* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Ca Ba V - VCOMcc
Survey
Document related concepts
Transcript
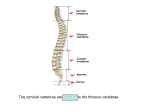
Lecture 2-3: Embryology of Bone and Muscle BONE DEVELOPMENT: Axial Skeleton: skull, vertebrae (an IV discs), ribs, sternum, and hyoid bone o Skull is composed of 2 regions: 1. Neurocranium: houses the brain a. calvarium (Ca; vault) – top part b. basicranium (Ba; chondrocranium) – bottom part these two develop differently embryologically 2. Viscerocranium (splanchnocranium) o Vertebrae: 7 cervical, 12 thoracic, 5 lumbar, 5 segments of sacrum, 3-5 segments of coccyx o contains special sensory organs (vision, olfaction, etc) Thoracic curve was original curve developed, and cervical and lumbar develop later Cervical curve develops when infant hold head up Lumbar curve develops when infant begins to walk Sternum: manubrium, body, and xyphoid process Sternum have ridges along body due to fusion of separate bones before birth Appendicular Skeleton: pectoral girdle (scapula, clavical), pelvic girdle (hip), upper limbs, and lower limbs Bone Formation: o Major calcium store for body o Form in 2 ways: most bones only form by one process Few bones form by both processes (ex: clavical and mandible) as separate bones that later fuse Primary ossification center: site of initial bone formation 1. Intramembranous ossification (IO): form flat bones o composed of spongy bone (in middle) and compact bone (on outside) o o osteons very organized in compact bone, not so much in spongy periosteium: (bone membrane) lining the surface of compact bone on inside and outside holds bones together the primary ossification centers of IO become “eminences” where bones development started first begins ~week 7 and ends after birth osteocytes (bone cells) derive from either neural crest or paraxial mesoderm (sclerotome of somite) o Neural crest cells – form most bones of frontal part of skull o Paraxial mesoderm cells – form most bones of posterior skull o mesenchymal cell (neural crest or paraxial mesoderm cells) osteoblast osteocyte STEPS: o 1. Mesenchymal cells aggregate together & form a membrane w/ surrounding CT o 2. Mesenchymal cells differentiate into osteoblasts which deposit organic portion of bone osteoid (1/3 of bone = organic) o 3. As ostoid is deposited, osteoblasts move apart & become isolated & begin depositing a calcium matrix (inorganic/mineral component) now called osteocytes (mature bone cells) o 4. Mesenchymal cells at periphery (outside) of bone become the periosteum o membrane that lines surface of bone 5. On either side of the periosteium, osteoclasts (formed by fusion of multiple monocytes) enzymatically degrade/destroy bone matrix forms spongy bone Compact bone is formed by osteogenic (mesenchymal) cells in periosteum Clinical Correlation: o If skull fails to completely form o Cranial meningocele: meninges (membranes around brain/spinal cord) are pushed out (herniated) o o Meningocele = cavity of meninges Encephalocele: brain/neural tissue AND meninges herniated Failure of neural crest cells if on front of face Failure of paraxial mesoderm cells if on back of head Craniosynostosis: one or more of the sutures of infant skull prematurely fuses Changes growth pattern of skull depending on which suture fuses, skull cant expand, not enough space for brain to develop, skull and facial abnormalities Also referred to as “Cloverleaf” due to shape of head as a cloverleaf 2. Endochondral ossification (EO): (“within cartilage”) forms remaining bones (basicranium and post-cranial bones (all bones below skull) o basicranium (base of skull) – only part of skull that is not formed by IO begins ~week 5 and ends after birth osteocytes derived from somatic lateral plate mesoderm o mesenchymal cell chondrocyte (dies) o forms the cartilage then dies mesenchymal cell osteoblast osteocyte (same as intramembranous) cartilage “model” made, then replaced w/ bone STEPS: o 1. mesenchymal cells (MCs) (derived from somatic lateral plate mesoderm and paraxial mesoderm cells (particularly schlerotome)) aggregate to form a “model” of developing bone o these then differentiate into chondrocytes (produce hyaline cartilage) 2. chondrocytes in center of model hypertrophy and produce alkaline phosphatase calcifies the matrix remaining cells around periphery form periosteum = membrane that surrounds bone o 3. a thin “bony collar” forms from periosteum around shaft blood