* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Chapter 91 - Extras Springer
Management of acute coronary syndrome wikipedia , lookup
Cardiac surgery wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
Atrial septal defect wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Electrocardiography wikipedia , lookup
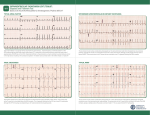
9 1 Supraventricular Tachycardias Hein J.J. Wellens Classification of Supraventricular Tachyarrhythmias . . . . . . . . . . . . . . . . . . . . . . . . . . . 1943 Other Findings Helpful in Making the Distinction Between the Different Types of Supraventricular Tachyarrhythmia . . . . . . . . . . . . . . . . . . . . . . . . . . . . 1948 Key Points • Supraventricular tachyarrhythmias (SVTs) are those tachycardias in which structures above the division of the bundle of His into the bundle branches are essential for their occurrence. • The width of the QRS complex during SVT ranges usually from 80 to 100 ms. Supraventricular tachyarrhythmia may present with a QRS complex of 120 ms or more when (1) permanent bundle branch block is present; (2) functional bundle branch block develops because of the rate of the tachycardia; (3) atrioventricular (AV) conduction during the SVT goes over an accessory AV pathway. • With atrial tachycardia, typically during the tachycardia, the electrocardiogram (ECG) shows that the P wave precedes the QRS complex, and the atrial rate during the tachycardia varies from 120 to 240 beats per minute. • Atrial flutter is associated with macro reentry in the right atrium with a regular atrial rate of 250 to 350 beats per minute and a ventricular rate that depends on AV nodal transmission characteristics. In most atrial flutter patients, the cavo-tricuspid isthmus is part of the flutter circuit. This is the area where catheter ablation is able to interrupt the reentry mechanism and cure the patient. • The most common type of atrial ventricular nodal reentry tachycardia (AVNRT) typically shows simultaneous activation of the atrium and the ventricle during the arrhythmia. • Accelerated atrioventricular junctional rhythms may occur with myocardial ischemia, with inflammation, after cardiac surgery, and in digitalis intoxication. • Accessory connections between the atrium and ventricle frequently participate in tachycardia circuits [atrioventricular reciprocating tachycardia (AVRT)]. • Alternating changes in the QRS complex during a narrow QRS tachycardia are highly suggestive of AVRT. • Adenosine given intravenously is the drug of choice for patients with SVT unless the patient has a history of bronchospasm. The Practical Approach to Diagnosis . . . . . . . . . . . . . . 1951 Treatment of Supraventricular Tachyarrhythmia . . . . . . . . . . . . . . . . . . . . . . . . . . . . 1951 Summary. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 1952 • Atrial flutter can best be terminated pharmacologically by ibutilide. • In most supraventricular tachycardias definitive cure is possible by catheter ablation therapy. Classification of Supraventricular Tachyarrhythmias Supraventricular tachyarrhythmias (SVTs) are those tachycardias in which structures above the division of the bundle of His into the bundle branches are essential for their occurrence. They can be classified as to their site of origin and mechanism as indicated in Table 91.1. As shown in that table, also accessory atrioventricular (AV) pathways and the ventricles may be incorporated in the tachycardia pathway. However, when AV conduction occurs over the AV node–His bundle branch system, they are classified as SVTs. When atrial fibrillation (see Chapter 92) is excluded, it is common to call the remaining SVTs supraventricular tachycardias. Each of these different types of SVTs has its own characteristic electrocardiographic features.1–3 The width of the QRS complex during SVT usually ranges from 80 to 100 ms. Supraventricular tachyarrhythmia may present with a QRS complex of 120 ms or more when (1) permanent bundle branch block is present, (2) functional bundle branch block develops because of the rate of the tachycardia, or (3) AV conduction during the SVT goes over an accessory AV pathway. (See also Chapter 96.) The