* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Management of Medication Induced Xerostomia An Evidence Based
Survey
Document related concepts
Transcript
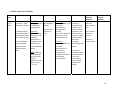
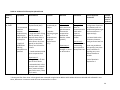
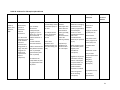
Management of Medication Induced Xerostomia An Evidence Based Report Kevin Chung, BSc* Payam Fakhri, B.ASc M.ASc* Larisa Naderiani, H.BSc* Adeela Nematullah, BHSc* Parastoo Salehi, H.BSc* * From the Faculty of Dentistry, University of Toronto, Toronto, Canada Key words: xerostomia, sialogogue, Salagen, anethole trithione, yohimbine, pilocarpine Abstract Purpose: To evaluate the evidence for saliva stimulants in the management of medication induced xerostomia. Methods: Data sources included MEDLINE, EMBASE, PubMed databases, All EBM Reviews, manual citation review of the relevant literature and content experts. Study selection and data extraction were carried out independently by at least two reviewers, with differences resolved by consensus. Eligible studies were clinical trials that evaluated the effects of saliva stimulants in patients with medication induced xerostomia. Results: Eight trials met the inclusion criteria: pilocarpine (n=4), yohimbine (n=2), anethole trithione (n=1) and 1 additional study comparing yohimbine and anethole trithione. Compared to no treatment or standard care, administration of saliva stimulants was associated with an increase in salivary flow rate and/or patient reported improvement in symptoms. Conclusion: There is evidence to support the use of saliva stimulants in the management of medication induced xerostomia. There is level A, grade I evidence to support the use of yohimbine, level B, grade II-1 evidence to support anethole trithione, and level B, grade II-1 evidence to support the use of pilocarpine in the management of medication induced xerostomia. 2 Xerostomia is defined as a subjective complaint of dry mouth.1 It is usually, but not always, associated with altered salivary quantity and/or quality. Dry mouth can be caused by the destruction of the salivary glands from radiotherapy to the head and neck region or by an autoimmune disease known as Sjogren’s syndrome. However, the most common cause of xerostomia is from the use of xerostomic drugs.2 Studies have shown that xerostomia affects 10-29% of the population.1-4 This increases in patients receiving palliative care and hospitalized patients to 30% and 77% respectively.2 Furthermore, the burden of illness is increasing due to the aging population. More than 500 medications are known to cause xerostomia.5 Drugs with anticholingergic or sympathomimetic effects are most commonly associated with dry mouth. This includes tricyclic antidepressants, antipsychotics, benzodiazepines, atropinics, β-blockers, and antihistamines.5 Establishing a relative risk for xerostomia as a result of a particular medication is difficult due to other contributing factors such as severity of concomitant adverse reactions, the pathophysiology of the disorder being treated and the dose of medication. Regardless, it has been established that the risk of xerostomia increases with the number of medications being taken. 3 Saliva is important for overall oral health and contributes to a person’s quality of life. The average person has an unstimulated/resting flow rate of 0.3 mL/min, and a stimulated flow rate of 4.0-5.0 mL/min.5 It is estimated that a 50% decrease in saliva needs to occur for xerostomia to become apparent.1 Xerostomic patients are more susceptible to rampant dental caries, frequent mucosal infections, and have difficulties in chewing and swallowing. They also have altered taste sensation, coughing episodes, voice disturbances, and speech difficulties.5 Treatment options for medication induced xerostomia include saliva substitutes, saliva stimulants, and acupuncture.1 This paper will focus on the array of saliva stimulants currently 3 available. There are numerous reports in the literature regarding the use of saliva stimulants in patients with xerostomia due to other etiologies. Furthermore, it was hypothesized that saliva stimulants would be effective in treating medication induced xerostomia because the afflicted patients have intact salivary glands, unlike xerostomic patients due to other etiologies (radiation induced xerotomia, Sjogren’s syndrome). The saliva stimulants commonly reported in the literature are pilocarpine, yohimbine, anethole trithione (AT), and chewing gums. Pilocarpine, a tertiary amine, is a non-selective muscarinic agonist with a mild β-adrenergic effect on salivary glands.6 Yohimbine, an indole alkaloid, is a selective α2-adrenergic antagonist. Anethole trithione, a bile secretion-stimulating drug, is a cholagogue that increases the availability of muscarinic receptors on the postsynaptic membrane of certain cells including salivary glands.5 Finally, chewing gums are a non pharmacological treatment that has been shown to physiologically stimulate salivary secretion in xerostomic patients.7 The purpose of this paper is to determine the evidence that support the use of saliva stimulants in the management of medication induced xerostomia from the perspective of a practicing dentist. Methods: Data Sources We attempted to identify all published studies assessing saliva stimulants in the management of medication-induced xerostomia. We searched the MEDLINE database (1990 to January, 2008), the EMBASE database (1990 to January, 2008) and All EBM Reviews (Cochrane DSR, ACP Journal Club, DARE, CCTR, CMR, HTA, NHSEED (from inception to 4 January, 2008)). The search strategy is shown in Appendix 1, and was supplemented by manual review of reference lists, as well as contacting content experts. The Canadian Dental Association and Ontario Dental Association websites were also search to identify clinical practice guidelines. The search strategy shown in Appendix 1 was also executed in PubMed. However, due to variations in indexing, the same search strategy resulted in over 200 000 articles. We felt that it was necessary to search PubMed in order to ensure the comprehensiveness of our search. Hence we executed a simpler search using the following keywords: xerostomia, pilocarpine, Salagen, anethole trithione, Evoxac, yohimbine. The search was limited to years 1990-2008 and to clinical trials. Study Selection Study selection was performed independently by two reviewers (PS, LN) at 3 stages: title & abstract, full text screening using PICO-C, and quality assessment. All disagreements were resolved by consensus. A study was included if it was a clinical trial, in humans, assessing a saliva stimulant therapy for medication induced xerostomia, and it assessed at least one of the following outcomes: stimulated or non-stimulated salivary flow rates (i.e., SSFR or NSFR, respectively) and/or patient reported improvement in dry mouth symptoms (visual analogue scale or VAS for example). Studies were excluded if they did not have at least one arm including patients with medication induced xerostomia or if they did not test a saliva stimulant. Although the search strategy employed excluded non-English sources, at the full text review stage it was again necessary to exclude studies of non-English origin that had only translated abstracts. Furthermore, studies that were not locally accessible through University of Toronto libraries were excluded (Figure 1). 