* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Primer Perkütan Koroner Işlem Sonrasında Clopidogrel Kullanımına
Cardiovascular disease wikipedia , lookup
Cardiac surgery wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
History of invasive and interventional cardiology wikipedia , lookup
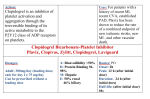
Primer Perkütan Koroner Işlem Sonrasında Clopidogrel Kullanımına Bağlı Diffüz Alveoler Hemoraji Adnan Kaya, Sami Ilhan, Mustafa Adem Tatlisu, Bayram Koroglu, Ahmet Oz Dr. Siyami Ersek Göğüs Kalp ve Damar Cerrahisi Eğitim ve Araştırma Hastanesi, İstanbul, Türkiye Antitrombotik ilaçlar stabil anjina pektoris ve akut koroner sendrom (Kararsız angina pektoris, ST segment yükselmesiz MI, ST segment yükselmeli MI) ile başvuran hastalar için olmazsa olmaz ve en uygun ilaç tedavisidir. Antiplatelet ve antikoagülan ilaçlar, akut koroner sendromda (AKS) ölüm ve transmural miyokard infarktüsü insidansını azalttı. Bu ilaçların trombüs oluşumunu engelleme ve trombositleri inhibe etme mekanizması ile benzer şekilde kanama riskini artırırlar. Burada göğüs ağrısı ile kliniğimize başvuran ve anterior miyokard infarktüsü tanısı konulan bir olgu sunulmuştur. Hastaya rutin klopidogrel 600 mg ve asetilsalisilic asit 300 mg oral başalndıktan sonra LAD’ye predilatasyon ve stent implantasyonu uygulandı. Klopidogrel alınmasından iki saat sonra koroner yoğun bakım ünitesindeki takibinde kanlı balgam ve nefes darlığı gelişti. Toraks yüksek rezonans bilgisayarlı tomografide diffüz alveoler hemoraji saptandı ve klopidogrel kesildi. Klopidogrele bağlı diffüz alveoler hemoraji çok nadir görülen bir komplikasyon olamakla birlikte bu ilacın ne kadar sıklıkta kullanıldığı düşünülürse tanı ve tedavinin önemi ortaya çıkar. Anahtar Kelimeler: Akut anteriyor myokard infarktüsü, klopidogrel kullanımı, diffüz alveolar hemoraji Diffuse Alveolar Hemorrhagea Due to Clopidogrel Use in A Patient Who Has Undergone Primary Percutaneouse Intervention Adnan Kaya, Sami Ilhan, Mustafa Adem Tatlisu, Bayram Koroglu, Ahmet Oz Dr. Siyami Ersek Cardiovascular Surgery Hospital, Istanbul, Turkey Antithrombotic drugs are inevitable and most suitable drug therapy for the patients presenting with stable angina pectoris and acute coronary syndromes (Unstable angina pectoris, Non-ST segment elevation MI, ST segment elevation MI). Antiplatelet and anticoagulant drugs has reduced the incidence of death and transmural myocardial infarction in acute coronary syndromes (ACS). Besides their favorable effect to inhibit thrombus formation, platelet inhibition in ACS by the same mechanism they increase bleeding risk. Here we present a case admitted to our institution with chest pain and in whom anterior myocardial infarction was diagnosed. After routine antiplatelet therapy with asetilsalisilic asit 300 mg per oral and clopidogrel 600 mg per oral the patient has undergone primary percutaneuse intervention which ended with predilatation and stent implantation of LAD. After two hour of ingestion clopidogrel the patient presented with bloody sputum and dyspnea in coronary care unit just after the intervention. Thorax high resonance computerized tomography (HRCT) revealed diffuse alveolar hemorrhagea in the case and clopidogrel stopped. Diffuse alveolar hemorrhagea due to clopidogrel is a very rare major complication and as we take into consideration how commonly it is used, diagnosis and management of this complication is crucial. Key words: Acute anterior Myocard Infarction, Clopidogrel Use, Diffuse alveolar Hemorrhagea, Complication Introduction The treatment combination of clopidogrel and aspirin reduces systemic ischemic events after percutaneous coronary intervention (PCI) in high risk patients (1-2). Additional anti trombotic drugs like GPIIb/IIIa inhibitors increase risk of minor and major bleeding as a side effect. Gastrointestinal bleeding is especially showed in GPIIb/IIIa inhibitors as a major bleeding complication. Here we discuss a patient who had a diffuse alveolar hemorrhage after primary percutaneous intervention which was attributed to clopidogrel. Case Report A 56-year-old male was referred to our tertiary cardiovascular and thoracic surgery center from an emergency department of general hospital. On his arrival he had a strong retrosternal chest pain which was radiating to left shoulder and both arms. In his medical history, he had HT treated with angiotensin receptor blockers, DM treated with subcutaneous insuline injections. In 2005 he had been amputated on his right foot under the knee because of diabetic foot. From this date asetilsalisilicasit 100 mg