* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Anticancer therapy education programme
Survey
Document related concepts
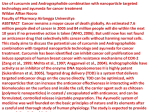
Transcript
North Trent Cancer Network North Trent Cancer Network Anticancer therapy education programme For health care professionals involved in the care of patients receiving intravenous, intramuscular, oral and/or subcutaneous anticancer therapy Health care professionals who are involved solely in the delivery of oral anticancer therapy should complete the North Trent oral anticancer therapy training programme. North Trent anticancer therapy education programme V3 October 2011 Page 2 of 97 Acknowledgements:Authors and contributors Joyce Burman, Doncaster and Bassetlaw NHS Foundation Trust Angela Gascoigne, Chesterfield Royal Hospital NHS Foundation Trust Anita Gill, Barnsley Hospital NHS Foundation Trust Pauline Pledge, Sheffield Teaching Hospitals NHS Foundation Trust Anne Pulfrey, Sheffield Teaching Hospitals NHS Foundation Trust Martin Salt, Sheffield Teaching Hospitals NHS Foundation Trust Gail Smith, Rotherham General Hospital NHS Foundation Trust Michel Thompson, Rotherham General Hospital NHS Foundation Trust Clare Warnock, Sheffield Teaching Hospitals NHS Foundation Trust Denise Wilkinson, Sheffield Teaching Hospitals NHS Foundation Trust Grateful thanks are given to all those who have provided their knowledge, expertise and time to the development of this Education Programme. Particular thanks are given to Lynda Campbell for her secretarial support in developing this document. First revision 2008 Clare Warnock, Sheffield Teaching Hospitals NHS Foundation Trust Second revision 2011 Clare Warnock, Sheffield Teaching Hospitals NHS Foundation Trust North Trent anticancer therapy education programme V3 October 2011 Page 3 of 97 North Trent anticancer therapy education programme V3 October 2011 Page 4 of 97 CONTENTS INTRODUCTION TO THE EDUCATION PROGRAMME MODULE 1 HEALTH AND SAFETY ISSUES Introduction Responsibilities with respect to Cytotoxic Drugs Protection of Staff Primary Route of Exposure Personal Protection Protect the Patient Protect the Environment Accidental Spillage, Contamination and Exposure to Cytotoxic Material Cytotoxic Chemotherapy Storage MODULE 2 HOW ANTICANCER THERAPY WORKS How anticancer therapy Works Mode of action of chemotherapy Biological agents: interferon, monoclonal antibodies Underpinning principles for anticancer therapy scheduling Aims of treatment MODULE 3 PRINCIPLES FOR THE ADMINISTRATION OF ANTICANCER THERAPY Introduction The Knowledge and Expertise of the healthcare practitioner Patient Information and Consent The role of Protocols in anticancer therapy The Provision of Supportive Therapy Assessment of Fitness to Receive Treatment Checking Procedures Measures to Prevent and Manage Acute Side Effects Administration of Intravenous anticancer therapy Vinca alkaloid administration Potential venous problems during intravenous administration of anticancer therapy Extravasation Extravasation Risk Factors Relating to Venous Access Steps for Assessing Patency Extravasation Risk Factors Relating to Drugs Extravasation Procedure Action to be Taken in and Extravasation Occurs Intramuscular/Subcutaneous Administration of anticancer therapy Oral anticancer therapy North Trent anticancer therapy education programme V3 October 2011 Page 5 of 97 MODULE 4 SIDE EFFECTS OF ANTICANCER THERAPY Anaphylaxis Nausea and vomiting Bone marrow depression Neutropenia Thrombocytopenia Anaemia Alopecia Altered bowel habit • Diarrhoea • Consiptation Cardiac toxicity Changes in cognitive function Central nervous system effects Fatigue Fertility Haemorrhagic cystitis Hand foot syndrome Mucositis (oral problems) Nephrotoxicity Neurotoxicity (including oxaliplatin pharyngo-laryngo dysesthesia) Pulmonary toxicity Skin reactions Tumour lysis syndrome MODULE 5 PATIENT ADVICE/INFORMATION Patient Information and anticancer therapy Patient Advice MODULE 6 ANTICANCER THERAPY COMPETENCY ASSESSMENT Definition of Terms Summary of Assessment Pathway Theoretical Assessment for the administration of anticancer therapy Practical assessments for the administration of anticancer therapy • Oral assessment • Intramuscular assessment • Infusional Assessment • Bolus (Peripheral) Assessment • Bolus (CVAD) Assessment References North Trent anticancer therapy education programme V3 October 2011 Page 6 of 97 1. Introduction to the Education Programme This is the third edition of the North Trent Cancer Network modular competency based training and assessment programme addressing all aspects of delivering anticancer therapy. The programme contains all of the elements necessary for health care practitioners to maintain the highest standard of care to cancer patients receiving anticancer therapy across the network. Anticancer therapy is the term used to describe non surgical and non radiotherapy based cancer treatment. It includes chemotherapy and biological therapies (for example, monoclonal antibodies). For the purpose of this education programme it does not include hormone based treatments. This training programme covers the following methods of delivery of anticancer therapy: • Intravenous infusion • Intravenous bolus • Intramuscular or subcutaneous • Oral This programme does not cover the following: • Paediatric anticancer therapy • Intrathecal chemotherapy. This is a separate procedure with its own rules and regulations to govern its practice. Health care professionals who are involved solely in the delivery of oral anticancer therapy should complete the North Trent oral anticancer therapy training programme. This has been designed for staff involved in assessing, administering or providing patient information to patients receiving oral anticancer therapy but who are not involved in administering intravenous, intramuscular or subcutaneous treatment. 2. Who the Programme is designed for The programme has been designed to support all healthcare professionals whose role may bring them into contact with anticancer therapy. Practitioners must fulfil the following criteria, agreed by the North Trent Cancer Network: • Registered health care practitioners who have at least six months post registration experience and have completed their local preceptorship programme Practitioners who have been assessed as competent in anticancer therapy/ chemotherapy administration using the North Trent training programme and have had a period of non-practice greater than three months (eg career break or secondment) must be assessed as safe to practice on an individual basis. Further training can be identified where necessary. Practitioners transferring from other NHS organisations who have completed a anticancer therapy/chemotherapy training programme will undertake theoretical and practical assessment as deemed appropriate by their manager. This must include • reading the North Trent anticancer therapy education programme and • a minimum of one practical assessment of competence for each route of administration they will be carrying out as part of their role. North Trent anticancer therapy education programme V3 October 2011 Page 7 of 97 3. Aims of the Programme This Anticancer therapy Education Programme is aimed at practitioners who administer and provide care for patients receiving anticancer therapy. The care of patients is directed towards safe practice and the prevention, early detection and minimisation of complications. Care is also directed towards the giving of information and support at a level and pace appropriate to the individual patient. The core principles that underpin the training programme are that practitioners will: (i) Understand the dimensions and limitations of their role. (ii) Know and understand the principles of safe administration and disposal of cytotoxic agents. (iii) Understand their personal accountability for practice under their appropriate professional regulations (e.g. the Nursing and Midwifery Council (NMC) Code of Professional Conduct) with particular emphasis on competence, personal accountability for practice and consent. (iv) Understand where their role involves the administration of anticancer therapy they must undertake specific training to the role (provided by the employer). The employee must not be involved in the administration of anticancer therapy until they are deemed competent to do so. (v) Understand that nurses will not be involved in the reconstitution of cytotoxic drugs. (vi) Understand that contact with anticancer therapy can be harmful to the unborn baby. Employees must let their employer know if they are pregnant and a risk assessment completed. You must NOT reconstitute or administer anticancer therapy if pregnant. Specific to intrathecal chemotherapy All staff will clearly understand that they must not be involved in the checking or administration of intrathecal cytotoxic chemotherapy until they have successfully completed specific intrathecal training requirements. 4. Learning Outcomes The expectations are that at the end of the education programme the healthcare practitioner will be able to: (i) Give an explanation of the ways in which anticancer therapy works (ii) Describe the principles behind the safe administration of anticancer therapy and the management and care of central and peripheral intravenous pathways (iii) Demonstrate knowledge of the anticancer therapy drugs used within the speciality, their toxicities and the short and long term side effects. (iv) Demonstrate knowledge of the equipment available to safely control the administration of anticancer therapy. (v) Demonstrate a knowledge and understanding of issues relating to safe handling and disposal of cytotoxics including: • COSHH regulations and local arrangements and policies for the safe storage and disposal of cytotoxic drugs. • Local policies relating to anticancer therapy and: • Personal protection (protective clothing, safe handling of cytotoxic drugs, handling of bodily waste). • Pregnancy. • Patient safety • Maintaining a safe environment. • Managing a cytotoxic spillage North Trent anticancer therapy education programme V3 October 2011 Page 8 of 97 (vi) (vii) Explain how good practice and adherence to policy is paramount in the prevention of extravasation. The health care practitioner (HCP) will also be able to describe the principles behind the early detection and management of extravasation Demonstrate knowledge and awareness of risk management, risk assessment and control measures surrounding anticancer therapy including knowledge of untoward incidents, appropriate action and their Trust’s reporting mechanisms. Responsibilities with Respect to Cytotoxic Drugs All staff involved in the administration, checking and storage of anticancer therapy should be familiar with the policies and procedures governing this practice. All staff have the following responsibilities: (i) (ii) (iii) (iv) strict adherence to the local procedures for checking anticancer therapy prior to administration including confirming that the prescription is safe and appropriate correct use of storage facilities required for anticancer therapy including correct temperature storage. consistent use of correct administration techniques and protocols. This includes ensuring all supportive therapy including pre-medication, anti-emetics and hydration fluids have been administered and the correct use of appropriate giving sets (including an in-line filter where applicable). maintaining a safe environment before, during and after administration. This includes assessing any risks to safe administration and the taking of appropriate action when there are compromising risk management issues involved in administering anticancer therapy identified. North Trent anticancer therapy education programme V3 October 2011 Page 9 of 97 MODULE 1 HEALTH AND SAFETY ISSUES (Please also refer to your local Health and Safety Policy) Introduction All staff have the responsibility to work within national and local policies e.g. Health and Safety at Work Act, Control of Substances Hazardous to Health (COSHH) and their local Health and Safety Policy. Maintaining a safe environment before, during and after administration is an essential component of safe practice. All HCP’s involved in anticancer therapy administration must assess any risks to safe administration on an ongoing basis. They must take appropriate action when compromising risk management issues are identified. Anticancer therapy will only be given in designated areas which are identified locally. Hazards to health have been identified for staff preparing and administering cytotoxic drugs as they have been identified as mutagenic, teratrogenic and carcinogenic (Dougherty and Lister 2008). This means they can potentially harm fertility, cause foetal damage and cause cancer. Because of these risks the Health and Safety Executive introduced guidelines governing the use of cytotoxic chemotherapy within the regulations called ‘Control of Substances Hazardous to Health’ (COSHH). The aim of a policy for handling and administering cytotoxics drugs is to prevent exposure or reduce it to a minimum. Protection of Staff There is a large body of evidence to suggest that healthcare personnel need to be adequately protected to ensure they are not exposed to potentially harmful substances when involved in the preparation and administration of cytotoxic drugs. Measures must be taken to reduce exposure Primary Routes of Exposure There are three routes of exposure to anticancer therapy: (i) (ii) (iii) Absorption through the skin. Inhalation. Ingestion (administering treatment and then eating something without washing your hands would be one way in which this could occur). Exposure to anticancer therapy is most likely to occur during drug preparation and administration but there are other times when staff can be exposed. For example, some anticancer therapy drugs can be excreted in the patients bodily fluids for up to 7 days post administration. Staff will be exposed to this when handling and disposing of body waste. It is important to wear gloves and aprons when handling body fluids/waste and pay careful attention to hand washing techniques (Tadman and Roberts 2007). Patients and relatives need to be informed about this risk of exposure from body fluids before they go home so that anyone coming into contact with the patient’s body fluids wears gloves and washes their hands afterwards. Patients should also be aware that anticancer therapy may be present in seminal fluid and vaginal secretions so a barrier method of contraception should be used if the patient has sexual intercourse in the week following treatment (Foster 2002). Patients on a continuous course of oral chemotherapy should use a barrier method of contraception for the duration of their treatment. North Trent anticancer therapy education programme V3 October 2011 Page 10 of 97 As a result of studies performed on nurses, pharmacists and pharmacy technicians, a number of safety measures have been introduced to protect personnel handling anticancer therapy drugs. Preparation and/or reconstitution of cytotoxic drugs can only be carried out by pharmacy staff in a specially equipped area; no other staff should undertake this task. There are specific procedures and protocols for pharmacy staff to adhere to within their departments to ensure their protection. There are a few exceptions where a drug has a very short expiry once reconstituted which make it logistically very difficult for pharmacy to prepare e.g. each formulation of asparaginase. Where this is the case policies and procedures must be in place and followed to ensure this is achieved safely. Warning: under no circumstances may staff who are pregnant or who suspect they may be pregnant be involved with: Administering cytotoxic drugs. Cleaning up a cytotoxic spillage. Handling cytotoxic patient waste. • • • Personal Protection A number of regulatory requirements have been set to protect healthcare personnel who prepare or administer cytotoxic drugs. Disposable gloves, a plastic apron and eye protection must be worn when directly dealing with cytotoxic drugs to protect skin and clothing. Gloves and plastic aprons should always be worn when dealing with patient’s waste which can be disposed of following the standard waste management procedures (Allwood, Stanley and Wright 2002). The most important method of protection is common sense and good technique. • • • Gloves – Disposable gloves must always be worn when handling anticancer therapy. Aprons – Should be made of plastic or low permeability material. Goggles – See local policy. Protect the Patient Care must be taken to prevent accidental spillage of the cytotoxic agents onto the patient’s clothing and skin. This can be achieved by using a plastic covered pillow and/or a plastic backed dressing sheet placed under the patients arm or line when administering the treatment. Protect the Environment Care should be taken to prevent contamination of the area in which the drugs are being administered. A hard plastic tray with a raised edge must be used for transportation and containment of the drugs. Luer lock syringes must be used for all bolus anticancer therapy. Accidental Spillage, Contamination and Exposure to Cytotoxic Material All accidental spillages, contamination and exposure to cytotoxic drugs involving ingestion, inhalation or contamination of the skin, must be dealt with immediately and first aid measures must be administered as soon as possible. North Trent anticancer therapy education programme V3 October 2011 Page 11 of 97 Cytotoxic drug Spillage Refer to North Trent spillage policy. A spillage kit must be available in areas where anticancer therapy is being administered. Skin Contamination Immediately wash the area with copious amounts of soap and water Eye Contamination Immediately irrigate the eye with a sterile eyewash solution (or water, if eyewash solution is not available), as some cytotoxic drugs may cause corneal ulceration. The affected eye must be examined by a medical practitioner experienced in carrying out ophthalmic assessment. Clothing Contamination Immediately change clothing and treat as contaminated linen. All staff have the responsibility to report accidents, untoward incidents and near misses using their Trust’s incident reporting system. Cytotoxic Waste Disposal Anticancer therapy must be disposed of safely to minimise the potential of contamination to all groups of staff involved in waste management. Anticancer therapy is disposed of separately from other waste. Refer to local policies for specific waste management procedures. Risk assessments The health care practitioner involved in administering anticancer therapy must maintain a safe environment before, during and after administration. Where they feel there are compromising risk management issues involved in administering cytotoxics (eg visitors), s/he must take action to reduce that risk to an acceptable level before proceeding further. Where the risk issue cannot be resolved, s/he must inform the nurse in charge, physician and pharmacy of the problem. An incident form must be completed, and concise documentation made within the nursing record where appropriate. Storage Anticancer therapy must be stored as directed by the Pharmacy Department, ensuring that COSHH regulations are complied with. Items that have not been stored correctly may become quickly unusable, and may not be available out of normal working hours. This may compromise the patient’s treatment by causing unnecessary interruption. Correct storage will also prevent expensive wastage of drugs. As soon as treatment arrives from pharmacy the correct storage method must be identified on the pharmacy label. Where refrigeration is required, it should be stored in designated temperature monitored fridges in the clinical area. Once reconstituted anticancer therapy has a relatively short time in which it can be used. Attention should be paid to the expiry dates, particularly where there is more than one bag or syringe of the same drug. Anticancer therapy should not be administered directly after removal from the refrigerator to prevent venous spasm and vein pain. Each item of treatment will be contained is a sealed plastic bag. These bags should not be opened until the drug has been checked and is about to be administered. North Trent anticancer therapy education programme V3 October 2011 Page 12 of 97 MODULE 2 HOW ANTICANCER THERAPY WORKS How Cytotoxic Chemotherapy Works The Cell Cycle The cell cycle is the process by which cells divide and reproduce. The cell cycle has five stages: • Go - resting phase. During this stage the cell will be fulfilling its normal function and will not be reproducing. • G1 - growth phase where the cell prepares enzymes for synthesis required in the S phase • S - synthesis phase where DNA replication occurs • G2 – further growth and preparation for mitosis. During this phase the cell contains both its original, and its replicated DNA. • M – mitosis – cellular division during which the cell physically becomes two cells. In health, cellular division is a carefully regulated process in which cell division is triggered by the death of a cell. The genes that are responsible for regulating cell division are called oncogenes and tumour suppressor genes. Oncogenes produce proteins such as growth factors which drive cellular division; tumour suppressor genes block growth signals and act as the brakes to cellular division. In a cancer cell, mutations in these genes alter the control of cellular division. Oncogene mutation leads to too much, or the wrong type, of growth protein being produced while tumour suppressor gene mutation leads to a reduction in the ability to halt cell division. Either or both of these changes can lead to uncontrolled and frequent cell replication. Chemotherapy, works by disrupting the process of cell division. It is often more effective on cells which are dividing so it has a greater effect on cancer cells which divide more frequently than healthy cells. The rate of cell division in cancer cells is influenced by a number of factors including: The doubling time The rate of growth of a cancer is described as the doubling time – i.e. the amount of time it takes for a cancer to double in size. This can vary from hours to months. The doubling time is influenced by the characteristics of the parent cell (the cell which gave rise to the cancer). For example, the doubling time of a teratoma - average three weeks, is faster than that of a colorectal cancer - average three months (Tadman and Roberts 2007). Cancers which have a faster doubling time are more likely to have cells which are actively dividing. This can make them more susceptible to the action of chemotherapy. The degree of differentiation The degree of differentiation describes how closely the cancer cell resembles a mature functioning cell. A well differentiated cell has a close resemblance to a mature cell, while an undifferentiated cell bears little resemblance. The degree of differentiation is referred to as the grade of a cancer. Less differentiated cells will have fewer similarities to a mature cell; they tend to divide more frequently and are more likely to metastasise. These are termed high grade cancers. The size of the cancer Cancer growths which are smaller in size tend to have a faster growth rate and are more likely to have replicating cells North Trent anticancer therapy education programme V3 October 2011 Page 13 of 97 Mode of action of chemotherapy Chemotherapy