prevalence of SVT has been estimated to be 2.25/1000 persons and the incidence 35/100,000 person-years.4 Atrial Tachycardia As shown in Table 91.1, different forms of atrial tachycardia need to be recognized. Typically, during tachycardia the electrocardiogram (ECG) shows that the P wave precedes the QRS complex (Fig. 91.1). The atrial rate during tachycardia varies from 120 to 240 per minute. The polarity of the P 19 4 3 CAR091.indd 1943 11/24/2006 1:29:04 PM 19 4 4 chapter Atrial tachycardia Paroxysmal Incessant Atrial flutter Atrial fibrillation AVNRT AV junctional accelerated rhythm Digitalis induced Post cardiac surgery Infectious Ischemic AVRT (circus movement tachycardia) Reentry DAD + + + + (mult.circ) + ? + I Abn Auto II + + III V1 V6 + + + + Abn, abnormal; AP, accessory pathway; Auto, automaticity; AV, atrioventricular; AVNRT, AV nodal reciprocating tachycardia; AVRT, atrioventricular reciprocating tachycardia; DAD, delayed after depolarization; multi.circ., multiple circuits. or AV nodal tachycardia (common type) 15 TABLE 91.1. Classification of supraventricular tachyarrhythmias according to site of origin and mechanism 91 atrial tachycardia circus movement tachycardia CN 78295 800 ms FIGURE 91.2. Example of a paroxysmal atrial tachycardia. Note the sudden onset of the arrhythmia after three conducted sinus beats with a P wave that precedes the QRS complex but has a different configuration from the sinus P waves. The arrhythmia stops spontaneously after 11 tachycardia beats. wave, the PR interval, and the ratio between P waves and QRS complexes depend on the site of origin in the atrium, the rate of atrial impulse formation, and the AV nodal transmission characteristics. The paroxysmal form is the most common type of atrial tachycardia and is characterized by a sudden onset and cessation of the arrhythmia (Fig. 91.2). The behavior of this arrhythmia during programmed electrical stimulation of the heart and its response to different antiarrhythmic drugs suggest that paroxysmal atrial tachycardia is based either on reentry or on triggered activity. Triggered activity is an arrhythmogenic mechanism resulting from delayed afterdepolarizations.5 However, it is not always possible to identify the exact mechanism of paroxysmal atrial tachycardia. A relatively rare but serious arrhythmia is the incessant (or permanent) form of atrial tachycardia (Fig. 91.3). In patients with this rhythm disturbance, the arrhythmia is present for more than 50% of the day. The rate of atrial impulse formation, which is most likely caused by abnormal automaticity, increases during exercise. The persistent nature of the tachycardia and the inability to control the ventricular rate by failure to prevent rate increase of the arrhythmia and 1 : 1 AV conduction may result in a dilated (tachycardiainduced) cardiomyopathy.6,7 Recognition that the arrhythmia is the cause rather than the consequence of the cardiomyopathy is important. Destruction of the atrial area of abnormal impulse formation by catheter ablation leads to cure of the arrhythmia and improvement in pump function. Atrial tachycardias may be uni- or multifocal. Multifocal tachycardias are usually accompanied by additional cardiac disease or obstructive pulmonary disease. Localizing Atrial Tachycardia FIGURE 91.1. Three types of supraventricular tachyarrhythmia (SVT) and the relation between QRS and P wave during tachycardia. Note that in atrial tachycardia, P precedes QRS; P occurs simultaneously with QRS in the common type of atrioventricular (AV) nodal tachycardia and follows QRS in circus movement tachycardia using a fast-conducting accessory AV pathway, also called an atrioventricular reentrant tachycardia (AVRT). CAR091.indd 1944 The ability to cure atrial tachycardia by catheter ablation requires accurate identification of the site of origin of the arrhythmia (in case of focal tachycardia), or a critical part of the tachycardia pathway (in reentrant atrial tachycardia). This should precede the catheter ablation procedure by careful intraatrial activation mapping during the tachycardia. However, the 12-lead ECG can already give an indication 11/24/2006 1:29:04 PM 19 4 5 s u p r av e n t r i c u l a r