* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Radiographic Interpretation of Infections of Jaws Pericoronitis
Acute pancreatitis wikipedia , lookup
Neonatal infection wikipedia , lookup
Periodontal disease wikipedia , lookup
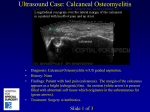
Schistosomiasis wikipedia , lookup
Chagas disease wikipedia , lookup
Hepatitis C wikipedia , lookup
Hospital-acquired infection wikipedia , lookup
Infection control wikipedia , lookup
Hepatitis B wikipedia , lookup
Osteochondritis dissecans wikipedia , lookup
Multiple sclerosis signs and symptoms wikipedia , lookup
Radiographic Interpretation of Infections of Jaws Pericoronitis 1 Pericoronitis • Erupting or partially impacted third molars • Inflamed gingiva • Trismus • Cellulitis Pericoronitis (R/F) • In early stages stages, minimal radiographic changes • Radiolucency adjacent to the crown • Ill-defined periphery • Sclerotic border in late stage • Osteomyelitis, in sever cases 2 Normal Follicular Space 3 4 Acute Suppurative Osteomyelitis Acute Suppurative Osteomyelitis • Dental infection – most common cause • Other causes: fracture, wound, hematogenous spread • Common organisms: Staph. aureus, Staph. S ap a albus, bus, tuberculosis, ube cu os s, actinomycosis, syphilis, mixed organisms 5 Suppurative Osteomyelitis • May involve either jaw • Localized in maxilla, diffuse in mandible • Severe pain • temperature, WBC count Suppurative Osteomyelitis (R/F) • • • • • • Early stages: no radiographic changes Ill-defined periphery Decrease in the density of bone Followed by increased radiolucency Sclerosis at later stages Sequestra: nonvital bone 6 Suppurative Osteomyelitis (R/F) • • • • • Resorption Periosteal new bone formation Proliferative periostitis Fistula formation Radiographic features similar to malignant lesions 7 Sequestrum 8 9 10 In-class Exercise: Case 1 • 4 month old baby • Meningitis 11 Nuclear Medicine Study 12 13 14 15 In-class Quiz : Case 2 Chronic Focal Sclerosing Osteomyelitis 16 Chr. Focal Sclerosing Osteomyelitis • • • • Sclerosing or condensing osteitis Younger, < 20 yrs Mostly mandibular first molar Large carious lesion Focal Sclerosing Osteomyelitis (R/F) • Initial stage – no radiographic signs • Rarefying osteitis – radiolucent area • Sclerosing osteitis – dense sclerotic bone, trabeculation difficult to identify • Difference with idiopathic osteosclerosis 17 18 19 Chronic Diffuse Sclerosing Osteomyelitis Chr. Diffuse Sclerosing Osteomyelitis • May not be associated with carious teeth • Intermittent, recurrent episodes of swelling, pain, fever • Any age, mostly elderly patients • Prevalence in African American • Chronic low grade infection • Pain, if present, is often mild • Acute exacerbation 20 Chronic Osteomyelitis With Proliferative Periostitis Garre’s Periostitis 21 Chronic Osteomyelitis With Proliferative Periostitis • Garre’s Garre s Periostitis (1893) • Younger, <25 yrs • Mostly mandible Garre’s Periostitis (R/F) • • • • Often associated with a carious tooth Mottled, predominantly lucent Focal overgrowth of bone “Onion-skin” appearance : layering of cortical bone 22 23 24 In-class exercise: Case 3 25 Osteoradionecrosis Osteoradionecrosis • • • • Radiotherapy (40 to 80 Gy) Decreased vascularity Low defense High susceptibility to extraction, perio, pulpal disease, disease denture sore 26 Osteoradionecrosis (R/F) • Similar to osteomyelitis • Diagnosis established by history 27 28 ONJ, BON, BRON • Osteonecrosis of the jaw • Bisphosphonate-associated osteonecrosis of the jaw • Bisphosphonate-related osteonecrosis of the o e ja jaw Clinical features of ONJ • Spontaneous or after extraction • Initially asymptomatic • Pain, tooth mobility, mucosal swelling, erythema, ulceration • Early stage: minimal radiographic changes • Late stage: R/F of osteomyelitis or cancer • Widened PDL spaces 29 Potential risk factors • Dentoalveolar trauma • Duration of BP treatment • Type of BP: i.v. BP is more problematic Staging • Stage 1: exposed, necrotic bone that is asymptomatic • Stage 2: exposed, necrotic bone, with pain and infection • Stage 3: Exposed, necrotic bone in patients ti t with ith pain, i iinfection, f ti and d pathologic fracture, extraoral fistula, or osteolysis extending to the inferior border 30 Florid Cemento-osseous Dysplasia Florid Cemento-osseous Dysplasia • Wide Wide-spread spread form of periapical cemental dysplasia • Mostly female, middle-aged, African, Asian • May ay not o be sy symptomatic po a c 31 Florid Cemento-osseous Dysplasia • Poor vascular supply – prone to infection • Osteomyelitis, if infected • Preventive management Florid C-O Dysplasia (R/F) • • • • • Usually bilateral bilateral, both jaws Well-defined sclerotic border Internal content of mixed density Large irregular masses Hypercementosis 32 33 Maxillary Sinusitis (will discuss in Unit 12) Maxillary Sinusitis • • • • Acute, chronic and recurrent Acute Allergic Infectious Dental sources – Periapical lesions – Traumatic extractions (Oro-antral fistula) 34 Maxillary Sinusitis (R/F) • Thickening of mucosal lining • Cloudy appearance in periapical or panoramic • Bony erosion – Fungal infection – Carcinoma – Chronic infection 35 36 37 38