drugs can be classified by their mode of action. Some chemotherapy drugs work at particular points in the cell cycle – these drugs are called cell cycle phase specific. For example: • aspariginase acts on cells in G1 phase, when enzmes are being synthesised in preparation for the S phase of the cell cycle • 5-flurourcil (5-FU) and methotrexate act in the S phase when the cell is replicating its chromosomes • bleomycin and etoposide act on cells in the G2 phase • vinblastine acts in the M phase when cells divide. Other chemotherapy agents are non cell cycle phase specific and can work at any point in the cell cycle, including the resting phase, G0, when the cell is not dividing Chemotherapy drugs have different modes of action. Examples are as follows: Alkylating Agents (e.g. cyclophosphamide, cisplatin, melphalan) These work by causing abnormal formation of the “new” DNA during mitosis ensuring that the DNA strands are not able to separate. Antibiotics (e.g. doxorubicin, epirubicin) These work by interfering with the production of DNA and prevent the DNA strands separating. Antimetabolites (e.g. methotrexate, gemcitibine) These work by “imitating” normally existing metabolites which are required for successful cell division. Antimetabolites are taken up by the cell during the resting phase, and they then prevent the cell from continuing in the cell cycle. They are cell cycle specific. Mitotic inhibitors (e.g. vinca alkaloids, taxanes) Vinca alkaloids: act by blocking cell division (mitosis) and are therefore cell cycle specific to the M phase. taxanes: prevent mitosis by binding to microtubules Log kill One term which is used to describe an underlying principle of how chemotherapy works is log kill. The log kill is a measure of the cells killed as a percentage of the total number/size of the tumour. The aim of chemotherapy is to reduce the number of cells to a level where the body’s immune response can take over and destroy the remaining cancer cells. This is why treatment often continues even when the tumour is no longer visible on scan. Beyond a certain size the tumour is too small to see but there is always the risk that some cells may still be present. North Trent anticancer therapy education programme V3 October 2011 Page 14 of 97 How biological therapies work Biological therapies aim to produce an anti-cancer effect either by activating the patient’s immune system or by administering natural substances present in the immune system as treatments (Tadman and Roberts 2007). Immunotherapy Interferon is produced by the immune system in response to viral infections. Interferon as a cancer treatment acts on a cancer by • Interfering with tumour cell growth • Affecting the expression of oncogenes • Making tumour cells more vulnerable to being killed by the immune system • Reducing the amount of blood vessels around a tumour (Tadman and Roberts 2007) Interferon is used most often in the treatment of leukaemia, lymphoma and renal call carcinoma. Monoclonal antibodies Monoclonal antibodies are designed to bind specifically to cell surface molecules or protein markers expressed by a cancer cell. The monoclonal antibody recognises the specific protein markers and locks onto them. They then have several modes of actions including: • Blocking/inhibiting the growth signal pathways • Recruiting the bodies immune system to attack and kill the cancer cell • Inducing cell lysis (the death of a cell due to break down of the cell membrane) Monoclonal antibodies have different modes of action for example: Herceptin The human epidermal growth factor-2 (HER2) plays a role in the regulation of normal breast growth and development. However, in some breast cancers HER2 is overexpressed leading to unregulated cell growth. Herceptin is a targeted therapy for HER-2 over-expressing cancers. It binds to the HER2 receptor site and inhibits the effects of the growth factor (Cooke 2000). Rituximab Rituximab has been designed to bind to a molecule called CD20, a cell surface protein expressed in around 93 percent of patients with B cell lymphoma. Once it is attached to the CD20 molecule, rituximab attracts other immune cells to the protein and these induce apoptosis (cell death) in the cancerous cell (Feltham 2008). Bevacizumab (Avastin®) Cancer growths need to develop their own blood supply to be able to grow and survive. This process is called angiogenesis. Bevacizumab is a monoclonal antibody targeted against vascular endothelial growth factor (VEGF), which plays a key role in the process by which tumours develop their own blood supply. Bevacizumab is an anti-angiogenic treatment which binds to VEGF to inhibit the development of the blood supply to the cancer (Blowers and Hall 2009). North Trent anticancer therapy education programme V3 October 2011 Page 15 of 97 Tyrosine kinase inhibitors (TKI’s) Growth factor receptors known as the erbB or HER receptors are found on several different types of cancer cells. These receptors play a role on the normal processes of cell growth and development. However in some cancers these growth receptors are over-expressed leading to unregulated cell growth. One of the ways in which these growth receptors function is through the activation of a protein inside the cell called a tyrosine kinase enzyme. This protein can cause the cancer cell to grow. Drugs have been developed to inhibit the activation of this enzyme which may then stop the cell dividing. These drugs are called tyrosine kinase inhibitors (TKI’s). Examples of TKI’s include Erlotinib/Tarceva®, Sunitinib/Sutent®, Imatinib/Glivec® and lapatinib. Underpinning principles for anticancer therapy The aim of anticancer therapy is to maximise the destruction of the cancer cells while minimising the damage to the normal cells. Two approaches which are used to achieve this are: 1) administering combinations of anticancer therapy drugs and 2) administering anticancer therapy drugs in cycles (Souhami and Tobias 2005). Combinations of drugs Anticancer therapy regimens frequently include the administration of more than one type of drug. For example, R-CHOP involves the administration of the following drugs: rituximab, doxorubicin, vincristine and cyclophosphamide. High dose steroids – prednisolone - are given as part of this regimen. The principles that underpin this practice are as follows: The different modes of action of each of the drugs can be used to combined and greater effect. o This effect can be achieved at lower and safer doses than if only one drug was being given As cancer growths are often comprised of different types of cell with varying sensitivities to different drugs, giving drugs with different modes of action increases cell kill Combining drugs that have different side effects allows an increased destruction of the cancer cells with a reduction in the overall incidence and severity of side effects o Each of the drugs that are given within the regimen should have different side effect profiles as much as possible Scheduling of anticancer therapy in cycles In a course of anticancer therapy there are planned intervals between the administration of each dose and/or cycle of treatment. The principles that underpin this practice are as follows: each time treatment is given only a proportion of the cancer cells are killed. The number of cells killed increases with the number of cycles given. some chemotherapy agents work at specific points in the cell cycle. The intervals increase the chance of cells being in this phase when the treatment is given the intervals allow for the recovery of healthy cells. Cancer cells are poor at cell repair while normal healthy cells can repair sub-lethal damage North Trent anticancer therapy education programme V3 October 2011 Page 16 of 97 When combining and scheduling anticancer therapy the following factors are considered: The intervals between doses are a balance between the time required to allow normal cells to recover while minimising the opportunities for the cancer to continue to grow The intervals allowed often reflect the recovery time required for a particular drug. For example, carboplatin is often given four weekly to provide enough time of the bone marrow to recover The aims of treatment Drug regimen selection will take into consideration the intentions of treatment, for example curative or palliative. Curative The aim of curative treatment is to eradicate all measurable disease. It is given when there is a good potential for cure – for example the cancer is very sensitive to anticancer therapy (e.g. lymphoma, teratoma) or the cancer is being treated at an early stage. Curative treatment is more likely to be intensive and may involve administering drugs with a high side effect toxicity profile. Efforts are made to reduce delays in the treatment schedule and avoid dose reductions where possible as this can impact on the potential outcomes of treatment. Palliative The aim of palliative treatment is to extend survival, alleviate symptoms and improve quality of life. Palliative treatment should carefully balance the potential long and short term benefits that could be gained from treatment against the potential distress associated with side effects and the impact of treatment on quality of life. Adjuvant Anticancer therapy is frequently given alongside other cancer treatments such as radiotherapy and/or surgery. The term used to describe this is adjuvant treatment. Anticancer therapy can also be given before another cancer treatment with the aim of reducing the size of the cancer growth to increase the potential effectiveness of surgery or radiotherapy. When given before another treatment the term used is neoadjuvant. North Trent anticancer therapy education programme V3 October 2011 Page 17 of 97 MODULE 3 PRINCIPLES FOR THE ADMINISTRATION OF ANTICANCER THERAPY Introduction It is expected that all staff will perform informal risk assessments as part of their roles in relation to anticancer therapy. Staff should act appropriately in addressing any identified area of concern to prevent any untoward incident. Where wider issues are identified in relation to cytotoxic treatment as part of an informal risk assessment, a formal risk assessment should be implemented as soon as possible. Key principles govern the administration of anticancer therapy all routes. These relate to: The knowledge and expertise of the staff administering treatment. Patient information and consent. The role of protocols and calculation of doses. Providing appropriate supportive treatments (eg anti-emetics, hydration fluids). Assessment of whether the patient is fit to receive treatment. Checking procedures. The prevention and management of acute side effects. (RCN 2010, Dougherty and Lister 2008). The Knowledge and Expertise of the HCP Staff involved in the administration of chemotherapy should have received appropriate education and training in order to gain the knowledge and skills required. This involves developing a good understanding of the following aspects of care: The health and safety issues associated with handling, administering and disposing of cytotoxic material (see Module1). The key components of patient care including: • Consent, patient information, education and support Knowledge of the drug: Drug properties (vesicant or non vesicant), appropriate method of administration, short and long term side effects and potential adverse reactions • Common regimens and protocols including: • Dose calculations, supportive treatments, rate and route of delivery and the range of appropriate doses. Competence in the techniques required for delivering chemotherapy. • For example, IV drug administration, infusion equipment competence, cannulation skills, CVAD skills • Where possible these competencies should be gained in the administration of less toxic substances before learning to use them in the administration of chemotherapy North Trent anticancer therapy education programme V3 October 2011 Page 18 of 97 Patient Information and Consent Consent Before receiving anticancer therapy the patient needs to provide informed consent. Written consent is required before treatment is commenced and every time the regimen is changed. It is also important to determine whether or not the patient is willing to proceed prior to each treatment. Informed consent goes beyond the patient signing their name on a form. Davies (2003) states that “it is the outcome of a process of communication between the health professional and the patient over the nature of their treatment alongside a discussion of the possible risks and benefits of treatment”. The patient should be fully informed of the details of treatment; specifically when, where and how it will be given, possible side effects, how to prevent and manage them and how to contact the treatment centre for advice and support. Patients should also be provided with written information (see module 5 for further details on patient information). Fertility Some anticancer therapies have an impact on fertility and can cause infertility at standard or high doses. Other agents can have an effect on fertility but the actual effect depends on a range of factors including age, individual susceptibility and the patients level of fertility prior to commencing treatment (Davies 2003, Knobf 2006, Royal College of Physicians 2007, Thaler-DeMers 2006). Male patients receiving treatment that could effect fertility should be offered the opportunity of sperm banking. For female patients it is possible to store fertilised ova. However, this can be difficult to achieve as it can take a few months for this process resulting in treatment delays. It is vital to check that these issues have been discussed with the patient prior to administering treatment. Women can remain fertile during treatment even if their menstrual cycle becomes disrupted or stops and they should be advised to use effective contraception during and after treatment. It has been proposed that effective contraceptive precautions should be recommended in all males and females once treatment is commenced and for at least one year after it is completed (Royal College of Physicians 2007). The Role of Protocols in anticancer therapy Anticancer therapy administration is governed by the use of protocols. Protocols set out the number of days over which a regimen is given, when specific drugs are to be given, the dose of each drug and any supportive treatments. There are many different protocols used in haematology and oncology and it is important that you have a good understanding of the protocols commonly used in your clinical area. You should also have easy access to information on any treatment protocols that you are using. Scheduling of Drug Administration The protocol identifies the number of days over which a regimen is given (referred to as a cycle) and when specific drugs are to be given within the cycle. The number of days in a cycle varies between protocols, for example, some protocols may have a 28 day cycle others a 21 day cycle. The following is an example of drug schedule within a protocol. The Gemcitabine/Carboplatin lung protocol is a 21 day regimen. Patients receive Gemcitabine on days 1 and 8 and Carboplatin on day 1. They then have a break for the rest of the cycle. Twenty-two days after starting cycle 1 they begin day 1 of cycle 2. North Trent anticancer therapy education programme V3 October 2011 Page 19 of 97 Calculation of Dose Treatment protocols also determine the dose of the drugs to be given to each patient as the dose is often dependant on the patient’s body surface area (BSA). This approach to calculating doses of anticancer therapy plays a role in maintaining the therapeutic ratio; the dose that balances maximum cancer cell kill with safe or manageable levels of side effects/toxicities. Giving too little can reduce the potential benefit from treatment in terms of cure/survival, giving too much can cause severe side effects that the patient may not be able to tolerate. An accurate measurement of BSA is an essential component of safe anticancer therapy administration. As a patient progresses through their treatment their BSA will need to be reviewed prior to each cycle as significant weight loss or gain require a change in the doses prescribed. The unit of measurement for BSA is metres squared (M2) and it is calculated from the patient’s height and weight. Once the BSA is known the dose of each drug is calculated by multiplying the protocol dose by the BSA. For example, according to the protocol a dose of chemotherapy is 50mg per M2 the patient has a BSA of 1.8 M2. The dose is calculated (50 X 1.8 = 90 mg) so this patient would receive 90 mg of the drug. The Provision of Supportive Therapy Treatment protocols also stipulate the administration of other drugs that are given to minimise or prevent side effects. Examples are contained in table one. Table 1: Examples of supportive therapies for specific anticancer therapies Name of supportive therapy When it is given 0.9% Normal Saline infusion 1 – 2 litres Before and after Cisplatin. Folinic acid Twenty four hours Counteracts the action of Methotrexate and after reduces severity/incidence of mucositis and Methotrexate bone marrow suppression. administration Ifosfamide produces a metabolite called IV infusion with acrolein that can damage the urothelium Ifosphamide. (lining of the urinary tract). This can cause haemorrhagic cystitis. Mesna reacts with acrolein to prevent this damage . Mesna Chlorphenarimine, Paracetamol, Steroids Cisplatin is renal toxic. IV fluids are given to promote diuresis during and post Cisplatin administration to ensure the drug passes rapidly through the renal system. Prior to Rituximab North Trent anticancer therapy education programme Why it is given To reduce the severity and incidence of hypersensitivity reactions V3 October 2011 Page 20 of 97 Appropriate antiemetics are also identified in the protocol. Many agents cause nausea and vomiting, but the degree of severity, referred to as the ematogenic potential, varies. Those drugs that have medium to high ematogenic potential eg Cisplatin and Doxorubicin have antiemetics, such as Graniestron and Dexamethasone, prescribed as part of the protocol for the regimen. Patients who are receiving treatment with a lower ematogenic potential have “as required” antiemetics prescribed. Where regular antiemetics are prescribed it is important to ensure they are administered while the patient is in hospital and/or the patient is advised how and when to take them once they have been discharged home. Assessment of Fitness to Receive Treatment The patient’s physical, psychological, emotional and social needs will be assessed prior to the commencement of each course of treatment. Appropriate referrals will be made as a result of this assessment. Prior to receiving anticancer therapy a number of tests will be carried out to identify whether it is safe for the patient to receive a particular treatment. The tests required are usually identified in the protocol. Some tests are carried out to ensure the patient is able to tolerate the potential toxicity of the drug. Examples include: • • • Renal function tests before giving drugs that are renal toxic eg Cisplatin Blood pressure checks prior to monoclonal antibodies associated with hypertension (e.g. bevacisumab, sunitinib) Cardiac investigations prior to giving cardiotoxic drugs eg Doxorubicin, herceptin (Mallinson 2003). Other tests are carried out to ensure that the patient is fit enough to receive treatment. Blood tests of renal and liver function and full blood count are routinely carried out when a patient is receiving chemotherapy, usually prior to each course. These include: Blood Chemistry (U&E’s) and Liver Function (LFT’s) Many anticancer therapy agents are activated in the liver and/or excreted via the kidneys. Assessing renal and liver function provides an indication of whether the patient will be able to effectively metabolise and excrete the drugs being given. Full Blood Count (FBC) Bone marrow depression is a potential side effect of many anticancer therapy agents (see page 41). To minimise the risk of infection, sepsis and/or bleeding the patient’s white cell, platelet and haemoglobin counts need to be above a certain level before treatment can be given. Before the first dose of anticancer therapy the FBC can be taken one to two weeks earlier, but once the patient has started a course of treatment it should be checked 1 to 2 days before the next treatment is given, unless stipulated otherwise. This is to ensure that the FBC is adequate as counts can change over a few days depending on where the patient is in the treatment cycle. The low point usually occurs 5 to 10 days after administration (see page 38). There may be exceptions to this depending on factors such as diagnosis or regimen and this should be checked against the local protocols. North Trent anticancer therapy education programme V3 October 2011 Page 21 of 97 Checking Procedures Prior to the administration of anticancer therapy the environment must be checked, this should include the availability of: • Cytotoxic spillage kit. • Anaphylaxis kit. • Eye Contamination Kit. • Extravasation kit. • Cytotoxic waste disposal. • Resuscitation equipment. As with all drug administration it is essential that procedures are in place to ensure that the right treatment is given to the right patient at the right time. However, this is particularly important with anticancer therapy as it presents special dangers because • many agents have a narrow therapeutic index and are toxic even at therapeutic dosages, • anticancer therapy regimens are highly complex and • the timing of administration of particular drugs is dependant on the protocol that the patient is receiving (Schwappach 2010). Checking procedures to minimise the potential for errors are set out clearly in local anticancer therapy administration procedures. It is vital to ensure that the correct drug is given to the correct patient at the correct time. Prior to administering treatment the practitioner should check the following: The Patient • Understands their treatment including the side effects, measures they could take to minimise or prevent them and the actions to take if they occur. • Has provided informed consent and feels prepared and supported. • Has been assessed by the appropriate health care practitioner (HCP) as being fit to receive the treatment. • Has had the tests specified by the protocol carried out (including FBC and other appropriate tests) and these have been assessed as satisfactory by an appropriate health care professional. The Prescription The practitioner should check that the prescription: • Is clear, unambiguous, accurate and appropriate for that patient that day. • Clearly identifies the route of administration that is appropriate for the protocol. • Includes all concurrent medication or fluids that are part of the protocol (NMC Standards for medicines management 2008, Dougherty and Lister 2008) The practitioner will ensure the correct drug is given to the correct patient at the correct time. This involves checking the following against the prescription with a second registered nurse; drug name, dose, diluent (type and volume), expiry date, date and time for administration, route of administration, duration and/or rate of infusion. The prescription must have been signed by the doctor and have been verified by a pharmacist. North Trent anticancer therapy education programme V3 October 2011 Page 22 of 97 The identity of the patient must also be checked by the