* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Transcutaneous Cardiac Pacing
Survey
Document related concepts
Transcript
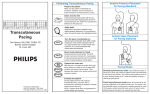
HUP Hospital of the University of Pennsylvania Clinical Practice Policy/Procedure KEYWORDS: NURSING 4B-04-07 Nursing Practice Manual Transcutaneous Cardiac Pacing Page 1 of 8 POLICY Cardioversion Defibrillation Epicardial Pacemaker External Pacemaker HeartStart MRx HeartStart XL Permanent Pacemaker Transthoracic Pacemaker Transvenous Pacemaker Transcutaneous pacing is a method of stimulating the myocardium through the chest wall via two large pacing electrodes. The use of a transcutaneous pacemaker may be initiated by an Emergency Department, Adult Intensive Care Unit or Intermediate Care Unit Registered Nurse for cardiac pacing as indicated below, as an alternative to endocardial stimulation. The nurse will initiate this procedure when prescribed by a physician/NP/PA. On general care units, the physician/NP/PA will initiate and manage this therapy. The physician/NP/PA will stay with the patient as an urgent transfer to a higher level of care is arranged. REFER TO: SCOPE 1-12-11 Administration of Moderate Sedation for Diagnostic or Therapeutic Intervention All Registered Nurses in the Emergency Department, Adult Intensive Care and Intermediate Care Units. BCC-01-02 Defibrillation A. Transcutaneous pacing is indicated in patients with hemodynamically unstable bradycardias unresponsive to pharmaceutical intervention. B. Transcutaneous pacing is most useful in those patients in whom the slow heart rate is the most likely cause of the inadequate perfusion. C. Bradycardia resulting from inadequate circulating volume or hypoxia is NOT managed by transcutaneous pacing (e.g., hypothermia, hypovolemia, hypoxia, shock). D. Transcutaneous pacing is indicated in high degree heart block: Mobitz type II, second degee block or third degree block. E. Transcutaneous pacing is NOT recommended for asystole or INDICATIONS BCC-01-03 Synchronized Cardioversion FORMS: Code Recording Form 135000-3 Sedation/Analgesia Monitoring Flowsheet Page1 HUP-105A-2 Page2 HUP-105B-2 PEA. Begin CPR. SUPPLIES A. Transcutaneous pacemaker (defibrillator/AED) with monitor: Philips HeartStart MRx or HeartStart XL or Agilent heartstream XL. HUP Clinical Practice Policy/Procedure Hospital of the University of Pennsylvania NURSING 4B-04-07 Nursing Practice Manual Transcutaneous Cardiac Pacing Page 2 of 8 Philips HeartStart XL Philips HeartStart MRx Agilent heartstream XL HUP Clinical Practice Policy/Procedure Hospital of the University of Pennsylvania NURSING 4B-04-07 Nursing Practice Manual Transcutaneous Cardiac Pacing Page 3 of 8 B. Hands free cable. C. Hands free pacing pads: “ConMed Padpro Defibrillation/Pacing/Cardioversion/Monitoring Electrodes": Lawson # 145327 D. Electrocardiogram (ECG) cable: “3 lead cable”: Lawson #204335 E. ECG electrodes: “EKG Q-Tracer”: Lawson #124542 F. Monitor recorder paper: “Medi-trace paper”: Lawson #100849 G. Advanced cardiac life support (ACLS) equipment. H. Sedatives or analgesics as indicated. PROCEDURE A. B. Preparation 1. Explain procedure to patient or family member as necessary. Inform the patient of potential sensations and that sedation may be necessary. 2. Verify the patient’s identity using two unique identifiers. 3. Verify that informed consent has been obtained in non-emergency situations. 4. Perform hand hygiene and apply gloves. 5. Obtain baseline vital signs. 6. Assess patients pain status and administer analgesics and/or sedation as indicated and prescribed. 7. Prepare the patient's chest and back as needed by clipping excess hair. Do not shave. Connection 1. Turn power to external pacing unit on. NOTE: Note the ECG cannot be slaved off the bedside monitor. The pacing output will destroy the bedside monitor. 2. Place ECG leads on the patient and connect leads to the proper cable. Select a lead to display a clear ECG waveform with an upright R wave. 3. Securely connect pacing electrodes to pacing cable. 