5 Study Data Extraction For each study, three reviewers (AN, LN, PS) independently extracted data on study design, patient characteristics, therapeutic interventions and the following clinical outcomes: stimulated or non-stimulated salivary flow rate or patient reported improvement in symptoms. This data extraction was guided by a PICO-C form (Figure 2). In studies with multiple arms, data extraction was completed only on the control arm and the medication-induced xerostomia arm, where possible. Disagreements regarding data extraction were resolved by consensus and discussion with a forth reviewer (PF). Study Quality Assessment Two reviewers (PS, LN) independently assessed the quality of the included trials using the “Checklist to assess evidence of efficacy of therapy or prevention”, developed based on multiple adaptation sources 8 (see sample in Figure 3). The maximum possible checklist score was 17. It was decided that studies receiving a score below 8.5 would be excluded. Additionally, each study was classified and graded according to the Canadian Task Force for Preventive Health Care (CTF PHC)levels of evidence by two independent reviewers (LN, PS). Any disagreements regarding study quality were resolved by consensus among reviewers. Study Analysis Results from randomized controlled trials were considered to determine the Relative Risk (RR) and the Number Needed to Treat (NNT) where possible. Results: Data Sources & Study Selection The search strategy employed, identified 866 potential articles relevant to the aforementioned keywords: 840 from Ovid Medline and 26 in PubMed. Completion of title and 6 abstract review according to the aforementioned inclusion/exclusion criteria yielded 55 relevant articles. Study Data Extraction Articles deemed relevant from the previous stage (55) were pooled into a custom inclusion/exclusion database and accessed in full text to apply PICO-C analysis. Upon removal of duplicates (3), inaccessible sources (12), non-English full texts (4), studies which were not clinical in nature (9), and studies with incompatible patient populations (13), 14 sources progressed to the quality assessment stage. Reference lists of these full text articles were also reviewed for relevant sources. One study progressed to quality assessment from this search. All gum-based interventions were eliminated at this stage, since data could not be extracted specific to medication-induced xerostomic patients. As such, data could not be proven significant for this group independent of others. Reason for exclusion is tabulated in Table 1. Study Quality Assessment At this stage, 15 studies were subjected to the checklist analysis and CTF PHC grading. Only 8 articles scored above the previously established cut off (8.5). Study Analysis Unfortunately, quantitative measures could not be calculated based on the limited results reported in the aforementioned studies. Attempts to contact authors for additional information were not fruitful at the time of this report, at least not in the time limitations imposed. Compilation of Evidence Tables Consequently, three treatment approaches were identified for further analysis: AT, yohimbine, and pilocarpine. Each treatment strategy yielded the following number of relevant 7 articles: AT (1), yohimbine (2), pilocarpine (4), with 1 additional study addressing both yohimbine and AT in a comparative nature (1). Anethole Trithione: One study received the highest level of evidence and the CTF PHC grade ascertained was A-I, reflecting a true randomized control trial. 9 The other study yielded a lower score (B-II, 1) primarily due to its incomplete blinding technique and inappropriate use of randomization. 11 The randomization scheme was inadequate as patients were randomly assigned to treatment and control groups by the DDS following a complete exam. Furthermore, AT dosage was not specified in milligrams, only noted to be “one tablet”. Between the two studies, there was conflicting evidence: Bagheri et al. 9 showed no significant increase in NSFR after 5 days while Hamada et al. 11 showed marked increase after 14 days. However, since dosage was not specified in the study by Hamada et al. 11, it may have been a confounding factor so a long term versus short term effect could not be established based on these results alone. Yohimbine: All of the three studies included for the yohimbine intervention were randomized control trials that yielded unanimous CTF PHC scores of A-I. Furthermore, the xerostomic drugs prescribed in all three studies were of a psychiatric nature (major depressive disorder and/or psychoses). In general, acute administration of 10 mg yohimbine yielded a significant increase of NSFR. 12,13 However, variable types and levels of adverse effects were reported by each. Isolated evidence exists to suggest acute low doses of yohimbine (4mg) increased NSFR significantly as well, but was not collaborated by the other studies. Likewise, Bagheri et al. 9 found that a more chronic yohimbine administration regime (3x6mg/day for 5 days) did increase 8 NSFR over a 5 day span but this result was not corroborated. With all studies, minor issues in methodological quality existed, as discussed further. Pilocarpine: The highest level of evidence and CTF PHC grade merited by these studies was B II-1, mainly due to lack of randomization and/or incomplete blinding. 2, 4, 14 Two studies used a single acute dose of 5mg 4, 14, while 2 studies used a more chronic dose of 5mg TID for 7 and 14 days. 2, 3 Both acute and chronic doses resulted in short term improvement of xerostomia symptoms as measured by VAS scales 2, 3 and salivary flow rates. 