same two registered nurses. This should take place next to the patient and include checking the patients name, patient identification number and date of birth. Shulmeister (2008) identifies a wide range of possible factors which can increase the risk of patient misidentification including: • mispronouncing the patients name, • referring to patients by their first name only, • passively checking the patients name rather than asking them to state it, • not using wristbands, • taking shortcuts in checking such as checking the patients identification at the initial drug administration but not as subsequent administrations, • using face recognition based on a belief that you know your patients. Efforts must be made to minimise the potential of these factors to occur by using correct checking procedures. In particular the patient must be involved in this check whenever this is possible by being asked to state their name and date of birth. Where this is not possible (for example language or communication barriers) extra caution and additional actions may be required to ensure patient safety. Evidence from survey studies shows that patients frequently observe, report, and intercept errors. For example, patients recognize that incorrect drugs or incorrect doses of the correct drug are being given or that devices such as infusion pumps have malfunctioned. As patients are the only individuals present during every treatment and consultation, they are a valuable resource for safe delivery of anticancer therapy (Schwappach 2010). They should not be relied on to detect errors but involving the patient in their care and listening to their concerns, along with safe checking procedures and administration systems, can help to reduce the potential for mistakes. Assessment of drug interactions Many anticancer therapy agents can interact with other medications, herbal products and supplements, either prescribed or purchased over the counter. In some cases medicines may need dose adjustment or additional monitoring in order to continue treatment; others are contraindicated. Some groups of medications are more likely to interact with anticancer therapy than others, for example • Warfarin, Low molecular weight heparins e.g. Dalteparin, Aspirin, Non Steroidal AntiInflammatory, and many herbal products can affect platelet counts • Antacids, Ranitidine and Proton Pump Inhibitors e.g. Lansoprazole, Omeprazole, may affect the absorption of oral treatments. • Anti-epileptic medications, HIV medications, Claithromycin/Erythromycin, Rifampicin, Antifungals and St John’s Wort commonly affect metabolism of drugs by the liver. • Any medications with a narrow therapeutic window (i.e. small increase in dose causes big increase in toxicity) should also be considered e.g. Digoxin, Warfarin, Phenytoin, Theophylline, Lithium. This is not an exhaustive list, if the patient is taking any of these products, or you have any concerns the full drug history should be ascertained and interactions checked by pharmacy. North Trent anticancer therapy education programme V3 October 2011 Page 23 of 97 Measures to Prevent and Manage Acute Side Effects Acute side effects are those that can occur while treatment is being administered. Examples of acute side effects include: (i) (ii) (iii) (iv) (v) Cholinergic reactions associated with Irinotecan Hypersensitivity reactions associated with Taxol Fevers and chills associated with Bleomycin Central nervous system effects associated with Ifosphamide Haemorrhagic cystitis associated with Ifosphamide When administering anticancer therapy it is essential to be aware of any potential adverse reactions that can occur during administration of particular drugs. Anaphylaxis is a potential acute side effect that can occur during administration regardless of the route of administration. The signs, symptoms and management of anaphylaxis are described on page 36. Some monoclonal antibodies, including herceptin and rituximab are associated with an increased incidence of hypersensitivity reactions. Patients need to be closely monitored for signs of hypersensitivity reactions during administration of these drugs. Premedication to reduce the incidence and severity of these reactions are given before they are administered. Rituximab is given according to a protocol which outlines the rate of administration. The rate of administration varies according to the number of treatments the patient has received and the patient’s reaction to rituximab. For example, the first time a patient is given rituximab the infusion is given at a relatively slow rate. If the patient does not have a hypersensitivity reaction while this dose of rituximab is being given it can be given at a faster rate on subsequent infusions. The rate of administration for each cycle is clearly set out in the rituximab protocol which must be followed. Pre-medication is given before rituxmab to reduce any hypersensitivity reactions. The pre-medication is set out in the rituximab protocol and includes: chlorphenarimine, paracetmol and steroids Having discussed the principles that underpin the administration of all anticancer therapies, the next section identifies some of the key issues relating to particular routes. Methods of administration of Intravenous anticancer therapy Cytotoxic drugs can be administered intravenously by bolus injection or continuous infusion via peripheral cannula or central venous access device (CVAD). The potential benefits and hazards of these approaches are as follows: Bolus Injection Bolus injection allows for continual assessment of the integrity of the vein and early detection of infiltration/extravasation. However, it can increase the risk of vein irritation due to the constant contact of the drug with the vein. This can cause pain at the insertion site and lead to difficulties with distinguishing between venous spasm and extravasation. Bolus Injection via a Side Arm of a Free Flowing Infusion Bolus via a side arm assists with dilution of potentially irritant drugs and aids rapid circulation away from the insertion site. It also allows for continual assessment of vein integrity and the early detection of extravasation. This method is recommended for the administration of bolus vesicant drugs. However, small veins/cannula can lead to a slow rate of infusion and the drug can come back up the giving set. North Trent anticancer therapy education programme V3 October 2011 Page 24 of 97 Infusional administration Infusional administration allows increased dilution of the drug reducing chemical irritation at the site. However, blood return cannot be assessed frequently and the longer the infusion, the greater the possibility of needle dislodgement. Extravasation may be difficult to detect until a large volume has infiltrated so whenever possible this method should not used for vesicants (Dougherty 2008). Infusion based anticancer therapy can be given as: • Intermittent. • Continuous. • Ambulatory continuous infusion. This is given via a central line access and allows patients to receive treatment at home. The method chosen for administration will depend on a combination of factors including the drug, dose and treatment schedule/timing. A small number of anticancer therapy agents require administration via specially designed giving sets. For example taxol needs to be given through a taxol giving set which has an in line filter. Other agents may require light sensitive infusion sets. Vinka alkaloid administration Vinca alkaloid drugs include vincristine, vinblastine, vinorelbine and vindesine. All Vinca alkaloid chemotherapy is dispensed in 50 ml mini-bags. This practice aims to reduce the possibility of accidental intrathecal administration of vinca alkaloid drugs. Vinca alkaloid chemotherapy agents are vesicants (see page 27). In most cases vesicant agents are given as a bolus drug at the side arm of an infusion to enable close observation of the vein during administration. The same high levels of assessment and observation are required when administering vinca alkaloid drugs as a bagged infusion. During the infusion of vinca alkaloids the practitioner must remain with the patient observing the vein and ensuring the anticancer therapy is being administered safely. Steps must be taken to ensure the vein is patent prior to, and during, the administration of the vinca alkaloid. Prior to commencing vinca alkaloid administration an infusion of sodium chloride 0.9% should be run as a free flow infusion. During infusion the nurse will assess that the cannula/CVAD is patent and safe to use. The cannula/CVAD should not be used if any of the following signs of infiltration/ extravasation are present: • • • Pain, redness, swelling or blistering near the cannula site. Indurations, swelling or leakage from the cannula site Absence of free flow during administration of an infusion (Hadaway 2007, Saureland 2006, Dougherty 2008) If patency has been established and no problems are experienced the vinca alkaloid drug should be given as a free flow infusion at the prescribed rate (usually 5- 10 minutes). Following administration of the vinca alkaloid the line should be flushed with a sodium chloride 0.9% infusion as prescribed. The table overleaf presents the potential local effects which can occur in the vein and surrounding tissue with anticancer therapy administration. It is essential that the nurse administering intravenous treatment has a good understanding of these complications and the actions they can take if they occur. North Trent anticancer therapy education programme V3 October 2011 Page 25 of 97 Potential problems that can occur with the vein and surrounding tissues with anticancer therapy administration (Dougherty 2008, Sauerland 2006, Wells 2008). Symptom Explanation Cold sensation along the vein. Often related to the difference between the temperature of the drug and the temperature of the patient. Local allergic reaction (flare response). Red streak, blotching or hive like erythema from the insertion site along the vein caused by a venous inflammatory response. There may also be itching at the site. Symptoms usually subside within 30 minutes with or without treatment. Chemical phlebitis. Caused by the repeated administration of irritant drugs. Early signs include pain, oedema, redness and sensation of warmth. Can make it difficult to find veins future for cannulation. Discolouration of the veins. Later side effect. Mechanism unknown, usually disappears 2 – 3 months after treatment and causes no other adverse effects. Incidence highest with particular drugs eg 5 FU and Vinblastine. Vessel irritation. An irritant is an agent that can cause aching, tightness and phlebitis along the injection site or along the vein with or without an inflammatory reaction. Presenting symptoms include aching and tightness at the site and erythema or dark discoloration along vessel. Venous spasm. Sudden involuntary contraction of a vein resulting in temporary stopping of the flow of blood through the vein caused by a cold infusion or irritation by the drug being infused. Presenting symptoms include pain and cramping above the infusion site. Action: Consider the likely cause. If it could be the speed of infusion – continue at a slower administration rate. If it could be from chemical irritation – dilute the drug being given further if possible and/or run at a slower rate North Trent anticancer therapy education programme V3 October 2011 Page 26 of 97 Extravasation Extravasation is the inadvertent administration of a vesicant drug or solution from a vein into the surrounding healthy tissue (Sauerland 2006). The majority of anticancer therapy agents are capable of causing irritation and damage to the vein and surrounding tissue if they are accidentally administered outside of the vein. However, some agents are also vesicants. A vesicant is a drug that causes formation of blisters with subsequent tissue necrosis which requires treatment to limit tissue damage (Dougherty 2008). The potential consequences of extravasation with vesicant drugs include: • progressive tissue damage, • functional and sensory impairment due to damage to vital structures such as tendons, ligaments and nerves • surgical intervention such as skin grating and debridement if tissue damage is severe • psychological distress • litigation from the patient (EONS 2007, Hadaway 2007) Preventing extravasation is an essential component of the care of patients during the administration of intravenous therapy and a range of measures can be taken to minimise the potential for extravasation. These include factors relating to venous access and factors relating to the drug being administered. Extravasation Risk Factors Relating to Venous Access Cannulation Technique The skill level of the person performing cannulation is a key risk factor for the occurrence of extravasation (EONS 2007). When cannulation is problematic assistance should be sought from an experienced cannulator. It is recommended that help should be sought after two failed attempts at cannulation. Measures to aid cannulation in difficult veins and promote vasodilation may be useful eg heat pads (dependant on local policy). Cannulation Site The size and quality of blood vessels is an important factor to consider in preventing extravasation. Cancer patients often have poor venous access due to multiple episodes of venepuncture/cannulation and an increased occurrence of damaged veins from previous treatment administrations. This can make vein choice difficult (Wells 2008). Arms with occluded venous or lymphatic drainage (eg lymphoedema, SVCO) should not be used. In patients with breast cancer the arm of the unaffected side should be used for cannulation whenever possible. There is a risk of poor lymphatic and venous circulation in the arm on the affected side, particularly, if the patient has had surgery and axillary node clearance. If there are problems with venous access on the unaffected side advice should be sought from the Consultant before using the other arm. Pathological vascular conditions can also give rise to physical problems with cannulation, for example, Raynauds disease, diabetes, radiation damage. These conditions can lead to poor venous access and a decreased sensation of pain reducing the patient’s awareness of problems at the cannula site during treatment administration. Steroid therapy may suppress the inflammatory response reducing the visible signs of extravasation. North Trent anticancer therapy education programme V3 October 2011 Page 27 of 97 The degree of harm that can occur following extravasation can be influenced by the location of the cannula. Large diameter veins of the mid-forearm are preferred for drug administration as there would be less functional impairment if extravasation damage occurred. Veins over vital nerves or tendons or those at sites of flexion should be avoided due to the potential impact of damage on nerve and joint function. In particular, veins in the antecubital fossa should not be used as the large amount of subcutaneous tissue in the area can make early detection of extravasation difficult (EONS 2007). The aim of cannulation for the administration of anticancer therapy is to use the optimal vein ie a palpable vein which will adequately take the cannula being used and allow the necessary venous access for the drug being given. Vein selection should be based on this assessment. For this reason a large palpable vein on the hand may be preferable if there is poor venous access on the mid-forearm (Dougherty 2008). Other factors which need to be considered are the length of time the cannula needs to be in place and the degree of supervision which the cannula will receive during administration. Cannulation below (distal) to an earlier attempted cannulation, or venepuncture site can lead to leakage of the anticancer therapy through the previous puncture sites and should be avoided (EONS 2007). Choice of Intravenous Device Short and flexible peripheral catheters with a small gauge are recommended as they: • Are less likely to puncture the posterior wall of a small vein. • Cause less pain on insertion. • Increase the blood flow around the needle, increasing the dilution of the drug. • Reduce the risk of mechanical phlebitis. • Are less likely to lead to scar tissue formation. (Hadaway 2007, Dougherty 2008) Central venous access devices (eg Hickman/PICC lines) are preferred if cannulation is likely to be difficult or the patient is going to receive a course of irritant drugs, as there is less chance of displacement from the vein (EONS 2007). However, the chance of extravasation is NOT eliminated with central venous access devices and extravasation into the chest wall, neck and thoracic cavity can cause significant tissue damage. Causes of extravasation with a central venous access device include dislodgement of the catheter, thrombosis at the tip causing back tracking, and catheter fracture caused by “pinch off syndrome”. If the CVAD was inserted into the subclavian vein and changing the patient’s position relieves the obstruction, suspect pinch-off syndrome. Obtain a chest x ray to assess for catheter compression. Be sure to inform the radiology department about the reason for the test so they can position the patient correctly. As this complication is associated with a risk of line fracture and extravasation the CVAD should not be used if this is confirmed. The cannula or CVAD and infusion giving set must be secured appropriately to reduce the risk of dislodgement and irritation of the vein (Hadaway 2007). Administration techniques Vein patency assessment prior to, and during, administration is essential to prevent extravasation. When possible chemotherapy should be given through a newly sited cannula as the quality of venous access can deteriorate the longer a cannula remains in place. Extra care must be taken if a previously sited cannula is to be used. If there is ANY doubt as to the patency of a cannula before or during chemotherapy administration it must be re-sited (EONS 2007). North Trent anticancer therapy education programme V3 October 2011 Page 28 of 97 Steps for Assessing Patency Peripheral Intravenous Cannula • Remove any bandaging and check the dressing over the cannula is intact. • Check the cannula entry site is free from inflammation, swelling, redness, leakage. • Check patency by observing the cannula site in use. If an IV infusion is in progress observe the cannula while this is being given, otherwise flush with 0.9% Sodium Chloride. • Check that: - No resistance is felt during injection/there are no interruptions to free flow. - No leakage or swelling occurs around the cannula site. - There is good blood return. - The patient does not experience discomfort or change in sensation at the cannula site. If any problems occur consider re-siting the cannula. Hickman/PICC Lines • Check the exit site is free from inflammation, redness and/or swelling • Assess whether the line has moved: - Does the line seem longer? - Is the Dacron cuff on a Hickman line visible? - Does the patient report a difference in the length of the line? - Is the length of the PICC line different from the PICC insertion details? • Check patency by observing the CVAD in use. If an IV infusion is in progress observe the CVAD while this is being given, or flush with 0.9% Sodium Chloride. Check that: - No resistance is felt during injection/there are no interruptions to free flow. - No leakage or swelling occurs around the CVAD site. - There is good blood return. - The patient does not experience discomfort or any changes in sensation at the CVAD site, in the chest/neck/ear or arm Assess the extremity, chest and neck for signs of venous thrombosis If any of these problems are observed do not proceed with drug administration, refer to the doctor/ experienced central line practitioner. Problems may indicate that the line is incorrectly positioned, it may have become dislodged or migrated, it may be partially or completely blocked. Further investigation is required to ensure the CVAD can be used safely. This may include radiology investigations to confirm line tip location or actions to manage partial line blockage. For further information see North Trent Central Venous Access Device policy If fluid can be infused easily but blood return is absent this can indicate persistent withdrawal occlusion, commonly caused by the formation of a fibrin sheaf over the tip of the lumen. This has the potential to occlude the catheter causing leakage of fluid around the CVAD site leading to infiltration/extravasation. Patency must be ascertained before using the CVAD, particularly prior to giving vesicant or irritant drugs. Refer to the Flowchart for the Management Persistent Withdrawal Occlusion (PWO) (see North Trent CVAD policy). Implanted ports are associated with an increased risk of extravasation/infiltration than other CVAD’s. When accessing a port use a non coring needle of the proper size and length. Inspect for fluid leakage and oedema and other signs of needle dislodgement. Do not use unless you are confident the ports has been accessed correctly and is patent. North Trent anticancer therapy education programme V3 October 2011 Page 29 of 97 Extravasation Risk Factors Relating to Drugs Knowledge of the Vesicant Potential of a Drug Prior to administering anticancer therapy it is essential to know the potential damage that can be caused by the particular drug being given if extravasation should occur and the correct course of action that should be taken. Some agents bind to the DNA of surrounding tissue and can be present months after the extravasation has occurred, consequently, tissue destruction can occur over time. Following vesicant extravasation tissue damage may not occur immediately and visual inspection at the time is not enough to determine the potential for, or extent of, damage. Follow up after the event to assess damage is essential. Amount of vesicant infiltrated Continuous visual inspection of the site plays an important role in the early detection of extravasation and should be employed when a vesicant is being given. Early detection is more difficult during a continuous infusion of treatment and regular and frequent inspection of the cannula site should take place. Patient involvement Patients play a vital role in preventing and minimising extravasation. The role of the patient in alerting staff to potential problems is crucial and patients need to be informed of the signs of potential problems (eg pain, change in sensation, redness, swelling) and be encouraged to inform the staff immediately if they occur (EONS 2007). Be extra vigilant in patients with altered sensory function that can reduce awareness of problems at the cannula site, or those who cannot communicate easily. Extravasation Procedure The following describes the actions to be taken following extravasation of cytotoxic chemotherapy. Not all chemotherapy is vesicant (i.e. can cause severe tissue damage when given into the surrounding tissue) but most chemotherapy potentially causes irritation and injury to the tissue and should be treated according to the following procedure. If tissue damage is suspected then treatment must be initiated quickly. Objectives Each practitioner will be able to: 1. Recognise the potential danger of extravasation injuries associated with specific drugs/solutions which they administer 2. Prevent the complication occurring 3. Recognise the early stages of extravasation 4. Initiate appropriate treatment Recognition of extravasation from a peripheral