4. Peel off protective covering from pacing electrodes and place pacing electrodes on the patient in either anterior/lateral position or anterior/posterior position. The electrodes should not be placed over wires, drains, dressings, ECG electrodes, implanted HUP Clinical Practice Policy/Procedure Hospital of the University of Pennsylvania NURSING 4B-04-07 Nursing Practice Manual Transcutaneous Cardiac Pacing Page 4 of 8 cardioverters/defibrillators, pacemakers, or medication patches. Do not place pads over open incisions, cuts, sores, or metal objects. See images 3 and 4. Image 3: Anterior/lateral lead placement: Anterior/lateral placement: The negative electrode is placed on the left lateral chest over the fourth intercostal space in the midaxillary line. The positive electrode is placed on the anterior right in the subclavicular area. Image 4: Anterior/posterior lead placement: Anterior/posterior placement: The negative lead is placed on the left anterior chest, about halfway between the xiphoid process and the left nipple with the upper edge of the electrode just below the nipple line. The positive lead is placed on the left posterior chest just below the scapula and lateral to the spine. Note: In female patients, position the negative electrode under the breast. C. Initiate Pacing 1. Print a rhythm strip of the patient’s baseline rhythm. 2. Select the pacing rate as determined by the physician/NP/PA. The rate range is typically 60 to 100 beats/min to maintain an adequate cardiac output. HUP Clinical Practice Policy/Procedure D. Hospital of the University of Pennsylvania NURSING 4B-04-07 Nursing Practice Manual Transcutaneous Cardiac Pacing Page 5 of 8 3. Select the desired mode of pacing, either "demand" or "fixed" mode. • Demand: This mode of pacing uses the sensing function to pace. In the demand mode the pacemaker will "sense" the patient's intrinsic rate and will only pace when the patient's own heart rate drops below the preset rate set on the transcutaneous pacemaker. • Fixed: In this mode the pacer will pace at the set rate independent of the patient's own rate. The use of this mode is rare. 4. Press stop/start button. 5. Set current output (mA) as follows: Set pacer to demand mode. Increase mA from minimum setting until capture is achieved (indicated by a widened QRS, > 0.12 msec, and broad T wave after each pacer spike). Maintenance pacing outputs should be set at approximately 10 mA above the threshold. NOTE: milliampere (mA) is the amount of electricity sent through the pacing pads in order to stimulate the heart. Determining Capture and Optimal Threshold 1. Determining Capture: It is important to recognize when stimulation has produced a ventricular response. Ventricular response is normally characterized by suppression of intrinsic QRS and production of an ectopic QRS complex and T wave. Capture can also be confirmed by auscultation and by palpation of the pulse. a. Auscultate and/or palpate for a pulse to ascertain mechanical capture. It is safe to touch the patient while pacing. Refrain from touching the gelled portion of the hands free pacing pad. A minor electrical shock hazard exists. Observe the patient for evidence of improved perfusion. Skeletal muscle twitching should be expected but is not an indication of pacing capture. b. If electrical and mechanical capture/pulse is obtained then check for a blood pressure. It is often difficult to assess the pulse or blood pressure during pacing due to muscle contractions. Using the right side of the body for pulse and BP assessments may be helpful. c. A pulse oximeter is a powerful tool when used in conjunction with the pacer/ECG monitor for confirming capture because both mechanical and electrical activities can be measured. ECG alone is not enough to verify that the patient's heart is providing cardiac output. d. Patients response to pacing must be verified by signs of improved cardiac output, such as: a palpable pulse rate the same as the rate which paced pulses are being delivered, a rise in blood pressure, and/or improved skin color. e. If patient's mental status improves then physician/NP/PA may order sedation for patient discomfort secondary to muscular contractions of the chest wall. Use Sedation/Analgesia Monitoring Flowsheet Page1 HUP-105A-2 Page2 HUP105B-2. HUP Hospital of the University of Pennsylvania Clinical Practice Policy/Procedure 1. NURSING 4B-04-07 Nursing Practice Manual Transcutaneous Cardiac Pacing Page 6 of 8 HUP Nursing Policy Administration of Sedation/Analgesia 1-12-11 Capture 2. E. Determining Optimal Threshold: The ideal output current (mA) is