4, 14 Only two of the four articles considered long term effects following chronic dosing. One study2 tested for long terms effects over 5 weeks and found no significant increase in salivary flow rates. In contrast, another study suggested a prolonged effect after a 1 week observation period. 3 The lowest grade was assigned to Mercadante et al.3 due to lack of randomization and blinding. Of the three studies that reported adverse effects, presentation, duration, and severity were too variable to draw comparisons across studies. 2, 3, 4 With all studies, minor issues of in methodological quality existed, and will be further considered in the subsequent section. Discussion: This evidence based report demonstrates that there is good/fair evidence in the published literature for saliva stimulants in the management of medication induced xerostomia. Our findings are consistent with previous reports of promising results of these medications in patients with radiation induced xerostomia and in patients with Sjogren’s syndrome. Our review of the literature shows that there is good evidence for the use of yohimbine, and fair evidence for pilocarpine and anethole trithione in the management of medication induced xersotmia. While all the aforementioned treatments were found to be effective in the short term, one study supports 9 the use of anethole trithione as a long term treatment to alleviate the symptoms of medication induced xerostomia. This, however, warrants further study. Also, as previously mentioned, we attempted to include chewing gums as saliva substitutes due to their physiological effects. However, the three studies on chewing gums identified in our review of titles and abstracts included xerostomic patients due to numerous etiologies and it was not possible to extract data specifically for medication-induced xerostomia patients. Hence, these studies were excluded. Our results demonstrate that saliva stimulants are in fact a useful and promising therapy in patients with medication induced xerostomia. The validity of this finding is supported by the following considerations. Firstly, there was remarkable consistency across studies. All patients who received saliva stimulants improved and this treatment effect was statistically significant and therefore not due to chance. It is important to differentiate between statistical and clinical significance. Improvement was observed in not only subjective but also objective measures indicating that these results were not only statistically significant but were also clinically important. As previously discussed there were some methodological issues and threats to internal validity in the included studies. Only 4 studies were described as randomized. In many instances the randomization sequence was not described and therefore the adequacy of randomization could not be ascertained. In one instance where the randomization sequence was described as a dentist ‘randomly’ allocating patients to treatment and control groups, the randomization sequence was not considered adequate. Furthermore, none of the included studies compared treatment and control groups with regards to prognostic factors prior to the start of the study. Only 2 out of 8 studies were described as double blinded. Therefore bias and the placebo effect likely influenced the results. Furthermore, only 4 out of 8 studies reported complete follow-up or a loss to follow-up of less than 20%. Unfortunately, none of the studies reported adequate data to 10 facilitate the calculation of a relative risk or odds ratio. Therefore, although the treatment effect was reportedly beyond chance, the size and precision was the treatment effect could not be determined. Despite the methodological shortcomings, we feel that the results from these studies are largely valid. In addition, these results are generalizable. Most of the studies included in our evidence-based report were conducted in University/Hospital settings. However, given the condition, it is likely that patients suffering from medication induced xerostomia seeking care in a University/Hospital setting are likely similar to patients seeking care for the same condition in a private practice setting. Furthermore, a majority of the included studies considered other clinically relevant outcomes, namely adverse effects of the medications. In most cases, these adverse effects were minor, the most common adverse effect being sweating. Some studies reported a small number of patients dropping out due to these adverse effects. Due to the rarity of this loss, it was not considered to be a threat to external validity. Another important consideration in evaluating the external validity or generalizability of these findings is whether the likely treatment benefits are worth the potential harms and costs. It is conceivable that many patients may be opposed to taking more medication to alleviate the symptoms of medications that they are currently receiving. Many patients may opt for more conservative treatment options to alleviate their symptoms, for example, saliva substitutes or sugarless candies. While, the ultimate decision-maker is the patient, it is our responsibility as health-care providers to outline all the potential options available. As our evidence-based report demonstrates, saliva substitutes, namely pilocarpine, yohimbine and anethole trithione are viable options in the management of medication induced xerostomia. In fact these medications may be a foremost choice in patients in long term care facilities, who receive limited attention from 11 caregivers, or patients with trisumus who are unable to chew gums or rinse their mouth with saliva substitutes or patients with severe symptoms that are not responsive to more conservative treatment options. Some other potential weaknesses of our evidence based report are as follows. First, we searched only the English language literature. However, there is some debate regarding the degree of bias introduced by the exclusion of non-English literature. A study of a number of disease areas has shown that language restricted meta-analyses, compared to language inclusive meta-analyses, does not differ with respect to the estimate of benefit of the effectiveness of an intervention. 