* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download ACALCULOUS CHOLECYSTITIS IN 14
Survey
Document related concepts
Transcript
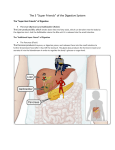
The West London Medical Journal 2010 Vol 2 No 2 pp 11- 14 ACALCULOUS CHOLECYSTITIS IN 14-YEAR OLD BOY WITH NO PREDISPOSING FACTORS Amanda Shreders[1], Colin Michie[2] ABSTRACT The natural history of cholecystitis varies with the age and sex of the patient. This condition most commonly presents in adult women with cholesterol gallstones in the cystic duct. In men the condition is usually acalculous without obvious stone, but it tends to follow another illness. Cholecysitis is very uncommon in children and is usually acalculous (1,2,3). We present a case of acalculous cholecystitis (AC) that was atypical in that no antecedent abnormality was identified. Financial Declarations: none Keywords: acalculous, paediatric, cholecystitis, adolescent abdominal pain CASE REPORT A 14 year old boy presented with a sharp non-radiating pain in the right upper quadrant. He had no chronic medical problems nor preceding illness. His neonatal course had been smooth; his birth weight at term was approximately 3 kg. There were two hospital admissions in early childhood for unrelated minor surgical procedures. There was no family history of jaundice, haemolysis, gallbladder disease or dyslipidemia. He was not receiving any medications and had no history of allergy or adverse drug reactions. On examination he was pyrexial. There was no anaemia or jaundice, clubbing or dysmorphic features. He weighed 57.0 kg and was 162.0 cm tall (BMI 21.7, 75th centile for age). The cardiovascular and respiratory systems were normal. There was guarding in the right upper quadrant with a positive Murphy sign and no rebound tenderness. A rectal examination was not carried out. There was no abdominal distension, no palpable masses and bowel sounds were normal. The skin and mucosae were healthy, his hair and nails unremarkable. 1 2 St Matthews University, Florida, USA. Department of Paediatrics, Ealing Hospital NHS Trust 11 THE WEST LONDON MEDICAL JOURNAL 2010 2, 2 An abdominal CT scan showed a mildly distended gallbladder with a thickened wall measuring 6 mm, consistent with cholecystitis. There was no bile duct dilation and the pancreas and kidneys were normal. Abdominal ultrasound scan confirmed these findings; no gallstones were identified. Blood results for this patient showed an elevated C-reactive protein throughout admission ranging from 176 mg/L on admission to a peak on day three at 384 mg/L. The white cell count was raised at 15 x10^9 on admission, 20.5 x10^9 on day 3 (a neutrophilia), and blood cultures remained negative. Routine electrolytes, bilirubin, alkaline phosphatase, and liver transaminases were all normal. Haemolysis was excluded by the normal hemoglobin, red blood cell indices and blood film. A diagnosis of acalculous cholecystitis (AC) was made; treatment with intravenous cefuroxime and metronidazole was initiated. Gentamicin was substituted on day three because of the persistent high white count and CRP. Following this change in antibiotics the patient improved rapidly; he was discharged on day seven for outpatient follow-up. He has received an elective laparoscopic cholecystectomy. A year after surgery he remains well with no further episodes of abdominal pain; his routine blood investigations remain within the normal range. DISCUSSION Cholecystitis or inflammation of the gallbladder is most commonly secondary to a gallstone that obstructs the outflow of bile into the common bile duct and gives rise to distention of the gallbladder (1). Resultant decrease in blood flow and lymphatic drainage is thought to cause ischemia and inflammation in the gall bladder, both of which further distend the gallbladder. Bile stasis from outflow obstruction can also lead to ascending bacterial infection, most frequently from Escherichia coli. Gallstones form following supersaturation of the bile with cholesterol. This situation may arise in conditions of high cholesterol intake, obesity, hypo-secretion of bile acids or phospholipids, decreased gall bladder motility or a combination or these (4,5,6). Pathologies of red cells leading to increased fragility and turnover are associated with the development of pigment gallstones. Crohn’s disease patients have an increased prevalence of gallstones due to terminal ileum