t a c h y c a r d i a s I V1 II V2 III V3 aVR V4 aVL FIGURE 91.3. Example of an incessant atrial tachycardia. This patient, initially showing 2 : 1 and later 1 : 1 AV conduction, has been continuously in tachycardia for 12 years and presented with a dilated cardiomyopathy. V5 V6 aVF where the atrial tachycardia is originating. This is done by analyzing the P-wave axis and P-wave duration during atrial tachycardia. Examples are given in Figures 91.4 to 91.6. The ECG for localizing the site of origin of an atrial tachycardia is helpful when the arrhythmia arises on the free wall of the right or left atrium or low in the intraatrial septum, but it is less helpful when the site of origin of atrial tachycardia is on the right or left side of the intraatrial septum. Atrial Flutter Observations during atrial activation mapping indicate that macro reentry in the right atrium is the common mechanism in atrial flutter.8,9 The atrial rate is regular and varies between 250 and 350 per minute, with the ventricular rate depending 1 sec 7900 on AV nodal transmission characteristics. The flutter rate may be slower in case of atrial enlargement, the use of drugs that slow conduction velocity in the atrium, or following an unsuccessful catheter ablation attempt. Atrial flutter is 2.5 times more prevalent in men than in women and very seldom occurs before the age of 50 years, and the incidence increases with aging, heart failure, and chronic obstructive lung disease.10 The classic saw-toothed pattern of atrial activity is the electrocardiographic hallmark of the arrhythmia. Carotid sinus massage–induced AV block facilitates recognition of the arrhythmia (Fig. 91.7). Figure 91.8 illustrates the two most common types of atrial flutter. Occasionally, other circuits in the right or left atrium may lead to ECG patterns of atrial flutter.11 In most atrial flutter patients, the cavotricuspid isthmus (the area in between the tricuspid valve II II I I I p p I II II III III III III V1 V1 V6 FIGURE 91.4. Example of an atrial tachycardia originating in the lateral upper part of the left atrium. The negative P wave in lead I indicates a left atrial origin. The P wave axis in the frontal plane, pointing toward lead III, betrays a superior origin. The width of the P wave (110 ms) tells that the arrhythmia is originating in the lateral wall of the atrium with sequential activation of the left and right atrium. CAR091.indd 1945 V6 81537 FIGURE 91.5. Atrial tachycardia with an origin low in the intraatrial septum. Note the superior axis (negative P waves in II and III) and the short duration of the P wave. The latter indicates an origin close to the septum with simultaneous activation of both atria. 11/24/2006 1:29:04 PM 19 4 6 chapter 91 II I II I p III I II V1 III V5 III V1 V6 400 ms FIGURE 91.7. Carotid sinus massage reveals that atrial flutter is the underlying rhythm at the atrial level. V6 81537 FIGURE 91.6. Atrial tachycardia originating in the superior part of the right atrium. Note the P wave axis in the frontal plane pointing toward lead III. pathway, and retrograde conduction over a rapidly conducting pathway (slow-fast AVNRT). During tachycardia, this results in an ECG with the P wave either completely hidden in the QRS complex or distorting the terminal portion of the QRS complex. This pattern is represented in Figure 91.1, and an ECG of the arrhythmia is shown in Figure 91.9. The P wave can be hidden in the QRS, not only because of the simultaneous activation of the atrium and the ventricle during the common type of AVNRT, but also because the P wave is very narrow (60–80 ms) since atrial activation starts low in the intraatrial septum. The common type of AVNRT occurs twice as often in women as in men. The arrhythmia also develops on average 10 years earlier in women than in men (29 ± 16 versus 39 ± 16, respectively).14 The uncommon type of paroxysmal AVNRT is characterized by a P wave that follows the QRS complex, the mechanism being retrograde conduction over a slow pathway and anterograde AV nodal conduction over either a rapid or a slow pathway. The RP interval is long, and the P wave becomes located more in the middle of two QRS complexes or in front of the next QRS