15 Furthermore, we did not search the grey’s literature. Thus although we did not formally conduct a funnel plot analysis, some, however small, element of publication bias is likely. Also numerous sources of heterogeneity existed in our included studies. These ranged from the definition of xerostomia, to the outcomes assessed: subjective (salivary flow) or objective (patient reported improvement in symptoms). For this reason we did not combine results across studies through a meta-analysis. Furthermore, comparisons between the different saliva stimulants could not be made and therefore, and therefore the ‘best’ saliva stimulant, if it exists, could not be determined. Our report demonstrates that evidence for the use of saliva stimulants in the management of medication induced xerostomia ranges from fair to good based on the CTF PHC. There is level A, grade I evidence to support the use of yohimbine, level B, grade II-1 evidence to support anethole trithione, and level B, grade II-1 evidence to support the use of pilocarpine in the management of medication induced xerostomia. There is some support in the literature for long term effects of anethole trithione; however, this requires further investigation. Unfortunately, no 12 conclusions could be made on the effectiveness of chewing gums. Further evidence from randomized controlled trials is needed to establish relative risk reduction. 13 References: 1. Guggenheimer, J., & Moore, P. A. (2003). Xerostomia: Etiology, recognition and treatment. The Journal of the American Dental Association, 134(1), 61-69. 2. Davies, A. N., Daniels, C., Pugh, R., & Sharma, K. (1998). A comparison of artificial saliva and pilocarpine in the management of xerostomia in patients with advanced cancer. Palliative Medicine, 12(2), 105-111. 3. Mercadante, S., Calderone, L., Villari, P., Serretta, R., Sapio, M., Casuccio, A., et al. (2000). The use of pilocarpine in opioid-induced xerostomia. Palliative Medicine, 14(6), 529-531. 4. Aframian, D. J., Helcer, M., Livni, D., Robinson, S. D., Markitziu, A., & Nadler, C. (2007). Pilocarpine treatment in a mixed cohort of xerostomic patients. Oral Diseases, 13(1), 88-92. 5. Porter, S. R., Scully, C., & Hegarty, A. M. (2004). An Update of the Etiology and Management of Xerostomia. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontics, 97(1), 28-46. 6. Ferguson, M. M. (1993). Pilocarpine and Other Cholinergic Drugs in the Management of Salivary Gland Dysfunction. Oral Surgery, Oral Medicine, Oral Pathology. 75(2), 186191. 7. Aagaard, A., Godiksen, S., Teglers, P. T., Schiodt, M., & Glenert, U. (1992). Comparison between new saliva stimulants in patients with dry mouth: A placebo-controlled doubleblind crossover study. Journal of Oral Pathology & Medicine, 21(8), 376-380. 8. Leake, J., Checklist to assess evidence of efficacy of therapy or prevention. 2006, Faculty of Dentistry, University of Toronto. Unpublished document. Course notes DENT 300Y 14 2007. Adapted from Fletcher RH, Fletcher SW, Wanger EH. Clinical Epidemiology: The essentials. Third edition. Baltimor: Williams and Wilkens, 1996; and Sackett DL, Richardson WS, Rosenburg W, Haynes RB. Evidence-based medicine: How to practice and teach WBM. Second edition. New York: Churchill Livingstone, 1997. 9. Canadian Task Force for Preventive Health Care, http://www.ctfphc.org/, 2008. 10. Bagheri, H., Schmitt, L., Berlan, M., & Montastruc, J. L. (1997). A comparative study of the effects of yohimbine and anetholtrithione on salivary secretion in depressed patients treated with psychotropic drugs. European Journal of Clinical Pharmacology, 52(5), 339-342. 11. Hamada, T., Nakane, T., Kimura, T., Arisawa, K., Yoneda, K., Yamamoto, T., et al. (1999). Treatment of xerostomia with the bile secretion-stimulating drug anethole trithione: A clinical trial. American Journal of the Medical Sciences, 318(3), 146-151. 12. Bagheri, H., Picault, P., Schmitt, L., Houin, G., Berlan, M., & Montastruc, J. L. (1994). Pharmacokinetic study of yohimbine and its pharmacodynamic effects on salivary secretion in patients treated with tricyclic antidepressants. British Journal of Clinical Pharmacology, 37(1), 93-96. 13. Bagheri, H., Schmitt, L., Berlan, M., & Montastruc, J. L. (1992). Effect of 3 weeks treatment with yohimbine on salivary secretion in healthy volunteers and in depressed patients treated with tricyclic antidepressants. British Journal of Clinical Pharmacology, 34(6), 555-558. 15 14. Alajbeg, I., Hladki, N., Alajbeg, I. Z., Rosin-Grget, K., Vucicevic-Boras, V., & CekicArambasin, A. (2005). The treatment effects of pilocarpine in patients with xerostomia. Periodicum Biologorum, 107(2), 201-206. 15. Moher, D.P., B. Klassen, T. Schulz, K. Berlin, J. AR, J. et al., What contributions do languages other than English make on the results of meta-analyses? Journal of Clinical Epidemiology, 2000. 53(9): p. 964-72. 16. Aagaard A, G. U. (1991). Comparison between new saliva stimulants in patients with xerostomia (IADR abstract 1991). Journal of Dental Research, 70(Special Issue/Abstracts):407 (Abs 1134) 17. Abelson, D. C., Barton, J., & Mandel, I. D. (1990). The effect of chewing sorbitolsweetened gum on salivary flow and cemental plaque pH in subjects with low salivary flow. Journal of Clinical Dentistry, 2(1), 3-5. 18. Allen, J., & L.V. (1993). Pilocarpine oral solution. U.S.Pharmacist, 18(10), 136-137146. 19. Banoczy, J., Dombi, C., Czegledly, A., & Sari, K. (1994). A clinical study with lactoperoxidase-containing gel and toothpaste in patients with dry mouth syndrome. Journal of Clinical Dentistry, 5(3), 65-69. 20. Bernardi, R., Perin, C., Becker, F. L., Ramos, G. Z., Gheno, G. Z., Lopes, L. R., et al. (2002). Effect of pilocarpine mouthwash on salivary flow. Brazilian Journal of Medical & Biological Research, 35(1), 105-110. 21. Bjornstrom, M., Axell, T., & Birkhed, D. (1990). Comparison between saliva stimulants and saliva substitutes in patients with symptoms related to dry mouth. A multi-centre study. Swedish Dental Journal, 14(4), 153-161. 16 22. Butt, G. M. (1991). Drug-induced xerostomia. Journal (Canadian Dental Association), 57(5), 391-393. 23. Cevimeline (evoxac) for dry mouth.(2000). Medical Letter on Drugs & Therapeutics, 42(1084), 70. 24. Chambers Toth, B. B., Keene, H. J., & Martin, C. G. (1998). Assessment of salivary flow and functional improvement in cancer patients with oral pilocarpine as treatment for analgesia-induced xerostomia. (AADR abstract). Journal of Dental Research, 77(S 1 A.), 290. 25. Chambers, M., Martin, C., Toth, B., Payne, R., Muscoplat, C., Shrotriya, R., et al. (1997). Assessment of functional improvement in cancer patients with oral pilocarpine as treatment for analgesia-induced xerostomia. Supportive Care in Cancer, 5 Suppl, 164. 