* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download SAD Drugs
Survey
Document related concepts
Transcript
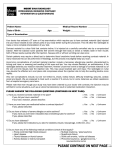
Self-Administered Drug Exclusion List R2 This updated article, published originally 09/26/2013 with an effective date of 09/30/2013 has been further revised for publication 10/08/2013, still to be effective 09/30/2013, and replaces the prior article in its entirety. The prior article in this series, from “ Medicare A News,” Issue 2109 June 2013, and “ Medicare B News,” Issue 286 June 2013 is being revised to add the following new drugs effective September 30, 2013: Certolizumab Pegol (Cimzia), J0718, Methylnaltrexone (Relistor), J2212, Phentolamine mesylate (Regitine), J2760, Unclassified Drug (Methylnaltrexone bromide), J3490, Unclassified Drug (Tesamorelin acetate), J3490, Unclassified Drug (Trimix), J3490, Unclassified Drug (Liraglutide GLP-1, Victoza®), J3490 and Unclassified Biologics (Simponi-anti-TNF (Golimumab), J3590 and abatacept (Orencia subcutaneous), J3590. This revised list (from an earlier draft) indicates abatacept administered by subcutaneous injection should be coded as J3590. The code J0129, which is specific for only the intravenous formulation of abatacept (Orencia), has been removed from and is not included in Noridian’s self-administered drug (SAD) determinations. The unclassified drug Acthar – ACTH gel (J3490) is changed to HCPCS code J0800. All other information remains the same. This article provides notification of the Noridian SAD determinations. The following SAD list is current as of 09/30/2013. However, the Contractor Medical Directors (CMDs) review the list on an ongoing basis and may update and republish at their discretion. The SAD review process only applies to medications described by Internet Only Manual (IOM) Medicare Benefit Policy Manual, Publication 100-02, Chapter 15, Section 50.2 at http://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Downloads/bp102c15.pdf . Further, effective 9/30/2013, the Centers for Medicare and Medicaid Services has determined that the two drugs abatacept (J0129 Orencia®), and golimumab (J3590 for Simponi® Aria™) are each separate drugs as defined in the Medicare Benefit Policy Manual, Publication 100-02, Chapter 15, Section 50.1 (ref. http://www.cms.gov/Regulations-andGuidance/Guidance/Manuals/Downloads/bp102c15.pdf ) and are not usually self-administered. They are therefore covered pharmaceuticals when other conditions of coverage are met and the use is a medically necessary intravenous infusion incident to a physician’s service. For dates of service on and after 12/01/2013, to indicate that it was medically necessary to use this formulation for this specific administration of either of the drugs abatacept (J0129 Orencia®), or golimumab (J3590 for Simponi® Aria™), the provider is to place the appropriate HCPCS code for the drug on one claim line and one of the appropriate IV administration codes (96365, 96366, 96367, 96368, 96374 or 96375) on an adjacent line of the same claim. The medical record must clearly document why this specific form of the drug and this mode of administration was medically necessary for this patient for this specific administration. To indicate that these conditions of coverage have been met, the provider must append the KX modifier to both the drug code (J0129 for Orencia® or J3590 for Simponi® Aria™) and to the associated IV administration code (96365, 96366, 96367, 96368, 96374 or 96375). If these conditions of coverage are not met, then the provider is to place the appropriate GA, GZ or GY code on both the drug and the IV administration code. Claims for J0129 Orencia® and claims for J3590 for Simponi® Aria™ submitted without a KX, GA, GZ or GY modifier on both the drug and IV administration codes will be returned unprocessable. Providers are reminded that convenience for the beneficiary or for the provider does not meet medical necessity under Medicare. Therefore concern for a patient’s financial liability or that a patient’s compliance with the medication regimen will suffer if the drug is not provided incident to a physician’s service, does not justify medical necessity. Additionally, effective 9/30/2013, the Centers for Medicare and Medicaid Services has determined that the drug certolizumab in its lyophilized powder form for reconstitution (J0718 Cimzia®, used for the lyophilized form) is an individual drug (distinct from J0718 Cimzia®, used for the non-lyophilized form) as defined in the Medicare Benefit Policy Manual, Publication 100-02, Chapter 15, Section 50.1 (ref. http://www.cms.gov/Regulations-andGuidance/Guidance/Manuals/Downloads/bp102c15.pdf ) and is not usually self-administered. It is therefore a covered pharmaceutical when other conditions of coverage are met and the use is a medically necessary reconstitution of the lyophilized powder form with subcutaneous injection, provided incident to a physician’s service. For dates of service on and after 12/01/2013, to indicate that it was medically necessary to use this formulation for this specific administration of the drug, the provider is to place the appropriate HCPCS code for the drug (J0718 used for the lyophilized form) on one claim line and the appropriate subcutaneous administration code (96372) on an adjacent line of the same claim. The medical record must clearly document why the lyophilized form of the drug was medically necessary for this patient for this specific administration. To indicate that these conditions of coverage have been met, the provider must append the KX modifier to both the drug code (J0718) used for the lyophilized form and to the associated subcutaneous administration code (96372). If these conditions of coverage are not met, then the provider is to place the appropriate GA, GZ or GY code on both the drug and the subcutaneous administration code. Claims for J0718 for the non-lyophilized form, if submitted, must have appended the appropriate GY modifier on both the drug code (J0718) and on the associated subcutaneous administration code (96372), reflecting the non-covered status as a usually self-administered drug. Claims for J0718 submitted without a KX, GA, GZ or GY modifier on both the drug and subcutaneous administration codes will be returned unprocessable. Providers are reminded that convenience for the beneficiary or for the provider does not meet medical necessity under Medicare. Therefore concern for a patient’s financial liability or that a patient’s compliance with the medication regimen will suffer if the drug is not provided incident to a physician’s service, does not justify medical necessity. Additionally, based on chronic, frequent injections, typically by the patient and with prolonged use, Noridian has determined that the following drugs are usually self-administered and therefore NOT COVERED by the Medicare program effective for dates of service on/after the date of service listed. (The article “Self-Administered Drugs – Process to Determine Which Drugs Are Usually Self-Administered by the Patient” was published on the Noridian website, https://www.noridianmedicare.com. Descriptor Generic Code Name J0135 J0270 J0275 J0630 J0718 J0800 J1324 J1438 J1559 J1562 J1595 J1675 J1744 Injection , Adalimumab, 20 mg Injection, alprostadil per 1.25, mcg Alprostadil urethral suppository, variable Injection, calcitonin salmon, up to 400 units Injection, Certolizumab pegol, 1 mg Corticotropin, up to 40 units Injection, enfuvirtide, 1 mg Injection, etanercept, 25 mg Injection, immune globulin, 100 mg Injection, immune globulin, 100 mg Injection, glatiramer acetate, 20 mg Injection, histrelin acetate, 10 mcg Injection, Icatibant, 1 mg Descriptor Brand Name Humira® Exclusion Basis for Exclusion Effective Exclusion1 End Date Date A, B 11/01/2003 N/A Alprostadil®, Caverject®, 01/15/2003 N/A Edex®, Prostin VR Pediatric® Muse® Calcimar®, Miacalcin® 01/15/2003 N/A A, B A, B A, B 01/15/2003 N/A A, B Cimzia (self- administered form only) 09/30/2013 N/A Acthar* - ACTH gel 06/26/2013 N/A Fuzeon® 05/01/2004 N/A Enbrel® 01/15/2003 N/A Hizentra® 02/15/2011 N/A Vivaglobin® 04/15/2007 N/A Copaxone® 05/01/2004 N/A Supprelin LA® 07/15/2006 N/A Firazyr® 07/31/2012 N/A Humalog®, Humulin®, Iletin®, Insulin Lispro®, Lantus®, Levemir®, NPH, Injection, insulin per J1815 Pork Insulin, Regular Insulin, 11/01/2003 N/A 5 units Ultralente®, Velosulin®, Humulin R®, Iletin II Regular Pork®, Insulin Purified Pork, A, B A, B A, B A, B A, B A, B A, B A, B A, B3 J1817 J1830 J2170 J2212 J2354 J2440 J2760 J2940 J2941 J3030 J3110 J3140 Relion®, Lente Iletin I®, Novolin R®, Humulin R U500® Humalog®, Humulin®, Insulin for Vesolin BR®, Iletin II NPH administration Pork®, Lispro-PFC®, through DME per 50 Novolin®, Novolog®, units (i.e. insulin Novolog Flexpen®, Novolog pump) Mix®, Relion Novolin® Injection interferon Betaseron® beta-1b, 0.25 mg Injection, Iplex®, Increlex® mecasermin, 1 mg Methylnaltrexone, Relistor* 0.1 mg Injection, ocetreotide, non-depot form for Sandostatin® sub-q or intravenous injection, 25 mcg Injection, papaverine N/A HCL, up to 60 mg Injection, Phentolamine Regitine* mesylate, up to to 5 mg Injection, somatrem, Protropin® 1 mg Humatrope®, Genotropin Nutropin®, Biotropin, Genotropin®, Genotropin Miniquick®, Injection somatropin, Norditropin®, Nutropin®, 1 mg Nutropin AQ®, Omnitrope®, Saizen®, Saizen Somatropin RDNA Origin®, Serostim®, Serostim RDNA Origin, Zorbtive® Injection sumatriptan Imitrex® succinate, 6 mg Injection, Forteo® teriparatide, 10 mcg Injection, testosterone suspension , up to 50 A, B3 01/15/2003 N/A 01/15/2003 N/A 04/15/2007 N/A 09/30/2013 N/A B, C A, B A, B B 10/15/2005 N/A 11/01/2003 N/A A, B A, B 09/30/2013 N/A 01/15/2003 N/A B, C B, C 01/15/2003 N/A 01/15/2003 N/A 11/01/2003 N/A 10/15/2005 N/A A, B B A, B mg Injection, testosterone J3150 propionate, up to 100 mg Injection, Metrodin®, Bravelle®, J3355 urofollitropin, 75 IU Fertinex® J34902 Unclassified