* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Drugs and Food Interactions Which Increase The Effects Of Warfarin
Survey
Document related concepts
Transcript
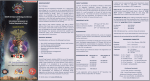
Drugs and Food Interactions Which Increase The Effects Of Warfarin Highly Probable Probable Alcohol (if concomitant liver disease), amiodorone, anabolic steroids, cimetidine, clofibrate, cotrimoxazole, erythromycin, fluconazole, isoniazid (600mg/d), metronidazole, miconazole, omeprazole, phenylbutazone, piroxicam*, propafenone, propranolol, sulfinpyrazone ( biphasic with later inhibition) Possible Acetaminophen, chloral hydrate, ciprofloxacin, dextropropoxphene, disulfiram, itraconazole, quinidine, phenytoin (biphasic with later inhibition), tamoxifen, tetracycline, flu vaccine Acetylsalicylic acid, disopyramide, fluorouracil, ifosfamide, ketoprofen, lovastatin, metozalone, moricizine, nalidixic acid, norfloxacin, ofloxacin, propoxyphene, sulindac, tolmentin, topical salicylates, cefamandole, cefazolin, gemfibrozil, heparin, indomethacin, sulfisoxazole *NSAIDS with no effect include: ketoralac, naproxen and ibuprofen Drug and Food Interactions Which Decrease the Effects Of Warfarin Highly Probable Probable Barbiturates, carbamazepine, chlordiazepoxide, cholestyramine, griseofulvin, nafcillin, rifampin, sucralafate, high vitamin K content foods, enteral feeds, large amounts of avocado Dicloxacillin Possible Azathiprine, cyclosporine, etretinate, trazodone Overdosage/Toxicity Guidelines INR Greater than the therapeutic level but < 5.0 Patient Situation Action and No significant bleeding Lower the dose or omit a dose and resume therapy at a lower dose when the INR is at a therapeutic level. * > 5.0 but < 9.0 and No significant bleeding Omit the next one or two doses, monitor the INR more frequently, and resume therapy at a lower dose when the INR is at therapeutic level. Alternatively, omit the dose and administer vitamin K, 1 to 2.5 mg orally, particularly if the patient is at increased risk of bleeding. If more rapid reversal is required because the patient requires urgent surgery, administer vitamin k, 2 to 4 mg orally, with the expectation that a reduction of the INR will occur in 24 h. if the INR is still high, administer an additional dose of vitamin K, 1 to 2 mg orally (all grade C compared with no treatment). >9 and No significant bleeding Hold off on warfarin therapy and administer a higher dose of vitamin K, 3 to 5 mg orally, with the expectation that the INR will be reduced substantially in 24 to 48 h. Monitor the INR more frequently and administer additional vitamin K if necessary. Resume therapy at a lower dose when the INR reaches the therapeutic level (all grade 2C compared with no treatment). with Serious bleeding Hold off on warfarin therapy and administer vitamin K, 10 mg by slow IV infusion, supplemented with fresh frozen plasma or prothrombin complex concentrate depending on the urgency of the situation. Administration of vitamin K can be repeated every 12 h ( grade 2C). > 20 *If the INR is only minimally greater than the therapeutic range, no dose reduction may be required ( grade 2C) For patients with life- threatening bleeding, hold off on warfarin therapy and administer prothrombin complex concentrate supplemented with vitamin K, 10mg by slow IV infusion. Repeat this treatment as necessary, depending on the INR (grade 2C). Available Tablet Strengths And Colors Of Coumadin Strength 1 mg 2 mg 2.5 mg 3 mg 4 mg 5 mg 6mg 7.5 mg 10 mg Color Pink Lavender Green Brown Blue Peach Teal Yellow White References: 1. Hirsh J, Dalen JE, Anderson DR, et al. Oral anticoagulants: mechanism of action, clinical effectiveness, and optimal therapeutic range. Chest 2001: 119; 8S-21S. 2. Ansell J, Dalen, JE, Anderson D, Deykin D. Managing Oral Anticoagulant Therapy. Chest 2001: 119; 22S-38S. Updated by: Keith T. Veltri, R.Ph., Pharm D. Candidate, St.. John’s University College of Pharmacy 2001 Warfarin (Coumadin) Flow Sheet Patient Name: Rm #: Date of Birth: Indication: Duration: Target INR: Start Date: Expected D/C Date: Recommended Therapeutic Range for Oral Anticoagulant Therapy Indications: INR: Prophylaxis of venous thrombosis (high-risk surgery) 2.0-3.0 Treatment of venous thrombosis Duration of Therapy Treatment of PE 12 mos-life : Prevention of systemic embolism Tissue heart valves AMI (to prevent systemic embolism) * Valvular heart disease AF Mechanical prosthetic valves (high risk) Bileaflet mechanical valve in aortic position 2.0-3.0 3-6 months: First event with reversible or timelimited risk factor 6 month : Idiopathic VTE, first event First event with: Cancer, until resolved Anticardiolipin antibody Antithrombin deficiency Recurrent event, idiopathic or with thrombophelia 2.5-3.5 2.0-3.0 *if oral anticoagulant therapy is elected to prevent recurrent MI, an INR of 2.5 to 3.5 is recommended, consistent with US Food and Drug Administration recommendations. DATE: CURRENT DOSE: INR: NEW DOSE: COMMENTS: