* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Body mass index predicts discontinuation due to ineffectiveness and
Pharmacognosy wikipedia , lookup
Drug interaction wikipedia , lookup
Adherence (medicine) wikipedia , lookup
Prescription drug prices in the United States wikipedia , lookup
Drug design wikipedia , lookup
Neuropharmacology wikipedia , lookup
Polysubstance dependence wikipedia , lookup
Pharmaceutical industry wikipedia , lookup
Drug discovery wikipedia , lookup
Theralizumab wikipedia , lookup
Prescription costs wikipedia , lookup
Pharmacokinetics wikipedia , lookup
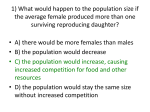
BJD British Journal of Dermatology M E D I C A L D E R MA T O L O GY Body mass index predicts discontinuation due to ineffectiveness and female sex predicts discontinuation due to side-effects in patients with psoriasis treated with adalimumab, etanercept or ustekinumab in daily practice: a prospective, comparative, long-term drug-survival study from the BioCAPTURE registry* J. Zweegers,1 J.M.P.A. van den Reek,1 P.C.M. van de Kerkhof,1 M.E. Otero,1 A.L.A. Kuijpers,2 M.I.A. Koetsier,3 W.P. Arnold,4 M.A.M. Berends,5 L. Weppner-Parren,6 P.M. Ossenkoppele,7 M.D. Njoo,7 J.M. Mommers,8 P.P.M. €mig,1 R.J.B. Driessen,1 W. Kievit9 and E.M.G.J. de Jong1,10 van Lu 1 Department of Dermatology and 9Department of Epidemiology, Biostatistics and Health Technology Assessment, Radboud University Medical Center, Nijmegen, the Netherlands 2 Maxima Medisch Centrum, Eindhoven/Veldhoven, the Netherlands 3 Gelre Ziekenhuizen, Apeldoorn, the Netherlands 4 Ziekenhuis Gelderse Vallei, Ede, the Netherlands 5 Slingeland Ziekenhuis, Doetinchem, the Netherlands 6 Jeroen Bosch Ziekenhuis, Den Bosch, the Netherlands 7 Ziekenhuisgroep Twente, Almelo/Hengelo, the Netherlands 8 St Anna Ziekenhuis, Geldrop, the Netherlands 10 Radboud University, Nijmegen, the Netherlands Linked Comment: Egeberg. Br J Dermatol 2016; 175:247–248 Summary Correspondence Jeffrey Zweegers. E-mail: [email protected] Accepted for publication 19 February 2016 Funding sources This work was supported by the University Medical Centre St Radboud Foundation, which received funding from Pfizer, Janssen and AbbVie for the project. Pfizer, Janssen and AbbVie played no role in the design and execution of this study or in data collection, data management, data analysis, interpretation of the data, manuscript preparation, manuscript review or manuscript approval. Conflicts of interest See Appendix 1 below. *Plain language summary available online DOI 10.1111/bjd.14552 340 Background Predictors for successful treatment are important for personalized medicine. Predictors for drug survival of biologics in psoriasis have been assessed, but not split for different biologics or for the reason of discontinuation. Objectives To compare long-term drug survival between the outpatient biologics adalimumab, etanercept and ustekinumab in patients with psoriasis, and to elucidate predictors for overall survival and drug discontinuation due to ineffectiveness and side-effects for each biologic separately. Methods Ten years of data were extracted from the prospective, multicentre, longterm BioCAPTURE registry. Kaplan–Meier survival analyses and confounder-corrected multivariate Cox regression analysis for drug survival (MCR-DS) were performed to compare drug survival between biologics. To elucidate the predictors for different reasons of discontinuation for each biologic, univariate Cox regression analyses and multivariate Cox regression analyses for predictors (MCR-P) with backward selection were performed. Results In total, 526 treatment episodes – 186 adalimumab, 238 etanercept and 102 ustekinumab – were included covering 1333 treatment years. MCR-DS showed a significantly higher overall survival for ustekinumab compared with adalimumab and etanercept. MCR-P showed that higher body mass index (BMI) was a predictor for discontinuation due to ineffectiveness for etanercept and ustekinumab and that female sex was a predictor for discontinuation due to sideeffects for adalimumab, etanercept and ustekinumab. Conclusions Ustekinumab has the highest confounder-corrected long-term drug survival in psoriasis treatment, compared with adalimumab and etanercept. British Journal of Dermatology (2016) 175, pp340–347 © 2016 British Association of Dermatologists Long-term drug survival of biologics in psoriasis, J. Zweegers et al. 341 Higher BMI is a predictor for discontinuation due to ineffectiveness in etanercept and ustekinumab, and female sex is a consistent predictor for discontinuation due to side-effects in all three outpatient biologics. What’s already known about this topic? • • • Drug survival of biologics for psoriasis has been analysed, but few publications used prospective multicentre daily-practice data. These studies found that ustekinumab had the highest confounder-corrected overall drug survival, but they did not split survival analysis for the different biologics or