vessel penetrates the bony collar (diaphysis) introducing osteogenic cells (aka. MCs) and osteoclasts o 4. osteogenic cells differentiate into osteoblasts/osteocytes and form spongy bone = primary ossification center center of shaft o spongy bone is deposited and resorbed repeatedly 5. marrow (medullary) cavity forms due to 1. Chondrocyte death and 2. Osteoclast activity o 6. Process is repeated in the epiphysis = secondary ossification center formation of epiphysis Two regions of cartilage remain at end of EO: 1. Articular cartilage: cushions and supports joints 2. Epiphyseal plate/cartilage: site of bone growth (length) o growth plate allows for growth during life o eventually plate becomes all bone (no longer cartilage) no more growth occurs occurs very early in Dwarfism Development of Vertebrae: o Vertebrae and annulus fibrosus (fibrous portion of the IV disc) formed by sclerotome cells Schlerotomal cells migrate medially from each side and unite to make own half of each vertebrae Four somites unite from each side unite to form each vertebrae: Two somites from each side create each half Two other somites from below and above migrate inferomedially and superomedially (sclerotomal resegmentation) and unit “boundary” w/in a somite where sclerotomal cells separate sclerotomal fissure (SF) spinal nerves emerging from spinal cord pass thorugh the space created at the SF by the migrating sclertomac cells w/in a somite and can then access a muscle Development of Invertebral Discs o Where vertebrae are formed, notochord die off o Left over Notochord between vertebrae will form intervertebral dics This leftover notochord forms 2 regions: 1. Nucleus pulposus (NP, inner part) and 2. Annulus fribrosus (AF, outer part) Sclerotomal cells (paraxial mesoderm) migrate medially and surround the nucleus pulposus to form the Annulus fibrosus (AF) o AF = cartilage that forms around the nucleus pulposus (NP) o Clinical Correlation: Chordoma: notochordal cells remain in the vertebral bodies A rare, but very serious malignant form of cancer Diseases caused by failure of vertebrae to form: Spina Bifida: caused by incomplete formation of vertebral laminae, typically occurs in lumbrosacral region due to inadequate sclerotomal cell contribution severity depends on how many vertebra are involved and if neural tissue is displaced Meningocele: involves only meninges Mylomeningocele: involves meninges AND neural tissue Congential Kyphosis and Lordosis: Failure of vertebrae to form in proper dimensions anteriorly and/or posteriorly leads to wedging of vertebrae Individual displays either excessive thoracic curve (kyphosis) or excessive lumbar curve (lordosis) Scoliosis: excessive lateral curvature due to unequal distribution of sclerotomal cells from somites on either side of embryo o may form correctly on one side but not correctly on other causing lateral wedge may result in hemivertebrae Congential Spondylolisthesis: vertebrae form completely, but not in the correct place the forward displacement (sits further forward) of a vertebrae Particularly L5 sitting on top of sacrum Result of abnormal positioning of vertebrae during development, creating risk for slipping Development of Ribs: formed by EO o Sclerotomal cells proliferate and migrate along the body wall (segmentally and bilaterally) forming costal processes o costal processes grow a short distance from vertebrae along the entire vertebral column, but only continue to grow in the thoracic region (T1-T12), thus giving rise to ribs genes are turned off at ALL regions but in thoracic region forming ribs costal processes on all vertebrae are result of initial formation of ribs until genes were turned off During growth, rib is completely fused/part of vertebrae Once rib makes it around to front side, then apoptosis occurs leading to two separate bones that articulate with each other Cells grow on tips of ribs as they move anteriorly (sternal plate), leading to fusion/formation of sternum when they unite o Clinical Connection: Cervical Rib: formation of an extra rib, most commonly seen in cervical region can be unilateral or bilateral Costal synostosis: fusion of ribs Ribs can also vary in number (missing), underdeveloped, fused, or bifid can lead to breathing difficulty Development of the Sternum: o Sclerotome cells migrate (after making the vertebra and ribs) will bump into the somatic lateral plate mesoderm will then proliferate, condense, and chondrofy