26. Chambers, M., Toth, B., Martin, C., Payne, R., Muscoplat, C., Gallagher, S., et al. (1997). Assessment of salivary flow improvement in cancer patients with oral pilocarpine as treatment for analgesia-induced xerostomia. Proc-Annu-Meet-Am-Soc-Clin-Oncol, 27. Chow, L. C., Takagi, S., Shern, R. J., Chow, T. H., Takagi, K. K., & Sieck, B. A. (1994). Effects on whole saliva of chewing gums containing calcium phosphates. Journal of Dental Research, 73(1), 26-32. 28. Feldman, R. S., Richter, R., Barnett, M., & Vincent, J. (1992). Sialogogue effects of sugar-free mint in medication-associated xerostomia (AADR abstract). Journal of Dental Research, 71(AADR Abstracts):163 (Abs 462) 17 29. Fox, P. C., Atkinson, J. C., Macynski, A. A., Wolff, A., Kung, D. S., Valdez, I. H., et al. (1991). Pilocarpine treatment of salivary gland hypofunction and dry mouth (xerostomia). Archives of Internal Medicine, 151(6), 1149-1152. 30. Hamada, T., Nakane, T., Kimura, T., Arisawa, K., Yoneda, K., Yamamoto, T., et al. (1999). Treatment of xerostomia with the bile secretion-stimulating drug anethole trithione: A clinical trial. American Journal of the Medical Sciences, 318(3), 146-151. 31. Hay, K. D., & Morton, R. P. (2003). The efficacy of casein phosphoprotein-calcium phosphate complex (DC-CP) [dentacal] as a mouth moistener in patients with severe xerostomia. New Zealand Dental Journal, 99(2), 46-48. 32. Kirstila, V., Lenander-Lumikari, M., Soderling, E., & Tenovuo, J. (1996). Effects of oral hygiene products containing lactoperoxidase, lysozyme, and lactoferrin on the composition of whole saliva and on subjective oral symptoms in patients with xerostomia. Acta Odontologica Scandinavica, 54(6), 391-397. 33. Lee, S. K., Chung, J. W., Lee, S. W., & Kho, H. S. (1995). The effect of pilocarpinecontaining chewing gum in xerostomia. (IADR abstract 1995). Journal of Dental Research, 74(Special Issue - Abstracts of Papers (73rd General Sessioand Exhibitioof the International Associatiofor Dental research June 28-July 1, 1995) Singapore)):576 (Abs 1403) 34. Lemaire, V. (1992). Pilocarpine in the treatment of dry mouth. [Traitement De La Secheresse Buccale Par La Pilocarpine.] Concours Medical, 114(9), 778. 18 35. Lokken, P., & Birkeland, J. M. (2005). Drugs and oral dryness. [Medikamenter og munntorrhet.] Tidsskrift for Den Norske Laegeforening, 125(5), 581-582. 36. Maeda, M., Araki, M., Fujisawa, T., Shibuya, Y., & Sugino, K. (2004). A trial of cevimeline hydrochloride (evoxac) for patients with sjogren's syndrome and dry mouth. Nishinihon Journal of Dermatology, 66(1), 48-52. 37. Masters, K. J. (2005). Pilocarpine treatment of xerostomia induced by psychoactive medications. American Journal of Psychiatry, 162(5), 1023. 38. Mercadante, S. (1998). Pilocarpine as an adjuvant to morphine therapy. Lancet, 351(9099), 338-339. 39. Morita, Y., Senami, M., Maruya, H., Urushibara, T., & Yasuda, M. (2004). Efficacy of oral balance gel for dry mouth in preoperative patients. Japanese Journal of Anesthesiology, 53(7), 772-776. 40. New approaches to preventing xerostomia.(2006). The Journal of Supportive Oncology, 4(2), 87-88. 41. Olsson, H., Spak, C. J., & Axell, T. (1991). The effect of a chewing gum on salivary secretion, oral mucosal friction, and the feeling of dry mouth in xerostomic patients. Acta Odontologica Scandinavica, 49(5), 273-279. 42. Oral pilocarpine for xerostomia.(1994). Medical Letter on Drugs & Therapeutics, 36(929), 76. 43. Pilocarpine adds to the range of treatment options in xerostomia.(1995). Drugs and Therapy Perspectives, 5(8), 5-7. 19 44. Rantanen, I., Pienihakkinen, K., Tenovuo, J., & Soderling, E. (2002). Betaine-containing toothpaste and subjective symptoms of dry mouth: A clinical study. (ORCA abstract). Caries Research, 36(3), 218. 45. Rantanen, I., Tenovuo, J., Pienihakkinen, K., & Soderling, E. (2003). Effects of a betaine-containing toothpaste on subjective symptoms of dry mouth: A randomized clinical trial. Journal of Contemporary Dental Practice [Electronic Resource], 4(2), 1123. 46. Risheim, H., & Arneberg, P. (1993). Salivary stimulation by chewing gum and lozenges in rheumatic patients with xerostomia. Scandinavian Journal of Dental Research, 101(1), 40-43. 47. Salah, R. S., & Cameron, O. G. (1996). Pilocarpine for anticholinergic adverse effects associated with desipramine treatment. American Journal of Psychiatry, 153(4), 579. 48. Shen, X. L., Wang, Z. C., & Xu, H. D. (1999). Pilocarpine in treating xerostomia caused by psychotropic drugs. Shanghai Psychological Medicine, 11(1), 21-22. 49. Shetty, K. (2005). Dentistry. clinic assesses effect of medication on dry mouth syndrome. HIV Clinician, 17(3), 11-14. 50. Ship, J. A. (2002). Diagnosing, managing, and preventing salivary gland disorders. Oral Diseases, 8(2), 77-89. 51. Silvestre Donar, F. J., Miralles Jorda, L., & Martinez Mihi, V. (2004). Protocol for the clinical management of dry mouth. [Tratamiento de la boca seca: Puesta al dia.] Medicina Oral, 9(4), 273-279. 20 52. Simons, D., Kidd, E. A., Beighton, D., & Jones, B. (1997). The effect of chlorhexidine/xylitol chewing-gum on cariogenic salivary microflora: A clinical trial in elderly patients. Caries Research, 31(2), 91-96. 53. Soderling, E., Le Bell, A., Kirstila, V., & Tenovuo, J. (1998). Betaine-containing toothpaste relieves subjective symptoms of dry mouth. Acta Odontologica Scandinavica, 56(2), 65-69. 54. Stewart, C. M., Jones, A. C., Bates, R. E., Sandow, P., Pink, F., & Stillwell, J. (1998). Comparison between saliva stimulants and a saliva substitute in patients with xerostomia and hyposalivation. Special Care in Dentistry, 18(4), 142-148. 55. Stone, P., & A'Hern, R. (1999). Artificial saliva versus pilocarpine for xerostomia. Palliative Medicine, 13(1), 81-83. 56. Sung, J. M., Kuo, S., Lee, S., Cheng, M., Guo, H., & Huang, J. (2002). A randomized, single-blind, placebo controlled, cross-over, study of oral pilocarpine for xerostomia and interdialytic weight gain in hemodialysis patients [abstract]. Nephrology Dialysis Transplantation, 17(Suppl 1), 271. 57. Taubert, M., Davies, E. M. R., & Back, I. (2007). Dry mouth. British Medical Journal, 334(7592), 534. 58. Tokiyasu, Y., Watanabe, S., Hirasawa, M., Suzuki, S., Fujita, K., Oda, M., et al. (1997). Effect of parasympathonimetic drugs on salivary flow rate. Oral Therapeutics and Pharmacology, 16(3), 126-130. 21 59. Valdez, I. H., & Fox, P. C. (1993). Diagnosis and management of salivary dysfunction. Critical Reviews in Oral Biology and Medicine, 4(3-4), 271-277. 60. Wang, Z. C., Shen, X. L., & Xu, H. D. (2000). A controlled clinical study of pilocarpine nitrate in the treatment of dry mouth caused by psychotropic drugs. Chinese Journal of Pharmacoepidemiology, 9(2), 59-60. 