for different reasons of discontinuation. Different predictors for overall drug survival were found in prospective and retrospective studies. What does this study add? • • • This study reports on a longer period of drug survival than previous studies. Ustekinumab has a higher confounder-corrected drug survival and higher survival for discontinuation due to ineffectiveness and side-effects than adalimumab and etanercept. Higher body mass index (BMI) predicts discontinuation due to ineffectiveness in etanercept and ustekinumab, and female sex is a consistent predictor for discontinuation due to side-effects in all three biologics. Adalimumab (ADA), etanercept (ETA) and ustekinumab (USTE) have enriched the therapeutic armamentarium of dermatologists by increasing the number of drugs available for outpatient psoriasis treatment.1 In order to optimize psoriasis treatment strategies in clinical practice, several real-world studies have assessed drug survival of individual biologics,2–8 compared drug survival between biologics9–18 or searched for clinical characteristics that might predict the discontinuation of biological agents.2–7,9,11,12 Drug survival is a comprehensive measure of effectiveness and safety and the preferences of both the patient and physician, and reflects the probability a patient will stay on the drug over time.19 Although drug survival is becoming an increasingly popular outcome measure in biological treatment of psoriasis, still only a limited number of daily-practice studies are available that used prospective data from multiple centres to compare biological agents.9–12 Also, several different clinical characteristics have been stated to predict treatment discontinuation in prospective and retrospective studies, but were usually analysed only for treatment discontinuation in general (i.e. overall drug survival) and for all included biologics instead of performing analysis for each biologic separately. This has the potential of missing important predictors, as predictors for discontinuation might differ between different reasons of discontinuation and between biologics. Among predictors for drug discontinuation in general, female sex is mentioned most often, especially in prospective studies.2,3,9,11,12,15 Female sex has also been found to predict overall survival of biological treatment in other inflammatory diseases.20 Thus far, research into predictors for © 2016 British Association of Dermatologists discontinuation split for ineffectiveness and side-effects has gained little attention. Moreover, the few studies that have addressed this issue have not been conducted with the same variables at the start, leading to a heterogeneity in the selection of candidate predictors.2,3 In the current study, drug survival of the three biologics was assessed with the aim to elucidate predictors for the drug survival of ADA, ETA and USTE both as a group and separately per biologic for overall drug survival, and drug failure due to ineffectiveness and side-effects. The study set out to elucidate the predictors for these most commonly prescribed outpatient biologics in a uniform way, by selecting the candidate predictors from a set of baseline variables that were similar for each biological treatment, and to elucidate predictors for different reasons of discontinuation for each biologic separately. This approach might aid physicians in their treatment strategies and increase awareness for those patients at risk of discontinuing that specific biological treatment. Patients and methods BioCAPTURE BioCAPTURE (Continuous Assessment of Psoriasis Treatment Use Registry with Biologics) is a registry with prospective clinical practice data on biological treatment of plaque psoriasis.10,21 Data from all real-world consecutive patients starting biological treatment from one academic and eight nonacademic centres were included. Patients participating in clinical trials were excluded. BioCAPTURE was approved by the British Journal of Dermatology (2016) 175, pp340–347 342 Long-term drug survival of biologics in psoriasis, J. Zweegers et al. medical ethics committee and, although not mandatory, informed consent was obtained from every patient. Patients with psoriasis were treated according to the European and Dutch guidelines,22,23 and treatment recommendations were made by the treating physician. Data extraction Patient characteristics and reason for treatment discontinuation (ineffectiveness, side-effects or other) were extracted from BioCAPTURE for all patients from the inception of the registry (2005) until May 2015. Baseline variables that were extracted were age at start of biologic; sex; weight; body mass index (BMI) divided into six categories9 (underweight < 185, normal weight 185–2499, overweight 250–2999, obese I 300–3499, obese II 350–3999, obese III > 40 kg m 2); positive family history of psoriasis; psoriatic arthritis; duration of psoriasis until start of biologic; baseline PASI score; biological