* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download changes of the vaginal biocenosis in cervical dysplasic lesions
Diagnosis of HIV/AIDS wikipedia , lookup
Traveler's diarrhea wikipedia , lookup
Dirofilaria immitis wikipedia , lookup
Hepatitis B wikipedia , lookup
Schistosomiasis wikipedia , lookup
Anaerobic infection wikipedia , lookup
Clostridium difficile infection wikipedia , lookup
Middle East respiratory syndrome wikipedia , lookup
Gastroenteritis wikipedia , lookup
Sexually transmitted infection wikipedia , lookup
Sarcocystis wikipedia , lookup
Neonatal infection wikipedia , lookup
Human cytomegalovirus wikipedia , lookup
Carbapenem-resistant enterobacteriaceae wikipedia , lookup
Human papillomavirus infection wikipedia , lookup
Oesophagostomum wikipedia , lookup
Microbicides for sexually transmitted diseases wikipedia , lookup
Cervical cancer wikipedia , lookup
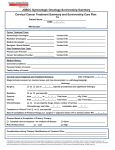
ORIGINAL ARTICLES CHANGES OF THE VAGINAL BIOCENOSIS IN CERVICAL DYSPLASIC LESIONS Elena Bernad1, Doru-Mihai Anastasiu1, Razvan Ilina2, Delia Hutanu3, Marius Virjan1, Cosmin Brisan4 REZUMAT Introducere: Este bine cunoscut faptul că disturbarea biocenozei vaginale prin prezenţa unor factori infecţioşi poate duce la modificări celulare locale, care pot preceda dezvoltarea unor leziuni cervicale. Material şi metode: Am realizat un studiu în cadrul Clinicii Universitare de Obstetrică şi Ginecologie „Bega” din Timişoara, în perioada 01.07.2008-15.03.2009, pe un număr de 113 paciente cu rezultate patologice la testul Babeș-Papanicolaou. Am urmărit de asemenea prezenţa altor factori infecţioşi în afară de virusul papilloma uman. S-au recoltat probe pentru examen bacteriologic şi cultură de la nivel vaginal. Rezultate: Într-un procent ridicat a fost identificată o disturbare a biocenozei vaginale, prin prezenţa unor factori infecţioşi - 41,6% dintre paciente având un rezultat pozitiv la examenul bacteriologic sau la cultură, 71% prezentând infecţie cu HPV. Mai mult, în grupul cu leziuni HSIL s-a observat un procent crescut de probe pozitive pentru floră bacteriană (63,6% din pacientele cu HSIL au prezentat examen bacteriologic sau culturi pozitive). Cea mai mică incidenţă în alterarea ecosistemului vaginal a fost observată la pacienţi cu citologie ASCUS (23,5%). Concluzii: Având în vedere asocierea proceselor pre-neoplazice cu inflamaţiile genitale cronice, un control regulat care ar evidenţia şi trata infecţiile vaginale ar fi foarte important pentru a preveni leziunile canceroase. Cuvinte cheie: biocenoza vaginală, vaginita, citologie Babes-Papanicolaou, leziuni precanceroase ABSTRACT Introduction: It is well known that disturbing vaginal biocenosis throught the presence of infectious factors can be blamed for the celular changes which precede the development of the lesional cervix. Material and methods: We have performed a study at the Bega University Clinic of Obstetrics and Gynecology, from Timisoara, between 01.07.2008-15.03.2009, on a number of 113 pacients with pathological results of the Babes-Papanicolaou cytology; we were also interested in the involvement of other infectious factors aside the human papilloma virus. Vaginal discharge samples were taken for bacterial tests and cultures. Results: In a large procentage of cases a clear disturbance of the vaginal biocenosis was observed, due to a variety of infectious factors – 41.6% of the pacients included in the cohort had positive bacteriological tests or cultures, 71% HPV infection from the investigated pacients. Furthermore, in the cohort with HSIL cytology we saw the greatest percentage of positive samples for pathological bacterial flora (63.6% of the pacients with HSIL cytology had a positive bacteriological test or culture), the lowest incidence of vaginal ecosistem alteration was observed in the pacients with ASCUS cytology (23.5%). Conclusions: Due to the association of pre-neoplasic processes with chronic genital inflamations, a regular examination with the discovery and treatment of vaginal infections is of utmost importance for the prevention of cancerous lesions. Key Words: vaginal biocenosis, vaginitis, Babes-Papanicolaou cytology, precancerous lesion INTRODUCTION Cervical cancer is an important public health problem worldwide, considering that this condition is the second cause of mortality through cancer in women, following breast cancer, causing yearly over a quarter of a million deaths globally.1,2 Department of Obstetrics/Gynecology, 2 Department of Surgical Oncology, Victor Babes University of Medicine and Pharmacy, Timisoara, 3 Biology Department, West University, Timisoara, 4 Clinical Emergency County Hospital, Timisoara 1 Correspondence to: Ass. Prof. Elena Bernad, Bega Hospital of Obstetrics and Gynecology, 12 V. Babes Str., Timisoara, Tel. +40-745-395220. Email: [email protected] Received for publication: Feb. 01, 2010. Revised: Apr. 20, 2011. _____________________________ 54 TMJ 2011, Vol. 61, No. 1 - 2 In developed countries, where the screening