* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Echocardiographic diastolic parameters and risk of atrial
Heart failure wikipedia , lookup
Electrocardiography wikipedia , lookup
Saturated fat and cardiovascular disease wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Jatene procedure wikipedia , lookup
Cardiovascular disease wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Coronary artery disease wikipedia , lookup
Heart arrhythmia wikipedia , lookup
Ventricular fibrillation wikipedia , lookup
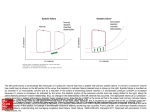
CLINICAL RESEARCH European Heart Journal (2012) 33, 904–912 doi:10.1093/eurheartj/ehr378 Heart failure/cardiomyopathy Echocardiographic diastolic parameters and risk of atrial fibrillation: the Cardiovascular Health Study Michael A. Rosenberg 1*, John S. Gottdiener 2, Susan R. Heckbert 3, and Kenneth J. Mukamal 4 1 Beth Israel Deaconess Medical Center, Cardiovascular Institute, 185 Pilgrim Road, Baker 4, Boston, MA 02215, USA; 2Department of Medicine, University of Maryland Hospital, Baltimore, MD, USA; 3Department of Epidemiology, University of Washington, Seattle, WA, USA; and 4Department of General Medicine and Primary Care, Beth Israel Deaconess Medical Center, Boston, MA, USA Received 13 April 2011; revised 16 August 2011; accepted 13 September 2011; online publish-ahead-of-print 11 October 2011 Aims Atrial fibrillation (AF) is the most common sustained arrhythmia in the elderly, and shares several risk factors with diastolic dysfunction, including hypertension and advanced age. The purpose of this study is to examine diastolic dysfunction as a risk for incident AF. ..................................................................................................................................................................................... Methods We examined the association of echocardiographic parameters of diastolic function with the incidence of AF in 4480 and results participants enrolled in the Cardiovascular Health Study, an ongoing cohort of community-dwelling older adults from four US communities. Participants underwent baseline echocardiography in 1989–1990 and were followed for incident AF on routine follow-up and hospitalizations. After 50 941 person-years of follow-up (median follow-up time 12.1 years), 1219 participants developed AF. In multivariable-adjusted age-stratified Cox models, diastolic echocardiographic parameters were significantly associated with the risk of incident AF. The most significant parameters were the Doppler peak E-wave velocity and left atrial diameter, which demonstrated a positive nonlinear association [HR 1.5 (CI 1.3 –1.9) and HR 1.7 (CI 1.4 –2.1) for highest vs. lowest quintile, respectively], and Doppler A-wave velocity time integral, which displayed a U-shaped relationship with the risk of AF [HR 0.7 (CI 0.6 –0.9) for middle vs. lowest quintile]. Each diastolic parameter displayed a significant association with adjusted NT-proBNP levels, although the nature of the association did not entirely parallel the risk of AF. Further cluster analysis revealed unique patterns of diastolic function that may identify patients at risk for AF. ..................................................................................................................................................................................... Conclusion In a community-based population of older adults, echocardiographic measures of diastolic function are significantly associated with an increased risk of AF. ----------------------------------------------------------------------------------------------------------------------------------------------------------Keywords Atrial fibrillation † Diastolic dysfunction † Ageing † Echocardiography Introduction The prevalence of atrial fibrillation (AF) in the population is increasing.1 Some 2.3 million adults in the USA currently have AF, a figure expected to increase to 5.6 million by the year 2050, with more than 50% being more than 80 years of age.2 In addition to advanced age, hypertension is a well-known risk factor for AF,3 and has been shown to be predictive for the development of AF in large population studies.4 Despite these well-known associations, the specific mechanisms through which these processes act to cause AF are less well known. Diastolic dysfunction refers to impairment in the ventricular filling phase of the cardiac cycle. It is often broken down into several components, including impaired myocardial relaxation, increased left atrial pressure, decreased left ventricular compliance, and deficiencies in atrial contraction.5 Impairment in any single component, or often several at once, can cause increased pressure to be transmitted back to the atria, pulmonary veins, and lungs. As a result, diastolic dysfunction has been associated with increased mortality,6 as well as increased risk of hospitalization7 and congestive heart failure.8 Atrial fibrillation and diastolic dysfunction share many common risk factors, including ageing and hypertension.9 – 11 Hypertension * Corresponding author. Tel: +1 617 667 8800, Fax: +1 617 206 9570, Email: [email protected] Published on behalf of the European Society of Cardiology. All rights reserved. & The Author 2011. For permissions please email: [email protected] 905 Echocardiographic diastolic parameters and risk of AF itself, as well as left-ventricular hypertrophy that occurs as a result of chronic hypertension, is a well-known risk factor for diastolic dysfunction.12 In addition, diastolic dysfunction, such as AF, increases with age,13 and patients given the diagnosis of diastolic dysfunction were more likely to have AF at the time of diagnosis.14 Smaller, shorter-term studies have shown that certain subtypes of diastolic dysfunction are at greater risk of AF.15 Yet, despite their shared risk factors and association, large studies with long-term follow-up examining the relationship between diastolic dysfunction and incident AF are lacking. In this study, we examined the characteristics of diastolic function measured by echocardiography on the incidence of AF in a large cohort of participants over 65 years of age adjusting for known risk factors for AF. Methods Population The design and objectives of the Cardiovascular Health Study have been previously described.16 In brief, CHS is a longitudinal study of 5201 men and women aged 65 years, randomly selected from Medicare lists in Pittsburgh, PA; Forsyth County, NC; Sacramento, CA; and Hagerstown, MD. The original cohort was enrolled in 1989 – 1990; a second cohort of 687 African-Americans was recruited in 1992– 1993, but is not included in these analyses as they did not undergo baseline echocardiography. The institutional review board at each centre approved the study, and each participant gave informed consent. The baseline examination included a standardized questionnaire, validated previously by Psaty et al.,17 assessing a variety of risk factors, including smoking, alcohol intake, history of stroke, coronary heart disease, and heart failure, self-reported health status, and medications on enrolment. The physical examination included measurements of height, weight, and seated blood pressure measured with a random-zero sphygmomanometer,17 as well as a resting 12-lead ECG. Laboratory examinations included measurement of total cholesterol, high-density lipoprotein cholesterol, fasting glucose, C-reactive protein, serum creatinine,18 and NT-proBNP,19 although NT-proBNP was only available in 3464 individuals in the analytic data set (see below). Of the initial 5201 individuals in the original population, 130 people were excluded due to prevalent AF. We also excluded an additional 130 participants due to the presence of mitral stenosis or greater than moderate aortic insufficiency or mitral regurgitation. We excluded 180 participants with a confirmed history of stroke due to concerns that prevalent AF, and subsequent thromboembolism, may have been the aetiology of the stroke; these subjects had a particularly high risk of subsequent stroke that validated this concern. An additional 281 participants were excluded due to the absence of major echocardiography information used in this study to analyse diastolic dysfunction, leaving a final study population of 4480 subjects. Echocardiography The design of the echocardiography protocol used in CHS has been described in detail elsewhere.20 Briefly, for each subject, a baseline echocardiogram was recorded onto super-VHS tape with a Toshiba SSH-160A cardiac ultrasound machine using a standardized protocol. Videotapes were reviewed at the central Echocardiography Reading Center using an offline image-analysis system equipped with customized computer algorithms. Quality-control measures included standardized training of echo technicians and readers, periodic technician observation by a trained echocardiographer, blind duplicate readings to establish interreader and intrareader measurement variabilities, periodic reader review sessions, phantom studies on the ultrasound equipment, and quality-control audits. Echocardiographic parameters included qualitative two-dimensional left ventricular systolic function, qualitative two-dimensional left ventricular chamber size, M-mode-based parasternal long-axis left atrial dimension (LA diameter), and Doppler mitral valve inflow consisting of early and late peak velocity (peak E and A velocity, respectively), and velocity time integral (E and A wave VTI, respectively) and Doppler mitral valve first third of early filling velocity.20 The Doppler mitral valve inflow images were obtained from two averaged beats of pulse-wave Doppler image obtained through placement of the cursor at the mitral valve leaflet tips in the apical four-chamber view,20 with measurements of peak E and A velocities, and velocity time integrals taken on the same image. We also included ratios of peak early-to-late velocity (E/A ratio) and ratio of early-to-late velocity time integrals (E/A VTI ratio). M-mode-based quantitative measurements of fractional shortening and left ventricular dimensions were only available in a subset of individuals, and thus were excluded from the analysis. Although left atrial volume has been described as a more accurate measure of left atrial size than two-dimensional left atrial diameter,21 only the M-mode-based parasternal long-axis-derived left atrial diameter was available in most participants. To evaluate how closely this single linear measure estimated left atrial volume, we used results from a second echocardiogram from 1994 to 1995 in which left atrial volume was measured in a subset of CHS participants.21 We found a Spearman correlation of parasternal long-axis LA diameter with LA volume of 0.73 among 372 participants free of prevalent or incident congestive heart failure. Determination of incident atrial fibrillation Participants were contacted every 6 months for follow-up, alternating between a telephone interview and a clinic visit for the first 10 years and by telephone interview only after that. An annual resting ECG was obtained yearly through the ninth year of follow-up. Discharge diagnoses for all hospitalizations were entered into the database. Adjudication of cardiovascular events was performed by a centralized events committee.22 Annual study ECGs were interpreted by the EPICARE ECG reading centre, where the diagnoses of AF or atrial flutter were verified.23 When hospital discharge diagnosis International Classification of Diseases, Ninth Revision, code identified AF or atrial flutter, AF was considered to be present as of the date of hospital admission. [A prior study determined the positive predictive value of hospital discharge diagnosis to be 98.6% for diagnosis of AF in CHS23 and a Holter substudy identified that only 1 in 819 subjects (0.1%) had persistent or intermittent AF not identified by the above measures.]24 Analysis SAS version 9.2 (SAS Institute, Cary, NC, USA) was used for all analyses. The primary outcome was the development of incident AF, with the follow-up