cannula Extravasation should be suspected if any of the following signs are present: • Pain, redness, swelling or blistering near the cannula site. This should be distinguishable from a feeling of cold which may occur during the administration of some drugs/solutions • Induration (the hardening of a usually soft area of skin), swelling or leakage from the cannula site • Absence of blood return • Resistance on the plunger of the syringe during bolus administration • Absence of free flow during administration of an infusion Note: One or more of the above may be present. If extravasation is suspected or confirmed action must be taken immediately (Hadaway 2007, Dougherty 2008) North Trent anticancer therapy education programme V3 October 2011 Page 30 of 97 Early firm induration with or without tenderness has been shown to be a reliable sign of eventual ulceration • When the full thickness of the skin is damaged the surface may appear very white and cold with no capillary filling and later may develop a dry, black eschar • Ulceration is not usually evident until one or two weeks after the injury when the eschar sloughs to reveal the underlying cavity, ulcers have a typical necrotic yellowish fibrotic base with a surrounding rim of persistent erythema (National Extravasation Information Service 2005) It is important to distinguish extravasation from a flare reaction or venous spasm. A flare reaction is a local allergic reaction in the vein to the drug being given. The reaction looks like a nettle rash, and is accompanied by streaking erythema or hives along the affected vein. It is not usually painful and is not usually associated with swelling or loss of blood return. The reaction typically tends to subside after 30-60 minutes (Wickman 2006). If the flare reaction is mild you can continue administration at a slower rate and with increased dilution. If more severe stop administration until the reaction subsides, then continue at a slow rate. Venous spasm is caused when the vein is irritated by an intravenous infusion. This is usually due to the irritant nature of the drug being administered, the cold temperature of the infusion fluid or too rapid administration of an infusion or bolus injection. Symptoms of venous spasm include cramp type pain and/or slowing or stopping of the infusion. As discomfort at the cannulation site or a burning/stinging pain are one of the first symptoms of extravasation all changes in sensation must be investigated to exclude the possibility that an extravasation has occurred (Dougherty 2008). If venous spasm has occurred it can be managed by slowing the infusion rate or diluting the drug further. Recognition of an extravasation from a Central venous access device Although extravasation is less likely to occur with a central venous access device than with a peripheral cannula, it is still possible. To minimise the risk of extravasation, the line should be checked for patency prior to use. If blood return is absent follow the Algorithm for Persistent Withdrawal Occlusion (See North Trent Central Venous Access Device policy). If there is any doubt about line patency seek the advice of a senior member of medical staff Extravasation from CVAD’s tend to be more severe than from a cannula, as it is often more difficult to detect and a greater amount of the drug may have extravasated before the patient or nurse is aware of the problem. Signs of central catheter infiltration/extravasation: • Aching/discomfort in the shoulder and neck - this symptom is the most common and should not be overlooked • Pain or burning of chest wall • Leakage from catheter exit site • Swelling of chest wall • Aching/discomfort in the chest wall • Fluid leakage at or around exit site and along subcutaneous canal. Early detection and prompt appropriate action is required to prevent possible • Skin necrosis • Scarring around the tendons, nerves and joints • Secondary infection and abscess formation • Contracture of affected limbs • Amputation. North Trent anticancer therapy education programme V3 October 2011 Page 31 of 97 Managing a suspected extravasation from a CVAD is dependant on clinical assessment of the symptoms, site of extravasation and the type and volume of drug involved. An individual risk assessment must be carried out and should include a senior member of the medical team and an experienced nurse practitioner. If extravasation is suspected the CVAD must not be used until patency has been verified. ACTION TO BE TAKEN IF AN EXTRAVASATION OCCURS VIA A PERIPHERAL CANNULA 1 On suspecting extravasation stop the injection/ infusion immediately. 2 Assess the extent of the extravasation, the drug involved and any help needed. 3 Leave the cannula in place. 4 Explain to the patient what you suspect may have happened and the procedure for dealing with it. 5 Aspirate any residual drug and blood through the cannula to remove as much of the drug from the site as possible and minimise tissue damage. Protective goggles must be worn at this stage. 6 Remove the cannula. Mark round the extravasated area with a pen to provide a baseline for monitoring the extent of the extravasation. Cover area with sterile gauze 7 Inform doctor if drug involved is group B or C or there are concerns about a group A drug extravasation. 8 Follow the treatment of extravasation guidelines according to the chemotherapy grouping pathway. Treatment using an antidote must be prescribed by a doctor prior to administration unless there is a nurse present who has completed a competency in administering the specific antidote required under a patient group direction. If the drug is not covered by the guidelines contact pharmacy for advice. 9 If group B or C or large volume A consider need for referral to the plastic surgery team 10 Provide analgesia as required. Consider use of antihistamine if appropriate. 11 Measure the affected area and document in the patient record. Arrange photographs with the medical photographer if available if there are any visible signs of an extravasation. 12 Complete the North Trent extravasation reporting form. Complete local incident reporting form. Ensure copies are sent to the appropriate personnel according to local policy. 13 Complete the Green National Extravasation Reporting Card and submit to Birmingham. http://www.extravasation.org.uk/greencard 14 Observe the site regularly for erythema, indurations, blistering or necrosis. For inpatients monitor the site at least daily and document progress/changes in the nursing record. 15 When the patient is discharged home ensure appropriate follow up arrangements are in place. Provide drug guideline specific written information on the ongoing care of the affected area. Ask the patient/ carer to observe the site at least daily and contact the hospital if they notice an increase in discomfort, blistering or peeling of the skin. North Trent anticancer therapy education programme V3 October 2011 Page 32 of 97 16 Patients with extravasations from Group A drugs should be asked to contact the ward/department where they were treated if they have any concerns. If factors suggest that extravasation is more likely to be problematic with a patient in this group (e.g. large volume of chemotherapy extravasated) arrange for the patient to be contacted by the ward/dept. where they received treatment within 48 hours after discharge. 17 Patients with extravasations from Group B or C drugs should be asked to return for assessment of the effected area within 48 hours following discharge. Follow up care should be documented on the North Trent extravasation follow up form After 48 hour further follow-up will be based on the individual assessment. Some patients may need to be recalled for further review and discussion with the consultant regarding referral to other health care professionals. Where appropriate liaise with tissue viability nurse and/or plastic surgeons if indicated. If there is visible tissue damage, take a photograph of the affected area, and file in the patients medical notes. Referral to plastic surgeons following group B, C or large volume A extravasation must be considered. This is particularly the case if any of the following criteria are present. • • • • • • Pain or changes in sensation that continue to be present once the immediate extravasation incident has passed Lesion greater than 2 centimetres Functional changes Blistering Induration (the hardening of a usually soft area of skin) Affected area appears white and/or cold with reduced capillary filling (absence of blanching) However, referral must be considered if there are concerns about the extent or consequences of any extravasation incident. North Trent anticancer therapy education programme V3 October 2011 Page 33 of 97 ACTION TO BE TAKEN IF AN EXTRAVASATION OCCURS VIA A CVAD 1 On suspecting extravasation stop the injection/ infusion immediately and investigate further. An individual risk assessment must be carried out and should include a senior member of the medical team and an experienced nurse practitioner. 2 On confirmation of extravasation assess the extent of the extravasation, the drug involved, the volume, the site and any help needed. 3 Leave the CVAD in place at this point. 4 Explain to the patient what you suspect may have happened and the procedure for dealing with it. 6 If extravasation is confirmed aspirate any residual drug and blood through the CVAD to remove as much of the drug from the site as possible and minimise tissue damage. Protective goggles must be worn at this stage. Follow the treatment of extravasation guidelines according to the chemotherapy grouping pathway. Treatment using an antidote must be prescribed by a doctor prior to administration. If the drug is not covered by the guidelines contact pharmacy for advice. 7 Provide analgesia as required. Consider use of antihistamine if appropriate. 8 Measure the affected area and document in medical notes (doctor), and nursing record (nurse). Arrange photographs if there are any visible signs of an extravasation. 9 Discuss and organise plans for line removal. If Hickman line or port consider seeking advice from plastic surgeons regarding removal to minimise tissue damage. All CVADS: A referral to the plastic surgeons should be considered at the earliest opportunity. 10 Complete the North Trent CVAD extravasation reporting form. Complete incident reporting form. Ensure copies are sent to the appropriate personnel according to local policy. 11 Complete the Green National Extravasation Reporting Card and submit to Birmingham. 12 Observe the site regularly for erythema, indurations, blistering or necrosis. For inpatients monitor the site at least daily and document progress/changes in the nursing record. 13 When the patient is discharged home ensure appropriate follow up arrangements are in place. Provide the patient with information on the ongoing care of the affected area. Ask the patient/ carer to observe the site at least daily and contact the hospital if they notice an increase in discomfort, blistering or peeling of the skin. 14 All Patients with CVAD extravasations should be asked to return for assessment of the effected area within 48 hours following discharge After 48 hour further follow-up will be based on the individual assessment. Some patients may need to be recalled for further review and discussion with the consultant regarding referral to other health care professionals. Where appropriate liaise with tissue viability nurse and/or plastic surgeons if indicated. If there is visible tissue damage, take a photograph of the affected area, and file in the patients medical notes. North Trent anticancer therapy education programme V3 October 2011 Page 34 of 97 Documentation of extravasation Extravasation events must be thoroughly documented and reported. Clear record keeping will facilitate the patient’s ongoing care. It may also be required in the case of litigation (Dougherty 2008). The purpose of documentation following extravasation is to: • • • • Provide an accurate account of what happened and the action that was taken Protect the healthcare professionals involved (showing they followed correct procedures) Gather information on extravasations, how and when they occurred – for audit purposes Highlight any possible deficits in practice which require review (EONS 2007) Intramuscular/Subcutaneous Administration of anticancer therapy Only a few anticancer therapy drugs can be administered via this route as many are too irritant, can cause tissue damage and/or they cannot be absorbed by this route (Dougherty and Lister 2008). Prior to intramuscular administration it is important to check the patient’s platelet count. The count should be above 50 to reduce the risk of excessive bleeding at the injection site. The principles of safe practice used for the administration of intravenous anticancer therapy must be applied when administering intramuscular/subcutaneous agents. For example, protective equipment should be used and waste must be disposed of as cytotoxic waste. Oral anticancer therapy One of the misconceptions about oral anticancer therapy is that it has less potential side effects than treatment given by other routes in particular the intravenous route. However, it is important to note that some oral anticancer therapy drugs have potentially severe and distressing side effects. Some oral anticancer therapy drugs have a coating which protects the drug and/or prevents it from coming into contact with the patients oral mucosa. It is important to asses the patients ability to swallow the tablet/capsule whole before they take oral anticancer therapy. If they are unable to do so liaise with the doctors and pharmacy about appropriate alternatives/action. Each oral anticancer therapy will have its own instructions for dose and timing of administration. Some agents need to be taken at particular times in relation to food (e.g. pre or post meals). Others cannot be taken within a certain time of other medication – for example, capecitabine must not be taken within 2 hours of antacids. It is important to confirm that the patient understands this information when they are given their tablets to take home. Oral anticancer therapy is often taken by the patient at home. Patient information is an essential aspect of care as it is vital that the patient understands the importance of adhering to the administration schedule prescribed. North Trent anticancer therapy education programme V3 October 2011 Page 35 of 97 It is essential to ensure that the patient understands the following: how to take the tablets (dose, time, frequency, duration of course) the medicine has been prescribed for them and should not be given to anyone else the medicine should be stored in a safe place – particularly out of the reach of children what to do if they miss a dose – i.e. they should not try to catch up but should miss that dose and take the next dose as prescribed the side effects of treatment and what to do if they experience them how to obtain further supplies to return any unused tablets to the hospital pharmacy (Dougherty and Lister 2008) It is vital that patients on oral anticancer therapy are aware that if they develop side effects they must contact the treatment centre for advice before they take their next dose. They must be informed that they should not continue their course of treatment until they have spoken to a member of the oncology team. Issues to be considered with administering oral anticancer therapy include: (i) Always wear gloves when handling oral anticancer therapy and use minimal handling techniques. (ii) Never crush tablets or open capsules as there is a risk of powder being released that could be inhaled. Liaise with the doctors/pharmacy if the patient is unable to take a tablet or the dose prescribed cannot be given by the tablets dispensed. (iii) Assess that the patient is able to swallow the medication whole before you give it to them and ensure they know they should not chew of crush the tablet/capsule. (iv) Wash hands after administering tablets. (v) Ensure the patient takes the tablet when you give it to them, do not leave it for them to take “later”. Administering oral anticancer therapy in the inpatient care setting A recent National Patient Safety Alert identified specific risks associated with patients being admitted to hospital who are currently on a course of oral anticancer therapy (NPSA 2008). These relate to decision making around the continuation of treatment and potential errors in prescription and administration. Decisions around continuation of oral anticancer therapy On admission to hospital patients may be experiencing side effects of their oral anticancer therapy which requires a cessation of treatment or dose reduction. A decision must be made by a senior oncology doctor (SpR or above) as to whether the patient should continue their course of treatment prior to it being prescribed and administered. To ensure this the doctor prescribing the medication must consult with a senior medical member of the oncology medical team prior to it being prescribed. The nurse administering oral anticancer therapy must ensure that the decision to continue with treatment has been agreed by a senior oncology doctor. Correct prescribing of oral anticancer therapy It is essential that the patient receives the correct dose and schedule of oral anticancer therapy. This information is contained on the chemocare prescription which may not be available when the patient is admitted. Prior to prescribing the oral anticancer therapy a copy of the chemocare prescription should be obtained. A copy of the prescription can be obtained from pharmacy dispensary or it can be printed from chemocare. When oral anticancer therapy is prescribed on the inpatient drug chart, the nurse must also check the drug against the chemocare prescription before administration. North Trent anticancer therapy education programme V3 October 2011 Page 36 of 97 MODULE 4 SIDE EFFECTS OF ANTICANCER THERAPY Potential Systemic Side Effects The incidence and severity of the side effects of anticancer therapy are related to the specific drugs used and the dose being given. This section is a description of some of the more common side effects, which can occur as a result of anticancer therapy. It is important to note that patient information and advice on the side effects of treatment must relate to the specific regimen the patient is receiving. Side effects can be classified as immediate, short and long term. However, some side effects do not fit neatly within this time frame – for example bone marrow depression can occur before 7 days post treatment administration. Similarly, fatigue can occur within days of treatment administration, but can continue for many weeks or months. Onset Time Side Effect Immediate Occurs within thirty minutes of administration. Venous pain Facial/body flushing Cardiac Arrhythmias Hypotension Hypersensitivity reactions Anaphylaxis Haemorrhagic cystitis Abnormal tastes and smells Short to medium term Occurs within hours and up to seven days of administration. Discoloration of urine Tumour lysis syndrome Nausea and vomiting Stomatitis/mucositis Tumour pain CNS toxicity Anorexia Fatigue Constipation Diarrhoea Taste aberration Medium to Long Term. Occurs later than seven days and may be cumulative in nature. Bone Marrow depression Alopecia Hand foot syndrome Dermatitis Liver dysfunction Renal toxicity Cardiac toxicity Peripheral neuropathy Pulmonary fibrosis Changes in fertility North Trent anticancer therapy education programme V3 October 2011 Page 37 of 97 Anaphylaxis Anaphylaxis is a severe, life-threatening, generalised or systemic hypersensitivity reaction. It is characterised by rapidly developing life-threatening airway and/or breathing and/or circulation problems usually associated with skin and mucosal changes (Resuscitation council 2008). Anaphylaxis is a medical emergency - death can occur within seconds. Anaphylactic reactions can be biphasic in up to 5 % of cases and the reaction may reoccur between 1 and 72 hours later. Identifying factors that can lead to an increased risk of occurrence of anaphylaxis is essential before giving anticancer therapy to a patient. Some patients are at increased risk of anaphylaxis and it is good practice to assess the patient’s history of allergies and discuss any increased risk factors with the medical team prior to administering treatment. Increased risk factors include patients: With a history of asthma, eczema or allergies Who have had previous reactions to drugs Who have reacted to the drug currently being given on a previous occasion. Some anticancer therapy agents are also associated with increased incidence of anaphylactic or hypersensitivity reaction. These include: monoclonal antibodies, carboplatin, cisplatin, L-asparaginase and taxanes (Souhami and Tobias 2005). Local procedures should be in place for early detection and prompt treatment when giving any drugs associated with an increased risk of hypersensitivity reaction. Signs and Symptoms of Anaphylaxis • Itching or strange metallic taste in the mouth. • Rash or urticara (hives) anywhere on the body • Facial and generalised flushing • General feelings of agitation, irritability, a sense of being unwell but the patient finds it difficult to be specific, light headedness/weakness. • Swelling of tongue, lips or throat • Hoarse voice, stridor • Hypotension • Tachycardia • Difficulty in breathing, wheeze • Abdominal cramps, nausea • Respiratory collapse/unconsciousness (Resuscitation Council UK 2008) Treatment Should any of the above symptoms develop you should: (i) (ii) (iii) (iv) (v) (i) (ii) (iii) Stop administration of drug. Assess patient for airway, breathing and circulation. Put out an urgent call for emergency medical help. Elevate patients legs, start oxygen 10-15/litres/min. If signs of shock, stridor, wheeze or respiratory distress, give Epinephrine (Adrenaline) 0.5ml of 1 in 1,000 (1mg/1ml) IM as prescribed. Change IV giving set and give 0.9% saline quickly (500ml/5minutes) as prescribed. Do not give colloids in anaphylaxis. Check vital signs. Repeat Epinephrine after 5 minutes if no improvement. Patients may also be given Piriton 10mg and Hydrocortisone 200mg IV, IV fluids and nebulisers eg Salbutamol as prescribed. (Resuscitation Council UK 2008) North Trent anticancer therapy education programme V3 October 2011 Page 38 of 97 Nausea and Vomiting There are three types of nausea and vomiting associated with anticancer therapy: Acute: Starts within minutes to hours of treatment administration and resolves within 24 hours Delayed: Occurs 16 to 24 hours post treatment and persists for hours to days Anticipatory: A conditioned response in which the patient experiences nausea and/or vomiting in anticipation of receiving their treatment. This often occurs when acute/delayed nausea and vomiting were not well managed at previous administrations Nausea and vomiting in relation to anticancer therapy is referred to as chemotherapy induced nausea and vomiting (CINV). It is drug type and dose related and is thought to involve the actions of the vomiting centre and the chemoreceptor trigger zone in the brain and the neuro-transmitters dopamine, serotonin and substance P (Tadman and Roberts 2007). Anti-emetics used in the prevention and treatment of CINV work by blocking the action of the neurotransmitters. They include serotonin (5HT3) antagonists such as Granisetron and Ondansetron and dopamine antagonists such as Domperidone. Aprepitant is a relatively new anti-emetic which