naivety; antitumour necrosis factor (anti-TNF) naivety and the presence of at least one comorbidity in the medical history (hepatitis B or C, chronic kidney or liver disease, HIV or cancer, except for nonmelanoma skin cancer)2,24 that would have excluded the patient from participating in trials of biologics. When a patient had received different biologics over time, the first treatment episode of each biologic was used for analysis. In case the patient interrupted the biological treatment for ≤ 90 days, the treatment episode was considered to be continuous. Ninety days is a widely accepted maximum interruption period.9,10,15 All available long-term data were used for drug-survival and predictor analyses. Long-term drug-survival analysis Drug survival was analysed using Kaplan–Meier estimates. An event in the overall survival analysis was defined as any discontinuation of biological treatment. Additional analyses for the events ‘side-effects’ and ‘ineffectiveness’ were also carried out. Censoring was performed for patients still on biological treatment at the moment of data lock, or patients who were lost to follow-up or for reasons other than the reason of interest. For USTE the last date plus 8, 10 or 12 weeks, depending on the dosing regimen of the patient, was chosen for the primary analyses. As USTE has a low frequency of administration and the discontinuation date can influence drug survival, a sensitivity analysis was performed with the last date of injection of ustekinumab as the discontinuation date. This conservative approach is described in Appendix S1 (see Supporting Information). Confounder correction for long-term drug survival Baseline variables were compared between treatment groups using one-way ANOVA in case of parametric distribution and the Kruskal–Wallis test in case of nonparametric distribution. British Journal of Dermatology (2016) 175, pp340–347 Categorical variables were compared using the v2-test. Significantly different characteristics between ADA, ETA and USTE were corrected for with multivariate Cox regression analysis for drug survival (MCR-DS) in order to adjust for their possible confounding effect when comparing drug survival between different biologics. Some variables were highly correlated and therefore only one variable was chosen for the confounder correction based on P-value; weight was chosen over BMI and biologic naivety was chosen over anti-TNF-a naivety. Sex and age at the start of the biologic were set as fixed variables. Possible confounders, that is the variables that were significantly different between treatment groups, were added as covariates to the MCR-DS. Hazard ratios were extracted from the models and are described. Predictors for drug survival To elucidate the predictors for drug survival of ADA, ETA and USTE as a group and separately per biologic for overall drug survival, and drug failure due to ineffectiveness and sideeffects, firstly all baseline variables were tested with univariate Cox regression analysis with the P-value set at < 02. Possible predictor variables were then incorporated in the multivariate Cox regression analysis for predictors (MCR-P, to distinguish this multivariate analysis from the previously mentioned MCRDS). On the basis of the univariate analysis, BMI was chosen over weight for the multivariate analyses with MCR-P. For MCR-P, backward selection was performed to elucidate the final predictors. All analyses were performed with SPSS version 20.0 (IBM, Armonk, NY, U.S.A.). A P-value < 005 was considered significant. Variables with a Gaussian distribution were presented as mean SD, nonparametrically distributed variables as median (interquartile range) and categorical data as n (%). Results Patients In total, 526 treatment episodes were included – 186 ADA, 238 ETA and 102 USTE – with a total of 1333 years of treatment. The characteristics of the patients at inclusion in BioCAPTURE are shown in Table 1. The majority of patients were male (609%, n = 226), overweight (median BMI 278) and had a positive family history of psoriasis (660%). Psoriatic arthritis was present in 286% of patients. The median PASI score at baseline was 132. Baseline patient characteristics The baseline patient characteristics per biologic are presented in Table 2. The median baseline weight was significantly higher for USTE (920 kg) and ADA (880 kg) than for ETA (840 kg; P = 0002 and 0025, respectively). The median baseline BMI was significantly higher for ADA (290 kg m 2) and USTE (282 kg m 2) than for ETA (277 kg m 2; © 2016 British Association of Dermatologists Long-term drug survival of biologics in psoriasis, J. Zweegers et al. 343 Table 1 Baseline patient characteristics Baseline patient characteristics Age at start of biologic (years), mean SD Sex (male), n (%) Height (cm), mean SD Weight (kg), median (IQR) Body mass index (kg m 2), median (IQR) Positive family history of psoriasis (yes), n (%) Psoriatic arthritis diagnosed by a rheumatologist (yes), n (%) Duration of psoriasis until start of biologic (years), median (IQR) Baseline PASI score, median (IQR) First ever treatment episode in BioCAPTURE (n = 371) 475 128 226 (609) 1754 89a 860 (220)b 278 (66)a 245 (660)c 106 (286)d overall drug survival was in favour of USTE (1 year: 840% USTE, 758% ETA, 746% ADA; 5 year: 61% USTE, 41% ADA and 34% ETA). The percentages decreased for ADA to 35% at 6 years and for ETA to 20% at 10 years of treatment. Survival rates of drug survival split for ineffectiveness were again in favour of USTE with percentages of 79% for USTE, 54% for ADA and 45% for ETA at 5 years of treatment. These percentages decreased further for ADA to 50% at 6 years and for ETA to 31% at 10 years. Five-year survival percentages for discontinuation due to side-effects were 83% for USTE, 80% for ETA and 76% for ADA. These percentages were 70% for ADA at 6 years and 70% for ETA at 10 years of treatment. Sensitivity analyses yielded similar percentages (Appendix S1; see Supporting Information). 199 (176)e 132 (77)f IQR, interquartile range; PASI, Psoriasis Area and Severity Index. Missing data: a79, b75, c13, d18, e2, f11. P = 0033 and P = 0029, respectively), but not for ADA compared with USTE (P = 0094). The median baseline PASI score was significantly higher for USTE (134) and ETA (132) than for ADA (111; P = 0007 and P < 0001, respectively). Patients were significantly less often biologic naive and anti-TNF-a naive in treatment episodes of USTE compared with ADA (P = 0004 and P = 0012, respectively) and ETA (P < 0001 in both analyses). Long-term drug-survival analysis All available data on long-term drug survival for ADA, ETA and USTE are shown in Figure 1. During 5 years of treatment, Comparing long-term drug survival corrected for confounders Confounder correction was performed on drug-survival analysis by incorporating the significantly different baseline patient characteristics into MCR-DS (Table 2). Age and sex were set as fixed variables. Using all long-term data (Fig. 1), overall drug survival corrected for confounders showed a significantly higher value for USTE compared with ADA [hazard ratio (HR) 174, 95% confidence interval (CI) 109–280] and for USTE compared with ETA (HR 216, 95% CI 131–356). For ADA and ETA, overall survival was similar (HR 077, 95% CI 056– 107). Confounder-corrected drug survival of discontinuation due to ineffectiveness showed a significantly higher survival for USTE compared with ADA (HR 274, 95% CI 142–528) and for USTE compared with ETA (HR 291, 95% CI 146–578). Survival of ADA vs. ETA showed no differences (HR 080, 95% CI 054–117). Confounder-corrected drug survival of discontinuation due to side-effects showed a significantly Table 2 Baseline patient characteristics per biologic Baseline patient characteristics Adalimumab (n = 186) Etanercept (n = 238) Ustekinumab (n = 102) Age at start of biologic (years), mean SD Sex (male), n (%) Height (cm), mean SD Weight (kg), median (IQR) BMI (kg m 2), median (IQR) Positive family history of psoriasis (yes), n (%) Psoriatic arthritis (yes), n (%) Duration of psoriasis until start of biologic (years), median (IQR) Baseline PASI score, median (IQR) Biologic naive (yes), n (%) Anti-TNF-a naive (yes), n (%) 487 128 469 127 501 125 0072a 106 (570) 1755 85 (missing: 16) 880 (240) (missing: 16) 290 (65) (missing: 17) 127 (683) (missing: 6) 146 (613) 1748 85 (missing: 66) 840 (243) (missing: 65) 277 (35) (missing: 66) 154 (647) (missing: 6) 66 (647) 1767 89 (missing: 8) 920 (212) (missing: 4) 282 (67) (missing: 8) 69 (676) (missing: 3) 041b 022a 0005c 0038c 064b 61 (328) (missing: 7) 205 (184) (missing: 2) 71 (298) (missing: 5) 204 (105) 28 (275) (missing: 9) 196 (96) 033b 085c 111 (72) (missing: 7) 65 (349) 73 (392) 132 (82) (missing: 7) 152 (639) 174 (731) 134 (115) (missing: 4) 19 (186) 25 (245) IQR, interquartile range; BMI, body mass index; PASI, Psoriasis Area and Severity Index; TNF, tumour necrosis factor. aOne-way b 2 v -test, cKruskal–Wallis test. © 2016 British Association of Dermatologists P-value < 0001c < 0001b < 0001b ANOVA, British Journal of Dermatology (2016) 175, pp340–347 344 Long-term drug survival of biologics in psoriasis, J. Zweegers et al. (a) (b) (c) Fig 1. (a) Ten-year drug survival for adalimumab, etanercept and ustekinumab. (b) Ten-year drug survival with discontinuation due to ineffectiveness split per biologic. (c) Ten-year drug survival with discontinuation due to side-effects split per biologic. higher survival of USTE compared with ADA (HR 235, 95% CI 102–537) and USTE compared with ETA (HR 258, 95% CI 102–652). Drug survival of ADA compared with ETA was not statistically different (HR 093, 95% CI 052–166). Oneand 5-year confounder-corrected drug-survival data are presented in Appendix S1 (see Supporting Information). Predictors for long-term drug survival Variables from the univariate analyses that were incorporated into MCR-P for the different biologics are shown in Table S1 (see Supporting