* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download What is Epidemiology
Meningococcal disease wikipedia , lookup
Traveler's diarrhea wikipedia , lookup
Leptospirosis wikipedia , lookup
Oesophagostomum wikipedia , lookup
History of biological warfare wikipedia , lookup
Bioterrorism wikipedia , lookup
African trypanosomiasis wikipedia , lookup
Marburg virus disease wikipedia , lookup
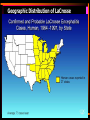
2009 flu pandemic by country wikipedia , lookup
Introduction to Outbreak Investigation Epidemiology What is Epidemiology? • “Epidemiology is the study of the distribution and determinants of healthrelated states or events in specified populations, and the application of this study to the control of health problems.” -CDC What is Epidemiology? • Science of Public Health that studies: – Distribution of disease – Determinants of health/disease – Specific populations • Look for patterns of disease – Time, place, personal characteristics • Interventions – Prevention is key What does Epidemiology study? • • • • Just about anything Health-related Infectious disease Chronic disease How is Epidemiology Used? • Population/community health assessment • Personal decision-making • Complete clinical picture • Evaluate interventions • Search for cause – Exposure and relationship to disease – Outbreak investigation Epidemiologic Information • • • • Case definition Person Place Time Case Definition • • • • Standard set of criteria Clinical and lab Allows for comparison Sensitive vs. Specific Case Definition • Smallpox – Clinical Description • An illness with acute onset of fever >101 °F followed by a rash characterized by vesicles or firm pustules in the same stage of development without other apparent cause. – Laboratory Criteria for Confirmation • Isolation of smallpox (variola) virus from a clinical specimen, or • Polymerase chain reaction (PCR) identification of variola DNA in a clinical specimen, or • Negative stain electron microscopy (EM) identification of variola virus in a clinical specimen (Level D laboratory or approved Level C laboratory) Suspected Case of Smallpox • A case that meets the clinical case definition but is not laboratory confirmed and does not have an epidemiological link to a confirmed or probable case of smallpox, OR a case that has an atypical presentation that is not laboratory confirmed but has an epidemiological link to a confirmed or probable case of smallpox. Atypical presentations of smallpox include a) hemorrhagic lesions OR b) flat, velvety lesions not appearing as typical vesicles nor progressing to pustules. Probable Case of Smallpox • A case that meets the clinical case definition that is not laboratory confirmed but has an epidemiological link to another confirmed or probable case. Confirmed Case of Smallpox • A case of smallpox that is laboratory confirmed. Case Definition Gradient Low Specificity High Specificity Suspected Probable Confirmed Working Case Definition • Smallpox Outbreak - Anyone who meets original case definition - Anyone with fever (>101 °F ) or rash who was in a confirmed exposed area during the BT event or came in contact with a confirmed or probable case should be considered a case. Person • • • • • Age Sex Race/Ethnicity Socio-Economic Status Behaviors Place • Geographic Distribution – Natural – Clustering vs. uniform • • • • Home Work School Hospital room Geographic Distribution of LaCrosse “Place” in LaCrosse Case Investigation • Neighborhood • Home visits • Mosquito Breeding Sites – Tires – Pots – Standing Water Clustered - Scattered - Time • • • • • • Onset of symptoms Incubation Period Infectious Period Seasonality Baseline vs. epidemic Interval • Long-term trends • Shorter for environmental exposure Measles Outbreak • • • • • • Baseline Normal occurrence Onset Incubation period Infectious period Mode of transmission Time in Outbreak investigation Visited health dept. Conference in Nairobi Home Church activities Rash onset ER Visit Health dept. notified IgM results Interventions 28 19 July 26 August 2 9 September 16 Measles Southwestern VA, 1999 5 Index case First generation case Second generation case Third generation case 3 2 1 0 24 57 81 11 0 -1 14 3 -1 17 6 -1 20 9 -2 23 2 -2 26 5 -2 8 29 -1 24 57 810 11 -1 14 3 -1 17 6 -1 9 Cases 4 September October Date of Onset Incidence •Number of new events occurring in a defined population during a specified period of time •Incidence = New cases/population at risk/time •Used to measure current disease activity •Allows comparison between areas with different populations Contrasts with Prevalence • Prevalence is the number of new and existing cases divided by the total population (can be during a period of time or at a given point) • Prevalence = (New cases + existing cases)/Total population - Can be expressed as a percent - Can give a picture of disease burden within a population Information for any outbreak • • • • • • • • • Symptom onset date Symptoms present and agent if known Suspected exposure date if known Residence Age Gender Laboratory testing Outbreak Case Definition Organized case information in a line list Exposure • Possible Cause of illness • Know your agent/disease – Clinical picture – Pathogenesis – Mode of transmission – Natural Reservoir – Common Vehicle or Vector Chain of Infection Transmission • Direct – Contact – Droplet • Portal of Exit • Portal of Entry • Indirect – Airborne – Vehicle – Vector • Mechanical vs. biologic Types of Outbreaks • Propagated – Indicative of person to person transmission • Point-source – Indicative of a common exposure to a contaminated vehicle or reservoir Measles Southwestern VA, 1999 5 Index case First generation case Second generation case Third generation case 3 2 1 0 24 57 81 11 0 -1 14 3 -1 17 6 -1 20 9 -2 23 2 -2 26 5 -2 8 29 -1 24 57 810 11 -1 14 3 -1 17 6 -1 9 Cases 4 September October Date of Onset Figure 3. Onset of Illness in Wilsonburg Grade School 20 18 16 Number of Cases 14 12 10 Sick 8 6 4 2 0 12pm 5/1 6pm 12am 5/2 6am 12pm 6pm 12am 5/3 Date and Time of Onset in 6 Hour increments. 6am 12pm 6pm Analytic Epi Studies • Associations between exposure and disease • Experimental • Observational – Cohort – Case Control – Cross-sectional Cohort Study • Objective: In a population of individuals initially free of disease, determine the risk factors associated with development of disease. – Select Population – Categorize individuals based on presence or absence of select risk factors – Follow individuals to determine which develop disease • Good for rare exposures Case-Control Study • Objective: Compare risk factors in diseased and non-diseased individuals to determine possible associations. – Select population – Select cases that meet the disease case definition – Select non-diseased individuals from the population to act as controls – Gather previous exposure/risk factor histories from both groups • Many outbreak investigations use this study design • Good for rare diseases John Snow and Cholera • “Broad Street Pump” – 1854 cholera epidemic in London – Looks at cholera deaths – Geographical mapping • Where do cases live? • Where do cases work? – Water source Use of Two-By-Two Tables • Calculate association between disease and exposure Ill Well Exposed a b Unexposed c d Total Total N ad/bc = Odd Ratio Relative Risk Interpreting Measures of Association • Odds ratios and risk ratios measure the degree of relatedness of an exposure and a health event (an outcome) • The farther away the OR/RR is from 1, the more we would say the exposure and outcome are associated • Confidence intervals and p-values help to determine if association is due to chance OR = 12 x 17/2 x 5 = 204/10 OR = 20.4 People who ate from menu A were about 20 times more likely to have diarrhea than those that did not eat from menu A. More OR interpretation • OR = odds of exposure among ill odds of exposure among well • If OR(RR) > 1, then the exposure is a risk factor for being ill • If OR < 1, then the exposure is protective of illness • If OR = 1, then there is no association between exposure and illness • OR can NEVER be negative! P-value • Used in LOTS of statistical tests • A guide to tell us that a result is “significant” • Generally at the 95% level • p < 0.05 = Significant at the 95% level = there is a 95% probability that the result is accurate (not by chance) • Example: OR=4, p-value=0.01 • Example: OR=15, p-value=0.36 95% Confidence Intervals • Used with risk ratios and odds ratios • Tell us about both precision and accuracy • With an OR or RR we have estimated the magnitude of the association – 95% confidence intervals tell us that we can be 95% sure that the true association is somewhere in that interval • Example: OR = 7 95%CI= (5.2, 8.8) • Example: OR = 7 95%CI= (0.4, 18.7) Strength of Association • Magnitude of Odd Ratio • 95% Confidence Interval or P-value • Be careful – Plausibility – Confounding Attack Rate AR = # of people who became ill x10n # of people at risk – People at risk could be those at a party, in a class, on a cruise ship… – Usually express AR as a %, so n = 2 Secondary Attack Rate • Measure of frequency of new cases among contacts of known cases SAR = # cases among contacts of primary cases during the period total # of contacts The calculations • • • • # # # # of of of of children in day care center = 70 ill children at day care center = 7 contacts (of those 7) at home = 25 ill contacts = 5 • AR = 7/70 = 0.1 x 100 = 10% AR • SAR = 5/25 = 0.2 x100 = 20% SAR Summary • • • • • Case definition, person, time, place Know disease/agent Recognize Point-Source vs. Propagated Set up analytic epi study Measures of association