time being that from baseline until first episode of AF, death, or end of follow-up. We used Cox proportional hazards models, with independent hazard functions for each year of participant age. The initial base model incorporated the following covariates, selected based on relevance from prior studies and univariate associations with the risk of AF within this cohort: gender; height; BMI; ECG findings of first degree AV block (PR interval greater than 906 200 ms), bradycardia (heart rate , 60 b.p.m.), Q waves in a regional distribution or any ventricular conduction delay (including right bundle branch block, left bundle branch block, or intraventricular conduction delay);25,26 history of congestive heart failure (based on clinical diagnosis by the treating physician), diabetes (American Diabetic Association definition), hypertension (defined as blood pressure greater than 140/90 mmHg, or on medications to reduce high blood pressure), or self-reported history of myocardial infarction;17 systolic and diastolic blood pressure, fasting glucose and creatinine level measured on enrolment; the use of diuretics beta-blockers, calcium channel blockers and ACE inhibitors on enrolment; and peak FEV-1, also measured on enrolment. To avoid assumptions about linearity, echocardiographic variables were examined in quintiles, and were initially inserted into the model and tested for heterogeneity across quintiles using the Wald Chi-square test. These were then examined simultaneously, with exclusion of non-significant echocardiographic variables from the model. Schoenfeld residuals and time-varying covariates were used to test for violation of the proportional hazards assumption; none were noted. We performed a sensitivity analysis on the 3464 participants in whom NT-proBNP levels were available, further adjusting our Cox models for NT-proBNP. We also tested adjusted mean NT-proBNP levels for each quintile of significant echocardiographic parameter using generalized linear models. As an additional exploration, hierarchical cluster analysis was performed using the Ward method27 in which individuals were clustered into six groups according to the three primary echocardiographic parameters. Initial studies revealed that this clustering algorithm divided participants relatively evenly, with the exception of one group of four individual outliers, who were excluded from the analysis, leaving five well-balanced groups. Qualitative graphical examination of eigenvalues confirmed reasonable separation of clusters. Clusters were analysed within the base model as mentioned above, as well as in a substudy of the 3464 participants with NT-proBNP levels. NT-proBNP levels were also measured for each cluster. Results Of 4480 participants studied for median follow-up of 12.1 years (interquartile range 6.6 –17.2 years; total 50 941 person-years), 1219 developed AF. Characteristics of the study population are shown in Table 1. The diastolic parameters we studied had values consistent with prior studies of elderly populations,28 – 31 and were normally distributed across the population. When inserted into the base model, we found that M-mode parasternal long-axis LA diameter, early Doppler mitral valve inflow velocity (peak E velocity), and late inflow Doppler mitral valve velocity time integral (A wave VTI) were the strongest predictors of incident AF. The Doppler mitral valve late inflow velocity (peak A wave velocity) was significantly associated with incident AF, but only when the A wave VTI was excluded; thus we did not include it in our final model. We also did not include the mitral valve Doppler peak velocity E/A ratio, the VTI E/A ratio, or the first third filling of early diastole in the final model, as none of these parameters was significantly associated with the AF incidence. Table 2 demonstrates the hazard ratio for quintiles of each of these diastolic parameters, as well as qualitative LV function and chamber size, when all three significant diastolic M.A. Rosenberg et al. Table 1 Selected baseline characteristics of 4480 CHS participants, including echocardiography parameters and incidence of AF Characteristic ................................................................................ Demographics Age (years, mean + SD) 72.6 + 5.5 Male gender, n (%) BMI (mean + SD) 1880 (42) 26.4 + 4.5 ................................................................................ Medical history CHF, n (%) MI, n (%) 139 (3) 415 (9) DM, n (%) 1263 (28) HTN, n (%) 2493 (56) Medications Diuretics, n (%) 1082 (24) ................................................................................ Beta-blockers, n (%) 556 (12) Calcium channel blockers, n (%) ACE inhibitor, n (%) 509 (11) 272 (6) Digoxin, n (%) 277 (6) ................................................................................ Cardiac function Normal systolic function, n (%) Mildly depressed systolic function, n (%) 4103 (92) 230 (5) Severely depressed systolic function, n (%) 133 (3) ................................................................................ Echocardiography Doppler peak E velocity, m/s (mean + SD) Doppler peak A velocity, m/s (mean + SD) 0.71 + 0.17 0.80 + 0.21 Doppler E wave velocity time integral, cm (mean + SD) 12.0 + 5.0 Doppler A wave velocity time integral, cm (mean + SD) 8.7 + 3.2 M-Mode left atrial diameter, cm (mean + SD) 3.9 + 0.6 E/A velocity ratio (mean + SD) 0.93 + 0.35 ................................................................................ Outcome Atrial fibrillation, n (%) 1219 (27.2) Data presented in the table are mean and SD for continuous variables and number of cases with percentage in parentheses for categorical variables. BMI, body mass index; CHF, congestive heart failure; MI, history of myocardial infarction; DM, diabetes mellitus; HTN, hypertension. See Text for details of echocardiography data. parameters are included in the model. Both the LA diameter and peak E velocity displayed an increasing relationship with the risk of AF. The A wave VTI displayed a U-shaped relationship with the AF incidence, with the lowest risk in the middle quintile and highest risk in the two extreme quintiles. Kaplan –Meier curves for the predictive diastolic parameters of peak E velocity, A wave VTI, and LA diameter are shown in Figure 1. The serum NT-proBNP level has been shown to be linearly associated with the risk of incident and prevalent AF.19 Within the subset of the larger sample in whom levels had been obtained, we found NT-pro-BNP was strongly associated with the risk of AF when inserted in the base model along with predictive diastolic 907 Echocardiographic diastolic parameters and risk of AF Table 2 Hazard ratio for incident atrial fibrillation according to echocardiographic parametersa Parameter Quantile/group Adjusted HR 95% CI P heterogeneity Peak E velocity 1 (0.16– 0.56 m/s) 2 (0.57– 0.65 m/s) 3 (0.66– 0.73 m/s) 4 (0.74– 0.83 m/s) 5 (0.84– 1.85 m/s) 1.0 0.983 1.095 1.172 1.549 – 0.807–1.197 0.900–1.334 0.961–1.429 1.275–1.883 ,0.001 1 (1 –6 cm) 2 (7 –7 cm) 3 (8 –9 cm) 4 (10–10 cm) 5 (11–80 cm) 1.0 0.881 0.742 0.803 0.946 – 0.716–1.085 0.622–0.886 0.645–1.001 0.772–1.160 0.005 1 (1.5–3.3 cm) 2 (3.3–3.7 cm) 3 (3.7–4.0 cm) 4 (4.0–4.4 cm) 5 (4.4–6.5 cm) 1.0 1.002 0.954 1.176 1.696 – 0.818–1.228 0.774–1.177 0.961–1.440 1.386–2.075 ,0.001 Normal Mildly depressed Severely depressed 1.0 1.227 1.077 – 0.937–1.605 0.694–1.670 0.33 Normal 1.0 – 0.55 Mildly dilated Severely dilated 1.072 1.212 0.839–1.368 0.844–1.741 ............................................................................................................................................................................... ............................................................................................................................................................................... A wave VTI ............................................................................................................................................................................... Left atrial diameter ............................................................................................................................................................................... LV systolic function ............................................................................................................................................................................... LV chamber size a Adjusted for gender, height, BMI, any AV block on ECG, bradycardia on ECG, any Q waves on ECG, any history of ventricular conduction disease on ECG, history of congestive heart failure, diabetes, hypertension, or myocardial infarction, systolic, and diastolic blood pressure, random glucose and creatinine level, diuretic use, beta-blockers, calcium channel blockers, and ACE inhibitors, and peak FEV-1, as well as peak E velocity, A wave VTI, LA diameter, qualitative LV systolic function, and qualitative LV chamber size. Figure 1 (A) Kaplan– Meier curve for quantiles of Doppler early mitral inflow velocity on survival free from atrial fibrillation, with adjustment for risk factors (see text). (B) KM curve for Doppler late mitral inflow velocity time integral. (C ) KM curve for M-mode derived left atrial size. 908 M.A. Rosenberg et al. Figure 2 BNP levels according to specified quantiles of Doppler early MV inflow velocity, late MV inflow VTI, and M-mode LA size, with adjustment for base model variables (see text for details). *P , 0.05 vs. lowest quintile. †P , 0.05 vs. middle quintile. parameters (HR 3.80, 95% CI, 2.92–4.95, for quintile 5 vs. quintile 1). Diastolic parameters remained significantly associated with the risk even with adjustment for NT-proBNP, although inclusion modestly reduced the risk estimates associated with diastolic parameters. For example, the HR for the highest quintile vs. the lowest quintile of peak E velocity decreased from 1.58 (CI 1.26–1.970) to 1.46 (CI 1.17–1.83) and HR for the highest quintile vs. lowest quintile of LA size decreased from 1.76 (CI 1.41– 2.21) to 1.63 (CI 1.30 –2.04). Likewise, the hazard ratio for the middle quintile vs. the lowest quintile of late flow velocity integral increased from 0.70 (0.57–0.86) to 0.78 (0.64–0.96). To further explore the relationship between serum NT-proBNP and diastolic function, we examined levels of NT-proBNP for each of the predictive diastolic parameters, LA diameter, peak E velocity, and A wave VTI, after adjustment for base model co-variates (Figure 2). Both peak E velocity and LA diameter displayed a trend toward increased NT-proBNP with increasing velocity and size (Figure 2, peak E velocity Ptrend , 0.001; LA diameter Ptrend ¼ 0.02). A wave VTI displayed a decreasing relationship with the NT-proBNP level, with the lowest quintile having the highest mean NT-proBNP level (Ptrend , 0.001). Although we found certain individual metrics of diastolic function to be independently associated with the AF incidence, a number of studies have used multiple diastolic parameters to classify patients into categories of diastolic dysfunction.6,15,32 As we were missing many of the parameters used in these studies, such as deceleration time, pulmonary vein inflow, and tissue Doppler, rather than attempting to ‘fit’ the patients into one of these categorization schemes, we chose to explore patterns of diastolic dysfunction based on echocardiographic parameters of diastolic function through the use of cluster analysis. We clustered participants using the three predictive diastolic parameters LA diameter, peak E velocity, and A wave VTI (for details, see Analysis in the Methods section). The characteristic diastolic echocardiographic parameters of each of the five clusters are shown in Table 3. Notably, only Clusters 4 and 5 were associated with increased risk of incident AF when included in the base model, with HR of 1.65 and 1.67, respectively (Table 4). These clusters had the common characteristic of having peak E velocity increased from the population mean. Cluster 2, in which the LA size