programs using the cytological examination Babes-Papanicolaou are correctly and completely implemented, the detection and treatment of asymptomatic precancerous lesions, which are curable in almost 100% of the cases, is possible.3 Still, five of six women with cervical cancer live in developed countries and 80% of them are diagnosed in a late stage of the disease.4 The persistent infection with approximately 15 carcinogen genotypes of human papillomavirus (HPV) determine practically all the cases of cervical neoplasia, as well as precancerous lesions and in situ carcinoma.5 The vaginal ecosystem is a complex and dynamic system of microorganisms which interact with local factors to maintain the balance of this environment. The endogenous microflora comprises a variety of microorganisms of which we can mention aerobic, anaerobic and optionally anaerobic ones. Of these, Doderlein bacilli (Lactobacillus acidophilus) represent a special category in the vaginal ecosystem, having a role in maintaining the acidity that characterizes the vaginal secretion in physiological conditions and plays a vital role in avoiding the colonization of the vagina with pathogenic organisms, including those which produce bacterial vaginitis and candidiasis, infections of the urinary tract or sexually transmitted diseases. Aside lactobacilli, in the normal vaginal secretion there are also a number of aerobic bacteria of the diphteroid type, Streptococcus, Staphylococcus or anaerobic (Peptococcus, Peptostreptococcus, Bacteroides speciae), as well as mycolpasma and isolated strains of Candida. Any change of the local conditions of the vagina (pH modification, temperature, hormonal impregnation etc.) can lead to colonization with possible or really pathogenic germs and the appearance of vulvo-vaginal infections. It is also known that altering the vaginal biocenosis, through the presence of infectious factors at this level, is involved in the initiation of some cellular changes at local level, which in time can lead to a lesional cervix; there are studies which show a high incidence of cervical dysplasia in patients with bacterial vaginitis.7- 9 MATERIALS AND METHODS - Low-risk HPV strains – 6, 11, 40, 43, 44, 54, 70; - Possible high-risk HPV – 26, 53, 66; - Other types of HPV – 69, 71 and 74. Also there were samples where the viral DNA was amplified, but the genotype involved could not be detected. RESULTS The cyto-bacteriological examination performed through the Babes-Papanicolau cytology has provided the following results: out of a total of 113 samples, 74 have been classifies LSIL according to the Bethesda classification (analogous to CIN I and cellular changes associated with HPV), 22 samples matched the HSIL changes, analogous to CIN II and CIN III, and 17 samples have been classified as ASCUS - atypical squamous cells. (Fig. 1) HSIL; 22; 19% ASCUS; 17; 15% LSIL; 74; 66% This paper presents a retrospective study done on a cohort of 113 patients between the ages of 18 and 79 years, which presented to the Bega Clinical Hospital of Obstetrics and Gynecology, Timisoara, in the interval 01.07.2008-15.03.2009. The study included patients which had pathological cytologies, and for which we Figure 1. Distribution of the results obtained at the cytobacteriological test in have monitored the association of infectious factors the studies cohort. aside the infection with HPV, through bacteriological samples and cultures from the vaginal secretion. Fig 1. Distribution TheofHPV DNAobtained resultsathave shown the following: the results the cytobacteriological test in the studies c All the patients included in the study had a Babes30 samples have been negative and 74 samples (71%) Papanicolaou cytology done, and samples were taken have been positive for the infection with different from the vaginal secretion for HPV DNA testing, as HPV genotypes. Among the positive samples, in 15 well as for other cultures and bacterial tests in order to cases we detected the simultaneous infection with detect the possible associated infectious factors. multiple strains of HPV. For the detection of the HPV infection the The detection of other infectious factors samples have been taken through brushing the cervix associated with the HPV infection, possibly involved and have been tested for HPV DNA, through the in the appearance of the lesional cervix, has been done polymerization chain reaction (PCR), for the following through the sampling of cultures and bacteriological HPVgenotypes: tests from the vaginal secretion. In a large number of - High-risk HPV strains – 16, 18, 31, 33, 35, 39, cases we have found the disturbance of the vaginal 45, 51, 52, 56, 58, 59, 68, 73, 82 – of these , strains 16, biocenosis with a variety of infectious factors. From 18, 31 and 45 have a very high oncogenic risk; the total number of 113 bacteriological tests, in 27 _____________________________ Elena Bernad et al 55 cases we have found the replacement of the normal vaginal flora formed by lactobacilli Doderlein, with