Drugs Liraglutide GLP-1, Victoza® J34902 Unclassified Drugs Trimix J34902 Unclassified Drugs Tesamorelin acetate J34902 Unclassified Drugs Methylnaltrexone bromide J34902 Unclassified Drugs exanatide (Byetta®), variable Kynamro* (mipomersen J34902 Unclassified Drugs sodium) Peginterferon alfa-2b J34902 Unclassified Drugs (Sylatron™) pramlintide acetate (Symlin®), J34902 Unclassified Drugs variable Unclassified Simponi*-anti-TNF J35902 Biologics (Golimumab) Unclassified J35902 anakinra (Kineret®), variable Biologics Unclassified efalizumab (Raptiva®), J35902 Biologics variable Unclassified peginterferon, alfa-2a J35902 Biologics (Pegasys®), variable Unclassified Peginterferon, alfa-2b (PegJ35902 Biologics Intron®), variable Unclassified pegvisomant (Somavert®), J35902 Biologics variable Unclassified J35902 Abatacept (Orencia®) Biologics Injection, interferon J9212 alfacon-1, Infergen® recombinant, 1 mcg Injection, interferon, J9213 alfa-2a, recombinant, Roferon-A® 3 million units Injection, interferon J9216 gamma-1b, 3 million Actimmune® units Leuprolide acetate, J9218 Lupron® per 1 mg A, B 10/15/2005 N/A 04/15/2007 N/A 09/30/2013 N/A 09/30/2013 N/A 09/30/2013 N/A 09/30/2013 N/A 04/01/2006 N/A 06/26/2013 N/A 06/26/2013 N/A 04/01/2006 N/A 09/30/2013 N/A 10/15/2005 N/A 05/01/2004 N/A 05/01/2005 N/A 11/01/2003 N/A 05/01/2004 N/A 9/30/2013 N/A A, B A, B A, B A, B A, B A, B A, B A, B A, B A, B A, B B, C A, B B, C A, B A, B B, C 11/01/2003 N/A B, C 11/01/2003 N/A B, C 01/15/2003 N/A 01/15/2003 N/A A, B Injection, sermorelin A, B 04/15/2007 N/A acetate, 1 mcg Injection, interferon A, B Q3025 beta-1a, 11 mcg for Avonex®, Rebif® 10/20/2010 N/A IM use 1 Key for basis for the decision “Usually Self-Administered”. A Excluded as "apparent on its face" Excluded based on predominant use(s) being chronic or recurrent, identifiable by the B patient and provided long-term and by self-administration C Excluded based on detailed review of Medicare claims data 2 These are non specific codes. Providers are reminded that no form of insulin, regardless of route of administration including intravenous, intramuscular, subcutaneous, or inhalation, is 3 reimbursable by Medicare. [This includes J8499: Insulin, inhaled (Exubera®), variable.] Q0515 If a beneficiary's claim for a particular drug is denied because the drug is subject to the “selfadministered drug exclusion,” the beneficiary may appeal the denial. Because it is a “benefit category” denial and not a denial based on medical necessity, an Advance Beneficiary Notice of Non-coverage (ABN) is not required. A “benefit category” denial (i.e., a denial based on the fact that there is no benefit category under which the drug may be covered) does not trigger the financial liability protection provisions of Limitation On Liability [under Section 1879 of the Act]. Therefore, physicians or providers may charge the beneficiary for such an excluded drug. Provider and Physician Appeals The hospital and a physician accepting assignment may appeal a denial under the provisions found in the IOM Medicare Claims Processing Manual, Publication 100-04, Chapter 29, Section 200 at http://www.cms.gov/Regulations-andGuidance/Guidance/Manuals/Downloads/clm104c29.pdf . Reasonable and Necessary Noridian will make the determination of reasonable and necessary with respect to the medical appropriateness of the drug to treat the patient’s condition and will continue to make the determination of whether the intravenous or injection form of a drug is appropriate, as opposed to the oral form. We will also continue to make the determination as to whether a physician’s office visit was reasonable and necessary. However, while a physician’s office visit may not be reasonable and necessary in a specific situation, the medical necessity of the injection will still be determined on its own merits based on this process for determining which drugs are usually selfadministered. Sources: IOM Medicare Benefit Policy Manual, Publication100-02, Chapter 15, Covered Medical and Other Health Services, Section 50.2, Determining Self-Administration of Drug or Biological; Transmittal 123, CR 6950 dated April 30, 2010 Revision History 10/08/2013 - The article is being revised to include the CMS determination that each of the drugs: abatacept and golimumab, when used as a medically necessary intravenous infusion incident to a physician’s service, and the drug certolizumab, when used as a medically R2 necessary injection in its lyophilized form incident to a physician’s service, are not to be considered usually self-administered. Coding instructions to document these situations are included with an effective date of 12/01/2013. 09/30/2013 - The article is being revised to remove the code for the intravenous formulation of abatacept (Orencia) described by J0129 effective 09/30/2013. The subcutaneous R1 formulation, currently described by the code J3590, is substituted with the effective date of 09/30/2013. Last Updated: October 25, 2013