* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Does dietary knowledge influence the eating behaviour of
Dietary fiber wikipedia , lookup
Low-carbohydrate diet wikipedia , lookup
Food politics wikipedia , lookup
Calorie restriction wikipedia , lookup
Body fat percentage wikipedia , lookup
Food studies wikipedia , lookup
Adipose tissue wikipedia , lookup
Fat acceptance movement wikipedia , lookup
Academy of Nutrition and Dietetics wikipedia , lookup
Obesity and the environment wikipedia , lookup
Abdominal obesity wikipedia , lookup
Diet-induced obesity model wikipedia , lookup
Food choice wikipedia , lookup
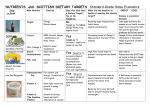
Human nutrition wikipedia , lookup
Editorial Does dietary knowledge influence the eating behaviour of adolescents? more than 40% of their daily energy and fat intake from out of home meals with the students having a low intake of fruit and vegetables and a high intake of fat.11 In order to develop a true understanding of adolescents’ eating behaviour and food choices it is necessary to briefly consider such behaviour from an ecological perspective.1 Four levels of influence impact on the nutritional health of teens. Firstly, individual or intrapersonal factors such as the psycho-social and biological factors immediately drive behaviour. Secondly, the social environment (or interpersonal factors) in which the adolescent lives, in terms of peers and family members, plays a strong role. Thirdly, one needs to place the adolescent in the perspective of his/her community and environment in terms of influences impacting on nutrition-related behaviour. Outside influences such as availability and access to fast food outlets, school tuckshops, food stores and vendors in the vicinity may play a role in his/her decision making. Lastly the macroenvironment needs to be understood in terms of the society in which the adolescent finds himself/herself. The latter influences include effects of mass media and advertising1. For example, research in the USA since the nineties has shown that advertisements on children’s programmes on television are frequently the direct opposite of the recommended diet. They are mainly for fast foods and for foods rich in sugar and fat. Very few, if any promulgate a fruit and vegetable intake.2 In South Africa there is little published data on adolescent food patterns and nutrition-related knowledge. The article by Venter et al in this issue of the SAJCN on dietary fat knowledge and intake of mid-adolescents attending public schools in the Bellville/Durbanville area of the city of Cape Town12 provides important information on dietary fat intake and knowledge of fat in the diet, especially when seen in the light of the food-based South African dietary guideline “eat fat sparingly”. For nutrition professionals the information has great merit. We learn that food items contributing most to total fat intake of these middle to upper income adolescents are margarine/ butter, full cream milk and cheese or cheese spread. Full cream milk and cheese are used by the learners 30% and 24%, respectively, five or more days a week. Additionally, many other sources of fat are consumed 3–4 times a week, including fried chicken, red meat, cold cuts, salad dressing/mayonnaise, doughnuts, and potato crisps.12 Sadly, knowledge on dietary fat was evaluated as poor in 52% of the group with only 25% knowing the lowest fat containing food and 26% the highest energy source of food.12 The good news for nutrition and health professionals is the finding that those learners who had the best nutrition scores were also those who reported being very interested in nutrition. Furthermore, the majority of learners who achieved average or good scores indicated nutrition incorporation in a school subject as their source of nutrition information. The association between fat knowledge and fat intake of learners was significant with those having a higher knowledge score also having a more desirable (prudent) fat intake. Many studies have reported that adolescents frequently consume an energy-dense diet which is of poor quality in terms of essential micronutrients.3-6 This is attributed to many factors including low meal frequency; skipping breakfast; high consumption of sweetened beverages; increased consumption of energy-dense foods; increased consumption of food away from home; and skipping meals.3-6 In the USA, food choices of adolescents do not meet the Dietary Guidelines for Americans; the diet is low in fruits and vegetables and dairy products and high in fat.7 Furthermore, a British study8 has reported data from national surveys in 1997 and eight years later. Sugarsweetened beverages remained the most popular choice of snack after eight years; however the frequency of consumption and the portion sizes were significantly higher. This last finding is of crucial importance to developing and fostering