* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download ICL Design ICM is Very Thin
Survey
Document related concepts
Transcript
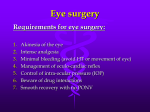
8/28/2015 Financial Disclosure: • Alcon, consultant Michael S. Petrik, MSc, OD, FAAO The author has received no financial gain nor proprietary investment in any of the companies or products presented today History of ICL Implantable Collamer Lens (ICL) Visian ICL™ (Staar Surgical) Over 500,000 have been implanted globally Intraocular lens made of collamer Removable/exchangable Very flexible (easy to inject, easy to explant) Easy to lathe: wide range of prescriptions Excellent optical perfomance (HD vision) ICL Design 100% Collagen & HEMA (hydroxyethyl methacrylate) copolymer i. First ICLs in Western World implanted in 1993: Roberto Zaldivar (Mendoza, Argentina) Christian Skorpik (Vienna, Austria) Paolo Pesando/Vincenso Assetto (Turin, Italy) ii. ICLM first approved in USA on Dec.26, 2005 iii. In Canada, ICM/ICH approved June 6, 2001 and Toric (TICM) approved June 8, 2005 Howard Gimbel implanted most TICM worldwide ICM is Very Thin < 100 um OPTIC Excellent biocompatibility 1) Protein repulsion – negative ionic charge, reduces protein adherence 2) Shields lens – Collamer attracts fibronectin, a protein that binds to collagen, which shields it from autoimmune attack by the body HAPTIC ≈ 100 microns FOOTPLATES 500-600 um Excellent transmittance and low reflectance 1 8/28/2015 ‘HD Vision’ with ICL 1. Corneal ‘Preservation’ Technique No corneal remodeling/injury ‘Sparing the cornea’ Nodal Point Optics Refractive correction sits further to back of the eye Closer to nodal point = best optical position PRK (Bowman’s) 2. Minimal Tissue Disruption Lens NOT sutured to structures Not removing tissue 3. Nodal Point Optics Light rays that are not refracted, but are translated down the optical axis ¾Refractive index 1.45 ¾UV Absorbing (10% transmission) LASIK (Stroma) ICL (sulcus) Myopic ICM: -3.0 to -20.0 (USA) -3.0 to -23.0 (CAN) Hyperopic ICH: +3.0 to +20.0 (CAN) ¾Removable/ Exchangeable ¾Very malleable/foldable Corrects cylinder at the individual axis Rotate +/- 22 degrees (CW or CCW) Toric TICM: -3.0 to -23.0 sph +1.0 to +6.0 cyl (CAN) 1. Diffuse lamellar keratitis 2. Central toxic keraotopathy 3. Epithelial ingrowth 4. Flap disturbance 5. Corneal striae/folds 2 8/28/2015 *Adults 19 – 45 years of age *No ocular pathology *Minimum 8mm dilated pupil (mesopic) *ACD ≥ 2.8 mm – measured from corneal endothelium (3.0mm preferred) *Angle grade VHIII to IV (>30 deg.) *Min. endothelial cell count ~2500 cells/mm2 *Stable refractive ≤ 0.50 D for 1 year *Low endothelium cell count <2000 cells/mm2 *Fuchs’ dystrophy or corneal pathology *Uveitis, pigment dispersion syndrome, retinal diseases, glaucoma, cataract *History of intraocular surgery *Blind in follow eye (amblyopia acceptable) *Diabetes, pregnant or nursing *The ‘20/40’ patient/expectations Keratoconus/Forme Fruste Thin corneal thickness Patients at risk for post op ectasia High refractive error in healthy eye Pseudophakia Amblyopia? Sulcus = depression or furrow Anterior to crystalline lens 3 8/28/2015 Placed in the posterior chamber of the phakic eye (sulcus) o The corneal endothelium benefits from a ‘shield function’ of the iris. Invisible to the eye Removable/exchangable No fixations into tissues (iris) Does not alter shape of the cornea or remove tissue WTW vs STS o Endothelium has a regenerative zone in the peripheral remodels over time. o Long term functioning of endothelium relies on the migration/remodeling of these cells. OCOS online ordering system International: Nidau, Switzerland USA: Monrovia, California STS BSS vs NaCl packaging ‘Swelling’ factor UBM provides a direct measurement of the STS *WTW is the only approved method by FDA Diameter ICM: 12.1, 12.6, 13.2, 13.7 (BSS) (mm) ICM: 11.5, 12.0, 12.5, 13.0 (NaCl) ICH: 11.0, 11.5, 12.0, 12.5 (NaCl) ¾ Cylinder is set to individual axis ¾ Lens implanted horizontally* 4 8/28/2015 Sulcus 1-2 weeks pre-op Must be large & patent: at least 0.8 to 1 mm Location: 10.30 o’clock and 1.30 o’clock, or (90°) apart in the superior iris Inadequate PIs can cause early post-op complications (IOP rise, pup. block) Manual Marking Horizontal Slit Live surgical tracking eliminates need for manual marking! 5 8/28/2015 180 ° 0° 5° CCW Diamond shaped marks indicate axial alignment. Plus axis at labeled if diamond marks at 0-180°. Plus axis at labeled + CCW rotation Plus axis at labeled – CW rotation Surgical Video to be played “THE VAULT” Myopic Hyperopic 6 8/28/2015 Degrees of ICL Vaulting High vault ICL Low vault • IOP spike! High IOP low 30s to 40s mmHg pupillary block/oversized ICL retained viscoelastic = ‘burp’ • Anterior Subcapsular Cataract 1.3% - US FDA Trial (0.6% significant) • Glaucoma (pigmentary, pup. block, ↑IOP) • Min. endothelial cell count <1500 mm2 = explant (World explantation rate is 1%) DO NOT dilate with cyclogel (can cause angle closure), use 1% trop./2.5% phenyl. IOP check: Caution if IOP >24 mmHg or 10 mmHg higher than pre-op IOP Elevation Retained Viscoelastic – burp and recheck Non-patent Iridotomies – repeat YAG Check PIs for patency Check ICL vault Low vault is common first 24 hours Intraocular procedure Pre-operative work up is more demanding Requires peripheral iridotomy *New version to eliminate PIs Cost $ = 2-4x more expensive than LASIK/PRK ¾ Treat high, low and astigmatic refractive errors (outside ranges of LASIK/PRK) ¾ Removable (LASIK/PRK are ‘committed’) ¾ Does not contraindicate future surgical procedures (cataract surgery) ¾ ICLs outperform LASIK/PRK in acuity and stability (Sanders and Vukich, 2006) 7 8/28/2015 Case 1 Case 1 Female, Caucasian, 23 years old, student from Oklahoma - heavily dependent on spectacles/soft contact lenses Implanted Toric ICL: OD: TICM125V4 -15.5 -6.00 x007 OS: TICM125V4 -18.0 -5.00 x180 Pre-op Cyclo Refraction: OD -11.50 -5.25 x010 OS -13.50 -3.75 x175 24 hour post op: VA: OD: 20/25+1 OS: 20/20-2 IOP: OD: 13mmHg OS: 13mmHg Vault: OD: 100% OS: 100% 3 month post op: VA: OD: 20/20-2 IOP: OD: 11mmHg OS: 13mmHg OS: 20/25Vault: OD: 110% OS: 110% Rx OD: +0.25 -0.25 x015 20/20-1 OS: +0.50 20/25+1 20/25-2 20/25-2 VD=13.75mm Pre-op Keratometry: OD 45.92@099, 42.99@009 OS 47.27@086, 43.77@176 ACD: Angles: CT: STS : IOP: OD 3.17, OS 3.28 (Pentacam) OD 40.5deg, OS 40.0deg (Pentacam) OD 526µm, OS 531µm OD 12.3, OS 12.4 (Sonomed) OD 15mmHg, OS 13mmHg Case 2 Case 2 Male, Caucasian, 36 years old, investment advisor, full time SCL/glasses, not a candidate for PRK/LASIK Implanted Toric ICL: OD: ICH120V3 +13.00 OS: ICH120V3 +13.00 Pre-op Cyclo Refraction: OD +7.00 20/20 OS +7.00 20/20 1 week post op: VA: OD: 20/20-2 OS: 20/25-2 IOP: OD: 14mmHg OS: 14mmHg Vault: OD: 100% OS: 100% 2 year post op: VA: OD: 20/20 IOP: OD: 13mmHg OS: 20/25+2 OS: 14mmHg Vault: OD: 75% OS: 75% Rx OD: -0.25 -0.25 x065 20/20 OS: -0.25 -0.50 x180 20/20 VD=13.75mm Pre-op Keratometry: OD 41.67@012, 42.29@102 OS 40.27@010, 41.36@100 ACD: OD 3.00, OS 3.00 (Pentacam) Angles: OD 31.1deg, OS 34.4deg CT: OD 537µm, 540µm STS: OD 11.6, OS 11.6 (Sonomed) IOP: OD 12mmHg, OS 12mmHg Case 3 Case 3 Male, Caucasian, 35 years old, auto technician from WA state, heavily dependent on spectacles/contacts Implanted Toric ICL: OD: TICM125V4 -7.50 -6.00 x025 OS: TICM125V4 -6.50 -6.00 x172 Pre-op Cyclo Refraction: OD -5.00 -4.25 x014 20/20 OS -4.00 -5.25 x174 20/20 24 hour post op: VA: OD: 20/20OS: 20/20IOP: OD: 14mmHg OS: 17mmHg Vault: OD: 75% OS: 50% 3 months post op: VA: OD: 20/20 IOP: OD: 16mmHg OS: 20/20OS: 17mmHg Vault: OD: 100% OS: 75% Rx OD: plano 20/20 OS: pl -0.50 x020 20/20 VD=13.75mm Pre-op Keratometry: OD 45.92@102, 42.61@012 OS 45.92@084, 42.13@174 ACD: OD 2.96, OS 3.04 (Pentacam) Angles: OD 39.7deg, OS 39.2deg CT: OD 542µm, 530µm STS: OD 11.8, OS 12.0 (Sonomed) IOP: OD 16mmHg, OS 17mmHg 8 8/28/2015 Case 4 Case 4 Female, Caucasian, 52 years old, bus driver - heavily dependent on spectacles, no contacts - pt at high risk for RD with refractive lensectomy Implanted Toric ICL: OD: TCIM120V4 -20.0 -1.00 x073 OS: TCIM120V4 -20.0 -3.00 x100 Pre-op Cyclo Refraction: OD -15.25 -1.25 x075 OS -16.50 -3.25 x102 24 hour post op: VA: OD: 20/25 OS: 20/70IOP: OD: 14mmHg OS: 14mmHg Vault: OD: 40% OS: 40% 12 month post op: VA: OD: 20/15-2 IOP: OD: 17mmHg OS: 15mmHg OS: 20/40-2 Vault: OD: 50% OS: 100% Rx OD: plano -0.50 x180 20/15 OS: -0.25 -1.25 x150 20/25-2 VD=13.75mm 20/20-1 20/50+2 (amblyopic) Pre-op Keratometry: OD 46.55@054, 46.17@054 OS 46.81@012, 45.49@102 ACD: OD 2.99, OS 2.93 (Pentacam) Angles: OD 41.8deg, OS 42.6deg CT: OD 535µm, 532µm STS: OD 11.43, OS 11.37 (Sonomed) IOP: OD 16mmHg, OS 16mmHg Visian CentraFLOW technology (V4c) Thank You! Eliminates the need for preoperative PIs! 9