Information). Predictors for adalimumab, etanercept and ustekinumab as one group of biologics MCR-P for overall survival showed that female sex (HR 145, 95% CI 110–192) and higher BMI (HR 118, 95% CI 104– 134) were predictors of discontinuation. MCR-P showed that higher BMI (HR 125, 95% CI 108–146) and biological naivety (HR 139, 95% CI 100–193) were predictors of discontinuation due to ineffectiveness and that female sex (HR 283, 95% CI 179–472) was a predictor of discontinuation due to side-effects. Predictors for adalimumab MCR-P for overall survival, as well as for survival due to ineffectiveness, yielded no significant predictors. BMI was the last variable in both analyses, but was not significant. MCR-P for side-effects showed that female sex (HR 291, 95% CI 135– 629) was a predictor of discontinuation. Predictors for etanercept Female sex (HR 177, 95% CI 118–264), higher BMI (HR 125, 95% CI 104–151) and the presence of specific comorbidities (HR 189, 95% CI 104–346) were predictors of overall discontinuation. MCR-P showed that higher BMI (HR 134, 95% CI 107–168) was a predictor for discontinuation British Journal of Dermatology (2016) 175, pp340–347 due to ineffectiveness. Female sex (HR 233, 95% CI 101– 535), higher BMI (HR 147, 95% CI 101–208) and age at start of ETA treatment (HR 142, 95% CI 106–192) were predictors for discontinuation due to side-effects. Predictors for ustekinumab MCR-P showed that higher BMI (HR 143, 95% CI 101– 203) was a predictor for overall survival. Higher BMI (HR 198, 95% CI 122–321) was a predictor for discontinuation due to ineffectiveness, and female sex (HR 402, 95% CI 100–1613) was a predictor of discontinuation due to sideeffects. In the group of patients with bodyweight > 100 kg who failed USTE due to ineffectiveness, five (83%) of six patients were treated with 90 mg and were thus treated according to the guidelines.22,23 The results of sensitivity analyses for drug survival of USTE from the date of last injection are presented in Figures S1–S3 (see Supporting Information). Side-effects resulting in discontinuation of the biological agent in female and male patients In total, 79 patients discontinued their biological treatment due to side-effects: 30 (38%) for ADA, 40 (51%) for ETA and nine (11%) for USTE. Side-effects per biologic are presented in Table S2 (see Supporting Information). Forty-five (57%) of the 79 patients were female. The numbers of female/male patients with side-effects leading to treatment discontinuation were 20 (25%)/10 (94%) for ADA, 19 (21%)/21 (14%) for ETA and six (17%)/three (4%) for USTE. There was a heterogeneity in experienced side-effects, and no pattern in the type of side-effect was found between female and male patients. Infections, mainly of the respiratory tract, were a common reason for discontinuing ADA and ETA, but not USTE treatment. There were also no patterns found for infections between female and male patients, or between ADA and ETA. The only side-effects that could be characterized as typical for female patients were a cystitis in one female patient during ADA treatment, breast cancer in one female patient on ETA © 2016 British Association of Dermatologists Long-term drug survival of biologics in psoriasis, J. Zweegers et al. 345 treatment and cervical cancer in one female patient on ETA treatment. One female patient on ADA treatment and one male patient on ETA treatment stopped their treatment due to feelings of depression. Biological dose The mean SD cumulative doses of the biologics were 2783 2353 mg for ADA, 9720 8746 mg for ETA and 632 587 mg for USTE (ADA, 50 18 mg per 2 weeks; ETA, 76 18 mg per week; USTE ≤ 100 kg, 69 32 mg per 12 weeks; USTE > 100 kg, 97 38 mg per 12 weeks). In our cohort, patients treated with ADA and ETA more often had a dose increase (i.e. a higher dose than the recommended label dose) than patients treated with USTE (ADA 40%, ETA 69%, USTE 27% of patients). Discussion This prospective, comparative, multicentre, long-term drugsurvival study showed that a higher BMI was a predictor for drug discontinuation due to ineffectiveness for ETA and USTE, and that female sex was a consistent predictor for discontinuation due to side-effects for ADA, ETA and USTE. USTE had the highest confounder-corrected long-term drug survival in psoriasis treatment, compared with ADA and ETA. Consistently with our study, a higher BMI was previously found to predict overall biological discontinuation in psoriasis treatment.25–27 BMI was also a predictor of overall biological survival in patients with rheumatoid arthritis.28 However, overall biological survival is a result of drug discontinuation due to ineffectiveness, side-effects and other reasons.19 Of these, ineffectiveness is the main reason for discontinuation of biologics in psoriasis treatment.9,11 Highlighting the predictors for ineffectiveness is therefore of interest. Our study elucidated that a higher BMI is a predictor of biological discontinuation due to