61. Watanabe, S., Hirasawa, M., Suzuki, A., Tokiyasu, Y., Suzuki, S., Fujita, K., et al. (1997). Evaluation of solid disperations of pilocarpine hydrochloride for salivary flow rate. Oral Therapeutics and Pharmacology, 16(3), 131-136. 62. Wynn, R. L., & Meiller, T. F. (2000). Artificial saliva products and drugs to treat xerostomia. General Dentistry, 48(6), 630-636. 22 Table 1. Excluded studies and reasons for exclusion. Author, Date Reason for Exclusion Ref. number Aagaard, A. et al., 1991 Can't locate 16 Aagaard,A. et al., 1992 Didn't have a cohort of patients with medication induced xerostomia 7 Abelson,D.C. et al., 1990 Didn't have a cohort of patients with medication induced xerostomia 17 Allen,Jr. et al., 1993 Not a study 18 Banoczy,J. et al., 1994 Pop= oral lichen planus 19 Bernardi,R. et al., 2002 Healthy pop 20 Bjornstrom,M. et al., 1990 Pharmacological but includes pts with non-med--cannot extract data on just med induced 21 Butt,G.M.,1991 Not a study 22 Chambers Toth,B.B. et al., 1998 Just an abstract 24 Chambers,M. et al., 1997 Can't locate 25 Chambers,M. et al., 1997 Duplicate 26 Chow,L.C. et al., 1998 Not xerstomia 27 Feldman,R.S. et al., 1992 Abstract of special issue, Can't locate 28 Fox,P.C. et al., 1991 Can't locate 29 Hamada,T. et al., 1999 Can't locate 30 23 Hay,K.D. et al., 2003 Sjogren's syndrome and radiation induced 31 Kirstila,V. et al., 1996 Not specified if meds inducing xerostomia,& results are reported mixed with Sjogren's and cancer subject groups 32 Lee,S.K. et al., 1995 Abstract of special issue, Can't locate 33 Lemaire,V., 1992 Not in english 34 Lokken,P. et al., 2005 Not in english 35 Maeda,M. et al., 2004 Not in english 36 Masters,K.J.,1998 Abstract only 37 Mercadante,S., 2000 Case report, Abstract only 38 Morita,Y. et al., 2004 Full text not found (Chinese) 39 Olsson,H. et al., 1991 Sjogren's disease 41 Rantanen,I. et al., 2002 Abstract for the study 38 which is excluded too 44 Rantanen,I. et al., 2003 Xerostomia is not Medication induced 45 Risheim,H. et al., 1993 didn't have a cohort of patients with medication induced xerostomia 46 Salah,R.S. et al., 1999 Full text not found (Chinese) 47 Shetty,K., 2005 duplicate 49 Ship,J.A., 2002 Study Review 50 Silvestre Donar,F.J. et al., Not a study, rather a series of general guidelines 51 24 2004 Simons,D. et al., 1997 Not xerostomia (cariogenic salivary microflora) 52 Soderling,E. et al., 1998 11/13 subjects = Sjogren's, all results reported as 1 group 53 Stewart,C.M. et al., 1998 duplicate 54 Stone,P. et al., 1999 Comment 55 Sung,J.M. et al., 2002 Can't locate 56 Taubert,M. et al., 2007 Can't locate 57 Tokiyasu,Y. et al., 1997 Can't locate 58 Valdez,I.H. et al., 1993 Not a study (review article) 59 Wang,Z.C. et al., 2000 Not in English 60 Watanabe,S. et al., 1997 Can't locate 61 Wynn,R.L. et al., 2000 Not a study 62 No author given, 2006 Xerostomia is radiation induced, not a study either 40 No author given, 2000 Not a study 42 No author given, 1995 Can't locate 43 25 Table 2a: Evidence for Anethole Trithione and Yohimbine (Comparative Study) Authors, Date Population Bagheri H, Schmitt L, Berlan M, and Montastruc J.L, 1997 ‐N=10 Intervention ‐double‐blinded ‐crossover study ‐pts on stable doses ‐pts randomly of TCA or neuroleptic allocated to Rx drugs (9 p.o., 1 yohimbine (3x6mg i.v.) for DSM IIIR Dx /day p.o.) or AT (3x of major depressive 25mg/day p.o.) for disorder(7) or 5 days @ 8/12/18 psychosis(3) hrs, respectively, all with ‐5 day washout subjective complaints period in between of dry mouth ‐NSFR recorded on ‐specified that doses day 1 (prior to Tx and Rx remained commencing on unchanged day 2), 6, 11, and throughout study 16. ‐16 days total ‐pts questioned about AE Controls Outcome Conclusions Critical appraisal comments ‐no placebo ‐pts compared to baseline NSFR recorded on day 1 ‐NB: effort was made so that ”all the drugs were given in form of similar capsules” ‐baseline NSFR was compared to post washout NSFR (day 11): no significant differences** ‐yohimbine increased NSFR 3‐5 fold in 5 days (p<0.01) ‐Failed to find AT effects on NSFR after 5 days, suggested insufficient duration for suspected mechanism of action ‐loss to follow up was not reported. ‐AT ineffective in 5 days (1.5 fold NSFR increase, not significant) ‐no AE reported with either drug ‐definition of xerostomia was not quantified CTFPHC Grade & Level of Evidence A ‐ I ‐yohimbine dosed based on previous research vs. AT dosed as was commonly used in clinical practice at the time of the study ** ensures washout was sufficient enough to claim no residual from one drug effected results of other pt(s): patient(s), TCA: tricyclic antidepressants, Dx: diagnosis, Rx: prescription, AE: adverse effects Table 2b: Evidence for Anethole Trithione Authors, Date Population Intervention Controls Outcome Conclusions Hamada, T. et al., 1999 ‐N= 36 ‐all pts on Rx antimuscarinic drugs , who exhibited greatly decreased NSFR with slightly decreased SSFR ‐Tx group :23 pt ‐Cx group: 13 pt ‐AT: 6 tablets/day (2 after each meal) for 14 days ‐topical use of artificial saliva 5‐6x daily Objective measures: ‐measured NSFR & SSFR in mL/10 min, on days 1 & 14 ‐AT increased NSFR as compared to baseline & controls (p<0.05) ‐AT increased SSFR as compared to controls (p<0.02) Subjective Measures: ‐pt reported symptom alleviation (dryness & irritation) 4 weeks post day 1 (p<0.001) ‐AT increased both SSFR & NSFR , objectively improving xerostomia symptoms after a short time (14 days) ‐subjectively pts reported continued symptom relief up to 2 weeks post study Conclusions and critical appraisals comments ‐not fully blinded (treating DDS assigned pts to Cx and Tx grps, neither DDS nor pts blinded) ‐mg dosage of tablets not specified ‐care received outside the study was not controlled for ‐tolerance of AE not clarified, but specified as “not severe” CTFPHC Grade & Level of Evidence B, II‐1 Tx: treatment, Cx: control 27 Table 3a: Evidence for Yohimbine Authors, Date Population Intervention Bagheri H, Schmitt L, Berlan M, and Montastruc JL, 1992* ‐N=20 (2 grps of 10) ‐all clinically depressed pts on Rx TCA for a min of 1 week (DSM III R criteria for Dx) who exhibited reduced salivary flow ‐no loss to follow up^ Protocol 2a): ‐10 mg acute yohimbine p.o. following overnight fast, prior to day 1 Protocol 2b): ‐randomly allocated pts to yohimbine or placebo, p.o. 4mg TID (at 8/12/18 hr) for 21 days ‐2 week washout period Controls Outcome Conclusions Critical Appraisal Comments Protocol 2a): ‐pt reported AE: ‐ensured pts ‐acute not on any administration of transient ‐increased NSFR 1 hr rhinorrhea, additional Yohimbine post acute acute diarrhea, drugs known to administration enhanced NSFR headache with modify salivary (p<0.005) in TCA pts facial flush outflow ‐therapeutic use ‐ baseline rates Protocol 2b): ‐definition of of Yohimbine considered per ‐measured NSFR at xerostomia not limited by short subject quantified duration of days 1/7/14/21 ‐no significant findings action ‐placebo used (Protocol 2b only) CTFPHC Grade & Level of Evidence A ‐ I *Please note protocol 1 was excluded due to the use of healthy volunteer not suffering from medication induced xerostomia. ^1 patient withdrew from study due to side effects upon acute administration of 10 mg yohimbine, but was replaced on day 0. 