* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Newsletter FAQs
Survey
Document related concepts
Transcript
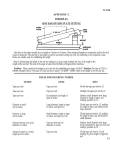
In this issue: ¾ Switching Antidepressants ¾ Omega 3 Fish Oils - Rx or OTC Newsletter FAQs Frequently Asked Questions – Winter 2010 SCORxE Newsletter FAQs shares highlights of answers to questions specifically asked by individual providers in the community. Such focus is not intended as an endorsement by SCORxE since a complete overview of a medical condition or situation is beyond the scope of the condensed newsletter format. The reader is responsible for using professional judgment in analyzing and interpreting this information before accepting and utilizing it in clinical practice. General Guidelines for Switching Antidepressant Medication (Following > 7 days exposure) First Antidepressant Switching To Discontinued Antidepressant Selective Serotonin Reuptake Inhibitor (SSRI) except Fluoxetine Fluoxetine (long half-life) SerotoninNorepinephrine Reuptake Inhibitor (SNRI) Bupropion Mirtazapine Nefazodone Tricyclic Antidepressant (TCA) Monoamine Oxidase Inhibitor (MAOI) Recommendation SSRI or Mirtazapine SNRI Bupropion or TCA Nefazodone MAOI Switch directly or cross taper Switch directly Cross taper, start with low dose if choose a TCA Taper SSRI prior to starting nefazodone Taper and allow 5 half-life wash out (1 week) – DO NOT COMBINE SSRI or Mirtazapine SNRI Bupropion or TCA Nefazodone MAOI SSRI or SNRI Bupropion, Mirtazapine, Nefazodone, or TCA MAOI Switch directly or cross taper start with a low antidepressant dose, consider allowing a 4-7 Switch directly day wash out period prior to Cross taper starting new antidepressant Taper prior to starting nefazodone Taper and allow 5 half-life wash out (5 weeks) – DO NOT COMBINE Switch directly or cross taper Cross taper SSRI, SNRI, Mirtazapine, or Nefazodone TCA MAOI SSRI SNRI, Bupropion, Nefazodone, or TCA MAOI SSRI SNRI, Bupropion, Mirtazapine, or TCA MAOI SSRI, SNRI, Bupropion, Mirtazapine, or Nefazodone TCA MAOI Switch directly SSRI, SNRI, Bupropion, Mirtazapine, Nefazodone, TCA, or MAOI Taper and allow 5 half-life wash out (1 week) – DO NOT COMBINE Cross taper and start with low TCA dose Taper and allow 5 half-life wash out (3-5 days) – DO NOT COMBINE Switch directly or cross taper Cross taper Taper and allow 5 half-life wash out (1 week) – DO NOT COMBINE Taper nefazodone prior to starting SSRI Cross taper Taper and allow 5 half-life wash out (1 week) – DO NOT COMBINE Cross taper Switch directly using equivalent doses Taper and allow 5 half-life wash out (1-2 weeks depending on TCA) – DO NOT COMBINE Taper and allow 14 day wash out – DO NOT COMBINE Reverse page contains more information comparing the different strategies for switching antidepressants. What are some important considerations that influence antidepressant switching strategies? SWITCHING to a different antidepressant requires consideration of patient preference, safety, adverse effects, potential medication interactions, pharmacokinetics, and cost. In general, if the first antidepressant is being discontinued due to intolerance following a brief exposure (< 7 days), it can be stopped and the second medication started (a direct switch). If the first drug is being discontinued due to symptomatic breakthrough or inadequate response after a longer exposure (more than 7 days), the approach selected should be based on the risk of discontinuation symptoms, side effects, and drug interactions. Switching may be accomplished by direct switching, medication tapering, cross tapering, or a wash out period. Tapering is advised with some medications. For example, abrupt discontinuation of any drug with anticholinergic side effects (e.g., tricyclic antidepressants) can cause cholinergic rebound; and abrupt discontinuation of some antidepressants can cause serotonin discontinuation syndrome. Serotonin discontinuation syndrome is more likely with: more than 5 weeks of therapy; higher doses; and use of medications with short halflives (e.g., paroxetine, venlafaxine). In cross tapering, the first medication dose is decreased over 3-7 days while initiating the new antidepressant. A wash out period between the first and second antidepressant may be necessary if there are clinically significant medication interactions. How does Lovaza® (GlaxoSmithKline) – an omega-3 fatty acid prescription product – compare to over-the-counter fish oil products to improve lipid profiles? After addressing life-style issues and ruling out diseases and medications (e.g., beta blockers, thiazides, estrogens) that can worsen lipid profiles, pharmacotherapy can help patients manage their dyslipidemia. Patients may self-treat with over-the-counter (OTC) fish oil supplements to benefit from the omega-3 fatty acids (FAs); now, a prescription (Rx) product, Lovaza®, is FDA approved as an adjunct to dietary modifications in patients with very high triglyceride levels (> 500 mg/dL). Each highly concentrated capsule (840 mg omega-3 FAs) contains two highly purified omega-3-acid ethyl esters, eicosapentaenoic acid (EPA) (465 mg) and docosahexaenoic acid (DHA) (375 mg). Patients may also request OTC fish oil products to self treat or save money if Lovaza® is not covered by insurance. There are no data comparing Lovaza® to OTC products. Most OTC dietary supplements contain about 200 – 400 mg omega-3 FAs per capsule despite being labeled with 1000 – 1200 mg fish oil. In general, OTC products have fewer quality control requirements compared to prescription medications. However, both Rx and OTC products are free of methylmercury and polychlorinated biphenyls (PCBs). The use of omega-3 FAs requires some careful considerations. In general, adverse effects are dose related. Omega-3 FAs can have antiplatelet effects, so use with other drugs that have antiplatelet or anticoagulant activity (e.g., aspirin, clopidogrel [Plavix®], selective serotonin-reuptake inhibitors, nonsteroidal anti-inflammatory agents, warfarin [Coumadin®]) should be closely monitored. Additionally, fish oil can increase LDLs (as much as 45% reported with Lovaza®, although there is no increase in atherogenic LDL particles), and at higher doses can worsen glycemic control in patients with diabetes. Currently, there are no data on morbidity/mortality specifically with Lovaza®. There is conflicting evidence of the health benefits of omega-3 FAs in primary and secondary prevention of cardiovascular disease (CVD), and the ideal intake of omega-3 FAs remains unclear. The American Heart Association (AHA) currently recommends the following: Population Recommendation Individuals without documented coronary heart disease (CHD) Individuals with CHD Individuals with high triglycerides (Individuals consuming > 3 grams omega-3 FAs from capsules should be under medical supervision to monitor for excessive bleeding) Eat fatty fish (e.g., mackerel, lake trout, herring, sardines, albacore tuna, salmon) at least twice a week. Include oils and foods rich in alpha-linolenic acid* (flaxseed, canola and soybean oils; flaxseed, walnuts, tofu and other forms of soybeans) About 1 gram daily of DHA plus EPA from fatty fish (preferred) or supplements under medical supervision 2 – 4 grams daily of DHA plus EPA provided as capsules under medical supervision * Alpha-linolenic acid can convert to omega-3 FAs in the body but the extent is modest and controversial. For more information about the consumption of fish and fish oils see: Anon. Fish and omega-3 FAs: American Heart Association Recommendation. Available at: http://www.americanheart.org/presenter.jhtml?identifier=4632. This address includes the link to the full 2002 scientific statement released by the American Heart Association entitled, Fish Consumption, Fish Oil, Omega-3 Fatty Acids and Cardiovascular Disease. References for this issue and additional information are available upon request from your SCORxE consultant, or send an email to [email protected]. For more information about our service, please call (843) 792-5915, or visit www.sccp.sc.edu/SCORxE.