ineffectiveness for both ETA and USTE, but was not a significant predictor for drug survival of ADA. Given the current results from different studies, one might consider that patients with psoriasis with a higher BMI should be encouraged to lose weight before and during their biological treatment. Indeed, a recently performed randomized controlled trial showed a positive effect of a diet–exercise combination over an information-only strategy on psoriasis severity in patients with psoriasis who were being treated with systemic agents such as biologics.29 In another randomized trial, psoriasis severity was significantly lower in the diet group than in the control group at 24 weeks of biological treatment.30 Previous studies on overall drug survival of biologics as a group have stated that female sex was a predictor for biological discontinuation in psoriasis treatment.2,3,9,11,12,15 Also, in rheumatoid arthritis and in axial spondyloarthritis, female sex predicted overall drug discontinuation of anti-TNF-a therapies grouped together.20,31 So far, only one study on predictors has highlighted ADA treatment for psoriasis by using data from a smaller BioCAPTURE cohort, and found that female © 2016 British Association of Dermatologists sex was a predictor for ADA discontinuation due to sideeffects.2 Our present study with extended data from BioCAPTURE shows that female sex is a predictor for drug discontinuation due to side-effects for ADA, ETA and USTE in psoriasis treatment. The exact reason behind this is unclear. No different pattern in the type or severity of side-effects was found between female and male patients in our study. The fact that female sex is a predictor in all three biologics suggests that there is no class effect and that other reasons should be considered. For example, although scarce, publications on this topic have demonstrated sex differences in the presentation of symptoms, prognosis of diseases and treatment outcomes, as well as in communication.32 In a study regarding hospital inpatients it was shown that severe adverse drug reactions were seen more often in women than in men.33 Regardless of the underlying reason, our results can increase the awareness among physicians that female patients have a higher chance of discontinuing biological therapy for psoriasis due to side-effects than male patients. There are several studies that have assessed biomarkers in order to predict treatment success for the individual patient, such as genetic, blood or tissue biomarkers.34 However, patient characteristics can also serve as predictors for treatment success. Our analyses contribute to the first steps of developing a predictive model for biological treatment in psoriasis. Other large prospective studies are needed to confirm our results. So far, only a small number of daily-practice studies have used prospective data from multiple centres to compare biological agents.9–12 Similar to the findings in these studies, our study with long-term data showed that USTE had the highest confounder-corrected overall drug survival compared with both ADA and ETA. Unique in our study is the confoundercorrected drug survival split for discontinuation due to ineffectiveness and side-effects. Again, USTE had the highest drug survival in both analyses compared with ADA and ETA. Moreover, infliximab and not USTE was the last-resort biologic for psoriasis treatment in this study. Also, doses were more often higher than the label dose in the order ETA > ADA > USTE. We do not expect that the missing data on weight had a major influence on our presented confounder-corrected drugsurvival outcomes, as ETA had more cases in total than USTE. Indeed, our results were similar when missing data on weight were imputed by the median weight of patients for that biologic. Our data, together with data from previous studies, might aid physicians in their choice of long-term biological treatment for patients with psoriasis. A limitation of our study is the lower number of patients than in nationwide registries from larger countries.9 Strengths of our study are the detailed documentation of patient characteristics in our registry, the multicentre and prospective setting, and the performed drug-survival analyses split for each biologic and split for reasons of discontinuation. Furthermore, candidate predictors were chosen from baseline variables that were similar for all biologics, increasing the homogeneity in analysis. British Journal of Dermatology (2016) 175, pp340–347 346 Long-term drug survival of biologics in psoriasis, J. Zweegers et al. In conclusion, this prospective, comparative, multicentre, long-term drug-survival study shows that higher BMI is a predictor for drug discontinuation due to ineffectiveness for ETA and USTE, and that female sex is a consistent predictor for discontinuation due to side-effects for ADA, ETA and USTE. Furthermore, USTE has the highest confounder-corrected longterm drug survival. Comparative results from the long-term drug survival aid the physician in choosing the most suited long-term treatment for their individual patients with psoriasis. Our data also help to increase the awareness among physicians that higher BMI influences drug survival in ETA and USTE, and that female patients are prone to discontinue ADA, ETA and USTE because of side-effects. 