a pathogenic flora represented by Gardnerella vaginalis, species of Candida, Trichomonas vaginalis or Lepthotrix vaginalis. Thus, as presented in Table 1, where we have represented the distribution of results of the bacteriological exams of the vaginal secretion, the most frequent infection was with Gardnerella vaginalis (12 cases), followed by vaginal candidosis (present in 8 cases) and the associated infection with both Gardnerella vaginalis and Candida albicans which was detected in 3 cases. Table 2. The distribution of results obtained in the cultures taken from the vaginal secretion. Positive cultures 36 Staphylococcus aureus 8 Escherichia coli 6 Enterococcus faecalis 5 Klebsiella 4 Enterococcus spp 3 Associations between different bacterial species 3 Other bacterial species 7 Negative cultures 77 Table 1. The results of the bacteriological testing of the vaginal secretion. Positive bacteriological tests 27 (23.9%) Gardnerella vaginalis 12 (10.6%) Candida 8 (7.1%) The corroboration the data obtained in obtained the Table 2. Theofdistribution of results in the tests performed to detect the pathogenic microbial 3 (2.6%) Gardnerella vaginalis associated with Candida flora of the inferior vaginal tract, with the those secretion. from the cyto-diagnostic examination of the cervix, 2 (1.7%) Trichomonas vaginalis has shown the frequent association of the alteration 2 (1.7%) Lepthotrix vaginalis of the vaginal ecosystem with modification of Negative bacteriological tests 86 (76.1%) the Babes-Papanicolaou cytology classified HSIL and an association in a lower percentage with LSIL modifications or ASCUS. In other words, the presence The cultures taken from the vaginal secretion have of the infectious factors in the vaginal secretion was Table 1. of The the bacteriological testing of vaginal shown the alteration theresults vaginalofbiocenosis with a detected in the 14 of the 22secretion patients with HSIL at the wide variety of infectious agents, of which the most cyto-diagnostic examination, 29 patients with LSIL frequently involved microorganisms were: Escherichia and only 4 patients with a cytology classified ASCUS. coli, Streptococcus beta haemolyticus, Klebsiella, (Fig. 2) Enterococcus faecalis, Staphylococcus aureus, Enterococcus spp. and Enterobacter aerogenes. Of the 113 cultures sampled, in 36 cases several pathogenically species developed, and 77 cultures have been negative. In Table 2 is presented the distribution of results obtained from the cultures sampled from the vaginal secretion. We need to mention the fact that five patients with a positive culture had associated the presence of Gardnerella vaginalis, detected Figure 2. Percentual distribution of the presence of the infectious factors, at the bacteriological test, and three patients with according to the cyto-diagnostic result. Fig 2. Procentual distribution of the presence of the infectious factors according to the cytoa positive culture has associated the presence of candidosis. Also it is very important to observe that diagnostic DISCUSSIONS result for 31 patients with positive bacteriological test or culture, no lactobacilli Doderlein were detected at Cervical intraepithelial neoplasia (CIN) and the bacteriological test. The study of the presence cervical cancer represent a major cause of morbidity of infectious factors at the level of the vaginal tract and mortality for women and was several times has shown the alteration of the vaginal biocenosis suggested that bacterial vaginitis can play an important in 47 of the patients in the cohort, in 13 cases part in the development of CIN.10 It has been proven there were associations between different bacterial that the presence of HPV infection in the cells of the species. cervix is a major factor in the initiation of the cervical _____________________________ 56 TMJ 2011, Vol. 61, No. 1 - 2 dysplasia processes, but not all pacients infected with HPV develop cervical lesions, this indicating that there are additional factors which together lead to the initiation of displasic transformation processes.11 Moreover there are studies which have shown a greater incidence of displasic changes of the cervix among the pacients with an alteration of the vaginal ecosistem.12,13 Bacterial vaginitis is a polimicrobial syndrome that affects the inferior genital tract, characterized by the replacement of the normal vaginal flora that comprises lactobacilli, with pathogenic flora mostly Gardnerella vaginalis, Mycoplasma hominis, Ureaplasma urealyticum, certain species of Mobiluncus or Prevotella, Chlamydia as well as other anaerobic organisms. Moreover, some Gardnerella vaginalis biotypes are more frequently associated with bacterial vaginitis with clinical manifestation.14,15 In our study, the presence of the infectious factors in the inferior genital tract was detected in greater procentage of cases (41.6% of the pacients included in the cohort had positive bacteriological tests or cultures), this fact proving the possible involvement