alone was increased, and Cluster 3, in which the A wave VTI alone was increased, were not associated with the risk of AF. When NT-proBNP was examined with the cluster data (Supplementary material online, Table S1), we found that interestingly, only Cluster 5 displayed evidence of effect attenuation with regards to risk for incident AF—HR 1.67 (CI 1.38– 2.01) for Cluster 5 without NT-proBNP and HR 1.53 (CI 1.23–1.91) with NT-proBNP included. Compared with the other groups, Cluster 5 also had an average higher unadjusted NT-proBNP level of 380 + 55 pg/dL, compared with the other clusters, with the next highest level in Cluster 4 of 293 + 32 pg/dL (Supplementary material online, Table S1). Discussion In this large population of older adults, with over 1000 cases of AF, we found a strong relationship between ventricular diastolic filling parameters and the risk of incident AF. Each of three markers of diastolic function—LA size, peak E velocity, and A wave VTI—independently predicted the development of incident AF. In addition, through the application of a novel technique in the study of diastolic function called cluster analysis, we identified groups of individuals at increased risk for AF, based on these variables. The importance of left atrial enlargement has been well described as a risk factor for incident AF,19,33 and thus our finding that increased LA diameter independently predicts AF is not surprising. However, to our knowledge, few if any of the 909 Echocardiographic diastolic parameters and risk of AF Table 3 Cluster Echocardiography parameters of clustersa Number Doppler MV early inflow velocity, m/s (mean + SD) Doppler MV late inflow VTI, cm (mean + SD) Left atrial size, cm (mean + SD) ............................................................................................................................................................................... 1 1377 0.71 + 0.11 7.6 + 1.7 3.33 + 0.48 2 1246 0.57 + 0.099 7.9 + 1.9 4.20 + 0.46 3 4 643 631 0.61 + 0.12 0.80 + 0.11 10.5 + 1.9 10.1 + 3.0 3.53 + 0.33 4.53 + 0.45 579 0.97 + 0.14 8.8 + 2.9 4.00 + 0.58 4476 0.71 + 0.17 8.7 + 3.2 3.86 + 0.60 5 Total/mean a See text for details of cluster analysis. Table 4 Hazard ratios for incident atrial fibrillation for each cluster with adjustment for base model variables* Cluster HR 95% CI ................................................................................ 1 1.0 – 2 3 1.04 1.03 0.88–1.24 0.84–1.27 4 1.65 1.36–1.99 5 1.67 1.38–2.01 Adjusted for gender, height, BMI, any AV block on ECG, bradycardia on ECG, any Q waves on ECG, any history of ventricular conduction disease on ECG, history of congestive heart failure, diabetes, hypertension, or myocardial infarction, systolic and diastolic blood pressure, random glucose and creatinine level, diuretic use, beta-blockers, calcium channel blockers, and ACE inhibitors, and peak FEV-1. *P(heterogeneity) , 0.001. Doppler-based echocardiographic variables have independently been shown to change the risk for incident AF. Our finding that both peak E velocity and the A wave VTI can be used in the prediction of AF in older individuals thus supports what many clinicians had long assumed: that there is a physiological mechanism for how certain risk factors like hypertension contribute to the development of AF, and that mechanism might be diastolic dysfunction. However, although our results suggest that even limited measures of diastolic dysfunction (compared with what is available with tissue Doppler, strain imaging, and pulmonary vein flow assessment) can be used to predict the development of AF, the complexity of the relationship demonstrates that much more needs to be learned about diastolic dysfunction and how it affects the electrical activity in the atrium. In this study, we found that such complexity may require novel analytical tools, and perhaps changes in some of the prior assumptions about how we describe diastolic function in terms of categorization. One important approach we used in this study was to examine diastolic parameters jointly and without assumptions about linearity. This approach was important because we found that all three significant diastolic parameters displayed nonlinear associations with the risk of incident AF. That risk would not have been detected had we simply included the continuous variables into a linear model, as prior studies have done.19 Instead, we were able to demonstrate that above ‘high’ peak E velocities (.0.84 m/s), the risk of AF increased nonlinearly, and at ‘normal’ A wave velocity time integrals (8–9 cm), the risk is nonlinearly decreased. In addition, through this method, we also found that prior relationships of diastolic parameters may not be useful, at least in regard to predicting AF. One example was our finding that the relationship between AF and diastolic filling patterns did not appear to follow the established pattern determined by the E/A ratio.14,15 In our population, because risk was increased with increased peak early filling velocity, but U-shaped with the A wave VTI, a simple ratio of these two factors was unlikely to categorize risk appropriately; hence, even with adjustments for nonlinearity, we did not detect a significant effect from the E/A ratio. Other studies have shown a similar U-shaped relationship between late, atrial-based, ventricular filling and risk of AF,34 supporting our finding that the nature of the early and late ventricular filling relationship is more complex with regard to risk of incident AF. The second approach employed in this study to explore the complex relationship between diastolic parameters and AF was to use an unsupervised hierarchical cluster analysis based on the diastolic echocardiography parameters. Many studies of diastolic dysfunction have used pre-determined classification schemes to group individuals to predict risk of AF,15 CHF,32 or mortality.6 One key limitation to this approach was demonstrated in the analysis by Tsang et al.,15 in their study of diastolic dysfunction on AF risk in 