healthy dietary practices in adolescents. It appears that dietary knowledge has an effect on nutrition behaviour and furthermore that this knowledge can be imparted at school. The literature shows that there have been many curriculum-based school nutrition programmes which have improved knowledge and eating behaviour of schoolchildren. The majority of these have been undertaken in primary schools in children aged between 8 and 11 years. Some of the best known examples are Pathways, CATCH, Kansas Lean, CHIC, Know Your Body and Eat Well and Keep moving.13-18 In these studies nutrition knowledge improved significantly after a nutrition curriculum taught by teachers. Furthermore, dietary fat intake decreased significantly in all these studies. Know Your Body was one In developing countries, urban residence and high socioeconomic status have been positively associated with frequency of intake of energy-dense foods in adolescents.9-11 A study in Costa Rica noted that 30% of adolescents exceeded the American Heart Association dietary recommendations for total fat and saturated fat and 50% reported a higher cholesterol intake.9 In China, a study by Shi et al10 found that high socioeconomic status and urban residence were positively associated with intake of high-energy foods such as foods of animal origin. In Benin it was noted that adolescents consumed S Afr J Clin Nutr 62 2010;23(2) Editorial of few studies which evaluated their intervention results after ten years. They found that the favourable serum changes at baseline were maintained at 10 years.17 These included total cholesterol, LDL cholesterol, HDL cholesterol and HDL-cholesterol ratio. References In high school adolescents there have been fewer school-based interventions however, but three studies which showed significant changes in knowledge and behaviour were TEENS, PATH and VYRONAS.19-21 TEENS, which was targeted at low income children in grades 7 and 8 was aimed at improving fruit and vegetable intake and decreasing fat intake of children using different types of school-based interventions. The most significant decrease in fat intake was in the intervention arm which included peer group counselling in addition to a nutrition curriculum-based arm. PATH was aimed at improving knowledge of minority students in grades 9 and 10. A nutrition education programme over 11 weeks resulted in a significant improvement in dietary intake (decreased saturated fat and cholesterol) and a significant improvement in dietary knowledge. In VYRONAS, a 12 week school-based nutrition education-based intervention resulted in a significant decreased energy and total fat intake even after a year. It also needs to be noted that some schoolbased interventions did not result in significant behaviour changes or showed very little improvement.22,23 Furthermore, long-term evaluations of school-based interventions remain scarce. 3. Moreno LA, Rodriguez G, Fleta J, Bueno-Lozano M, Lazaro A, Bueno G. Trends of dietary habits in adolescents. Crit Rev Food Sci Nutr 2010;50(2):106–112. In terms of recommendations we should be reminded of the burden of the chronic non-communicable diseases (NCDs) in South Africa and the associated high mortality rate from some of these diseases.24 Teenagers are on the brink of adulthood and it is likely that the dietary habits which have been fostered by the family and school will continue into adulthood. A low fat and saturated fat intake, on its own, is not adequate for the prevention of NCDs. Engelfriet et al25 postulate that “broader adherence to recommendations for daily intake of fruit and vegetables, fish and fatty acid composition may take away as much as 20-30% of the burden of cardiovascular disease and result in approximately one extra life year for a 40-yearold individual”. 13. Caballero B, Clay T, Davis SM, Ethelbah B, Rock BH, Lohman T et al. Pathways: a school-based, randomized controlled trial for the prevention of obesity in American Indian schoolchildren. Am J Clin Nutr 2003;78(5):1030–1038. 1. Story M, Neumark-Sztainer D, French S. Individual and environmental influences on adolescent eating behaviors. J Am Diet Assoc 2002; 102(3Suppl): S40–51. 2. Temple N, Steyn NP.Food advertisements on children’s programs on TV in South Africa. Nutrition 24 (2008)781–782. 4. Li M, Dibley MJ, Sibbritt DW, Yan H. Dietary habits and overweight/obesity in adolescents in Xi’an City, China. Asia Pac J Clin Nutr 2010;19(1):76–82. 5. Burgess-Champoux TL, Larson N, Neumark-Sztainer D, Hannan PJ, Story M. Are family meal patterns associated with overall diet quality during the transition from early to middle adolescence? J Nutr Educ Behav 2009;41(2):79–86. 6. Briefel RR. Wilson A, Gleason PM. Consumption of low nutrient, energy-dense foods and beverages at school, home, and other locations among school lunch participants and nonparticipants. 2009; 109 (2 Suppl): S79–90. 