of the alteration of the vaginal biocenosis, together with the HPV infection, in the development of the lesional cervix. Furthermore, in the cohort with HSIL cytology we saw the greatest percentage of positive samples for pathological bacterial flora (63.6% of the pacients with HSIL cytology had a positive bacteriological test or culture), the lowest incidence of vaginal ecosistem alteration was observed in the pacients with ASCUS cytology (23.5%). Of the 74 pacients with a LSIL cytology, 29 cases have shown the presence of the infectious factors throught the tests done (39.2%). The most frequent microorganisms involved in the alteration of the vaginal biocenosis at the pacients in our cohort were: Gardnerella vaginalis (15 patients), Candida (11 patients), Staphylococcus aureus (8 patients), Escherichia coli (6 patients). What is more, 13 patients in the cohort (11.5%) have presented an alteration of the vaginal ecosistem through the association of two or more pathogenic agents. Finally, it would be important to emphasize the fact that in what prevention and early detection of the premalignant and malignant cervical pathology are concerned, all women should have cytologies done every six months or at least once a year. Furthermore, the periodical colposcopic examination of the cervix should also be performed. CONCLUSIONS The increased incidence of infectious factors in patients with pathological results of the cytology shows that the statements, according to which these factors have an important part in the initiation of the displasic processes of the cervix together with HPV, have a real basis. Nevertheless, in the future, studies are needed to verify if this association exists, as well as research that helps in understanding the intimate mechanisms which initiate the dysplasic process. Until then, though, due to the frequent association of the pre-neoplasic associations with chronic vaginal inflammations, we deem extremely important the regular check-up with the detection and treatment of the genital infections, as a method of prevention of the appearance of the cancerous lesions. ACKNOWLEDGEMENTS This work has been supported by Romanian National Authority for Scientific Research, The National Plan for Research, Development and Inovation for the period 2007-2013, Programme III CAPACITIES, grant no: 54/2008. REFERENCES 1. Speck LM, Tyring SK. Vaccines for the prevention of human Papillomavirus infections. Skin Therapy Lett 2006;11(6):1-3. 2.Zonfrillo NJ, Hackley B. The quadrivalent human papillomavirus vaccine: Potential factors in effectiveness. Journal of Midwifery & Women’s Health 2008;53(3):188-94. 3.Murray CJL, Lopez AD. Global health statistics. Boston, Harvard School of Public Health, WHO and World Bank, 1996. 4.Stewart BW, Kleihues P. Cancers of the female reproductive tract. In WHO Cancer Report Lyon, France. IARC 2003;215-22. 5.Castle PE. Invited commentary: Is monitoring of human Papillomavirus infection for viral persistence ready for use in cervical cancer screening? Am J Epidemiol 2008;168(2):138-44. 6.Faro S. Vaginitis: diagnosis and management. Menopausal Study. Int J Fertil 1996;41(2):115-23. 7.Boyle CM, Uthayakumar S, Hlaket J, et al. Does bacterial vaginosis cause cervical neoplasia? Proceedings of the 29th Annual Meeting of the Society of Gynecologic Oncologists, February 7–11, 1998;108. 8.Guijon F, Paraskevas M, Rand F, et al. Vaginal microbial flora as a cofactor in the pathogenesis of uterine cervical intraepithelial neoplasia. Int J Gynaecol Obstet 1992;37(3):185-91. 9.Platz-Christensen JJ, Sundstrom E, Larsson P. Bacterial vaginosis and cervical intraepithelial neoplasia. Acta Obstet Gynecol Scand 1994;73:586-8. 10.Sweet RL. Gynecologic conditions and bacterial vaginosis: Implications for the non-pregnant patient. Infect Dis Obstet Gynecol 2000;8(34):184-90. 11.Bedell MA, Jones KH, Laimins LA. The E6–E7 region of human papillomavirus type 18 is sufficient for transformation of NIH 3T3 and Rat-1 cells. J Virol 1987;61(11):3635-40. 12.McDougall JK. Cofactors in the progression of HPV-associated tumors. In: Giraldo G, Salvatore M, Chieco-Bianchi L, Beth-Giraldo E, Editors. Advanced technologies in research. Diagnosis and treatment of AIDS in oncology, Basel: Karger. 1994;46:150-164. 13.Bosch FX, Manos MM, Munoz N, et al. International biological study on cervical cancer (IBSCC study group). Prevalence of human papillomavirus in cervical cancer: a worldwide perspective. J Natl Cancer Inst 1995;87(11):796-802. _____________________________ Elena Bernad et al 57 14.Aroutcheva AA, Simoes JA, Behbakht K, et al. Gardnerella vaginalis isolated from patients with bacterial vaginosis and from patients with healthy vaginal ecosystems. Clin Infectious Diseases 2001;33:1022–7. _____________________________ 58 TMJ 2011, Vol. 61, No. 1 - 2 15.Koumans EH, Kendrick JS. CDC Bacterial Vaginosis Working Group. Preventing adverse sequelae of bacterial vaginosis: a public health program and research agenda. Sex Transm Dis 2001;28:292-7.