840 elderly men and women, in which the only diastolic parameter that individually was correlated with AF risk was left atrial volume. As a result, although they developed and utilized a categorical approach to diastolic classification based on prior studies of diastolic function, the only clinically important factor was the LA volume, raising the question of whether categorization of diastolic function was even necessary. Although we found that other diastolic parameters were independently associated with AF risk, we still had no method to determine whether the highest risk individuals had the highest risk values for all diastolic parameters (i.e. largest LA diameter and peak E velocity, and most abnormal A wave VTI) or whether these parameters tended to segregate independently as well. To explore this question further, we employed the cluster analysis, in which we found that when ‘forced’ to divide into five groups based on diastolic function, it was two groups (Clusters 4 and 5) that were at increased risk. From this analysis, we made several interesting observations. 910 The first was the recognition that there might be groups not previously identified in standard classification schemes of diastolic dysfunction that were at an increased risk for incident AF. For example, Cluster 4 had both increased early and late filling (increased A wave VTI) compared with the mean, along with an increased LA diameter, and had a 65% increase in the risk of incident AF compared with Cluster 1. The diastolic properties of this group would not fall into one of the standard patterns of diastolic dysfunction (i.e. impaired relaxation, pseudonormalization, or restrictive filling),6,35 – 37 but may represent a separate AF risk group in whom larger atria and more atrial-based ventricular filling is associated with an increased risk of AF. Cluster 5, in which the peak E velocity was elevated, but atrial filling was relatively normal and the LA size was mildly increased, may correspond to the ‘pseudonormal’ or restrictive filling patterns, which have been associated with increased risk of AF,15 and perhaps might also explain why it was the only category in which inclusion of NT-proBNP appeared to attenuate the risk of AF, as this pseudonormal or restrictive filling patterns have been shown to have elevated natriuretic peptide levels.32,38 A second observation was that increased peak E velocity, common to both Clusters 4 and 5, appeared to be required for the development of incident AF, as neither increased LA size (Cluster 2) nor increased atrial-based ventricular filling (Cluster 3) in isolation was associated with an increased risk. This finding may have important clinical implications, since it suggests that in an older population, the peak E velocity may be the most important determinant of AF risk, with increased LA diameter and changes in the A wave VTI from normal being of secondary importance, although further studies would be necessary to validate this finding. A prior study by Patton et al.19 in this same elderly population demonstrated that random serum NT-proBNP level was highly predictive of AF incidence, when adjustments were made for known confounders. That study included only limited analysis of echocardiographic diastolic parameters, although subgroup analysis failed to identify an interaction between LA size and NT-proBNP level on AF incidence. One of the challenges of inclusion of biomarkers in regression models is that the impact of inclusion or exclusion of parameters rests primarily in the mechanism, and thus confounding relationship, by which the biomarker is associated with the increased AF incidence. For this reason, we chose not to include NT-proBNP in the original model since it remains unclear whether NT-proBNP itself causes AF or whether it is simply a marker of cardiac disease. When NT-proBNP was included in the model during a secondary analysis, we found that the predictiveness of each individual diastolic parameter decreased, suggesting a mechanistic link. However, both diastolic variables and NT-proBNP remained significantly predictive, indicating that each may be acting via other mechanisms to increase AF incidence. One interesting possibility mentioned earlier is that there may be a separate population of patients, as identified in Cluster 4, who have high atrial-based filling (increased A wave VTI) and LA enlargement, but relatively normal NT-proBNP levels, who are also at increased risk of AF, although further research is necessary to validate this finding. Few previous prospective studies have attempted to examine the association between diastolic function and AF, and none of M.A. Rosenberg et al. this size to our knowledge. One reason is that such a large number of factors have been associated with the risk of AF, such as hypertension, age, gender,3,4,39 BMI,40 GFR,41 bradycardia,42 FEV-1,43 as well as NT-proBNP level,19 that relatively large studies are needed to account fully for important confounders. One example of this limitation was demonstrated by Vasan et al.,34 who examined diastolic parameters in the Framingham cohort and found a trend towards increased risk of AF, although the association was not significant (P ¼ 0.08), likely as a result of being underpowered—only 85 individuals developed AF in their study. Other groups have examined the unadjusted risk,15 although such associations are limited by the inability to account for the multiple confounders associated with AF. A principal limitation of this study was that we were unable to incorporate many of the more ‘modern’ measures of diastolic function including tissue Doppler, strain rate and strain analysis, and left atrial volume applied across the entire population. This limitation was an expected consequence of a study spanning two decades; tissue Doppler, strain imaging, and other more advanced metrics were unavailable at the time of study enrolment. It is possible, but not yet proven, that more nuanced measures of diastolic function will in time demonstrate