to form sternal plates (bars) o Sternal bars meet in the middle and fuse craniocaudally (from top to bottom) to form the sternum o Cells of sternal bars differentiate segmentally forms sternebrae Begins as cartilage then begins to ossify forms one of two ossification centers in each sternebra o Ossification of sternum begins before birth but doesn’t completely fuse until ~30 yo o Xyphoid process can become “fork shaped” instead of pointed caused b/c fusion was never completed o Clinical Connection: (see pics in slides) Sternal Foramen: Incomplete fusion of ossification centers of a sternebra Sternal Cleft: results in incomplete fusion of the sternal bars Pectus Excavatum: overgrowth of ribs displaces sternum posteriorly Pectus Excavatum Pectus Carinatum: “Pigeon Chest” Sever cases require surgery to insure heart function isn’t effected Ribs grow abnormally outward causing sternum to be abnormal shape and position Absence of Sternum: just have ends of ribs, no sternum to attach to MUSCLE DEVELOPMENT: Development of Skeletal Muscle: Mature muscle cells very long, extend length of muscle, cells are multinucleated and nuclei are located at periphery of cell, and nuclei are closely associated w/ satellite cells (stem cells that serve to repair minor muscle damage) Muscles develop from somites where myotomal cells of somite will migrate dorsally and ventrally = referred to as myoblasts when they become migratory o Recall: dermatome, myotome, and schlerotome = somite Myoblasts begin to fuse and form a myotube it continues to grow as more cells are added eventually, mature muscle fiber is formed Small population of cells at periphery remain as satellite cells (don’t become fused, stay at periphery) Myoblasts that migrate dorsally (back) form epimere (big clump of back muscle) o Cells of epimere will segregate to form epaxial muscles = true back muscles o These work to extend the vertebral column o Innervated by dorsal rami Spinal nerve from developing spinal cord branch to form dorsal and ventral rami dorsal move backwards and innervate all back muscles, ventral move forward and innervate everything except true back muscles) Myoblasts that migrate laterally or ventrally (front) form hypomere (big clump of ventral muscle) o Cells of hypomere will segrate to form hypaxial muscles = flexors of vertebral column, muscles of neck and limbs, and diaphragm Clinical Connection: o Muscle Aplasia: abnormal muscle formation Poland Anomaly (Syndrome): results in unilateral absence of pectoralis major muscle More common in males and more frequently on the right Prune Belly Syndrome: absence of abdominal wall musculature Condition affects males 97% of the time LIMB DEVELOPMENT Limbs develop from ectoderm (skin and nerves) and lateral plate mesoderm (skeleton, joints, CT, vessels) Limb growth occurs in 3 dimensions: o 1. Proximal-distal (length) first, limb grows outward, flattens at end forms an ectodermal ridge along the tip = called apical ectoderm ridge (AER) AER secretes proteins that induce mitosis of mesodermal cells immediately deep to AER = progress zone secretes protein that sustain (keep alive) cells of the AER As progress cells divide and get further away from AER, they become too far to be affected by the proteins secreted by AER become mesenchymal mesoderm These cells are no longer influenced by the AER (they stop dividing and are left behind) and begin to differentiate into skeletal components of limbs therefore, limbs grow proximal to distal (cells are left behind along the way forming the bones of arms) o 2. Medial-lateral (i.e. formation/differentiation of thumb to pinky; asymmetry) directed by population of cells located on medial (caudal) aspect of limb bud at it’s origin zone of polarizing activity (ZPA) distance from one source (ZPA) to cells on other side of limb bud result in medial-lateral asymmetry pinky is medial and thumb is lateral grafting additional ZPAonto opposite side of limb buds results in duplicated digits o 3. Dorsal-ventral (back and front) – wont be discussed o Clinical Connection: these induce the asymmetry observed in mature limbs Limb Abnormalities: includes partial or complete loss of limbs, unilaterally or bilaterally Commonly due to maternal exposure to a teratogen (ex: thiladomide) Complete limb loss = Amelia Partial limb loss = meromelia Digit Formation: o Occurs via apoptosis of skin between fingers o Clinical Connection: Polydactyly: supernumerary (extra) digits Probably due to extra ZPA or could be caused by lack of apoptosis leading to extra cells forming an extra “limb” Syndactyly: fused digits Due to fused skin via problem in apoptosis Lecture 4: Radiology of Axial Skeleton ONLY KNOW IMAGES FROM THIS LECTURE! X-rays: (Plainfilms) o Ionizing radiation o Always available no matter where you are o Good for dense structures bones, dense muscles, solid organs, differentiates btw differences in density, can be enhanced w/ contrast o Only thing x-rays sees is dense material paint lines between diff tissues of diff densities Downside: Radiation poor discrimination of soft tissue have to look “through” all tissues o X-rays draw lines between adjacent tissues of different density overlapping structures can mask pathology Density can depend on both type of tissue (bone vs muscle vs hollow organ, etc) and THICKNESS of tissue o Understanding the structures of the body in 3D is ESSENTIAL to understanding imagery of any type!!! o NO 3D component to plainfilms! MRI o NO RADIATION o Tunable so able to demonstrate all tissues bones, muscle, solid and hollow organs o Downside: o Expensive Time-intensive Requires a lot of computer support ALL metal must be removed soft tissue more apparent than in Xrays not looking through tissue, looking through very specific slice of tissue no overlying tissue to mask things (very good detail) o by adjusting the image weight, can bring different tissues into highlight o and by taking a specific “slice’ through the body, have removed the overlying tissues can also give transverse (over top looking down) images (remember R&L are opposite) CT: spinning x-ray o LOTS of ionizing radiation – more than x-ray o Uses rotating x-ray emitter to obtain 3D image of body To get a 3D image, must take images in two axes (unlike plainfield that has no inherent 3D component) Can be used to build virtual models of desired structures o Good for almost all tissues o Faster than an MRI, not as good, but better than a plainfield o Can be enhanced w/ contrast o Advantage of CT is removal of overlying tissue signal via computer enhancement Downside: Radiation exposure Significantly more exposure than a plainfilm Requires significant computer support to produce images Not as clear as an MRI pictures are fuzzier o Gives “slice” through the body and transverse images o Resolution usually best w/ dense tissues (not so much soft issue unless contrast is used) o When looking at transverse section, must consider orientation of patient laying down supine and doctor is staring from feet to head (bottom to top) anterior = top, posterior = bottom, R&L are flipped Skull Base/Cervical Spines: o Cervical Spine: What you’re looking for with an X-ray: Alignment of bodies – look for smooth line Regular spacing dark space between vertebral bodies = IV discs (should be approx same from top to bottom) “dark line” in unusual places o dark line = less dense probably overlap? unusual regions of greater or lesser density in order to get satisfactory image of C1-2 interaction, an x-ray must be taken through open mouth Thoracic Spine: o What you’re looking for in X-ray: Alignment of spine Spacing Articulations Symmetry of rib cage Bone density External Occipital protuberance (EOP/Inion) – attachments include trapezius, ligamentum nuchei? Superior nuchal line passes through EOP/Inion – superficial cervical muscles attach here -muscles who’s principle function is to control position of the skull Inferior nuchal line – deep cervical muscles attach here -control position of skull Lecture 5: Superficial Back Posterior Shoulder Type of Back Muscles: o Superficial Muscles = extrinsic and move the appendicular muscles Hypaxial differentiation Innervated by ventral motor roots which split into ventral rami o Ventral roots are motor Deep Muscles = intrinsic and move the head and trunk, acting on the spine as principle extensors in lateral flexion and rotation spanning from pelvis to skull base Epaxial differentiation Innervated by dorsal sensory roots which split into dorsal rami o Dorsal and ventral roots converge to form a spinal nerve Dorsal roots are sensory spinal nerve then splits to form ventral rami and dorsal rami Superficial Back Muscles and Accessories: o Trapezius: Proximal: Medial third superior nuchal line, external occipital protruberance, ligamentum nuchae, T1-T12 spinous processes o Distal: Spine of scapula, acromion, lateral third of clavicle