works by blocking the receptors in the vomiting centre (neurokinin 1 receptors) that are activated by substance P. The steroid Dexamethasone is also widely used in the prevention and treatment of chemotherapy induced nausea (Miller 2004). Each of these antiemetics works in a different way and can be used in combinations to prevent or treat CINV. While different patients react differently to their anticancer therapy there are some risk factors which increase the potential for nausea and vomiting. These include: • Younger age (less than 50) • Female gender • No/minimal history of alcohol use • Prior CINV • History of travel sickness • Anxiety The ematogenic potential of specific agents has been identified and anti-emetic protocols have been established based on the degree of nausea and vomiting likely to occur with each drug. The table below provides examples of the ematogenic potential of a range of different agents. For drugs which are likely to result in moderate to severe nausea and/or vomiting prophylactic anti-emetics are prescribed. For example, patients receiving Cisplatin are given IV Dexamethasone and Granisetron prior to receiving their chemotherapy and regular oral Dexamethasone for the following three days. Aprepitant can also be given when there is an increased potential for CINV. When it is used in combination with standard anti-emetic therapy it provides benefit in the acute phase and also the delayed phase of CINV. North Trent anticancer therapy education programme V3 October 2011 Page 39 of 97 Examples of the ematogenic potential of different drugs HIGH RISK (>90%) Actinomycin D Carmustine Cisplatin High dose Cyclophosphamide Ifosfamide Cytarabine Dacarbazine MODERATE RISK (30-90%) Carboplatin Daunorubicin Doxorubicin (Adriamycin) Epirubicin Idurabicin Ifosphamide Melphalan Oxaliplatin Vonorelbine LOW RISK (10- 30 %) 5flourouracil Aspariginase Cytarabine Docetaxel Etoposide Fludarabine Gemcitabine Paclitaxel Pemetrexed The HCP has an essential role to play in managing nausea and vomiting. This includes: • preventing or minimising symptom occurrence and severity by ensuring the patient receives appropriate anti-emetics • assessing the effectiveness of the anti-emetics taken and ensuring they are reviewed if nausea and vomiting are not controlled • evaluating the physical, social and psychological impact that the symptom is having on the patient Patients may not always report the extent of their CINV as they may feel it is part of the treatment they have to put up with. They may also be concerned about appearing weak or their treatment being stopped. It is essential to tell patients before their treatment commences that CINV can be controlled. When the patient returns for the next treatment ask them about their symptom severity. If they did experience CINV check that their antiemetic regimen has been reviewed and reassure them that alternative anti-emetic options are available and CINV can be controlled for most patients. The assessment of nausea and vomiting should include the use of the common toxicity grading scores below (Vidal 2011). The aim of symptom control should be to achieve grade 1 or lower. Symptom Grade 1 Grade 2 Grade 3 Grade 4 Nausea Able to eat reasonable intake Intake significantly decreased but can eat No Significant intake ------- 1 episode in 24 hours 2-5 episodes in 24 hours 6-10 episodes in 24 hours Vomiting More than 10 episodes in 24 hours or parenteral or enteral support Patients on oral chemotherapy with nausea and vomiting of grade 3 or 4 or grade 2 for more than 24 hours should be advised NOT to continue their oral anticancer therapy treatment until they have been assessed by a senior oncology doctor. North Trent anticancer therapy education programme V3 October 2011 Page 40 of 97 Bone Marrow Depression Bone marrow depression is a temporary cessation of the bone marrow’s ability to produce blood cells. This can lead to neutropaenia, thrombocytopenia and anaemia. Neutropaenia Neutropaenia is the term used to describe an abnormally low number of circulating neutrophils (Grundy 2000, Wardley 2000). The neutrophil being the most important white blood cell needed to combat infection (Wardley 2000). Neutropenia is said to occur when the circulating netrophil count is less than 1 (Grundy 2000). Neutropaenia is the most common dose limiting toxicity associated with anticancer therapy. The nadir, the lowest point of the drop of the white cell count, commonly occurs 7-14 days after treatment administration. However, it can occur earlier or later than this in the treatment cycle and should always be considered if a patient presents with symptoms of infection. The white cell count usually improves by three to four weeks after administration, enabling further treatment to be given. All regimens can potentially cause neutropaenia. However, a number of risk factors are associated with a higher incidence. These include: the type and dose of the drug being given, previous history of neutropaenia with similar drugs, concurrent radiotherapy to sites containing bone marrow, older age, poor performance status, poor nutritional status and co-morbid conditions e.g. COPD, diabetes, cardiovascular disease, liver disease (Nirenberg 2006a). Patients with neutropaenia have an increased susceptibility to infection and a reduced ability to fight it (Coughlan 2008). Complications of neutropaenia include hospitalisation and reduced treatment efficacy due to delays in treatment and/or dose reductions as treatment is not usually given while the white cell count is low. The most significant potential consequence of neutropaenia is death due to infection and sepsis (NCEPOD 2008, Nirenberg 2006a). Patients must be made aware that their ability to fight infection can be compromised if they develop a low white cell count. They must be advised to contact the cancer centre if they develop an elevated temperature (37.5oc or above) or any signs of infection to arrange for admission for a full blood count test and assessment. In order to reduce the risk of infection patients should be advised to avoid sources of infection such as people with colds, sore throats, measles etc and people recently vaccinated with live vaccines such as MMR and DPT (diphtheria, pertussis, tetanus). Patients should be advised to avoid dental treatment while they are receiving chemotherapy due to the risk of introducing infection during dental procedures. If this treatment is necessary the blood count must be checked before it is carried out. The nursing care plan for a patient with a low white cell count should include: • Vigilant observation of temperature, pulse, blood pressure, respiratory rate, oxygen saturations and level of consciousness. • Careful hand washing by the patient and healthcare staff. This must be stressed to the patient as well as the hospital staff providing care. (Nirenberg 2006b). • Maintaining personal and oral hygiene; regular oral assessment and mouth care is essential due to the risk of opportunistic infections such as candida (Coughlan 2008). • Careful monitoring and aseptic handling of “at risk” sites such as cannula/central venous access devices. • Preventing trauma to the skin and mucous membrane eg avoiding the use of enemas and suppositories. • Avoiding actions such as catheterisation, which can potentially introduce infection. North Trent anticancer therapy education programme V3 October 2011 Page 41 of 97 Neutropenic Sepsis Patients with a low neutrophil count (below 1.0 x 109/l) are at risk of developing neutropenic sepsis. In patients with a reduced neutrophil cell count the onset of severe sepsis may be rapid and severe. It is important to note that the usual signs of infection may be absent as the immune response is inhibited, in many cases the first and only sign of infection may be a raised temperature (Coughlan 2008). In severe sepsis or septic shock the temperature may be low. The surviving sepsis campaign set out internationally agreed definitions and protocols for the detection and management of sepsis which provide a firm foundation for caring for patients with neutropaenic sepsis (Dellinger 2008). Definitions of sepsis and septic shock Sepsis Known or suspected infection with 2 or more of the following symptoms Temp above 38 or below 36 Pulse more than 90 Respiration rate more than 20 White cell count below 4 x 109/l or above 12 x 109/l o NB for neutropaenic patients the count would be below 1 x 109/l Severe sepsis Symptoms of sepsis PLUS organ dysfunction, low blood pressure or poor perfusion Indications of organ dysfunction: Systolic BP less than 90 (or mean BP less than 65) Altered mental state O2 saturation levels less than 95% Urine output less than 0.5 ml/kg/hr Serum lactate above 2 mmols INR above 1.5, APPT above 60 seconds Platelets less than 100 (however, this may be associated with treatment or underlying disease in chemotherapy patients) Septic shock Severe sepsis PLUS hypotension which does not respond adequately to fluid resuscitation (i.e. the rapid administration of IV fluids) Other signs: decreased capillary refill, skin mottling, positive fluid balance, metabolic acidosis (blood pH less than 7.35, bicarbonate less than 20 mmol) NB It is important to note that patients with neutropaenic sepsis can be critically ill with minimal symptoms as the clinical signs of septic shock can be subtle. They may NOT have pyrexia. Observe for pallor, mottled skin, tachycardia, altered mental state, anxiety, increased respiration rate and hypotension. North Trent anticancer therapy education programme V3 October 2011 Page 42 of 97 Key factors in the treatment of neutropaenic sepsis Bloods tests to include: o Full blood count, o blood cultures – if the patient has a CVAD both peripheral and CVAD cultures should be obtained o urea and electrolytes, lactate, glucose, liver function tests and clotting screen as appropriate Administration of intravenous antibiotics as soon as possible. The type of antibiotic is identified in the neutropaenic sepsis antibiotic protocol. o if the patient shows signs of severe sepsis or septic shock antibiotics should be given before the neutrophil count has returned • Vigilant monitoring of observations and patient’s condition using the hospital’s Early Warning Score system • Support through the physiological crisis o Oxygen to achieve saturation levels above 95% o IV fluids If BP below 90 (or 40 below the normal BP for the individual patient) intravenous fluid challenge should be given as prescribed Monitor urine output Risk assess with senior medical staff the need for urinary catheterisation balancing the need for accurate monitoring of urine output against the risk of infection. This decision should be made by a senior registrar or consultant Evaluate potential source of infection – Take specimens as indicated e.g. sputum, throat swab, urine, stool Regular medical review the efficacy of treatment must be reviewed by the medical team on a regular basis - at least daily o the nurse must notify the doctor promptly if they identify any deterioration in the patients condition, or if they have any concerns about the patients progress. If required the local escalation policy should be used appropriately Referral to the critical care medical team for advice and/or transfer should be considered at the earliest opportunity if the patient develops signs of severe sepsis, particularly if there has been no response to the fluid challenge or the serum lactate is elevated. North Trent anticancer therapy education programme V3 October 2011 Page 43 of 97 Thrombocytopaenia Reduction in platelet count leading to increased risk of bleeding. The normal count in men and women is 150 – 400 x109/l, (Tadman and Roberts 2007). The drop in platelet count may occur 7 – 10 days after treatment depending on drug dose. The count at which it is considered acceptable to give treatment may vary across specialities and the cancer network. Patient education is essential so the patient is aware of the need to report early any signs of a reduced platelet count e.g. bleeding gums, increased bruising, hypermenorrhea, tarry stools, blood in urine, coffee ground vomit. Patients should be advised to avoid activity that could cause injury and avoid dental treatment while they are receiving anticancer therapy. If this treatment is necessary they need to inform the dentist so checks of the blood count can be made. Advise the patient to shave using an electric shaver and to use a soft tooth brush when carrying out oral hygiene. They should also avoid drugs that interfere with platelet function eg aspirin and alcohol. If they are taking aspirin, as a prescribed drug, this should be discussed with the doctor. The patient is at greatly increased risk of bleeding with a count below 20 x109/l. When platelet counts becomes significantly depleted a platelet transfusion may be required to prevent or stop bleeding (refer to local guidelines). Anaemia Anaemia is the reduction in the red blood cell count below 13.5 (male) or 11.5 (female), (Hoffbrand & Pettit 1993). Symptoms include tiredness, breathlessness, pallor, weakness, impaired concentration and cognitive function (Foubert 2006). If the anaemia is problematic the patient may require a blood transfusion. Patients receiving adjuvant curative radiotherapy with anticancer therapy are likely to require blood transfusions if anaemic as the effectiveness of radiotherapy can be influenced by the presence of oxygen in the cells being treated. North Trent anticancer therapy education programme V3 October 2011 Page 44 of 97 Other side effects Alopecia Alopecia is one of the most distressing and visibly noticeable effects of anticancer therapy. It can challenge self esteem, threaten body image, act as a constant visible reminder of their diagnosis and lead to difficulty socialising, a feeling of being unattractive and relationship difficulties (Power 2008, Roe 2011). The incidence and severity of alopecia is dependant on the drug and the dose in the treatment regimen, examples are contained in the table below. Hair loss is often quantified between thinning and complete baldness, the term alopecia is used to define hair loss over 20% (Roe 2011). Hair loss is not confined to the head and can also include eyelashes, eyebrows, arms, legs, underarms and pubic areas. Examples of Drugs that always cause Alopecia Daunorubicin Doxorubicin Hydrochloride Ifosfamide Paclitaxel Epirubicin Docetaxel Etoposide Before they commence treatment with a drug that can cause hair loss the patient must be informed of the potential for hair loss and offered a wig referral. Hair loss often occurs 10 to 21 days after treatment and may occur suddenly and in large amounts. For this reason some patients prefer to have their hair cut in a shorter style before it begins to fall out. Hair loss is temporary and the hair will re-grow gradually after the course of treatment is completed. Patients should be: • • • • Informed of the possibility in alteration of colour and texture of the hair when it does re-grow. Advised on skin care (protecting the head from sunlight by using a high factor sun cream) and increased sensitivity to hot and cold temperatures Advised on hair care: for example, using a soft bristle brush, avoiding perms and colorants Informed about other local services that can provide support such as scarf and headware services With some regimens scalp cooling may be effective in preventing hair loss. A specially designed cooling cap is fitted tightly over the patient’s head to ensure maximum contact with the scalp aided also by applying an overcap. Scalp cooling is used to reduce scalp temperature causing constriction of blood vessels and thus decreasing the amount of drug that can pass into hair follicles. It also slows the metabolism rate activity in the follicles so the cells divide less rapidly and are less vulnerable to the action of chemotherapy. With scalp cooling there is a potential that the treatment will not reach all cancer cells that may be in the scalp so it is not appropriate for all patients (Roe 2011). The procedure used for scalp cooling is dependent on a variety of factors such as the dosage, plasma half life of the drugs being used and the patient’s ability to tolerate it. The details for scalp cooling procedures are set out in North Trent protocols. North Trent anticancer therapy education programme V3 October 2011 Page 45 of 97 Altered Bowel Habits Anticancer therapy can cause constipation or diarrhoea dependant on the drug given. Diarrhoea: Many anticancer therapy drugs cause mild to moderate diarrhoea. Diarrhoea can be a life-threatening complication of treatment. Consequences of prolonged or severe diarrhoea include dehydration, electrolyte disturbance, renal failure and hypovolaemic shock. Anticancer therapy induced diarrhoea can increase the patients susceptibility to infection, and can predispose neutropenic patients to develop neutopenic sepsis (Benson et al 2004, Cherny 2008). Assessment The treatment of anticancer therapy related diarrhoea should be based on an assessment of the individual patient alongside the grade and duration of diarrhoea. Other potential causes of diarrhoea must be considered, these include: infection, medication, constipation/ faecal impaction and bowel obstruction. The possibility of an infective cause or involvement, including Clostridium difficile (C.diff), must always be considered in any patient presenting with diarrhoea. An urgent stool sample must be sent as soon as possible for all patients admitted with diarrhoea. • Where diarrhoea is more likely to be treatment related appropriate anti-diarrhoeal medication should be commenced prior to obtaining the stool culture result. • If it is not an expected side effect or the patients anticancer therapy, or there are other signs of infection then anti-motility agents such as Loperamide and Codeine should not be used due to their direct action of slowing down the passage of stool through the bowel, prolonging mucosal exposure to the toxins. Consultation with microbiology is essential with these patients. Assessment criteria Assessment should include: • History of onset and duration of diarrhoea • Number of stools and stool composition (i.e. formed, liquid, presence of blood) • Consider other causes e.g. risk of sepsis, bowel obstruction, faecal impaction • Assessment of patient condition e.g. dehydration, electrolyte disturbance, pain • Medication profile • Dietary profile (to identify diarrhoeal-enhancing foods) • Send stool specimen The severity and grade of diarrhoea should be determined for all patients using the National Toxicity Criteria as shown in the table below. Interventions should be based on the assessment of the patient and the toxicity criteria and must follow the management of chemotherapy related diarrhoea guidelines. High risk symptoms include: temperature, sepsis, neutropenia, electrolyte disturbance, nausea and vomiting above grade 2, abdominal pain/cramping, frank blood in stools, dehydration, haemodynamic instability, diminished performance status. Patients with grade 3 or 4 diarrhoea (or grade 2 for more than 48 hours) are at risk of dehydration and will need admitting for symptom management, IV fluids and monitoring electrolytes. Their nursing care plan must include regular EWS observations (minimum 4 hourly or more frequent as indicated by condition) and fluid balance monitoring. . North Trent anticancer therapy education programme V3 October 2011 Page 46 of 97 Toxicity Criteria for Treatment Related Diarrhoea (adapted from National Cancer Institute guidelines) Grade 1 Grade 2 Grade 3 Grade 4 Patients without colostomy Increase of less than 4 stools a day compared with pre treatment Increase of 4 – 6 stools a day or nocturnal stools Increase of 7 or more stools a day or incontinence, or symptoms of dehydration, abdominal cramping Over 10 episodes a day or bloody diarrhoea or symptoms of dehydration or haemodynamic instability Patients with a colostomy Mild increase in loose watery colostomy output compared with pre treatment Moderate increase in loose watery colostomy output but not interfering with normal activity Severe increase in loose, watery colostomy output interfering with normal activity, abdominal cramping Severe increase in loose, watery colostomy output and/or symptoms of dehydration or haemodynamic instability Dietary advice for patients with anticancer therapy induced diarrhoea • Encourage fluid intake, aiming for an oral intake of 3L (approximately 8-12 cups) of clear non-carbonated fluids per day. Patients unable to tolerate oral fluids, should be admitted for parenteral rehydration. • Avoid alcohol and drinks with caffeine. • Eat 5 or 6 small meals rather than 3 large meals a day. • Reducing intake of high fibre foods e.g. wholemeal bread, high fibre breakfast cereals (such as All Bran, Bran Flakes, Weetabix) can be helpful for some people. • Spicy or rich foods can make symptoms of diarrhoea worse in some people. Diarrhoea relating to Irinotecan chemotherapy Irinotecan is associated with 2 potential causes of diarrhoea. The first is a cholinergic reaction which can occur during the administration of the drug or within the first 24 hours. Symptoms include acute abdominal cramps and severe diarrhoea. Prophylactic S/C Atropine is given immediately before administration and can be given again if the cholinergic symptoms occur. Diarrhoea occurring 24 hours after the administration of Irinotecan (referred to as delayed diarrhoea) is unlikely to be a cholinergic reaction. This diarrhoea can be severe and requires prompt treatment with the “Irinotecan Loperamide regimen” (see intranet). If the diarrhoea continues to be severe the patient will need admitting to hospital for fluid support to prevent dehydration. Patients on oral chemotherapy with diarrhoea grade 3 or 4 or grade 2 for more than 24 hours should be advised NOT to continue their oral anticancer therapy treatment until they have been assessed by a senior oncology doctor. Constipation: Due to their effects on the autonomic nervous system some drugs can cause constipation. These include the vinca alkaloids such as Vincristine. Some antiemetics, including graniestron, can exacerbate the symptoms. Patients must be given advice on managing constipation as part of the pre-treatment information. Patients receiving these drugs are at risk of developing paralytic illeus and must be advised to monitor their bowel actions and contact the treatment centre for advice if their constipation continues. North Trent anticancer therapy education programme V3 October 2011 Page 47 of 97 Cardiac toxicity The most common cardiac toxicities include congestive cardiac failure and cardiomyopathy. Cardiac effects can be acute. For example, ECG changes and arrhythmias can occur within hours of treatment administration with high risk drugs such as doxorubicin, daunorubicin and 5 fluorouracil (Mallinson 2003). Cardiac effects can also be long term and chronic. Long term cardiac toxicity is most commonly associated with the use of anthracyclines such as doxorubicin, daunorubicin or epirubicin. Anthracyclines directly damage the cardiac myocyte cells, resulting in cellular destruction within the cardiac tissue (Camp-Sorrel 2006). Cardiac changes have been related to total cumulative doses of anthracyclines. Cumulative drug dose is the single greatest risk factor; therefore, there are maximum doses of these drugs that can be given. Other drugs that can cause cardiac damage include high-dose cyclophosphamide, 5fluorouracil (and