the importance of diastolic filling properties on risk of AF, since an evident weakness of many present non-invasive measures is that they are indirect measures of diastolic function. In addition, it also possible that quantitative, rather than qualitative, measures of LV size and function would change the predictability of diastolic measures on predicting AF incidence; further studies would be necessary to explore this potential effect. Another important caveat to this study is that its findings may not necessarily be applicable to younger populations. It has been well described that the E wave velocity decreases naturally with ageing,44 and thus an elevated level that might be associated with pathology in an older population may be within normal range and not associated with increased AF risk in a younger population. Future studies in younger populations will be necessary to answer this question. In conclusion, in this study we found that diastolic filling parameters are predictive of increased risk of AF incidence. This association is complex, and required that we use an approach that made no assumptions about linearity, as well as a secondary analysis using the novel technique of hierarchical cluster analysis, to uncover some of the potential clinical and mechanistic associations. Further studies will be necessary to demonstrate whether changes in clinical practice, such as treatment adjustments based on diastolic filling parameters, can decrease the incidence of AF in patients at risk. Supplementary material Supplementary material is available at European Heart Journal online. Funding The research reported in this article was supported by contracts N01HC-85239, N01-HC-85079 through N01-HC-85086, N01-HC-35129, N01 HC-15103, N01 HC-55222, N01-HC-75150, N01-HC-45133, 911 Echocardiographic diastolic parameters and risk of AF and grant HL080295 and HL068986 from the National Heart, Lung, and Blood Institute (NHLBI), with additional contribution from the National Institute of Neurological Disorders and Stroke (NINDS). Additional support was provided through AG-023629, AG-15928, AG-20098, and AG-027058 from the National Institute on Aging (NIA). A full list of principal CHS investigators and institutions can be found at http://www.chs-nhlbi.org/pi.htm. S.R.H. also has received funding from the NHLBI grant R01 HL068986. 20. 21. 22. Conflict of interest: none declared. 23. References 1. Majeed A, Moser K, Carroll K. Trends in the prevalence and management of atrial fibrillation in general practice in England and Wales, 1994 – 1998: analysis of data from the general practice research database. Heart 2001;86: 284 – 288. 2. Go AS, Hylek EM, Phillips KA, Chang Y, Henault LE, Selby JV, Singer DE. Prevalence of diagnosed atrial fibrillation in adults: national implications for rhythm management and stroke prevention: the AnTicoagulation and Risk Factors in Atrial Fibrillation (ATRIA) Study. JAMA 2001;285:2370 –2375. 3. Kannel WB, Abbott RD, Savage DD, McNamara PM. Epidemiologic features of chronic atrial fibrillation: the Framingham study. N Engl J Med 1982;306: 1018– 1022. 4. Krahn AD, Manfreda J, Tate RB, Mathewson FA, Cuddy TE. The natural history of atrial fibrillation: incidence, risk factors, and prognosis in the Manitoba Follow-Up Study. Am J Med 1995;98:476 –484. 5. Quinones MA. Assessment of diastolic function. Prog Cardiovasc Dis 2005;47: 340 –355. 6. Redfield MM, Jacobsen SJ, Burnett JC Jr, Mahoney DW, Bailey KR, Rodeheffer RJ. Burden of systolic and diastolic ventricular dysfunction in the community: appreciating the scope of the heart failure epidemic. JAMA 2003; 289:194 – 202. 7. Cahill JM, Horan M, Quigley P, Maurer B, McDonald K. Dopplerechocardiographic indices of diastolic function in heart failure admissions with preserved left ventricular systolic function. Eur J Heart Fail 2002;4:473 –478. 8. Stevens SM, Farzaneh-Far R, Na B, Whooley MA, Schiller NB. Development of an echocardiographic risk-stratification index to predict heart failure in patients with stable coronary artery disease: the Heart and Soul study. JACC Cardiovasc Imaging 2009;2:11–20. 9. Tokushima T, Reid CL, Gardin JM. Left ventricular diastolic function in the elderly. Am J Geriatr Cardiol 2001;10:20–29. 10. Lewis JF, Maron BJ. Cardiovascular consequences of the aging process. Cardiovasc Clin 1992;22:25 –34. 11. Lee DS, Gona P, Vasan RS, Larson MG, Benjamin EJ, Wang TJ, Tu JV, Levy D. Relation of disease pathogenesis and risk factors to heart failure with preserved or reduced ejection fraction: insights from the framingham heart study of the national heart, lung, and blood institute. Circulation 2009;119:3070 –3077. 12. Vasan RS, Levy D. The role of hypertension in the pathogenesis of heart failure. A clinical mechanistic overview. Arch Intern Med 1996;156:1789 – 1796. 13. Zile MR, Brutsaert DL. New concepts in diastolic dysfunction and diastolic heart failure: part I: diagnosis, prognosis, and measurements of diastolic function. Circulation 2002;105:1387 –1393. 14. Chen HH, Lainchbury JG, Senni M, Bailey KR, Redfield MM. Diastolic heart failure in the community: clinical profile, natural history, therapy, and impact of proposed diagnostic criteria. J Card Fail 2002;8:279 – 287. 15. Tsang TS, Gersh BJ, Appleton CP, Tajik AJ, Barnes ME, Bailey KR, Oh JK, Leibson C, Montgomery SC, Seward JB. Left ventricular diastolic dysfunction as a predictor of the first diagnosed nonvalvular atrial fibrillation in 840 elderly men and women. J Am Coll Cardiol 2002;40:1636 – 1644. 16. Fried LP, Borhani NO, Enright P, Furberg CD, Gardin JM, Kronmal RA, Kuller LH, Manolio TA, Mittelmark MB, Newman A et al. The Cardiovascular Health Study: – 276. design and rationale. Ann Epidemiol 1991;1:263 17. Psaty BM, Kuller LH, Bild D, Burke GL, Kittner SJ, Mittelmark M, Price TR, Rautaharju PM, Robbins J. Methods of assessing prevalent cardiovascular disease in the Cardiovascular Health Study. Ann Epidemiol 1995;5:270 –277. 