disease and changes in enterohepatic circulation (7). A combination of a decreased bile acid pool, multiple surgical procedures and chronic illness may predispose patients to gallstone formation. Cholecystitis may also occur in the absence of stones, as first described in adults in 1844 and in some detail in children in 1966 (3). Some 6-17% of cholecystectomies show no gallstones on examination. Acute acalculous cholecystitis (ACC) carries a higher mortality rate as it is oftern follows a sepsis syndrome, burns, trauma, ventilation or prolonged use of narcotic pain medication. Total parenteral nutrition, dehydration, infections including hepatitis, Salmonella typhi, threadworm infections and malaria have been 12 ACALCULOUS CHOLECYSTITIS IN 14-YEAR OLD BOY WITH NO PREDISPOSING FACTORS specifically documented as a cause of acalculous cholecystitis. Mesenteric lymphadentitis leading to possible reactive hyperplasia of the cystic duct may initiate cholecystitis leading to initiate obstruction of bile flow. Chronic AC may result from a functional defect of the gall bladder causing bile stasis (69). Congenital malformations of the gallbladder must also be considered in the diagnosis of abdominal pain at any age. The gallbladder develops from a bud of the duodenum that gives rise to the gallbladder and cystic duct (10). Disruption of this process causes malformed gallbladders. Anomalies include double gallbladders, multiseptate gallbladders, vestigial or absent gallbladder. Multiseptate gallbladders are thought to occur from an arrest in the solid stage of development; these in particular may be related to non-specific abdominal pain (11). The majority of such anomalies show no syndromic association. Abdominal ultrasound and abdominal computed tomography may both be employed to evaluate adolescents with abdominal pain. Other imaging techniques such as oral cholecystography, cholescintigraphy, and magnetic resonance cholangioraphy are used prior to surgery to identify or exclude speicfic gallbladder anomalies (11). Scintigraphy is considered positive for cholecystitis when the gallbladder is not visualized one hour after injection of technitium-99; this suggests there is an obstruction of flow preventing bile entering or leaving the gallbladder. Regardless of age or cause, the mainstay of current treatment remains percutaneous cholecystectomy, together with systemic parenteral antibiotics. CONCLUSION The great majority of acalculous cholecystitis in children is related to acute or chronic illness. The case reported here is unusual in that no such association was identified. Gallbladder disorders should always be carefully excluded in adolescents suffering abdominal pain. Acknowledgements The authors would like to thank Dr. Donald Bentley for his helpful review of the script. REFERENCES [1] Holcomb GW, Jr, O’Neill, JA Jr. Cholecystitis, Cholelithiasis and Common Duct Stenosis in Children and Adolescents. Annals of Surgery 1980; 191: 626-635. [2] Rankin W. Acute Distention of the Gall Bladder in Children. Archives of Disease in Childhood 1955; 30:60-61. 13 THE WEST LONDON MEDICAL JOURNAL 2010 2, 2 [3] Bloom RA, Swain VA. Non-calculous distention of the gall-bladder in childhood. Archives of Disease in Childhood 1966; 41: 503-508. [4] Soderlund S, Zetterstrom B. Cholecystitis and Cholelithiasis in Children. Archives of Disease in Childhood 1962; 37:174-180. [5] Walker C. Aetiology of Cholelithiasis in Childhood. Archives of Disease in Childhood 1957; 32: 293-297. [6] Attilakos A, Prassouli A, Hadjigerogiou G, et. al. Acute acalculous cholecystitis in children with Epstein-Barr virus infection: a role for Gilbert’s syndrome? International Journal of Infectious Diseases 2009; 13: 161-164. [7] Hutchinson R, Tyrell PNM, Kumar D, et.al. Pathogenesis of gall stones in Crohn’s disease: an alternative explanation. Gut 1994; 35: 94-97. [8] Kumar A, Taksande A, Vilhekar KY. Acalculous cholecystitis by P. falciparum in a 3-year old child. Journal of Vector Borne Disease 2008; 45: 76-77. [9] Dowling RH. Review: Pathogenesis of gallstones. Alimentary Pharmacology and Therapeutics 2000; 14 (Suppl. 2): 39-47. [10] Rabinovitch J, Rabinovitch P, Rosenblatt P, Pines B. Congenital Anomalies of the Gallbladder. Annals of Surgery 1958; 145:161-168. [11] Patel N, Joshipura V, Haribhakti S, Soni H. Septate gallbladder in the laparoscopic era. Journal of Minimal Access Surgery 2008; 4:20-22. 14