capecitabine), paclitaxel (Taxol), ifosfamide, herceptin and lapatanib. The patient’s cardiac function must be monitored by MUGA scan or echocardiography prior to the first administration of herceptin or lapatinib and at regular intervals during the course of treatment. Hypertension is a side effect associated with the monoclonal antibodies sunitinib and Bevacizumab. Blood pressure monitoring is required prior to each cycle and more frequently if hypertension is identified. Medical treatment using anti-hypertensive medication is required if hypertension develops. In many cases it can be controlled without discontinuing treatment (Pyle et al 2008) All patients receiving anticancer therapy associated with cardiac toxicity must be informed of the risk and the need to contact the treatment centre immediately if they develop any symptoms. The symptoms include: chest pain, difficulty breathing, cough, leg or arm oedema or palpitations. Changes in cognitive function Changes in cognitive function have been identified as a potential side effect of chemotherapy. It is sometimes referred to colloquially as “chemo-brain” (Hess and Insel 2007). The symptoms include: impaired memory, reduced ability to plan and problem solve and forgetfulness. The effects vary between patients, different disease sites and types of chemotherapy, for example there is a higher incidence in women treated with chemotherapy for breast cancer than those with ovarian cancer (Hess and Insel 2007). This is a relatively new area of study so the patterns of incidence and recovery or decline are not yet known. As this is a subjective symptom it is important to inform patients that it may occur and encourage them to discuss any concerns they have (Nail 2006). Central nervous system (CNS) effects Ifosfamide can cause CNS side effects. Although the mechanism of damage is unclear, one possibility is that the accumulation of chloracetaldehyde (an ifosfamide metabolite) directly damages the nervous system (Nielson and Brant 2002). Signs and symptoms include: lethargy, confusion, somnolence, tonic-clonic spasms, motor unrest, mood swings, hallucinations, changes in the level of consciousness, coma and (rarely) death (Nielson and Brant 2002). If any of these symptoms occur drug administration should be stopped and supportive therapy given to manage symptoms. The symptoms usually resolve after a few days North Trent anticancer therapy education programme V3 October 2011 Page 48 of 97 Fatigue Fatigue has been consistently reported in research studies as one of the most frequently occurring and most troubling side effects of anticancer therapy. Fatigue relating to cancer and its treatment has been described as “an unusual, persistent, subjective sense of tiredness relating to cancer, or cancer treatment that interferes with usual functioning” (DeJong 2002). The unique qualities of cancer related fatigue are that it is • disproportionate to activity or exertion • not completely relieved by rest • does not correlate to activity levels • not relieved by addressing a deficiency such as sleep, food or water Patients’ experiences of treatment related fatigue have been found to vary according to the drugs being given and the schedule and method of administration (Miller 2007). While fatigue is a common problem for patients receiving anticancer therapy there is evidence to suggest that nurses may underestimate the incidence and severity of this problem for patients (Parsaie 2000). It is important to acknowledge the impact that this symptom can have on patients and provide them with information about its potential occurrence and ways of coping. Screening is recommended to identify the “7 treatable factors”: pain, emotional distress, sleep disturbance, anaemia, nutrition issues, de-conditioning or changes in activity levels and co-morbidities. Other potential factors to exclude include infection and electrolyte disturbance. A number of interventions to manage treatment related fatigue have been proposed. These include: actions such as exercising, balancing activity and rest, prioritizing and delegating activities, relaxation, diversion and sleep-enhancement techniques (Nijs et al 2008, Barsevik 2008). The effectiveness of each intervention is still being evaluated but there is increasing evidence to support the positive effects of appropriate level of exercise (Cramp 2008). Previously HCP’s have advised fatigued patients to rest. Many patients found this wasn’t helpful and some reported feeling just as tired after resting. More sleep and rest will not necessarily be beneficial as decreasing activity could lead to de-conditioning and decreased activity tolerance. The important thing is to promote good quality sleep and energy conservation. Appropriate advice on sleep includes • Maintain a regular sleep-wake schedule, avoid long afternoon naps • Avoid stimulating substances before bed time • Have a bedtime routine and keep at least an hour to relax before going to bed • Minimise night time environmental disruption and remove unpleasant stimuli (e.g. clocks) • Avoid lying in bed awake and don’t stay in bed any longer than they intend to sleep • Go to bed only when sleepy, use the bedroom only for sleep or sexual activity North Trent anticancer therapy education programme V3 October 2011 Page 49 of 97 Fertility The impact of anticancer therapy on fertility will depend on a number of factors including: gender, age and the specific drug(s) and dose(s) of treatment being given. Some anticancer therapy drugs have little impact on fertility while others cause infertility at standard doses (Knobf 2006, Thaler-DeMers 2006, Royal College of Physicians 2007). Male patients receiving anticancer therapy likely to cause infertility should be offered sperm banking. Sperm can be stored for up to 10 years. For female patients it is possible to store fertilised ova. However, this can be difficult to achieve as it can result in treatment delays. Anticancer therapy can also induce an accelerated menopause and women may need advice for coping with symptoms such as hot flushes and vaginal dryness (Knobf 2006, Foster 2002, Royal College of Physicians 2007). Women can remain fertile during anticancer therapy even if their menstrual cycle becomes disrupted or stops and should be advised to use effective contraception during treatment. Women are advised to wait 2 years before attempting parenthood – the main reason for this being that most recurrences occur within 2 years. Men are advised to wait for 1 year as the mutational risks from damaged sperm are most likely to occur within this period (Thaler-DeMers 2006, Royal College of Physicians 2007). Haemorrhagic cystitis Bleeding from the bladder. This side effect is associated with the drugs Ifosfamide and Cyclophosphamide (Cocburn and Michell 2002). It is caused by a by-product of the metabolism of these drugs (Acrolein) which can damage the urinary tract. During administration of high doses of these drugs the patient’s urine must be tested for the presence of blood and the doctor informed if blood is detected. Concurrent administration of Mesna is given to protect the bladder and extra doses of Mesna can be given if bleeding occurs. Hand foot syndrome The other name for this is palmar-plantar erythrodyesthesia. The incidence is increasing as it is associated with a number of drugs that are being used more widely such as capecitabine (Innes 2007). Symptoms include: Grade 1: Numbness, tingling, painless erythema and swelling Grade 2: Peeling, painful erythema and swelling, discomfort that affects activities of daily living Grade 3: Moist desquamation, ulceration, blistering and severe pain, unable to work or perform activities of daily living At grade 2 or above treatment with the drug that caused hand foot syndrome needs to be halted while the symptom is managed. The dose may need to be modified prior to being recommenced. Symptom management will depend on the severity of the condition and can include emollient cream, cooling, analgesia and wound care. It does diminish within a few days of stopping treatment but if left unmanaged it can progress rapidly so patient information about this symptom and its management is essential (Innes 2007, Webster 2007, Harold 2010). North Trent anticancer therapy education programme V3 October 2011 Page 50 of 97 Mucositis Oral problems are a common, and often predictable, consequence of anticancer therapy. They can be caused by the action of the particular agent on the oral mucosa. It can also be a secondary complication of neutropaenia as the mouth will become susceptible to infection. Oral mucositis is a dose and treatment limiting toxicity of several anticancer therapy agents (Harris 2008). The mouth is important for eating, drinking, speech, communication, taste, and breathing. Oral health is essential to ensure comfort, maintain nutritional status, protect against infection and maintain patient well being (Miller 2001). Moderate and severe oral dysfunction can significantly affect the patient’s quality of life. Consequences include: pain, difficulty communicating, infection, bleeding, poor nutritional status, taste changes, low mood, prolonged recovery, disturbed sleep, diminished well being and quality of life (Cawley 2005) Engaging the patient in the process of mouthcare can lead to improvements in oral health and the prevention of oral problems. It is important to teach the patient how to carry out oral assessment and oral hygiene (Cawley 2005). There must be careful assessment and monitoring of the oral cavity throughout the course of the chemotherapy, and encouragement of rigorous oral hygiene (Sieracki 2009). Oral assessment should be carried out daily in patients with actual or potential oral health problems (Yaeger 2000, Sieracki 2009). It should include an evaluation of the lips, oral mucosa, tongue, saliva and teeth. It also includes assessing alterations in voice, ability to swallow and level of discomfort (Jaroneski 2006). Where available an appropriate oral assessment tool should be used to structure and document the examination. Any evidence of oral disease should be reported to the doctor. Patients need to be informed of the need for good oral hygiene and told how to observe for signs of oral infection. Routine mouthcare should include brushing the teeth with a toothbrush and fluoride toothpaste twice daily (in the morning and before going to bed). Patients should also rinse the mouth with water to remove food debris after each meal. If patients have dentures they should follow the same routine but remove and clean their dentures. Patients who develop mucositis will require regular and frequent mouthcare, pain control and interventions to ensure their dietary and fluid intake are maintained (Cooley 2002). Nephrotoxicity A number of anticancer therapy agents have the potential to cause renal damage. Patient characteristics can also increase the chances of developing nephrotoxicity. For example, older patients and those with co-morbidities such as diabetes, hypertension and heart failure are at increased risk. Careful monitoring of blood chemistry is required in patients receiving chemotherapy that is nephrotoxic (Coburn and Mitchell 2002). Cisplatin is particularly nephrotoxic and IV fluids are given before and after Cisplatin administration to promote a good urine output so the chemotherapy is voided through the kidneys effectively. Throughout the administration of Cisplatin the patient’s fluid balance is monitored carefully to ensure the chemotherapy is being excreted effectively. If the urine output drops below 150 ml per hour during and immediately post administration, or the patient is in a positive fluid balance after they have received post hydration, the doctor should be informed so Mannitol, or a diuretic, can be administered. North Trent anticancer therapy education programme V3 October 2011 Page 51 of 97 Many anticancer therapy agents are excreted via the kidneys, which mean that renal function needs to be checked prior to treatment administration to prevent overall toxicity. This is measured by the serum creatinine (or creatinine clearance if the chemotherapy is particularly nephrotoxic). For agents excreted via the kidneys, dose reduction will be necessary if renal function is impaired. Bevacizumab can cause proteinuria which at very high levels can cause Nephrotic syndrome which is a potentially fatal condition characterized by persistently high levels of proteinuria. Bevacizumab-associated proteinuria rarely leads to renal dysfunction, however, patients’ urine protein levels need to be monitored using dipstick urinalysis prior to each bevacizumab infusion (Blowers 2009). Neurotoxicity Peripheral neuropathy is a dose limiting side effect of a number of anticancer therapy agents including cisplatin, oxaliplatin, paclitaxel (Taxol), etoposide and the vinca alkaloids eg Vincristine. The symptoms of peripheral neuropathy include pain, tingling, altered sensation and numbness which usually starts in the toes and/or finger tips. It then moves closer to the centre of the body (i.e from the fingers to the hands, wrist and arms and from the toes to the foot, ankle and calf). The symptoms can lead to difficulties with daily activities and can be painful having a negative impact on quality of life (Smith 2008). Peripheral neuropathy is usually a cumulative dose related side effect. If it is causing neurological dysfunction the treatment regimen will be reviewed and the dose of the causal drug reduced. The symptoms usually improve over time once treatment with the causal drug has ended but some residual effects may remain. The effects may continue for months beyond treatment completion. Oxaliplatin can result in 2 different types of peripheral neuropathy. The first is the neuropathy described above where the onset occurs following treatment and gradually improves over six to eight months. The second type is acute neuropathy which occurs 30 to 60 minutes after infusion. Patients can experience dysesthesia of the hands and feet, jaw tightening and a sense of difficulty breathing – not accompanied by respiratory distress (pharyngo-laryngo dysesthesia). This can be a very distressing side effect and patients must be informed about it prior to treatment so they can take preventative action. Pharyngo-laryngo dysesthesia is often associated with cold temperatures and patients should be advised to avoid cold drinks or food while they are having their treatment and to wear gloves and scarves when going into the cold (Armstrong 2005). Pulmonary toxicity Long term lung damage such as lung fibrosis can be induced by a number of chemotherapy agents. These drugs include: high dose bleomycin, cytarabine, high-dose cyclophosphamide, carmustine (BiCNU), mitomycin-C, busulfan, methotrexate, procarbazine, docetaxel (Taxotere) and gemcitabine (Camp-Sorrell 2006). High dose bleomycin is associated with pulmonary toxicity. Patients who have received extensive treatment with bleomycin may be at risk of developing respiratory failure if a general anaesthetic is given with high oxygen concentrations. Patients should be made aware of this and asked to inform health care professionals when this is appropriate. Patients who have received drugs associated with pulmonary toxicity should be advised to inform medical staff if they develop any respiratory problems or changes in the future. North Trent anticancer therapy education programme V3 October 2011 Page 52 of 97 Skin reactions A number of anticancer therapies can cause skin reactions and rashes. They are a relatively common side effect of a group of treatments called dual epidermal growth factor receptor (EGFR) inhibitors and tyrosine kinase inhibitors. Treatment with EGFR inhibitors has been associated with skin, hair and nail toxicities which are thought to be related to EGFR inhibition in the Epidermis (Camburn 2009). Erlotinib (tarceva) and laptanib are examples of this group of drugs. Skin reactions can be marked and very visible as they can appear on the face and trunk which can be very distressing for some patients. Patients are advised to use an emollient moisturiser on commencing treatment to manage dry skin reactions. Treatment that can be used on more severe reactions include antibiotics if infection is present, anti histamines if the skin is itchy and topical steroid cream if eczema is present. Refer to the EGFR skin reaction guidelines. Acne treatments are NOT recommended as the cause of the skin reaction is different and they will have little effect. If the rash is persistent and severe, referral to dermatology should be considered. Tumour Lysis Syndrome Tumour lysis syndrome (TLS) is an oncology emergency. It is a serious and potentially life-threatening complication of cancer therapy. It occurs when cancer treatments cause the destruction (or lysis) of a large number of rapidly dividing cancer cells, overwhelming the body’s ability to excrete the end products of cell death (Cantril 2004). As cells die they release potassium, phosphorous and nucleic acids into the systemic circulation. If the volume released exceeds the body’s ability to metabolise and excrete them it can cause electrolyte imbalances such as hyperkalaemia, hyperuricamia and hyperphosphataemia. These place the patient at risk of renal failure and cardiac abnormalities including ventricular tachycardia and cardiac arrest. Based on the presence of certain risk factors, patients can be placed into low, intermediate, or high-risk categories for developing tumour lysis syndrome (HeldWarmkessel 2010). • High-risk: bulky disease with a high sensitivity to chemotherapy e.g. Burkitt lymphoma, lymphoblastic lymphoma, T-cell acute lymphoblastic leukaemia or B-cell acute lymphoblastic leukemia. • Intermediate risk: diffuse large-cell lymphoma or another type of rapidly growing cancer. • Low-risk: indolent (slow-growing) lymphoma or another slowly proliferating cancer Tumour lysis syndrome usually starts within 24 - 48 hours of treatment commencing but it can occur up to 5-7 days after the start of chemotherapy (Tadman and Roberts 2005). Signs and symptoms of tumour lysis syndrome The early signs of TLS may not be readily apparent and may be detected by abnormal blood chemistry results (Cantrill 2004). The signs and symptoms of TLS include: High potassium, phosphate and urea blood chemistry levels decreased urine output, flank pain, hypertension, tachycardia, ECG changes, caridac arrhythmia, nausea and vomiting, diarrhoea, abdominal colic, muscle weakness, muscle cramps, twitching, confusion, delirium North Trent anticancer therapy education programme V3 October 2011 Page 53 of 97 The practitioner should observe the patient for these symptoms and seek medical review if any occur. In patients where there is a risk of tumour lysis syndrome blood chemistry tests must be carried out and checked frequently and nurses play a vital role in confirming that this has happened. Patients at high risk of developing TLS are often prescribed allopurinol as prophylaxis before commencing their chemotherapy. Intravenous fluids are also often given to optimise urinary output before, during and after chemotherapy administration. The patients urine output and fluid balance must be monitored carefully to ensure a good diuresis has been achieved (100 -150 mls/hour) and to detect any decrease in urine output. Other side effects of anticancer therapy include: • Anorexia, • Taste changes, • Reactivation of Radiotherapy sites eg Epirubicin and Doxorubicin. • Occular irritation. • Aching joints and muscles eg Paclitaxel. • Nail discolouration and ridges eg Bleomycin, lapatinib. • Tumour site pain. • Coloured urine (e.g. epirubicin, doxorubicin, itozantrone). • Increased risk of bleeding, not related to low platelets (e.g. Bevacizumab) • Veno–occlusive disease of the liver (VOD). VOD, is partial or total occlusion of the small blood vessels within the liver usually due to haemorrhage and/or thrombus, sometimes leading to irreparable damage to the liver and is a serious and potentially fatal complication of chemotherapy/radiotherapy. North Trent anticancer therapy education programme V3 October 2011 Page 54 of 97 MODULE 5 PATIENT ADVICE/INFORMATION Patient Information and anticancer therapy Providing clear information in relation to anticancer therapy treatment and side effects is an important aspect of patient care. Ensuring the patient has given informed consent to their treatment is essential before administering anticancer therapy. Patients need to be aware of the side effects of treatment so they can detect problems early and take action to minimise their severity or seek medical advice when it is necessary. For example, patients at risk of neutropaenia must know to seek advice if experiencing symptoms of infection when the white cell count may be low. Similarly patients receiving treatment that can cause diarrhoea must know how to take their antidiarrhoeal medication and also to contact the hospital if they have prolonged diarrhoea due to the risk of dehydration and electrolyte imbalance. Positive outcomes of patient information include: Helping patients gain a sense of control over their illness and treatment Increasing compliance with treatment Reducing the severity and incidence of side effects by providing advice on symptom management and supportive medicines Enabling a partnership relationship between patients and health care professionals Reducing the uncertainty patients feel about their illness and treatment Satisfying the need for information seeking, which for some is an important coping mechanism Enabling people to predict and plan their future (Brennan 2004, Moore 2007). Providing patient information can be challenging. Patients can feel overwhelmed by the amount of information they have been given, particularly as some will be complex medical information that may be unfamiliar to them (Leydon 2000). Patients also vary in their preferences for the amount, type and timing of information that they require (Brennan 2004, Cox 2006). Needs and preferences for information will vary between patients. There is some treatment related information that the patient must be given, and understand to ensure they are safe once discharged. For example, knowing when and how to contact the hospital for advice is essential information particularly in relation to life-threatening or debilitating side effects. The practitioner should, at all times, act in the best interest of the patient adopting the patient advocate role. Where they feel there may be issues with regard to lack of informed consent, s/he must ensure that this issue is fully resolved prior to anticancer therapy administration. If there is clearly a lack of understanding, the practitioner should give both written and verbal information at the patient’s level of understanding. If the practitioner still feels that the patient does not possess sufficient level of understanding and/or is not happy to proceed with treatment this must be brought immediately to the attention of the physician caring for that patient and the nurse in charge of the ward/department. Clear documentation in the patient records must accompany such issues. North Trent anticancer therapy education programme V3 October 2011 Page 55 of 97 As part of the patient education process the healthcare practitioner should assess the patient’s and family’s readiness to learn, level of literacy, information-seeking, and avoidance behaviours. Timing of information must be appropriate, for example, providing detailed information about