per orally once a day has started because of risk factors of coronary artery disease and peripheral artery disease. In his physical examination blood pressure was 137/89 mmHg, heart rate was 76 bpm, body temperature 37.1C and respiratory rate was 14/minute. Hemoglobin was 14.8 g/dL, white blood cell count was 15.300/mm3 and platelets were 290.000 /mm3. Creatinine kinase myocardial band(CK-MB) and troponin were positive. The electrocardiography revealed acute anterior myocardial infarction with ST segment elevation from V1 to V4 in precordial leads. As soon as the patient loaded with 600 mg clopidogrel and chewable aspirin 300 mg a diagnostic coronary angiography was made. The coronary angiography revealed total occlusion of proximal LAD with no antegrade and retrograde blood flow, a critical stenosis of distal right coronary artery( RCA) and proximal and mid significant stenosis of circumflex artery. Percutaneous coronary intervention planned to total occlusion of proximal LAD. After administration of 5,000 units of heparin the lesion passed with wire and predilatation with 2x20 mm size balloon (Invader, Alvimedica) was made. A bare metal stent of size 3X24 mm (Ephesos, Alvimedica) was implanted. LAD distal blood flow was TIMI-3 and the intervention ended. The patient admitted to intensive coronary care unit after PCI which took one hour with good hemodynamic parameters of 130/70 mmHg blood pressure and 73 bpm heart rate. One hour later we were alerted by the nurses that the oxigen saturation of patient’s has dropped 72 % by pulse oximetry and the patient started to cough. Rales in both lower segments of lungs were present in physical examination. Bloody sputum was observed and arterial blood gas confirmed decreased oxigen saturation to 70 %. The patients activated clotting time (ACT) was 227 seconds in intervention room and was 201 seconds after bloody cough. Immediate chest X-ray at bed side showed pulmonary edema like infiltration of both mid and basal segment of lungs. The patient took ortopnea position in bed despite the right femoral sheath. 2D echocardiography at bed side showed decreased ventricular performance (EF) to 30% with anterior and anteroseptal hypokinesia. Ruling out acute mitral regurgitation and papillary muscular rupture, continuous positive air pressure (CPAP) started and consultation of chest disease is demanded. 40 mg furosemide intravenous administered . After 45 minutes on CPAP therapy finally the oxigen saturation of the patient increased to 86% which was enough to transfer the patient to reveal computerized tomography of thorax which was ordered by the consultant of chest disease. Thorax high resonance computerized tomography (HRCT) demonstrated ARDS like bilateral ground glass opacities of lungs (Figure-1,2). Careful investigation of CT revealed ground glass opacities of lungs were accumulated in the posterior sides of the lungs (Figure-3) which was appropriate with the lying position of the patient. For the first time diffuse alveolar hemorrhage was taught to be cause of the clinical compromise of the patient. Repeated complete blood count (CBC) and activated clotting time testes were done. Hemoglobin dropped from 14.8 gr/dL to 11.1 gr/d L and the maximal ACT was 227 seconds which were obtained in the catheter laboratory. Bronchoscopic examination showed clots and blood in the trachea and bronchial tree without active bleeding which was conformation of diagnosis of diffuse alveolar hemorrhage one day later. Clopidogrel was stopped as an etiologic agent of this complication. We followed up the patient one week under aspirin and low molecular weight heparin (LMWH) without any more complication. The patient was transferred to cardiovascular surgery for revascularization of CX and RCA. Discussion Diffuse alveolar hemorrhage is an active bleeding into the alveolar space. It is usually associated with connective tissue disorders like microscopic poliangitis, Goodpasture’s syndrome, antiphospholipid antibody syndrome, Wegener’s disease where the working mechanism of bleeding is injured vessel walls due to immune reactions. Diffuse alveolar hemorrhage which is associated to antithrombotic drugs is not common. As the current guidelines suggest combination of different antithrombotic drugs in treatment of thrombosis for their additive effect bleeding as a side effect become obvious. Clopidogrel and glycoprotein IIb/IIIa inhibitors are recommended in the treatment of patients with unstable angina pectoris and NSTEMI(3) and current treatment guidelines for ST elevation myocardial infarction recommend that clopidogrel should