Action: Elevates, retracts pectoral girdle, superiorly rotates scapula Nerve: Accessory nerve 11 (CN XI) Scapular Movements: Elevation and depression Superior and inferior rotation Protraction and retraction Latissimus Dorsi: Proximal: T7 – L5 spinous processes, thoracolumbar fascia, dorsal sacrum, iliac crest Distal: floor intertubercular groove (on humerus) Action: Extends, adducts, medially rotates humerus Nerve: Thoracodorsal nerve A branch of the posterior cord of the brachial plexus made up of cranial nerve (CN) VI, VII, & VIII Possesses fibers that attach to the scapula as it crosses the inferior angle of the scapula Usually used to move upper arm, but can be used to move torso relative to fixed limb Commonly used in gymnastics, swimming, kayaking, crutch-walking o Thoracolumbar Fascia: Thick aponeurosis from iliac crest and dorsal sacrum to thoracic region Tri-laminar in lumbar region Three Layers that encase muscle: Posterior, Middle, and Anterior Btw Posterior and Middle encloses the erector spinus muscle Btw Middle and Anterior encloses quadratus lumborum o Triangle of Auscultation: thinnest area in back sounds the best o o Boundaries Superior = Latissimus dorsi Medial = border of scapula Lateral = trapezius Levator Scapulae: (1) Proximal: C1-C2 transverse processes and C3-C4 posterior tubercles Distal: superior angle of the scapula Action: Elevates, protracts pectoral girdle, inferiorly rotates scapula Nerve: C3-C4 ventral rami and dorsal scapular nerve Rhomboid Minor: (2) Proximal: C7-T1 spinous processes Distal: Medial border of scapula Action: Elevates, retracts pectoral girdle, inferiorly rotates scapula o Nerve: Dorsal scapular nerve Rhomboid Major: (3) Proximal: T2-T5 spinous processes Distal: Medial border of scapula Action: Retracts, elevates pectoral girdle, inferiorly rotates scapula Nerve: Dorsal scapular nerve Intermediate Back Muscles and Accessories: o Serratus Posterior Superior: Proximal: C7-T3 spinous processes Distal: Superior borders of ribs 2-5 Action: Weakly elevates ribs 2-5 can hear lung o Nerve: Ventral rami T2-5 Serratus Posterior Inferior: Proximal: T11-L3 spinous processes Distal: Inferior borders of ribs 9-12 Action: Weakly depresses ribs 9-12 Only weakly elevates (normal breathing in) NOT a muscle of respiration, only helps Only weakly depresses (normal breathing out) NOT a muscle of respiration, only helps Nerve: Ventral rami T9-12 Posterior Back Muscles: o o Teres Major: Proximal: Posterior surface inferior angle of scapula Distal: Medial lip intertubercular groove (of humerus) Action: Extends, adducts, medially rotates humerus Nerve: Lower subscapular nerve Deltoid: Proximal: (3) Spine of scapula, (2) acromion, (1) lateral third of calvicle Distal: Deltoid tuberosity of humerus Action: Anterior (1) flex, medially rotate humerus Lateral (2) abduct humerus Posterior (3) extend, laterally rotate humerus Nerve: Axillary Nerve o same as distal end of trapezius (Axe Body Spray = arm pit/axilla) Bursae: Flat sac of synovial membrane functions to lubricate the joint Usually 2 main ones for shoulder = 1. Subacromial under acromium and 2. Subdeltoid under deltoid o o o Clinical Causes of Bursitis: Calcifying tendinitis: calcification of the tendon and related degernative change Supraspinatous tendon avulsion: rotator cuff tear Supraspinatus: (1) Proximal: Supraspinous fossa Distal: Greater tubercle of humerus Action: Abducts humerus Nerve: Suprascapular nerve Infraspinatus: (2) Proximal: Infraspinous fossa Distal: Greater tubercle of humerus Action: Laterally rotates humerus Nerve: Suprascapular nerve Teres Minor: (3) Proximal: Posterior surface, middle lateral border of scapula Distal: Greater tubercle of humerus Action: Laterally rotates humerus Nerve: Axillary nerve (Axe Spray) o Subscapularis; Proximal: Subscapular fossa Distal: Lesser tubercle of humerus Action: Medially rotates humerus Nerve: Upper and lower subscapular nerves o (same as Teres Major) Rotator Cuff: Musculotendinous cuff of 4 muscles that adhere to the fibrous capsule of the glenohumeral joint Only muscles that articulate w/ the greater and lesser tubercle are part of rotator cuff Function stabilize the shoulder joint SItS in the shoulder joint Subscapularis, Infraspinatus, Teres MINOR, Supraspinatus o Serratus Anterior: (under scapula) Proximal: Ribs 1-8, laterally Distal: Anterior side of scapula along medial border Action: Protracts pectoral girdle, holds scapula to rib