the treatment regimen on the day the patient has been given their diagnosis is inappropriate. If possible the patient should be accompanied by a family member of friend to support them (Moore 2007). It is important to try and schedule enough time for patient information to ensure that key points can be reinforced and the patient has enough time to ask questions. If possible, education should take place in a private area and written information should be provided alongside verbal information (Moore 2007). Key patient advice includes the following: • • • • How the medication works How to take their medication (oral anticancer therapy and/or supportive medicines) Expected side effects and actions that can be taken to prevent them or minimise their severity Who to contact for advice and to report symptoms of concern Ensure the patient understands that they should monitor their temperature and contact the appropriate department if it is 37.5o c or above, or if they develop any other signs of infection. Due to the possibility of low platelet counts, advise patients to report any signs of bleeding or bruising. Aspirin and non-steroidal anti-inflammatory drugs should be avoided (unless already taking for a previous medical condition) as there is a risk of bleeding with these drugs, which will be enhanced by myelosuppression caused by chemotherapy. Preparations containing paracetamol can be used for pain control, but ensure the patient is aware that these will reduce their temperature if pyrexial. They should not take paracetamol to control a raised temperature as this can mask symptoms of infection. If nausea or vomiting or diarrhoea is severe or prolonged they must contact the appropriate department as they may be at risk of dehydration. If the patient has mucositis and is unable to maintain their fluid or nutrition intake, or the pain from this symptom is not controlled by oral analgesia they should contact the appropriate department as they may need to be admitted for analgesia and nutritional support. The above are basic instructions to give to the patient undergoing anticancer therapy and apply to many regimens. However, each agent and/or regimen is associated with its own specific side effects. This information is contained on the drug and regimen specific patient information leaflets which must be given to the patient and explained to them prior to commencing their treatment. A number of helpful websites and support groups are available and patients should be encouraged to access this information where this is appropriate North Trent anticancer therapy education programme V3 October 2011 Page 56 of 97 MODULE 6 ANTICANCER THERAPY EDUCATION PROGRAMME COMPETENCY ASSESSMENT Definition of Terms Trainer: The practitioner who delivers the training locally. Assessor: A HCP with two years experience in anticancer therapy administration, has been nominated by their line manager and has relevant post basic education in Haematology/oncology with a teaching and assessing qualification. Supervisor: A nurse who has been assessed as competent in the administration of anticancer therapy and can act as a witness to observe and supervise practice by a trainee Trainee: A person undertaking the programme. Staff who are to administer anticancer therapy, must have satisfactorily completed the North Trent Anticancer Therapy Education Programme. Nursing staff should participate in local teaching sessions in order to gain the theoretical knowledge that will underpin practice. The criteria for participation in training and assessment for nursing staff are as follows: (i) Must be a registered nurse/practitioner. (ii) Must have completed the local induction programme. (iii) Newly qualified staff must have completed a period of preceptorship including the formal drug assessment. The practitioner must also have been assessed as competent in the requisite associated skills for the route of administration. For example, • Intravenous medicines administration for nurses being trained in intravenous anticancer therapy administration • Central venous access devices for nurses being trained in administration via a CVAD • Any medical equipment devices being used to administer treatment There are three components to developing competence in the administration of anticancer therapy: (i) Theoretical training and assessment. (ii) Supervised practice. (iii) Formal practical assessment These components are described below. The process of supervised practice and practical assessment needs to be completed for each mode/route of administration. Training Sessions The training sessions will provide nursing staff with the essential theoretical knowledge required to underpin practice. The sessions will be based on the content of the North Trent anticancer therapy education programme. The content of the study day/s/sessions will provide the practitioner with a comprehensive knowledge base required for them to make informed judgments and decisions around anticancer therapy. North Trent anticancer therapy education programme V3 October 2011 Page 57 of 97 Following the study session the practitioner must complete the theory assessment. The expectation is that a minimum score of 100% is a pass. Any less than the minimum score will constitute a fail and the fractioned will be expected to retake the theory assessment. When a maximum of three attempts has been undertaken the practitioner will be referred to their line manager and an action plan formulated. Supervised Practice The trainee will have a period of practical training, where they will observe anticancer therapy being administered and then progress to delivering anticancer therapy under supervision. Supervised practice will be documented in the form of a progress diary with sections for both supervisor and trainee to record the session. At an agreed point when both supervisor and trainee are agreed that sufficient progress has been made the trainee will undertake two assessments against the competency statements as outlined in the structured clinical assessment. A trainee can administer anticancer therapy under supervision before completion of the theoretical assessment. However, the theoretical assessment must be completed before undertaking the first Observed Structured Clinical Evaluation (OSCE). Both theoretical and practical assessments need to be completed in order to pass the competency training. The entire process should be completed within a period of six months for each mode of administration; however, the pathways can run concurrently. Objectives At the end of the period of supervised practice the nurse will be able to: (i) Consistently show the ability to safely administer anticancer therapy via the route being assessed and demonstrate an ability to apply theory to practice. (ii) Provide fully documented evidence completed by both trainee and supervisor to support their progress. (iii) Demonstrate a level of confidence and competence consistent with proceeding to formal assessment. Formal assessment Formal assessment is carried out by a designated assessor against the competency statements in the assessment criteria, and should only take place at a point when the: (i) Trainee and supervisor agree a sufficient and consistent level of confidence and competence has been attained for that particular route of administration (ii) Trainee has completed two assessments against the competency statements, as outlined in the structured clinical evaluation (OSCE) with the supervisor. Objectives At the end of the formal assessments the practitioner will be able to: (i) Safely administer anticancer therapy as specified within the competency statements. (ii) Demonstrate successful completion of all of the competency statements and have attained a standard consistent with being deemed a competent practitioner. Competence On successful completion of the above criteria, the trainee will be deemed competent. In order to formalise and record this, both supervisor and trainee should complete (in full) the record of competency, which requires both signatures. The supervisor must ensure that a copy of this is given to the line manager and be retained for Trust/Hospital records in the trainee’s personal file. The trainee should also keep a copy of the document for their professional portfolio. North Trent anticancer therapy education programme V3 October 2011 Page 58 of 97 The trainee has the responsibility for maintaining competence through regular practice and update of knowledge. Where there are any concerns with regard to competence, either on the part of the trainee or on the part of the Trust, this must be addressed in full through retraining and where appropriate re-assessment. All concerns regarding competency must be addressed and documented before the nurse is allowed to practice unsupervised. Guidelines for Supervisor/Assessor Supervisors and Assessors must be competent to practice the indicated skill. The minimum number of supervised practices of the skill is indicated on the assessment sheet, which must be completed and signed by each supervisor. If the trainee is unable to practice the skill and demonstrate understanding to the required standard of assessment, one further assessment may be undertaken. On successful completion of the programme and the supervised practice, the practitioner will return a copy of the assessment sheet to their immediate line manager. Non-Achievement of Competence Non-achievement of competence will result in the trainee receiving immediate accurate and detailed feedback from the assessor; all of which will be documented. An action plan will then be devised outlining further development needs and strategies for achieving this. Further periods of supervised practice, support and guidance will be given prior to the trainee retaking the assessment. Trainees failing to achieve competence on their third assessment will be deemed unsuccessful of extending their scope of professional practice and should be discussed formally through the staff development review process. This would ensure that a fair and reasonable programme of support, which enabled sufficient opportunity for the trainee to progress, was provided and followed. Annual Update of Competence Competence for each route of anticancer therapy administration must be maintained and will be evaluated annually through the annual appraisal process. This will be achieved by: (i) Reading the NT Anticancer Therapy Education Programme and signing to indicate that this has been completed. (ii) Demonstrating that you are actively working within the area of practice for: Intravenous administration You should demonstrate that you are administering anticancer therapy on a regular and frequent basis i.e. continuous practice with a break of no longer than three months. If not administering anticancer therapy on a regular basis, or you have had a break in practice of three months or longer, you should identify a plan of action with your manager. This must include undertaking a minimum of one OSCE per route of administration prior to administering IV anticancer therapy unsupervised. Oral, IM and SC competence does not need to be reassessed practically following a break in practice unless the manager or staff member feels this is required. However, staff administering anticancer therapy via these routes must read the North Trent anticancer therapy education programme and demonstrate that they have the required level of knowledge for safe practice. North Trent anticancer therapy education programme V3 October 2011 Page 59 of 97 Summary of anticancer therapy Administration Assessment Pathway There are three components to developing competence in the administration of anticancer therapy: (i) Theoretical training and assessment. (ii) Supervised practice. (iii) Formal practical assessment The pathway must be followed for each route/ method of administration. The training session and theory package only needs to be attended/completed on one occasion as it covers all routes/ methods of administration. A trainee can administer anticancer therapy under supervision before completion of the theoretical exercise. However, both theoretical and practical sessions need to be completed in order to pass the competency training. Attend the theoretical study session Complete and pass theory assessment Practice administration of anticancer therapy under supervision. Keep a record of supervised practice in progress diary. When both supervisor and trainee are agreed that sufficient progress has been made complete 2 administrations of chemotherapy using the Objective Structured Consultation Exercise (OSCE) Complete final assessment by administering anticancer therapy using the OSCE. This must be carried out with a designated assessor North Trent anticancer therapy education programme V3 October 2011 Page 60 of 97 NORTH TRENT CANCER NETWORK THEORETICAL ASSESSMENT FOR THE ADMINISTRATION OF ANTICANCER THERAPY 1. (a) What are the three primary routes of exposure to anticancer therapy? (i) (ii) (iii) (b) Identify three ways you could minimise the risk of exposure when handling anticancer therapy (i) (ii) (iii) 2. (a) What action would you take in the event of eye contamination? (b) What action would you take in the event of skin contamination? 3. (a) Why should you accurately measure a patient’s height and weight before chemotherapy is prescribed? (b) A patient is receiving Doxorubicin at 60 mg per m2 and the patient has a BSA of 1.8. What dose should be prescribed? North Trent anticancer therapy education programme V3 October 2011 Page 61 of 97 4. At which points in a patient’s anticancer therapy regimen must you check that written consent has been obtained before administering chemotherapy? 5. Which types/location of vein should be avoided for intravenous anticancer therapy administration – indicate reasons for your answer 6. Why are short, flexible, small gauge catheters preferred for cannulation in patients receiving anticancer therapy? 7. When administering IV anticancer therapy which drug should be given first? 8. (a) Irritant (b) Vesicant List three things you would look for when you carry out a cannula check (a) (b) (c) 9. (a) What is a flare reaction? (b) What are the symptoms of a flare reaction? North Trent anticancer therapy education programme V3 October 2011 Page 62 of 97 10. (a) What are the causes of venous spasm? (b) What action would you take if venous spasm occurs? 11. What is an extravasation? 12. List four possible signs of extravasation (a) (b) (c) (d) 13. Identify two measures you can take to prevent extravasation or minimise the amount of drug infiltration if extravasation should occur. (a) (b) 14. (a) List the signs of anaphylaxis (b) What action would you take if a patient developed these symptoms while receiving anticancer therapy? North Trent anticancer therapy education programme V3 October 2011 Page 63 of 97 15. (a) What is tumour lysis syndrome? (b) list 5 symptoms of tumour lysis syndrome 16. Why does rituximab have its own administration rate protocol? 17 What investigations does a patient require prior to commencing Herceptin and at regular intervals while they are receiving their course of treatment? 18. What antiemetic(s) would you give to a patient who is receiving anticancer therapy that has a high risk of causing nausea and vomiting? (according to local policy) 19. There is a chemotherapy spillage during administration, what action would you take? 20. Where do you dispose of chemotherapy? 21. List two health and safety issues you would consider when administering oral Anticancer therapy (a) (b) 22. List two health and safety issues you would consider when administering anticancer therapy by the IM route (a) (b) North Trent anticancer therapy education programme V3 October 2011 Page 64 of 97 23. (a) List two examples of anticancer therapy related events that would be identified as an adverse incident (i) (ii) (b) What documentation would you complete following any adverse incident? 24. a) What are the potential risks associated with neutropenia? (b) What information would you make sure a patient understood in relation to the risks associated with neutropenia before they were discharged? 25. a) What are the potential risks associated with thrombocytopenia? (b) What information would you make sure a patient understood in relation to the risks associated with thrombocytopenia before they were discharged? 26. A patient on oral capecitabine contacts you to say that they have had profuse diarrhoea for 3 days and are feeling weak and dizzy. (a) they are due their next dose of oral capecitabine and ask you if they should take it what advice would you give them in relation to this? (b) What other action would you advise them to take? North Trent anticancer therapy education programme V3 October 2011 Page 65 of 97 27. What advice about contraception should you give to patients on anticancer therapy? 28. What considerations should be taken before administering Taxol? (a) relating to supportive medicines (b) relating to the infusion giving set 29. A patient is admitted who has been on oral anticancer therapy at home. The junior doctor has prescribed it on the drug kardex. What does a nurse need to check before administering the drug? a) b) 30. What are the usual side effects of the following drugs: (a) Doxorubicin (b) Vincristine (c) Methotrexate (d) Capecitabine (e) Herceptin (f) Cisplatin North Trent anticancer therapy education programme V3 October 2011 Page 66 of 97 NORTH TRENT CANCER NETWORK RECORD OF COMPETENCY FOR THE THEORETICAL ASSESSMENT FOR THE ADMINISTRATION OF ANTICANCER THERAPY Supervised Statement The trainee has completed the theoretical exercise and answered all questions correctly. Signature of Assessor: …………………………………………….. Print Name: ………………………………………………………… Date: ……………………………………… Signature of Practitioner: ……………………………………………………… Print Name: ………………………………………………………… Date: …………………………………………….. North Trent anticancer therapy education programme V3 October 2011 Page 67 of 97 North Trent anticancer therapy education programme V3 October 2011 Page 68 of 97 NORTH TRENT CANCER NETWORK ANTICANCER THERAPY ADMINISTRATION PROGRESS DIARY ORAL ANTICANCER THERAPY ADMINISTRATION Date Drug administered Supervisee Description/Self Assessment Signature Supervisors Assessment and Comments Signature Date Drug administered North Trent anticancer therapy education programme V3 Supervisee Description/Self Assessment October 2011 Signature Page 70 of 97 Supervisors Assessment and Comments Signature NORTH TRENT CANCER NETWORK OBJECTIVE STRUCTURED CONSULTATION EXERCISE FOR ADMINISTRATION OF ORAL ANTICANCER THERAPY Trainees Name: - st 1 Assessment 1 2 3. 4 5 6 Greet and accurately identify patient. Explains procedure to the patient. Ensures patient receives adequate verbal/written information specific to the drug/s and their side effects Gains patient’s verbal consent to treatment and ensures written consent is documented within the patient’s records. Assesses the patients psychological and emotional state and responds appropriately Assesses the patients ability to take oral treatment – i.e. there are no physical reasons why they can’t take the tablet/capsule in an oral form Prepares appropriate equipment demonstrating awareness of safe handling and protective measures. Checks environment to ensure everything is prepared for treatment Assesses the patient’s fitness for treatment. Reviews history since last attendance if appropriate. Demonstrates knowledge of appropriate laboratory results and BSA Makes the necessary checks to ensure the correct drug is administered to the correct patient at the correct time. These checks include: Name of patient Date of Birth Patient identification number Height, weight documented and correct BSA calculated Required blood tests documented as indicated by drug protocol Date and time the drugs are to be administered Recognises the name of the drug to be administered Checks the expiry date The signature of the prescriber is documented Checks the details of the patient with the prescription chart nd 2 Assessment rd 3 Assessment Yes Yes Yes No No No Yes Yes Yes No No No Yes Yes Yes No No No Yes Yes Yes No No No Yes Yes Yes No No No Yes Yes Yes No No No st 1 Assessment 7 8 9 10 Dispenses medication safely according to the local procedures. Ensures the patient takes the oral treatment. Monitors patient for signs of adverse side effects to drugs. Demonstrates knowledge of what actions are required should these occur. Document all aspects of the procedure fully and signs the prescription sheets. Checks the patient/carer understands the information and advice they have already been given and respond to any requests for information. Ensure the patient has all medication to take home and understands how to handle/ store them. Confirm the details of the next appointment and prior tests/ investigations as appropriate. Comments: - nd 2 Assessment rd 3 Assessment Yes Yes Yes No No No Yes Yes Yes No No No Yes Yes Yes No No No Yes Yes Yes No No No Yes Yes Yes No No No Signature Signature Signature Print name Print name Print name Date Date Date 12 North Trent anticancer therapy education programme V3 October 2011 Page 72 of 97 NORTH TRENT CANCER NETWORK RECORD OF COMPETENCY FOR THE ADMINISTRATION OF ORAL ANTICANCER THERAPY Supervised Statement The trainee has completed a minimum of three supervised session of administering oral anticancer therapy. The trainee has completed a formal assessment with the designated assessor. Signature of Assessor/Trainer: …………………………………………….. Print Name: ………………………………………………………… Date: ……………………………………… Practitioner Statement I have successfully completed the minimum of three supervised practice sessions, administering oral anticancer therapy. I have completed a formal assessment with the designated assessor. I now feel confident and competent in this specific area of drug administration and am happy to continue as an independent practitioner. I fully understand my responsibilities in terms of working within the specific Trust and local cytotoxic anticancer therapy guidelines and maintaining competence. I fully understand the principles of safe practice and the need to work within the guidelines for practice set out by my professional body (e.g. the Nursing and Midwifery Council Guidelines for Practice) Signature of Practitioner: ……………………………………………………… Print Name: ………………………………………………………… Date: …………………………………………….. North Trent anticancer therapy education programme V3 October 2011 Page 73 of 97 North Trent anticancer therapy education programme V3 October 2011 Page 74 of 97 6.6 NORTH TRENT CANCER NETWORK ANTICANCER THERAPY ADMINISTRATION PROGRESS DIARY INTRAMUSCULAR/SUBCUTANEOUS ANTICANCER THERAPY ADMINISTRATION Date Drug administered Supervisee Description/Self Assessment Signature Supervisors Assessment and Comments Signature Date Drug administered North Trent anticancer therapy education programme V3 Supervisee Description/Self Assessment October 2011 Signature Page 76 of 97 Supervisors Assessment and Comments Signature NORTH TRENT CANCER NETWORK OBJECTIVE STRUCTURED CONSULTATION EXERCISE FOR ADMINISTRATION OF INTRAMUSCULAR/SUBCUTANEOUS ANTICANCER THERAPY Trainees Name: - st 1 Assessment 1 2 3 4 5 6 7 Greet and accurately identify patient. Explains procedure to the patient. Ensures patient receives adequate verbal/written information specific to the drug/s and their side effects Gains patient’s verbal consent to treatment and ensures written consent is documented within the patient’s records. Assesses the patients psychological