/explain if not ●Ensure you are aware of patient and family's preferences ●Pay attention to appearance i.e. brush hair ●Ensure is adequately covered ●Never speak over the patient MOUTH CARE ●Give as frequently as possible -Use foam stick soaked in water /juice or preferred beverage -Apply white paraffin to lips. ●Use Saliva replacement spray/gel ●Instruct and assist family if they wish to be involved ● Chart when given PRESSURE AREAS/POSITION CHANGES ●Reposition for comfort ●Consider if patient has position of preference -Is balance between skin integrity and patient comfort ●Describe pressure areas daily on patient chart ●Ensure appropriate pressure relieving equipment used ●Chart each position change PERSONAL HYGIENE ●Assess if is clean and dry ●Offer bed bath at least once each day -Aim is to ensure patient is clean/fresh without causing distress ●Chart when any intervention given ●Chart if patient/family request no input ELIMINATION ●Check is clean and dry ●Manage continence using pads urinary sheath ● Chart urinary output and bowel actions ●Urinary retention and /or constipation can cause distress, pain and agitation -If so consider urinary catheter and/or PR intervention ASSESSMENT OF SYMPTOMS ●Score the severity of the symptom at each assessment -with 0 = absent 1 = low 2 = moderate 3 = severe ●Ask patient where able to respond ●Ask family how settled they feel patient is ●Always consider reversible causes such as constipation. positioning, urinary retention ●This enables ongoing assessment of symptoms over time -allowing changes to medication to make sure that the patient has the best control of symptoms possible ● Chart score at each review Observe for signs of PAIN ●Grimace ●frown ●groaning ●restlessness ●pain on movement ●If in pain give PRN analgesia and document effect Observe for signs of AGITATION ●Hallucinations ●Restlessness ●Disorientation ●Thrashing ●If agitated give PRN anti-psychotic and document effect Ongoing Assessment At each assessment consider the following interventionsObserve for signs of RESPIRATORY TRACT SECRETIONS ●Noisy audible breathing -may be more distressing to family than for patient ●Positioning and use of suction is also important ●Chart score at each review ●If problematic give PRN anti-spasmotic and document effect Observe for signs of NAUSEA &VOMITING ●Retching ●hiccups ●chart any occurrence of vomiting ●If problematic give PRN anti-emetic and document effect Observe for signs of BREATHLESSNESS ●Fast or laboured breathing -oxygen should only be used for patient comfort nasal canulae is often sufficient ●If problematic give PRN medication and document effect PRN MEDICATION & SYRINGE DRIVERS ●Use separate chart to record and monitor use of syringe driver ●If has symptoms give prn medication and monitor effect, if not resolved after 1 hour or symptom persistent than redose ●If needing more than 1-2 doses in 24 hour period then ensure medical team are aware as may need to increase/commence syringe driver EATING &DRINKING ●Ensure all patients who are able to eat and drink are offered small frequent drinks and soft diet -Chart input ●If unsafe swallow need to decide and document if appropriate to comfort feed accepting increased risks of aspiration CLINICALLY ASSISTED HYDRATION/NUTRITION (CA N/H) ●Status of hydration/nutrition must be reassessed each day ●If CA N/H insitu must decide if giving benefit, if no benefit or may be causing issues such as oedema etc then need to consider stopping. ●if CA N/H not in place then need to decide if may be of benefit i.e. may help with confusion agitation COMMUNICATION ●Check understanding ●Explain the situation ●What to expect ●How to alert staff to any problem or issue ●Inform re facilities and support services ●Check aware of carer communication sheet ●Touch is an important method of communication in those who cannot verbally communicate Support may be needed with social/financial issues, anxiety/depression frustration and anger are common people for experiencing loss LIAISON WITH MEDICAL TEAM ●Medical team should check and respond to patient daily chart and carer communication sheet at least daily ●refer to palliative care if any issue beyond scope of competence/any uncertainty or if patients symptoms have not settled within 24hours Management of Symptoms Symptom Pain Agitation Secretions Actions Aim- Patient is pain free ●Can use liquid opiod if able to swallow ●If usually on strong opioid and unable/finding it difficult to swallow will need to convert to syringe driver - see dose conversion chart for details of how to do this ●To calculate PRN analgesia dose divide total daily dose by 6. i.e if on a syringe driver with 30mg diamorphine over 24 hours then PRN dose will be 5mg Diamorhine S/C ●Standard doses on JAC Paracetamol 1g oral or IV Diamorphine* 2.5-5mg S/C PRN Oramorph* 5-10mg orally PRN (in pts able to swallow) (May be given at higher doses*) ●Other drugs that can be used where Aim- Patient is not agitated ●First exclude reversible causes such as urinary retention, constipation, pain, hypercalcaemia. ●Delirium is when patients are confused, disorientated and may experience hallucinations ●Anxiety is when patients are oreintated but frightened, upset and in turmoil Standard doses on JAC Midazalam* 2.5mg S/C PRN (Anxiety) Haloperidol* 2.5mg S/c PRN (Delirium) (May be given at higher doses*) Aim- Patient or carer not distressed by patients Standard doses on JAC Hyoscine Butylbromide 20mg S/C PRN excessive secretions ●Positioning may help either sitting up slightly or laying on either side may help drain secretions from airways ●Suction can also be used if needed Nausea &vomiting Breathlessness Medication Aim- Patient does not feel nauseated and is not prescribed includeAlfentanyl, Oxycodone, Methadone, tramadol, Fentanyl (nasal or buccal), ketamine, ketoralac, clonazepam ●Other drugs that can be used where prescribed includeLevomepromazine 6.25mg S/C, Olanzapine (Anxiety) Diazepam, Lorazepam, Clonazepam (Delerium) ●Other drugs that can be used where prescribed includeGlycopyronium Standard doses on JAC Haloperidol 1.5-2.5mg S/C PRN vomiting ●If previously on anti-emetic and having difficultly, cannot ●Other drugs that can be used where swallow or is nauseated/vomiting then convert at same prescribed includedose to a syringe driver Levomepromazine 6.25mg S/C PRN (delirium) Metoclopromide, Ondansetron, Granesetron (anxiety) Aim- Breathlessness is not distressing for the patient ●For tachypnoea (rapid shallow breathing) use diamorphine to slow and strengthen breathing ●For Anxiety/Distress use Midazalam to calm breathing Standard doses on JACDiamorphine 2.5-5mg S/c PRN (rapid breathing) Midazalam 2.5-5mg S/C PRN (anxiety/distress) For rapid breathing as per pain relief For anxiety/distress: ●Other drugs that can be used where prescribed includeLorazepam, diazepam, Clonazepam ●If patient has ongoing pain or other symptom then ensure has had a medical review and where appripriate has got a syringe driver or regular medication prescribed. ●It will take up to4-6 hours for a syringe driver to start to have effect, consider giving PRN medication at setup if patient symptomatic ●It usually takes 20-30 mins for PRN medications to start to have any effect and up to 1 hour for full effect to be reached, if symptoms not relieved in 1 hour then need to redose. ●To calculate subsequent doses review how much has been given in past 24 hrs if more than 1 or 2 doses (not pre-emptivley) then consider a 30-50% increase in regular dose. ●If patient unsettled for more than 24 hours request specialist palliative care team review