14 15 16 17 18 References 1 Nast A, Jacobs A, Rosumeck S et al. Efficacy and safety of systemic long-term treatments for moderate-to-severe psoriasis: a systematic review and meta-analysis. J Invest Dermatol 2015; 135:2641–8. 2 van den Reek JM, Tummers M, Zweegers J et al. Predictors of adalimumab drug survival in psoriasis differ by reason for discontinuation: long-term results from the Bio-CAPTURE registry. J Eur Acad Dermatol Venereol 2015; 29:560–5. 3 van den Reek JM, van Lumig PP, Driessen RJ et al. Determinants of drug survival for etanercept in a long-term daily practice cohort of patients with psoriasis. Br J Dermatol 2014; 170:415–24. 4 Puig L, Ruiz-Salas V. Long-term efficacy, safety and drug survival of ustekinumab in a Spanish cohort of patients with moderate to severe plaque psoriasis. Dermatology 2015; 230:46–54. 5 Spertino J, Lopez-Ferrer A, Vilarrasa E, Puig L. Long-term study of infliximab for psoriasis in daily practice: drug survival depends on combined treatment, obesity and infusion reactions. J Eur Acad Dermatol Venereol 2014; 28:1514–21. 6 Lopez-Ferrer A, Vilarrasa E, Gich IJ, Puig L. Adalimumab for the treatment of psoriasis in real life: a retrospective cohort of 119 patients at a single Spanish centre. Br J Dermatol 2013; 169:1141–7. 7 Esposito M, Gisondi P, Cassano N et al. Treatment adherence to different etanercept regimens, continuous vs. intermittent, in patients affected by plaque-type psoriasis. Drug Dev Res 2014; 75 (Suppl. 1):S31–4. 8 Clemmensen A, Spon M, Skov L et al. Responses to ustekinumab in the anti-TNF agent-naive vs. anti-TNF agent-exposed patients with psoriasis vulgaris. J Eur Acad Dermatol Venereol 2011; 25:1037– 40. 9 Warren RB, Smith CH, Yiu ZZ et al. Differential drug survival of biologic therapies for the treatment of psoriasis: a prospective observational cohort study from the British Association of Dermatologists Biologic Interventions Register (BADBIR). J Invest Dermatol 2015; 135:2632–40. 10 van den Reek JM, Zweegers J, Kievit W et al. ‘Happy’ drug survival of adalimumab, etanercept and ustekinumab in psoriasis in daily practice care: results from the BioCAPTURE network. Br J Dermatol 2014; 171:1189–96. 11 Gniadecki R, Bang B, Bryld LE et al. Comparison of long-term drug survival and safety of biologic agents in patients with psoriasis vulgaris. Br J Dermatol 2015; 172:244–52. 12 Gniadecki R, Kragballe K, Dam TN, Skov L. Comparison of drug survival rates for adalimumab, etanercept and infliximab in patients with psoriasis vulgaris. Br J Dermatol 2011; 164:1091–6. 13 Menting SP, Sitaram AS, Bonnerjee-van der Stok HM et al. Drug survival is not significantly different between biologics in patients British Journal of Dermatology (2016) 175, pp340–347 19 20 21 22 23 24 25 26 27 28 29 30 with psoriasis vulgaris: a single-centre database analysis. Br J Dermatol 2014; 171:875–83. Ross C, Marshman G, Grillo M, Stanford T. Biological therapies for psoriasis: adherence and outcome analysis from a clinical perspective. Australas J Dermatol 2016; 57:137–40. Esposito M, Gisondi P, Cassano N et al. Survival rate of antitumour necrosis factor-a treatments for psoriasis in routine dermatological practice: a multicentre observational study. Br J Dermatol 2013; 169:666–72. Umezawa Y, Nobeyama Y, Hayashi M et al. Drug survival rates in patients with psoriasis after treatment with biologics. J Dermatol 2013; 40:1008–13. Brunasso AM, Puntoni M, Massone C. Drug survival rates of biologic treatments in patients with psoriasis vulgaris. Br J Dermatol 2012; 166:447–9. Inzinger M, Wippel-Slupetzky K, Weger W et al. Survival and effectiveness of tumour necrosis factor-alpha inhibitors in the treatment of plaque psoriasis under daily life conditions: report from the Psoriasis Registry Austria. Acta Derm Venereol 2016; 96:207–12. van den Reek JM, Kievit W, Gniadecki R et al. Drug survival studies in dermatology: principles, purposes, and pitfalls. J Invest Dermatol 2015; 135:e34. Gulfe A, Kapetanovic MC, Kristensen LE. Efficacy and drug survival of anti-tumour necrosis factor-a therapies in patients with nonradiographic axial spondyloarthritis: an observational cohort study from Southern Sweden. Scand J Rheumatol 2014; 43:493–7. Zweegers J, van den Reek JM, van de Kerkhof PC et al. Comparing treatment goals for psoriasis with treatment decisions in daily practice: results from a prospective cohort of patients with psoriasis treated with biologics: BioCAPTURE. Br J Dermatol 2014; 171:1091–8. Zweegers J, de Jong EM, Nijsten TE et al. Summary of the Dutch S3-guidelines on the treatment of psoriasis 2011. Dutch Society of Dermatology and Venereology. Dermatol Online J 2014; 20:doj_21769. Pathirana D, Ormerod AD, Saiag P et al. European S3-guidelines on the systemic treatment of psoriasis vulgaris. J Eur Acad Dermatol Venereol 2009; 23(Suppl. 