28 Table 3b: Evidence for Yohimbine Authors, Date Population Intervention Controls Bagheri H et. al., 1994 ‐N=19 (Protocol 1: 9 pts) (Protocol 2: 10 pts) ‐all depressed pts on clomipramine or amitriptyline (DSM III R criteria for Dx), ‐NB: specified pts not taking other drugs known to modify salivary flow Protocol 1: ‐10mg yohimbine p.o. following overnight fast Protocol 2: ‐double blinded ‐cross over study ‐randomly allocated pts to placebo or 4mg yohimbine p.o. ‐1 week washout period ‐1&2: NSFR and pt reported VAS (0max‐10no dry mouth) measured at time 0(prior to tx), 1, 2, 3, 4 hrs ‐baseline rates considered per subject ‐placebo used (protocol 2 only) Outcome Conclusions Critical Appraisal Comments ‐yohimbine ‐only short term Protocol 1: effect was ‐increased NSFR up to restores a normal salivary observed (4hrs 4 hrs after outflow in pts only) administration, with dry mouth peaking at 2hrs induced by TCA ‐ loss to follow (P<0.05) ‐5 pts with side effects when used as an up was not acute tx in higher reported (rhinorrhea, facial dosage (10mg), flush and nausea) but has an ‐protocol 1 increased lacked placebo Protocol 2: ‐increased NSFR up to likelihood of side 3 hrs after effects administration in experimental ‐low dose of group(P<0.05) yohimbine (4mg) ‐no significant effects could be useful with placebo in tx of dry ‐no side effects mouth due to clomipramine without side effects CTFPHC Grade & Level of Evidence A, I 29 Table 4a: Evidence for Pilocarpine Hydrochloride Authors, Date Population Intervention^ Controls Outcome ‐ pilocarpine ‐ baseline rates Experiment 1: hydrochloride (PHC) considered per ‐ both whole subject saliva and minor Experiment 1: gland measures ‐ placebo: increased as ‐ crossover study ‐ single oral dose of 5mg cholinergic agent compared to 25 % placebo and PHC or placebo, on 2 Dexpanthenon baseline values separate days within 1 drops p.o. (p<0.05) week* & monitored saliva flow in 15 (minor (experiment 1 only) glands) to 30 (whole Experiment 2: saliva) min intervals for 2 hours ‐ no significant changes in minor ‐ 2 week washout period or whole saliva prior to experiment 2 Experiment 2: ‐5 mg (5 drops) 2% PHC p.o TID for 5 weeks ‐measured whole saliva at day 0 and in 5 weeks time, measured minor gland saliva every 7 days for 5 weeks * washout period not specified, may not have been held constant for all subjects Alajbeg I, et. al., 2005 ‐N=12 ‐ Dx xerostomia based on previous medical history, subjective pt reports & NSFR <0.2mL/min ‐ type(s) of medications inducing xerostomia not specified Conclusions Critical Appraisal Comments Experiment 1: ‐ 5 mg PHC shown to increase minor & whole saliva output as compared to placebo. Experiment 2: ‐ oral PHC did not produce long term increase in salivary flow rate. ‐ assignment of patients to treatment was not randomized (patients got both treatment on 2 separate days) ‐ pts were blind to the treatment, however, study personnel was not ‐wash out period was not specified, may have been insufficient in avoiding carry‐over effects between tx periods ‐lack of placebo in experiment 2 CTFPHC Grade & Level of Evidence B, II‐1 ^ Please note flow from minor salivary glands was measured using Periotron 8000TM while whole saliva was collected and calibrated in test tubes, differences in measures used were not accounted for in results 30 Table 4b: Evidence for Pilocarpine Hydrochloride Authors, Date Population Davies A.N., Daniels C, Pugh R, and Sharma K, 1998 ‐N=64 (inpatient & homecare) specific to medication induced xerostomia Intervention ‐Crossover study ‐pts randomly allocated to Pilocarpine (3x5 mg/day p.o.) for 2 weeks or 2‐3 sprays of mucin based ‐all “advanced” artificial saliva for 2 malignant cancer weeks pts on variable ‐1 week washout classes of period in between xerostomic Rx drugs (mean: 2, ‐effects measured via range: 0‐6) with VAS (before and after prognosis >6 each Tx period) & weeks, who questionnaire (after reported oral each Tx period) dryness (subjective) ‐checklist for AE (mild/moderate/seve re) applied after each Tx period Controls Outcome Conclusions Critical appraisal comments CTFPHC Grade & Level of Evidence ‐no placebo ‐not blinded, pt could tell whether spray or pill used ‐pts subjective VAS scores compared to pre and post Tx periods ‐other saliva stimulants and substitutes were not permitted during the study ‐VAS scores showed Pilocarpine was more effective than artificial saliva (p<0.003), but was associated with more side effects (p<0.001) ‐50/50 for pt preference of artificial saliva vs. Pilocarpine ‐Artificial saliva is effective in managing xerostomia in this specific pt population, but Pilocarpine results in a more marked improvement and is thus considered more effective (as reported by pts) ‐both products cause AE, tolerability varies (slightly more tolerable for Pilocarpine) ‐Significant Tx‐period interaction noted by authors: Pilocarpine carryover effect not well controlled for (results showed response to artificial saliva was greater when following Pilocarpine) ‐ no objective measures in outcomes B, II‐1 ‐large loss to follow up (63%) due to death and AE ‐side effects were mostly reported as “mild” (65%) but not elaborated upon ‐additional mouth care products permitted/uncontro lled (local analgesics, antifungals, antiseptics) ‐pt population very ill, not well generalisable 31 Table 4c: Evidence for Pilocarpine Hydrochloride Authors, Date Population Intervention Controls Aframian DJ et al., 2007 ‐N = 19 ‐ sialosis and xerogenic medication pts grouped together (author logic: many pts suffer from both) ‐loss to follow up = 1 ‐single dose 5mg pilocarpine p.o., 2 hrs post eating and toothbrushing ‐monitored vital signs (pulse, BP, temperature), NSFR, & SSFR at