7. Sebastian RS, Wilkinson Enns C, Goldman JD. US adolescents and MyPyramid: associations between fast food consumption and lower likelihood of meeting recommendations. J Am Diet Assoc 2009;109(2):226–35. 8. Kerr MA, Rennie KL, McCaffrey TA, Wallace JM, Hannon-Fletcher MP, Livingstone MB. Snacking patterns among adolescents: a comparison of type, frequency and portion size between Britain in 1997 and Northern I relend in 2005. Br J Nutr; 101(1):122—31. 9. Mong-Rojas R. Dietary intake as a cardiovascular risk factor in Costa Rican adolescents. J Adolescent Health 2001;28(4):328–37. 10. Shi Z, Lien N, Kumar BN, Holmboe-Ottesen G. Socio-demographic differences in food habits and preferences of school adolescents in Jiangsu Province, China. Eur J Clin Nutr 2005;59(12):1439–48. 11. Nago ES, Lachat CK, Hybregts L, Roberfroid D, Dossa RA, Kolsteren PW. Food, energy and macronutrient contribution of out of home foods in school-going adolescents in Cotonou, Benin. Br J Nutr 2010;103(2):281–8. 12. Current study. Dietary fat knowledge and intake of mid-adolescents attending public schools in the Bellville/Durbanville area of the City of Cape Town. 2010; 14. Luepker RV, Perry CL, Osganian V, Nader PR, Parcel GS, Stone EJ, Webber LS. The child and adolescent trial for cardiovascular health (CATCH). J Nutr Biochem 1998;9:525–534. 15. Harris KJ, Paine-Andrews A, Richter KP, Lewis RK, Johnston JA, James V. Reducing elementary school children’s risks for chronic diseases through school lunch modifications, nutrition education, and physical activity interventions. J Nutr Educ 1997;29:196–202. 16. Harrell JS, McMurray RG, Bangdiwala SI, Frauman AC, Gansky SA, Bradley CB.. Effects of a schoolbased intervention to reduce cardiovascular disease risk factors in elementary-school children: the Cardiovascular Health in Children (CHIC) study. J Pediatr 1996;128(6):797–805. 17. Manios Y, Moschandreas J, Hatzis C, Kafatos A. Health and nutrition education in primary schools of Crete: changes in chronic disease risk factors following a 6-year intervention programme. Br J Nutr 2002;88(3):315–324. 18. Gortmaker SL, Cheung LW, Peterson KE, Chomitz G, Cradle JH, Dart H et al. Impact of a school-based interdisciplinary intervention on diet and physical activity among urban primary school children: eat well and keep moving. Arch Pediatr Adolesc Med 1999;153(9):975–983. Ideally, South African children should learn about good nutrition at home and at school. There is sufficient convincing evidence that school-based curriculum-based nutrition programmes significantly increase children’s nutrition knowledge and improve their dietary behaviour. Additionally, schools should develop school wellness policies6 and limit access to unhealthier (high sugar, high fat) food options on the premises. The HealthKick, a collaborative research study of the MRC, HSRC and UCT Sports Science Institute is one such intervention aimed at producing a nutrition and physical activity curriculum for schools in South Africa to implement as part of Life Orientation for grades 4–6. If successful in improving nutrition knowledge and behaviour of children, it can serve as a model for other schools. 19. Birnbaum AS, Lytle LA, Story M, Perry CL, Murray DM. Are differences in exposure to a multicomponent school-based intervention associated with varying dietary outcomes in adolescents? Health Educ Behav 2002;29(4):427–443. 20. Fardy PS, White RE, Haltiwanger-Schmitz K, Magel JR, McDermott KJ, Clark LT, Hurster MM. Coronary disease risk factor reduction and behavior modification in minority adolescents: the PATH program. J Adolesc Health 1996;18(4):247–253. 21. Mihas C, Mariolis A, Manios Y, Naska A, Arapaki A, Mariolis-Sapsakos T, Tountas Y. Evaluation of a nutrition intervention in adolescents of an urban area in Greece-and long-term effects of the VYRONAS study. Public Health Nutr 2009;13(5):712–9. 22. Kain J, Uauy R, Albala C, Vio F, Ceda R, Leyton B. School-based obesity prevention in children; methodology and evaluation of a controlled study. Int Journal Obesity 2004;28(4):483–493. 23. Bere E, Veierod MB, Bjelland M, Klepp KI. Outcome and process evaluation of a Norwegian schoolrandomized fruit and vegetable intervention: Fruits and Vegetables Make the Marks (FVMM). Health Educ Res 2006;21(2):258–267. 24.Steyn K, Fourie J, Temple N (eds.). Chronic Diseases of Lifestyle in South Africa: 1995–2005. Parow: MRC, 2005. 25. Engelfriet P, Hoekstra J, Hoogenveen R, Buchner F, Van Rossum C, Verschuren M. Food and vessels: the importance of a healthy diet to prevent cardiovascular disease. Eur J Cardiovasc Prev Rehabil 2010;17(1):50–5. Dr Nelia Steyn Chief Research Specialist Centre for the Study of the Social and Environmental Determinants of Nutrition Knowledge Systems Human Sciences Research Council Correspondence to: Dr Nelia Steyn, e-mail: [email protected] S Afr J Clin Nutr 63 2010;23(2)