cage, superiorly rotates scapula Nerve: Long thoracic nerve (runs along surface of muscle) Cutaneous Nerve Supply: sensory o Posterior cutaneous nerves; medial branches of dorsal rami and lateral branches of dorsal rami o Lateral cutaneous nerves: posterior branches of ventral rami Anatomical Spaces: o Two geometric-shaped spaces formed by muscles near proximal arm containing neurovasculature o 1. Quadrangular Space: Boundaries: Teres minor, Teres Major, Surgical neck of humerus, and long head triceps Contents: Posterior circumflex humeral artery and Axillary nerve o 2. Triangular Space: Boundaries: Teres minor, Teres Major, and Long head triceps Contents: Circumflex scapular artery Blood Supply of Shoulder: o Subclavian artery of the thyrocervical trunk then branches to… o Superficial transverse cervical artery Deep dorsal scapular artery Suprascapular artery Rib 1 Axillary Artery Subscapular artery Thoracodorsal nerve Circumflex scapular artery Posterior humeral circumflex artery (seen in Quadrangular space) o Scapular anastomosis: a system connecting certain subclavian artery and their corresponding axillary artery forming a circulary anastomosis around the scapular Allows blood to flow past the joint in the event of occlusion, damage, or pinching of the transverse cervical artery, dorsal scapular artery, suprascapular artery, branches of subscapular artery, and branches of the thoracic aorta Lecture 6: Deep Back and Subocciptial Region Type of Back Muscles: o Superficial Muscles = extrinsic and move the appendicular muscles Hypaxial differentiation Innervated by ventral motor roots which split into ventral rami o Ventral roots are motor Deep Muscles = intrinsic and move the head and trunk, acting on the spine as principle extensors in lateral flexion and rotation spanning from pelvis to skull base Epaxial differentiation Innervated by dorsal sensory roots which split into dorsal rami Dorsal roots are sensory Includes 3 muscles splenius, erector spinae, transversospinales Deep Back Muscles and Accessories: Intrinsic muscles move head and trunk o Organized into grps based on attachment and function Deep to the extrinsic (superficial) muscles Nerves: Innervations from dorsal (posterior) rami of spinal nerves Arterial Supply: from posterior branches of aorta Thoracolumbar Fascia: Dense, tough connective tissue layer found throughout the back Extends from the iliac crest and dorsal sacrum upwards to the thoracic region and neck Serves as attachment point for several muscles including latissimus dorsi, internal oblique and transversus abdominis o o Continues into the neck as nuchal fascia Multiple layers anchored to spinous and transverse processes of lower thoracic & lumbar vertebrae Invests the intrinsic back muscles in a fascial compartment changes name as it moves along back to indicate location 1. Splenius Group: (only muscles in the superficial group of deep back muscles) Flat and broad, just deep to the sternocleidomastoid Origin: spinous processes and supraspinous ligament from C7-T6 Insertion: transverse processes of C1&C2 (cervicis), occipital bone, and mastoid process (capitis) Nerves: innervated by spinal nerve C1-C6 (posterior rami) Actions: bilaterally extend spine, unilaterally flex and rotate cervical spine o 2. Erector Spinae Muscles: Handles gross movements of the spine Nerves: dorsal (posterior) spinal rami Arterial Supply: posterior branches of aorta Includes Three Muscles: (I Like Sushi) Iliocostalis lumborum (more lateral) o Origin: common tendon attached to the iliac crest, posterior sacrum, spinous processes of lumbar vertebrae and supraspinous ligament o Inserts: into ribs in thoracic region and transverse processes in lumbar and cervical region o Actions: bilaterally extend spinal column, unilaterally act to flex spinal column ipsilaterally (same side) Longissimus throacis: middle of erector muscles (thoracic area) o Origin: common tendon w/ iliocostalis (iliac crest and sacrum) o Inserts: on ribs in thoracic region, transverse processes in thoracic and cervical regions, and onto the mastoid process of skull o Actions: bilaterally extend spinal column, unilaterally act to flex spinal column ipsilaterally (same as above) Spinalis: medial most of erector muscles (close to SPINE) o Origin: spinous processes and supraspinous ligament in lumbar and thoracic regions o Inserts: on spinous processes in upper thoracic and cervical regions o Actions: bilaterally extend