18. Cushman M, Cornell ES, Howard PR, Bovill EG, Tracy RP. Laboratory methods and quality assurance in the Cardiovascular Health Study. Clin Chem 1995;41: 264 –270. 19. Patton KK, Ellinor PT, Heckbert SR, Christenson RH, DeFilippi C, Gottdiener JS, Kronmal RA. N-terminal pro-B-type natriuretic peptide is a major predictor of 24. 25. 26. 27. 28. 29. 30. 31. 32. 33. 34. 35. 36. 37. 38. 39. 40. the development of atrial fibrillation: the Cardiovascular Health Study. Circulation 2009;120:1768 – 1774. Gardin JM, Wong ND, Bommer W, Klopfenstein HS, Smith VE, Tabatznik B, Siscovick D, Lobodzinski S, Anton-Culver H, Manolio TA. Echocardiographic design of a multicenter investigation of free-living elderly subjects: the Cardiovascular Health Study. J Am Soc Echocardiogr 1992;5:63–72. Aurigemma GP, Gottdiener JS, Arnold AM, Chinali M, Hill JC, Kitzman D. Left atrial volume and geometry in healthy aging: the Cardiovascular Health Study. Circ Cardiovasc Imaging 2009;2:282–289. Ives DG, Fitzpatrick AL, Bild DE, Psaty BM, Kuller LH, Crowley PM, Cruise RG, Theroux S. Surveillance and ascertainment of cardiovascular events. The Cardiovascular Health Study. Ann Epidemiol 1995;5:278–285. Psaty BM, Manolio TA, Kuller LH, Kronmal RA, Cushman M, Fried LP, White R, Furberg CD, Rautaharju PM. Incidence of and risk factors for atrial fibrillation in older adults. Circulation 1997;96:2455 –2461. Mozaffarian D, Psaty BM, Rimm EB, Lemaitre RN, Burke GL, Lyles MF, Lefkowitz D, Siscovick DS. Fish intake and risk of incident atrial fibrillation. Circulation 2004;110:368 –373. Furberg CD, Manolio TA, Psaty BM, Bild DE, Borhani NO, Newman A, Tabatznik B, Rautaharju PM. Major electrocardiographic abnormalities in persons aged 65 years and older (the Cardiovascular Health Study). Cardiovascular Health Study Collaborative Research Group. Am J Cardiol 1992;69: 1329 –1335. Blackburn H, Keys A, Simonson E, Rautaharju P, Punsar S. The electrocardiogram in population studies. A classification system. Circulation 1960;21:1160 – 1175. Ward JH. Hierarchical grouping to optimize an objective function. J Am Stat Assoc 1963;58:236 –244. Cohen GI, Pietrolungo JF, Thomas JD, Klein AL. A practical guide to assessment of ventricular diastolic function using Doppler echocardiography. J Am Coll Cardiol 1996;27:1753 – 1760. Kuznetsova T, Herbots L, Lopez B, Jin Y, Richart T, Thijs L, Gonzalez A, Herregods MC, Fagard RH, Diez J, Staessen JA. Prevalence of left ventricular diastolic dysfunction in a general population. Circ Heart Fail 2009;2:105 –112. Wierzbowska-Drabik K, Krzeminska-Pakula M, Chrzanowski L, Plewka M, Waszyrowski T, Drozdz J, Kurpesa M, Trzos E, Kasprzak JD. Age-dependency of classic and new parameters of diastolic function. Echocardiography 2008;25: 149 –155. Sagie A, Benjamin EJ, Galderisi M, Larson MG, Evans JC, Fuller DL, Lehman B, Levy D. Reference values for Doppler indexes of left ventricular diastolic filling in the elderly. J Am Soc Echocardiogr 1993;6:570 –576. Persson H, Lonn E, Edner M, Baruch L, Lang CC, Morton JJ, Ostergren J, McKelvie RS. Diastolic dysfunction in heart failure with preserved systolic function: need for objective evidence: results from the CHARM Echocardiographic Substudy-CHARMES. J Am Coll Cardiol 2007;49:687 –694. Schotten U, Neuberger HR, Allessie MA. The role of atrial dilatation in the domestication of atrial fibrillation. Prog Biophys Mol Biol 2003;82:151 –162. Vasan RS, Larson MG, Levy D, Galderisi M, Wolf PA, Benjamin EJ. Doppler transmitral flow indexes and risk of atrial fibrillation (the Framingham Heart Study). Am J Cardiol 2003;91:1079 – 1083. Nagueh SF, Appleton CP, Gillebert TC, Marino PN, Oh JK, Smiseth OA, Waggoner AD, Flachskampf FA, Pellikka PA, Evangelista A. Recommendations for the evaluation of left ventricular diastolic function by echocardiography. J Am Soc Echocardiogr 2009;22:107 –133. Lester SJ, Tajik AJ, Nishimura RA, Oh JK, Khandheria BK, Seward JB. Unlocking the mysteries of diastolic function: deciphering the Rosetta Stone 10 years later. J Am Coll Cardiol 2008;51:679 –689. Rakowski H, Appleton C, Chan KL, Dumesnil JG, Honos G, Jue J, Koilpillai C, Lepage S, Martin RP, Mercier LA, O’Kelly B, Prieur T, Sanfilippo A, Sasson Z, Alvarez N, Pruitt R, Thompson C, Tomlinson C. Canadian consensus recommendations for the measurement and reporting of diastolic dysfunction by echocardiography: from the Investigators of Consensus on Diastolic Dysfunction by Echocardiography. J Am Soc Echocardiogr 1996;9:736–760. Lubien E, DeMaria A, Krishnaswamy P, Clopton P, Koon J, Kazanegra R, Gardetto N, Wanner E, Maisel AS. Utility of B-natriuretic peptide in detecting diastolic dysfunction: comparison with Doppler velocity recordings. Circulation 2002;105:595 –601. Kannel WB, Wolf PA, Benjamin EJ, Levy D. Prevalence, incidence, prognosis, and predisposing conditions for atrial fibrillation: population-based estimates. Am J Cardiol 1998;82:2N –9N. Tedrow UB, Conen D, Ridker PM, Cook NR, Koplan BA, Manson JE, Buring JE, Albert CM. The long- and short-term impact of elevated body mass index on the risk of new atrial fibrillation the WHS (women’s health study). J Am Coll Cardiol 2010;55:2319 –2327. 912 41. McManus DD, Corteville DC, Shlipak MG, Whooley MA, Ix JH. Relation of kidney function and albuminuria with atrial fibrillation (from the Heart and Soul Study). Am J Cardiol 2009;104:1551 –1555. 42. Grimsmo J, Grundvold I, Maehlum S, Arnesen H. High prevalence of atrial fibrillation in long-term endurance cross-country skiers: echocardiographic findings and possible predictors—a 28 –30 years follow-up study. Eur J Cardiovasc Prev Rehabil 2010;17:100 –105. M.A. Rosenberg et al. 43. Kang H, Bae BS, Kim JH, Jang HS, Lee BR, Jung BC. The relationship between chronic atrial fibrillation and reduced pulmonary function in cases of preserved left ventricular systolic function. Korean Circ J 2009;39:372 –377. 44. Stork T, Mockel M, Danne O, Ewert C, Muller R, Bodemann T Eichstadt H, Hochrein H. Age-related hemodynamic changes during diastole: a combined M-mode and Doppler echo study. Int J Card Imaging 1990;6: 23 –30.