and emotional state and responds appropriately Prepares appropriate equipment demonstrating awareness of safe handling and protective measures. Checks environment to ensure everything is prepared for treatment Assesses the patient’s fitness for treatment. Reviews history since last attendance. Demonstrates knowledge of appropriate laboratory results and reassesses BSA Makes the necessary checks to ensure the correct drug is administered to the correct patient at the correct time. These checks include: Name of patient Date of Birth Patient identification number Height, weight documented and correct BSA calculated Required blood tests documented as indicated by drug protocol Date and time the drugs are to be administered Recognises the name of the drug to be administered and knows it is suitable for intravenous use Checks the expiry date The signature of the prescriber is documented Checks the details of the patient with the chemotherapy chart and designated checker Positions patient correctly for the procedure ensuring their comfort, privacy and dignity. Identifies appropriate site for injection. Administers medication safely nd 2 Assessment rd 3 Assessment Yes Yes Yes No No No Yes Yes Yes No No No Yes Yes Yes No No No Yes Yes Yes No Yes No Yes No Yes No No No Yes Yes Yes No No No Yes Yes Yes No No No st 1 Assessment 8 9 10 11 12 Monitors patient for signs of adverse side effects to drugs or procedure. Demonstrates knowledge of what actions are required should these occur. Documents all aspects of the procedure fully documented and sign the prescription sheets. Checks the patient patient/carer understands the information and advice they have already been given and respond to any requests for information. Ensure the patient has all medication to take home and understands how to handle/ store them. Confirm the details of the next appointment and prior tests/ investigations as appropriate. Documents all aspects of the procedure fully and signs the prescription sheets. nd 2 Assessment rd 3 Assessment Yes Yes Yes No No No Yes Yes Yes No No No Yes Yes Yes No No No Yes Yes Yes No No No Yes Yes Yes No No No Signature Signature Signature Print name Print name Print name Date Date Date Comments: - North Trent anticancer therapy education programme V3 October 2011 Page 78 of 97 NORTH TRENT CANCER NETWORK RECORD OF COMPETENCY FOR THE ADMINISTRATION OF INTRAMUSCULAR/SUBCUTANEOUS ANTICANCER THERAPY Supervised Statement The trainee has completed a minimum of three supervised session of administering intramuscular/subcutaneous anticancer therapy. The trainee has completed a formal assessment with the designated assessor. Signature of Assessor/Trainer: …………………………………………….. Print Name: ………………………………………………………… Date: ……………………………………… Practitioner Statement I have successfully completed the minimum of three supervised practice sessions, administering intramuscular/subcutaneous anticancer therapy. I have completed a formal assessment with the designated assessor. I now feel confident and competent in this specific area of drug administration and am happy to continue as an independent practitioner. I fully understand my responsibilities in terms of working within the specific Trust and local cytotoxic anticancer therapy guidelines and maintaining competence. I fully understand the principles of safe practice and the need to work within the guidelines for practice set out by my professional body (e.g. the Nursing and Midwifery Council Guidelines for Practice) Signature of Practitioner: ……………………………………………………… Print Name: ………………………………………………………… Date: …………………………………………….. North Trent anticancer therapy education programme V3 October 2011 Page 79 of 97 North Trent anticancer therapy education programme V3 October 2011 Page 80 of 97 NORTH TRENT CANCER NETWORK ANTICANCER THERAPY ADMINISTRATION PROGRESS DIARY INFUSIONAL ANTICANCER THERAPY ADMINISTRATION Date Drug administered Supervisee Description/Self Assessment Signature Supervisors Assessment and Comments Signature Date Drug administered North Trent anticancer therapy education programme V3 Supervisee Description/Self Assessment October 2011 Signature Page 82 of 97 Supervisors Assessment and Comments Signature NORTH TRENT CANCER NETWORK OBJECTIVE STRUCTURED CONSULTATION EXERCISE FOR ADMINISTRATION OF INFUSIONAL ANTICANCER THERAPY Trainees Name: - st 1 Assessment 1 2 3 4 5 Greet and accurately identify patient. Explains procedure to the patient. Ensures patient receives adequate verbal/written information specific to the drug/s and their side effects Gains patient’s verbal consent to treatment and ensures written consent is documented within the patient’s records. Assesses the patients psychological and emotional state and responds appropriately Prepares appropriate equipment demonstrating awareness of safe handling and protective measures. Checks environment to ensure everything is prepared for treatment Assesses the patient’s fitness for treatment. Reviews history since last attendance. Demonstrates knowledge of appropriate laboratory results and reassesses BSA Makes the necessary checks to ensure the correct drug is administered to the correct patient at the correct time. These checks include: Name of patient Date of Birth Patient identification number Height, weight documented and correct BSA calculated Required blood tests documented as indicated by drug protocol Date and time the drugs are to be administered Recognises the name of the drug to be administered and knows it is suitable for intravenous use Checks the expiry date The signature of the prescriber is documented Checks the details of the patient with the chemotherapy chart and designated checker 6 Positions patient correctly for the procedure ensuring their comfort, privacy and dignity. Checks the patient has suitable venous access and once cannula sited ensures that a flash withdrawal of blood can be made if appropriate. nd 2 Assessment rd 3 Assessment Yes Yes Yes No No No Yes Yes Yes No No No Yes Yes Yes No No No Yes Yes Yes No No No Yes Yes Yes No No No Yes Yes Yes No No No st 1 Assessment 7 8 9 10 11 12 13 Administers medication safely, assessing cannula site regularly. Gives drugs via the prescribed route at the prescribed rate in the appropriate order according to local guidelines. During administration monitors infusion rate and adjusts if required. Monitors patient for signs of adverse side effects to drugs or extravasation. Demonstrates knowledge of what actions are required should these occur. Removes the cannula or disconnects from venous access device on completion of treatment according to hospital guidelines. Document all aspects of the procedure fully documented and sign the prescription sheets. Checks the patient patient/carer understands the information and advice they have already been given and respond to any requests for information. Ensure the patient has all medication to take home and understands how to handle/ store them. Confirm the details of the next appointment and prior tests/ investigations as appropriate. Documents all aspects of the procedure fully and signs the prescription sheets. Comments North Trent anticancer therapy education programme V3 nd 2 Assessment rd 3 Assessment Yes Yes Yes No No No Yes Yes Yes No No No Yes Yes Yes No No No Yes Yes Yes No No No Yes Yes Yes No No No Yes Yes Yes No No No Yes Yes Yes No No No Signature Signature Signature Print name Print name Print name Date Date Date October 2011 Page 84 of 97 NORTH TRENT CANCER NETWORK RECORD OF COMPETENCY FOR THE ADMINISTRATION OF INFUSIONAL ANTICANCER THERAPY Supervised Statement The trainee has completed a minimum of three supervised session of administering infusional chemotherapy. The trainee has completed a formal assessment with the designated assessor. Signature of Assessor/Trainer: …………………………………………….. Print Name: ………………………………………………………… Date: ……………………………………… Practitioner Statement I have successfully completed the minimum of three supervised practice sessions, administering infusional anticancer therapy. I have completed a formal assessment with the designated assessor. I now feel confident and competent in this specific area of drug administration and am happy to continue as an independent practitioner. I fully understand my responsibilities in terms of working within the specific Trust and local cytotoxic anticancer therapy guidelines and maintaining competence. I fully understand the principles of safe practice and the need to work within the guidelines for practice set out by my professional body (e.g. the Nursing and Midwifery Council) Signature of Practitioner: ……………………………………………………… Print Name: ………………………………………………………… Date: …………………………………………….. North Trent anticancer therapy education programme V3 October 2011 Page 85 of 97 North Trent anticancer therapy education programme V3 October 2011 Page 86 of 97 6.8 NORTH TRENT CANCER NETWORK ANTICANCER THERAPY ADMINISTRATION PROGRESS DIARY BOLUS ANTICANCER THERAPY (PERIPHERAL CANNULA) ADMINISTRATION Date Drug administered Supervisee Description/Self Assessment Signature Supervisors Assessment and Comments Signature Date Drug administered North Trent anticancer therapy education programme V3 Supervisee Description/Self Assessment October 2011 Signature Page 88 of 97 Supervisors Assessment and Comments Signature NORTH TRENT CANCER NETWORK OBJECTIVE STRUCTURED CONSULTATION EXERCISE FOR ADMINISTRATION OF BOLUS (PERIPHERAL) ANTICANCER THERAPY Trainees Name: 1 2 3 4 5 6 Greet and accurately identify patient. Explains procedure to the patient. Ensures patient receives adequate verbal/written information specific to the drug/s and their side effects Gains patient’s verbal consent to treatment and ensures written consent is documented within the patient’s records. Assesses the patients psychological and emotional state and responds appropriately Prepares appropriate equipment demonstrating awareness of safe handling and protective measures. Selects appropriate method of administration (eg down a side arm of an infusion, directly to cannula etc). Checks environment to ensure everything is prepared for treatment Assesses the patient’s fitness for treatment. Reviews history since last attendance. Demonstrates knowledge of appropriate laboratory results and reassesses BSA Makes the necessary checks to ensure the correct drug is administered to the correct patient at the correct time. These checks include: Name of patient Date of Birth Patient identification number Height, weight documented and correct BSA calculated Required blood tests documented as indicated by drug protocol Date and time the drugs are to be administered Recognises the name of the drug to be administered and knows it is suitable for intravenous use Checks the expiry date The signature of the prescriber is documented Checks the details of the patient with the chemotherapy chart and designated checker Positions patient correctly for the procedure ensuring their comfort, privacy and dignity. Checks the patient has suitable venous access and once cannula sited ensures that a flash withdrawal of blood can be made if appropriate. st 1 Assessment Yes nd 2 Assessment Yes rd 3 Assessment Yes No No No Yes Yes Yes No No No Yes Yes Yes No No No Yes Yes Yes No No No Yes Yes Yes No No No Yes Yes Yes No No No st 1 Assessment 7 8 9 10 11 12 Administers medicaiton safely, assessing cannula site regularly. Gives drugs via the prescribed route at the prescribed rate in the appropriate order according to local guidelines. During administration monitors infusion rate and adjusts if required. Monitors patient for signs of adverse side effects to drugs or extravasation. Demonstrates knowledge of what actions are required should these occur. Removes the cannula or disconnects from venous access device on completion of treatment according to hospital guidelines. Document all aspects of the procedure fully documented and sign the prescription sheets. Checks the patient patient/carer understands the information and advice they have already been given and respond to any requests for information. Ensure the patient has all medication to take home and understands how to handle/ store them. Confirm the details of the next appointment and prior tests/ investigations as appropriate. nd 2 Assessment rd 3 Assessment Yes Yes Yes No No No Yes Yes Yes No No No Yes Yes Yes No No No Yes Yes Yes No No No Yes Yes Yes No No No Yes Yes Yes No No No Signature Signature Signature Print name Print name Print name Date Date Date Comments: - North Trent anticancer therapy education programme V3 October 2011 Page 90 of 97 NORTH TRENT CANCER NETWORK RECORD OF COMPETENCY FOR THE ADMINISTRATION OF BOLUS (PERIPHERAL) ANTICANCER THERAPY Supervised Statement The trainee has completed a minimum of three supervised session of administering bolus (peripheral) anticancer therapy. The trainee has completed a formal assessment with the designated assessor. Signature of Assessor/Trainer: …………………………………………….. Print Name: ………………………………………………………… Date: ……………………………………… Practitioner Statement I have successfully completed the minimum of three supervised practice sessions, administering bolus (peripheral) anticancer therapy. I have completed a formal assessment with the designated assessor. I now feel confident and competent in this specific area of drug administration and am happy to continue as an independent practitioner. I fully understand my responsibilities in terms of working within the specific Trust and local cytotoxic anticancer therapy guidelines and maintaining competence. I fully understand the principles of safe practice and the need to work within the guidelines for practice set out by my professional body (e.g. the Nursing and Midwifery Council) Signature of Practitioner: ……………………………………………………… Print Name: ………………………………………………………… Date: ……………………………………… North Trent anticancer therapy education programme V3 October 2011 Page 91 of 97 REFERENCES Albanell J and Baselga J (2000) Systemic Therapy. Emergencies Seminars in Oncology 27(3) 347-361 Allwood M, Stanley A (2002) The Cytotoxics Handbook 4th Edition Radcliffe Medical Press Armstrong T, Almadrones L, Gilbert M (2005) Chemotherapy induced peripheral neuropathy. Oncology Nursing forum 32(2) 305-311 Barsevick A e al (2008) Management of cancer related fatigue Clinical Journal of Oncology Nursing 12(5) 21-25 Benson et al (2004) Recommended guidelines for the treatment of cancer treatment induced diarrhoea: American Society of Clinical Oncology. Journal of Clinical Oncology 22 (14) 2918-2926 Blowers E, Hall K (2009) Managing adverse events in the use of bevacizumab and chemotherapy. British Journal of Nursing, 18, (6) 424-428 Camburn T (2009) A practical approach to managing the side effects of lapatinib Cancer Nursing Practice 8 (10) 21-27 Camp-Sorrel (2006) Cardio-respiratory effects in cancer survivors. Cancer Nursing 29 (2) supp. 55-59 Cantril C and Haylock P (2004) Tumour lysis syndrome. American Journal of Nursing 104 (4) 49-52 Cherney (2008) Evaluation and management of treatment related diarrhoea in patients with advanced cancer: a review Journal of Pain and Symptom Management 36 (4) 413-423 Coburn S and Mitchell S (2002) Acute renal failure: oncology nursing update. American Journal of Nursing vol 102, supp. 6-12 Cooley,C (2002) Oral Health: Basic or Essential Care?. Cancer Nursing Practice 1(3)33-39 Cooke T (2000) What is HER2? European Journal of Oncology Nursing 4. supp.1 2-9 Coughlan M, Healy C (2008) Nursing care, education and support for patients with neutropaenia. Nursing Standard 22 (46) 35-41 Cox A, Jenkins V, Catt S, Langridge C, Fallowfield L (2006) Information needs and experiences: an audit of UK cancer patients. European Journal of Oncology Nursing Vol.10 263-272 Cramp F, Daniel J (2008) Exercise for the management of cancer-related fatigue in adults Cochrane Database of Systematic Reviews. Issue 2 Davies C (2003) The impact of cancer treatment on male fertility. Cancer Nursing Practice 2 (4) 25-31 North Trent anticancer therapy education programme V3 October 2011 Page 93 of 97 Dellinger P et al (2008) Surviving sepsis campaign: international guidelines for the management of severe sepsis and septic shock. Critical Care Medicine, 36 (1) 296-327. DeJong N, Courtens A, Abu-Saad H, Schouten H (2002) Fatigue in Patients with Breast Cancer Receiving Adjuvant Chemotherapy: A Review of the Literature. Cancer Nursing 25(4) 283-297 DeNijs E, Ros W, Grijpdonk M (2008) Nursing interventions for fatigue during the treatment for cancer. Cancer Nursing 31 (3) 191- 206 Dougherty and Lister (2008) Royal Marsden Manual Clinical Nursing Procedures Blackwell London Dougherty (2008). ‘IV therapy: recognising the difference between infiltration and extravasation British Journal of Nursing 17 (14) 896-901 European Oncology Nursing Society (2007) Extravasation guidelines Feltham A (2008) Send in the clones. Cancer Nursing practice 7 (3) 19- 22 Foster R (2002) Fertility Issues in Patients with Cancer. Cancer Nursing Practice 1(1) 26-30 Foubert J (2006) Cancer related anaemia and fatigue: assessment and treatment. Nursing standard 20 (36) 50-57 Grundy M (2000) Nursing in Hematology Oncology. Baillere Tindall London Hadaway L (2007). ‘Infiltration and extravasation’. American Journal of Nursing 107 (8) 64-72 Harold K (2010) Effective management of adverse effects while on oral chemotherapy: implications for nursing practice European Journal of cancer care 19, 12-20 Harris D et al (2008) Putting evidence into practice. Evidence based interventions for the management of oral mucositis. Clinical Journal of Oncology Nursing 12 (1) 141 – 152 Hess L and Insel K (2007) Chemotherapy related change in cognitive function: a conceptual model. Oncology Nursing forum 34 (5) 981 -994 Innes G (2007) Hand-foot syndrome: exploring the provision of information for patients. Cancer nursing practice 6 (3) 29-33 Jaroneski L (2006) The importance of assessment rating scales for chemotherapy induced oral mucositis. Oncology Nursing Forum 33 (6) 1085 – 1090 Knobf T (2006) Reproductive and hormonal sequelae of chemotherapy in women Cancer nursing 29, 66-71 Mallinson J (2003) Cardiotoxicity Associated with Doxorubicin. Effects on the Heart of using Anthracyclines as Chemotherapy Agents. Cancer Nursing Practice Nov 2 (9) 30-34 North Trent anticancer therapy education programme V3 October 2011 Page 94 of 97 Miller M and Kearney N (2001) Oral care for patients with cancer: A review of the literature Cancer Nursing 24(4) 241- 254 Miller M and Kearney N (2004) Chemotherapy related nausea and vomiting – past reflections, present practice and future management European Journal of cancer care 13, 71-81 Miller M et al (2007) Patterns of fatigue during a course of chemotherapy European Journal of Oncology Nursing 11, 125–132 Moore S (2007) Facilitating oral chemotherapy treatment and compliance through patient/family–focused education Cancer Nursing 30 (2) 112 -121 Nail L (2006) Cognitive changes in cancer survivors Cancer Nursing 106 (3) Supplement. 48-53 National Chemotherapy Advisory group (2009) Chemotherapy services in England: Ensuring quality and safety NCAG, London National Confidential Enquiry into Patient Outcomes and Death (NCEPOD) (2008) For better or worse? A review of the care of patients who died within 30 days of receiving anti-cancer therapy, NCEPOD, London National Extravasation Service (2005) www.extravasation.org.uk last accessed July 2011 Nielsen E and Brant J (2002) Chemotherapy induced toxicity: assessment and interventions for patients at risk American Journal of Nursing Vol. 102, 16-19 Nirenmerg A, Bush A, Davis A, Friese C, Gillespe T, Rice R (2006a) Neutropaenic state of the knowledge part 1 Oncology Nursing Forum 33 (6) 1193 - 1201 Nirenmerg A, Bush A, Davis A, Friese C, Gillespe T, Rice R (2006b) Neutropaenic state of the knowledge part 2 Oncology Nursing Forum 33 (6) 1202 - 1208 The National Patient Safety Agency (2008) Rapid Response Report Risks of incorrect dosing of oral anti-cancer medicines Reference: NPSA/2008/RRR001 issued on 22 January 2008 Nursing and Midwifery Council (NMC) Code of Professional Conduct May 2008 Nursing and Midwifery Council (NMC) Standards for medicines management 2008 North Trent Cancer Network Guidelines for the Recognition and Treatment of Neutropaenic Sepsis 2011 Oakley C et al (2010) Safe practice and nursing care of patients receiving oral anticancer medicines: a position statement from UKONS. Ecancer 4, 177 Parsaie F, Golchin M, Asvadi (2000) A Comparison of Nurse and Patient Perceptions of Chemotherapy Treatment Stressors; Cancer Nursing 23(5) 371-374 North Trent anticancer therapy education programme V3 October 2011 Page 95 of 97 Power S and Condon C (2008) Chemotherapy induced alopecia: a phenomenological study Cancer Nursing Practice 7 (7) 44 - 47 Pyle L, Beirne D, Bird J, Hoggarth L, Jamieson C, Lane L (2008) Managing the side effects of sunitinib: a guide to empowering the patient Cancer nursing practice 7 (4) 42-46 Resuscitation Council UK (2008) Emergency Medical Treatment of Anaphylactic Reactions: Resuscitation council UK www.resus.org.uk Roe H (2011) Chemotherapy-induced alopecia: advice and support for hair loss British Journal of Nursing 20 (10) S4-11 Royal College of Nursing (2010) Standards for Intravenous Therapy; Royal College of Nursing Publications Royal College of Physicians, The Royal College of Radiologists, Royal College of Obstetricians and Gynaecologists (2007) The effects of cancer treatment on reproductive functions: Guidance on management. Report of a Working Party. London: RCP Saureland C, Engelking C, Wickham R, Corbi D (2006). ‘Vesicant extravasation part 1: mechanisms, pathogenesis and nursing care to reduce risk’, Oncology Nursing Forum Sieracki R., Voelz L., Johannik, T., Kopaczewski, D., Hubert K (2009) Development and implementation of an oral care protocol Clinical Journal of Oncology Nursing 13 (6)718-722 Schulmeister L (2008) Patient misidentification in oncology care. Clinical Journal of Oncology Nursing 12 (3) 495-498 Schwappach D., Hochreutener M. and Wernli M. (2010) Oncology Nurses’ Perceptions About Involving Patients in the Prevention of Chemotherapy Administration Errors. Oncology Nursing Forum 37(2) 84-91 Skills for Health Chemotherapy Workforce Competence Framework (2005) Smith E, Beck S, Cohen J (2008) The total neuropathy score: a tool for measuring chemotherapy induced peripheral neuropathy Oncology Nursing Forum 35 (1) 96-102 Souhami R and Tobias J (2005) Cancer and its management 5th Edition Blackwell publications Tadman M and Roberts D (2007) Oxford handbook of cancer nursing Oxford University Press Thaler-Demers (2006) Endocrine and fertility effects in male cancer survivors Cancer Nursing 29, 66-71 Vidal C (2011) Chemotherapy induced nausea and vomiting: A European perspective British Journal of Nursing 20 (10) s22-28 North Trent anticancer therapy education programme V3 October 2011 Page 96 of 97 Webster et al (2007) Palmar plantar erythodysesthesia (PPE): a literature review with comment on experience in a cancer centre European Journal of Oncology Nursing 11 (3) 238-245 Wells S (2008) Venous access in oncology and haematology patients Nursing Standard 22 (52) 39 – 46 Wickham R, Engelking C, Saureland C, Corbi D (2006). ‘Vesicant extravasation part 2: evidence based management and continuing controversies’, Oncology Nursing Forum 33 (6) 1143-1147 Yeager, K et al (2000) Implementation of an Oral Care Standard for Leukaemia and Transplantation Patients Cancer Nursing 23(1) 40-47 North Trent anticancer therapy education programme V3 October 2011 Page 97 of 97