spinal column, unilaterally act to flex spinal column ipsilaterally (same as above) o Transversospinales: (moves upward) deep group of intrinsic muscles Relatively short muscles located on the spine Attach to transverse processes inferiorly, spinous processes superiorly Muscles are in groove btw spinous and transverse processes Nerves: innervated by dorsal (posterior) rami (same as above) Consist of Three Muscles: differentiated by length of spinal column that it spans 1. Semispinalis: most superficial group o Found immediately deep to the spinalis muscles o Most prominent in upper thoracic and cervical regions o Arise from transverse processes of thoracic and cervical vertebrae o Insert into spinous processes 4-6 segments superior to origin and to occipital bone between nuchal lines o Actions: extend and contralaterally (opposite side) rotate spine 2. Mutlifidus: middle layer of group o Immediately deep to the spinalis and semispinalis muscles o Most prominent in the lumbar region o Arises from posterior superior iliac spine, sacrum, aponeurosis of erector spinae, etc. o Inserts: into spinous processes 2-4 segments superior (higher) to origin o Actions: stabilize spine during movement Prevents lumbar vertebrae from sliding off of sacrum Stabilizer of lower spine Keeps spine from severing cord during movement 3. Rotatores: deepest muscles of group o Deep to multifidus o Most prominent in thoracic region o Arise from transverse processes all along the spine o Insert into spinous processes 1 to 2 segments superior to origin o Actions: very TINY muscles—densely loaded with sensory nerves Most likely act as proprioceptive organs Minor Muscles of the Back: o These are small muscles, typically included in the deep group with the transversospinalis muscles o Nerves: all innervated by dorsal (posterior) rami of spinal nerves o EXCEPT anterior cervical intertransversarii only muscle on back that is anteriorly innervated Three Groups: 1. levator costarum: from spine to ribs arise from transverse processes of C7-T-11 insert on ribs inferior to vertebrae Actions: assist in elevating ribs during deep respiration, lateral flexion 2. intertransversarii (2 groups of these in the cervical regionanterior and posterior) arise from transverse process insert into transverse process superior to it Actions: laterally flex and stabilize spine Nerves: Anterior cervical Intertransversarii ventral (anterior) rami; Posterior cervical intertransversarii dorsal (posterior) rami 3. Interspinales: from spinous to transverse processes arise from spinous process insert into spinous process superior to it Actions: extend and rotate spine (minimally) RECAP: Intrinsic Back Muscles o Act on spine Principally extentors, aid in lateral flexion and rotation o Span from pelvis to skull base o Grp’d according to attachment and function o Innervated by dorsal (posterior) spinal rami o Thoracolumbar fascia forms compartment containing the muscles o Suboccipital Traingle and Muscles: Found at posterior base of skull, very small muscles Deep to trapezius, sternocleidomastoid, spelius, and semispinalis muscles Includes C1-C2, 4 small pairs of muscles, multiple nerves, and vertebral artery Nerves: innervated by dorsal (posterior) rami of C1 spinal nerve = suboccipital nerve Principally a motor nerve to muscles of triangle Posterior ramus of C2 = greater occipital nerve o Principally a sensory nerve to the suboccipital region of posterior scalp o Action: main function is posture Emerges inferior to obliquus capitis inferior Stabilize upper cervical spine and skull Arterial Supply: Vertebral Artery Major occupant of the triangle Found at apex of triangle (WAYYYY deep in the space) Arises from subclavian arter in root of neck, passes through transverse foramina of all cervical vertebrae except C7, come together to form basilar artery at forament magnum Action: rarely involves single muscles coordinated and synergistic Rectus Capitis Posterior: Contains two 2 muscles major and minor Rectus Capitis Major: o Spinous process of C2 and inferior nuchal line o Superiormedial (top) border of triangle Rectus Capitis Minor: o Posterior tubercle of C1 and inferior nuchal line o Not part of suboccipital triangle Obliquus Capitis: form superiolateral and inferior borders of triangle Obliquus Capitis Superior: o Transverse process of C1 and between nuchal lines Obliquus Capitis Inferior: o Spinous process of C2 and transverse process of C1