2):1–70. Garcia-Doval I, Carretero G, Vanaclocha F et al. Risk of serious adverse events associated with biologic and nonbiologic psoriasis systemic therapy: patients ineligible versus eligible for randomized controlled trials. Arch Dermatol 2012; 148:463–70. Di Lernia V, Tasin L, Pellicano R et al. Impact of body mass index on retention rates of anti-TNF-alfa drugs in daily practice for psoriasis. J Dermatolog Treat 2012; 23:404–9. Naldi L, Addis A, Chimenti S et al. Impact of body mass index and obesity on clinical response to systemic treatment for psoriasis. Evidence from the Psocare project. Dermatology 2008; 217:365–73. Carrascosa JM, Vilavella M, Garcia-Doval I et al. Body mass index in patients with moderate-to-severe psoriasis in Spain and its impact as an independent risk factor for therapy withdrawal: results of the Biobadaderm Registry. J Eur Acad Dermatol Venereol 2014; 28:907–14. Iannone F, Fanizzi R, Notarnicola A et al. Obesity reduces the drug survival of second line biological drugs following a first TNF-a inhibitor in rheumatoid arthritis patients. Joint Bone Spine 2015; 82:187–91. Naldi L, Conti A, Cazzaniga S et al. Diet and physical exercise in psoriasis: a randomized controlled trial. Br J Dermatol 2014; 170:634–42. Al-Mutairi N, Nour T. The effect of weight reduction on treatment outcomes in obese patients with psoriasis on biologic therapy: a © 2016 British Association of Dermatologists Long-term drug survival of biologics in psoriasis, J. Zweegers et al. 347 31 32 33 34 randomized controlled prospective trial. Expert Opin Biol Ther 2014; 14:749–56. Souto A, Maneiro JR, Gomez-Reino JJ. Rate of discontinuation and drug survival of biologic therapies in rheumatoid arthritis: a systematic review and meta-analysis of drug registries and health care databases. Rheumatology (Oxford) 2016; 55:523–34. Teunissen TA, Rotink ME, Lagro-Janssen AL. Gender differences in quality of care experiences during hospital stay: a contribution to patient-centered healthcare for both men and women. Patient Educ Couns 2016; 99:631–7. Davies EC, Green CF, Taylor S et al. Adverse drug reactions in hospital in-patients: a prospective analysis of 3695 patient-episodes. PLoS ONE 2009; 4:e4439. Villanova F, Di Meglio P, Nestle FO. Biomarkers in psoriasis and psoriatic arthritis. Ann Rheum Dis 2013; 72 (Suppl. 2):ii104–10. Appendix 1 J.Z. carries out trials for AbbVie, Janssen and Sciderm; and has received research grants for the independent research fund of the Department of Dermatology of Radboud UMC Nijmegen, the Netherlands from AbbVie. J.M.P.A.vdR. carries out clinical trials for AbbVie and Janssen; has received speaking fees from Eli Lilly and AbbVie; and has received research grants for the independent research fund of the Department of Dermatology of Radboud UMC Nijmegen, the Netherlands from AbbVie and reimbursement for attending a symposium from Janssen, Pfizer and AbbVie. P.C.M.vdK. serves as a consultant for Merck Sharp Dohme, Celgene, Centocor, Almirall, UCB, Pfizer, Sofinnova, AbbVie, Actelion, Galderma, Novartis, Janssen-Cilag, Eli Lilly, Amgen, Mitsubishi and LEO Pharma; and receives research grants from Centocor, Pfizer, Merck Sharp Dohme, Merck Serono, AbbVie and Philips Lighting. E.M.G.J.dJ. has © 2016 British Association of Dermatologists received research grants for the independent research fund of the Department of Dermatology of Radboud UMC Nijmegen, the Netherlands from Merck-Serono, Wyeth, AbbVie, Pfizer and Janssen; and has acted as a consultant and/or paid speaker for and/or participated in research sponsored by companies that manufacture drugs used for the treatment of psoriasis, including AbbVie, Janssen, MSD, Pfizer, Amgen and Lilly. M.D.N. serves as a consultant for Janssen. J.M.M. served as a consultant for Novartis and Celgene. W.P.A. served as a consultant for AbbVie and Janssen and travelled with Pfizer, AbbVie and Janssen to medical congresses for 50% of the fees. Supporting Information Additional Supporting Information may be found in the online version of this article at the publisher’s website: Appendix S1. Sensitivity and survival analyses. Fig S1. Ten-year overall drug survival with ustekinumab from the last date of injection. Fig S2. Ten-year drug survival with discontinuation due to ineffectiveness: sensitivity analysis with ustekinumab from the last date of injection. Fig S3. Ten-year drug survival with discontinuation due to side-effects: sensitivity analysis with ustekinumab from the last date of injection. Table S1. Variables selected as possible predictors from univariate Cox regression analyses. Table S2. Side-effects leading to discontinuation of the biologic reported per agent. Audio S1. Author Audio British Journal of Dermatology (2016) 175, pp340–347