be given for at least 12 months(4). DAH commonly described in patients under glycoprotein IIb/IIIa inhibitors therapy. A study conducted by Ali et al (5) found out the prevalence of pulmonary hemorrhage 0.5% for eptifibatide, 0.7% for abciximab, and 0.9% for tirofiban. Only 10 of the 5,382 patients (0.19%) who received abciximab in four clinical trials developed pulmonary hemorrhage (6). Ikeda et al (7) reported a case of DAH after coronary stent implantation in ST elevation myocardial infarction with aspirin and ticlopidine therapy and Kilaru et al (8) reported the first case of DAH after placement of a coronary stent with clopidogrel therapy. When the clinical situation of patient raises doubt of DAH conformation of the diagnosis with adjunct laboratory tests and imagining must be done as soon as possible. Contrast enhanced chest CT scan and bronchoscopic examination of air ways are preferred tools for diagnosis. Here we present a case admitted to our institution with anterior myocardial infarction and in whom DAH was diagnosed after two hours of 600 mg of clopidogrel ingestion. Here in this case this side effect was attributed to clopidogrel because the patient was already taking aspirin and the activated clotting time (ACT) was in normal therapeutic range. Yet the time interval from ingestion to bleeding also is suggestive for clopidogrel associated DAH. This must be third case report of DAH associated with clopidogrel use after Kilaru et al (8) and Kim et al(9) in the literature. Conclusion Diffuse alveolar hemorrhage (DAH) is a mortal bleeding complication of antithrombotic drugs if misdiagnosed. Clinical findings like compromise in hemodynamic, dyspnea, arterial oxigen saturation drop, hemoptysis, infiltration in chest X-ray, ARDS like chest CT findings, un explained hemoglobin drop, utilization of antithrombositer or anticoagulant drugs may help making diagnose of DAH. DAH as a complication of clopidogrel use is very rare to be found. If DAH is occurred, discontinuance of causative drug is advised. Acknowledgements None References 1. Peters RJ, Mehta SR, Fox KA, et al. Effects of aspirin dose when used alone or in combination with clopidogrel in patients with acute coronary syndromes: observations from the Clopidogrel in Unstable angina to prevent Recurrent Events (CURE) study. Circulation 2003;108: 1682-7. 2. Mehta SR, Tanguay JF, Eikelboom JW, et al. Double-dose versus standard- dose clopidogrel and high-dose versus low-dose aspirin in individuals undergoing percutaneous coronary intervention for acute coronary syndromes (CURRENT-OASIS 7): a randomised factorial trial. Lancet 2010;376:123343. 3. Braunwald E, Antman EM, Beasley JW, et al. ACC/AHA guidelines for the management of patients with unstable angina and non-ST-segment elevation myocardial infarction. A report of the American College of Cardiology/ American Heart Association task force on practice guidelines. J Am CollCardiol 2000;36:970–1062. 4. Kushner FG, Hand M, Smith SC Jr, et al. 2009 focused updates: ACC/ AHA guidelines for the management of patients with ST-elevation myocardial infarction (updating the 2004 guideline and 2007 focused update) and ACC/AHA/SCAI guidelines on percutaneous coronary intervention (updating the 2005 guideline and 2007 focused update) a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2009;54:2205-41. 5. Ali A, Hashem M, Rosman HS, Kazmouz G, Gardin JM, Schrieber TL. Use of platelet glycoprotein IIb/IIIa inhibitors and spontaneous pulmonary hemorrhage. J Invasive Cardiol 2003;15(4):186-8. 6. Cohen SA, Effron MB. Abciximab and alveolar hemorrhage. N Engl J Med 1998;339:1861-1863 7. Ikeda M, Tanaka H, Sadamatsu K. Diffuse alveolar hemorrhage as a complication of dual antiplatelet therapy for acute coronary syndrome. Cardiovasc Revasc Med 2011;12:407 11. 8. Kilaru PK, Schweiger MJ, Kozman HA, Weil TR. Diffuse alveolar hemorrhage after clopidogrel use. J Invasive Cardiol 2001;13:535-7. 9. Kim, Y., Lim, J., Lim, J., Kim, S., Jung, T., & Choi, W. (2013). Pulmonary Alveolar Hemorrhage after Clopidogrel Use for ST Elevation Myocardial Infarction. Korean Circulation Journal, 43(7), 497–499. doi:10.4070/kcj.2013.43.7.497 Figure Legends Figure-1; Coronal cut view of thorax contrast enhenced computerized thomogrphy showed diffuse ground glass opacities of both lungs. Figure-2; Transvers cut view of thorax contrast enhenced computerized thomography showed ground glass opacities of posterior segment of lungs. Figure-3; Sagittal cut view of thorax contrast enhenced computerized thomography showed ground glass opacities of posterior segment of lungs.