t=‐10(10 min prior to tx), 1, 2 and 3 hrs ‐AE recorded throughout ‐baseline rates considered per subject ‐no placebo Outcome Conclusions Critical Appraisal Comments ‐only short term ‐pilocarpine increased ‐pilocarpine both NSFR and SSFR tablets increase effect was after 1, 2 and 3 hrs post NSFR and SSFR in considered (3hrs) tx (all at least p<0.05 or short term more significant) (single dose) for pts taking ‐ not clear ‐common complaints xerogenic whether tx for xerogenic medications effects specific medication/sialosis grp and/or suffering to sialosis or from metabolic medication were: urinary sialosis induced frequency, sweating, xerostomia, dizziness, tremor ‐no significant confounding changes in vital variable in pt signs post population pilocarpine grouping administration ‐not blinded ‐pts not randomly assigned to tx (all received tx) CTFPHC Grade & Level of Evidence B, II‐1 32 Table 4d: Evidence for Pilocarpine Hydrochloride Authors, Date Population Intervention ‐pilocarpine: 3x5 mg drops/day, by mouth, for 1 week ‐xerostomia assessed pre Tx (day 0) and daily thereafter using pt graded scale (0:absent‐ 3:severe) ‐opioid dose, pain relief, and ‐no loss to follow AE assessed on same scale in up same intervals ‐increased opioid dose on days 1,3, and 4 Mercadante ‐N=21, (home S, et al., care & inpatient) 2000 ‐all “advanced” cancer pt with opioid Rx induced xerostomia, further defined by a min of T2‐T3 in pt rated symptom intensity^ Controls Outcomes Conclusions Critical appraisal comments CTFPHC Grade & Level of Evidence ‐open label (not blinded) ‐no placebo, pts compared to baseline measures (day 0) ‐NB: other medications used for symptom control were recorded but not controlled for ‐no significant correlation between opioid dose and xerostomia intensity was found ‐effects of Pilocarpine can be observed within 24 hours (day 1) (p<0.0005) ‐AE are variable in timing and presentation, if any ‐pilocarpine has a short onset of activity in almost all pts, taking effect virtually immediately and this is maintained throughout the period of drug administration (prolonged effect may exist after discontinued use) ‐xerostomia recurred in pts who discontinued Pilocarpine, but still responded to further tx with the drug (include or not? No numbers to support or ref) ‐no AE with significant intensity could be attributed to Pilocarpine ‐no objective measures for outcomes B, II‐2 ‐open label, no placebo ‐not blinded ‐pt population very specific, difficult to generalize results 33 Figure 1: Study Identification and Selection Potentially relevant studies identified and screened for retrieval (n = 866, Medline=840, PubMed=26) Studies excluded after title and abstract screening with exclusion criteria (n = 809) Studies retrieved in full text for detailed PICO‐C evaluation (n = 55) Added from manual review of reference lists (n=1) Studies excluded after detailed evaluation (n= 41) ‐ Does not address a cohort of patients with medication‐induced xerostomia (13) ‐ Non‐English (n = 4) ‐ Not a clinical study (n = 9) ‐Duplicate (n=3) ‐ Not accessible (n=12) Studies included in checklist quality assessment (n=15) Studies excluded after quality assessment, based on scoring <8.5 (n=7) Studies included in evidenced based report (n=8) Figure 2: PICO-C Data Extraction Form Study Type: Population N Definition/Diagnosis Medication that induces xerostomia Intervention Intervention: (gum, pilocarpine etc) Duration Dose Comparison Placebo/None/Other Outcome Saliva flow VAS scale (pt reported) Other/Comments/Critical Appraisals: 35 Figure 3: Checklist Used to Assess Efficacy of Therapy or Prevention Checklist to Assess Evidence of Efficacy of Therapy or Prevention 1. Was the study ethical? ___ 2. Was a strong design used to assess efficacy? ___ 3. Were outcomes (benefits and harms) validly and reliably measured? ___ 4. Were interventions validly and reliably measured? ___ 5. What were the results? Was the treatment effect large enough to be clinically important? ___ Was the estimate of the treatment effect beyond chance and relatively precise? ___ If the findings were “no difference” was the power of the study 80% or better ___ 6. Are the results of the study valid? • Was the assignment of patients to treatments randomised? ___ • Were all patients who entered the trial properly accounted for and attributed at its conclusion? i) Was loss to follow‐up less than 20% and balanced between test and controls ___ ii) Were patients analysed in the groups to which they were randomised? ___ • Was the study of sufficient duration? ___ • Were patients, health workers, and study personnel “blind” to treatment? ___ • Were the groups similar at the start of the trial? ___ • Aside from the experimental intervention, were the groups treated equally? ___ • Was care received outside the study identified and controlled for ___ 7. Will the results help in caring for your patients? Were all clinically important outcomes considered? ___ Are the likely benefits of treatment worth the potential harms and costs? ___ 36 Appendix 1: Medline Search Strategy # Searches Results 1 drug induced xerostomia.mp. [mp=ti, ot, ab, nm, hw, tx, kw, ct, sh, tn, dm, mf] 41 2 medication induced xerostomia.mp. [mp=ti, ot, ab, nm, hw, tx, kw, ct, sh, tn, dm, mf] 7 3 dry mouth.mp. [mp=ti, ot, ab, nm, hw, tx, kw, ct, sh, tn, dm, mf] 5158 4 xerostomia.mp. [mp=ti, ot, ab, nm, hw, tx, kw, ct, sh, tn, dm, mf] 18571 5 hyposalivation.mp. [mp=ti, ot, ab, nm, hw, tx, kw, ct, sh, tn, dm, mf] 392 6 oral dryness.mp. [mp=ti, ot, ab, nm, hw, tx, kw, ct, sh, tn, dm, mf] 346 7 1 or 2 or 3 or 4 or 5 or 6 8 saliva stimulants.mp. [mp=ti, ot, ab, nm, hw, tx, kw, ct, sh, tn, dm, mf] 30 9 pilocarpine.mp. [mp=ti, ot, ab, nm, hw, tx, kw, ct, sh, tn, dm, mf] 13889 10 toothpaste.mp. [mp=ti, ot, ab, nm, hw, tx, kw, ct, sh, tn, dm, mf] 3989 11 dentrifice.mp. [mp=ti, ot, ab, nm, hw, tx, kw, ct, sh, tn, dm, mf] 24 12 sialogogue.mp. [mp=ti, ot, ab, nm, hw, tx, kw, ct, sh, tn, dm, mf] 75 13 gum.mp. [mp=ti, ot, ab, nm, hw, tx, kw, ct, sh, tn, dm, mf] 14 anethole trithione.mp. [mp=ti, ot, ab, nm, hw, tx, kw, ct, sh, tn, dm, mf] 15 interferon alpha.mp. [mp=ti, ot, ab, nm, hw, tx, kw, ct, sh, tn, dm, mf] 16 cevimeline.mp. [mp=ti, ot, ab, nm, hw, kw, tx, sh, ct, tn, dm, mf] 436 17 yohimbine.mp. [mp=ti, ot, ab, nm, hw, kw, tx, sh, ct, tn, dm, mf] 18527 18 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 82010 19 7 and 18 1177 20 remove duplicates from 19 917 21 limit 20 to yr="1990 - 2008" [Limit not valid in: DARE; records were retained] 840 21663 13535 240 31803 37 38