the lowest value that will maintain capture. This is usually about 10% above threshold. Trouble Shooting Transcutaneous Pacing If the pacemaker spike is not in front of each QRS complex, then one of two problems may exist: 1. Failure to Capture: Failure to obtain capture occurs in demand and fixed mode. Increasing the OUTPUT (mA) may obtain capture. Be sure the pads have good skin contact. Check for correct pad placement. Failure to Capture 2. Undersensing: This problem occurs in demand mode only and is seen when the pacemaker discharges immediately after the patient's own QRS complex (the discharge occurs in the refractory period of the heart). In this case, the pads are not sensing the patient's heartbeat. Select a different monitoring lead or reposition the pads. Fixed pacing may be indicated. HUP Clinical Practice Policy/Procedure Hospital of the University of Pennsylvania NURSING 4B-04-07 Nursing Practice Manual Transcutaneous Cardiac Pacing Page 7 of 8 Undersensing F. G. Post Procedure Monitoring and Care 1. Provide continuous cardiac monitoring. 2. Reassess the patient’s comfort level and toleration of the interventions. 3. Obtain vital signs at least hourly. 4. Document the procedure and patient response per unit policy. 5. Consider transfer of patient to higher level of care. Complications with Transcutaneous Pacing 1. VF will not respond to pacing. It requires immediate electrical defibrillation. 2. Pulseless electrical activity (PEA) may occur following prolonged cardiac arrest or in other disease states with myocardial depression. In such instances, pacing may produce ECG response without effective mechanical contractions (PEA). 3. In presence of generalized hypoxia, myocardial ischemia, cardiac drug toxicity, electrolyte imbalance, and other cardiac diseases, pacing may evoke repetitive responses, tachycardia, or fibrillation. Defibrillation should always be readily available and extra caution is needed to keep stimulus amplitude just above threshold. 4. Pacing by any method tends to inhibit intrinsic rhythm. Abrupt cessation of pacing, particularly at rapid rates, can cause ventricular standstill and can be avoided by gradually turning down the pacing rate until an intrinsic QRS rhythm emerges. 5. The transcutaneous pacemaker may cause discomfort of varying intensity, which can be severe and preclude its continued use in conscious patients; unavoidable skeletal muscle contraction may be troublesome in very sick patients and may limit continuous use to a few hours. Erythema of the skin under the electrodes often occurs but is inconsequential. HUP Hospital of the University of Pennsylvania Clinical Practice Policy/Procedure NURSING 4B-04-07 Nursing Practice Manual Transcutaneous Cardiac Pacing Page 8 of 8 6. The transcutaneous pacemaker may cause skin breakdown. 7. This pacer is not appropriate for connection to internal pacer electrodes in contact with the myocardium. 8. Avoid touching the gelled area of the electrode while pacing. A minor electrical shock hazard exists. H. Defibrillator Controls. Please see HUP Nursing Policy BCC-01-02 Defibrillation. I. Cardioversion and Defibrillation. Cardioversion. Please see HUP Nursing Policy BCC-01-03 Synchronized REFERENCES American Heart Association (AHA). (2005). American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation, 112 (Suppl IV).Available online at www.circulationaha.org Best practices: Evidence-based nursing procedures Lippincott Williams & Wilkins, 263. Accessed 12/2010. Mosby’s Online Nursing Skills Resource: Transcutaneous Cardiac Pacing. Accessed 12/2010. HeartStart MRx HeartStart XL Agilent Hearty Steam XL REVIEWS/APPROVALS HUP Nursing Practice Committee Supersedes: “Transcutaneous Pacemaker”, (General Care Practice Manual), March, 1998; December 2003. “Transcutaneous Pacemaker", (ICU Practice Manual) 12/95. “Transcutaneous Pacemaker", (Nursing Practice Manual) December 1, 2006 Effective Date: December 30, 2011 Disclaimer Any printed copy of this policy is only as current as of the date it was printed; it may not reflect subsequent revisions. Refer to the on-line version for most current policy. Use of this document is limited to University of Pennsylvania Health System workforce only. It is not to be copied or distributed outside the institution without administrative permission.