and the inferior caval vein) is part of the flutter circuit. This is the area where catheter ablation is able to interrupt the reentry mechanism and to cure the patient.9 Atrioventricular Nodal Reciprocating Tachycardia The reproducible initiation and termination of paroxysmal AV nodal reciprocating tachycardia (AVNRT) by programmed stimulation of the heart suggests reentry as the underlying mechanism. This is supported by the finding of “dual” AV nodal conduction pathways in many of these patients.12,13 The common type of AVNRT typically shows simultaneous activation of the atrium and the ventricle during the arrhythmia. Anterograde conduction in the AV node during tachycardia is considered to occur over a slowly conducting A B 01042 96D674 I II III aVR aVL aVF V1 V2 V3 V4 V5 V6 CAR091.indd 1946 400 ms FIGURE 91.8. (A) “Counterclockwise” common atrial flutter, with negative flutter waves in leads II, III, and aVF, and positive flutter waves in V1. (B) “Clockwise” common atrial flutter with positive flutter waves in leads II, III, and aVF and negative flutter waves in V1. 11/24/2006 1:29:05 PM 19 47 s u p r av e n t r i c u l a r t a c h y c a r d i a s A I V1 I V1 II V2 II V2 III V3 III V4 aVR V5 aVL V6 aVF aVR FIGURE 91.9. Example of the common form of atrial ventricular nodal reentry tachycardia (AVNRT). Note the pseudo– S wave in leads II and III and the pseudo– incomplete right bundle branch block pattern in lead VI caused by the P wave during tachycardia. B aVL aVF complex (a long RP tachycardia). This is a rare arrhythmia that is seldom sustained and must be differentiated from an AV reciprocating tachycardia using a slowly conducting accessory pathway for ventriculoatrial conduction, a low atrial tachycardia, and a His bundle tachycardia with retrograde conduction to the atrium (Fig. 91.10). I VR VL VF 99426/3 V3 V4 V5 V6 400 ms Accelerated Atrioventricular Junctional Rhythm Accelerated AV junctional impulse formation (of a nonparoxysmal type) may occur in ischemia, with inflammation, after cardiac surgery, and in digitalis intoxication. The exact site of origin in the AV junction (bundle of His?) is not known. It is likely, however, as shown in Table 91.1, that the enhanced impulse formation is based on delayed afterdepolarizations (digitalis intoxication) or abnormal automaticity. Atrioventricular Reciprocating Tachycardia 1 3 2 4 1 = CMT using slow AP 2 = AVNR (uncommon type) 3 = Low atrial tachycardia 4 = His bundle tachycardia FIGURE 91.10. The four types of SVT resulting in an ECG during tachycardia showing a negative P wave in front of the QRS complex in lead II. Statistically most likely is an AVRT with AV conduction over the AV node and ventriculoatrial (VA) conduction over a slowly conducting accessory pathway (1). The other three possibilities are the uncommon form (fast-slow) of AVNRT (2), a low atrial tachycardia close to the AV node (3), or a His bundle tachycardia with retrograde conduction to the atrium (4). CAR091.indd 1947 Epicardial mapping and electrophysiologic investigations have shown that accessory connections between atrium and ventricle frequently participate in tachycardia circuits.15–17 An interesting subgroup of patients with SVT are those with a so-called concealed accessory pathway.18,19 These connections conduct the impulse only in the ventriculoatrial direction. They are often present in patients referred for evaluation of an SVT. During atrioventricular reciprocating tachycardia (AVRT), also called circus movement tachycardia, two types of concealed accessory pathways may be used (Figs. 91.11 and 91.12). Most common are patients using a rapidly conducting accessory pathway for ventriculoatrial conduction. The QRS is usually narrow, and characteristically the P wave is located shortly after the end of the QRS (the RP interval being shorter than the PR interval). The Pwave axis and width will tell where the atrial end of the accessory pathway is located. The group using a slowly conducting accessory pathway is small. Atrial activation follows the QRS complex but with an RP interval that is longer than the PR interval. This type of SVT must be differentiated from a low atrial tachycardia and an AVNRT of the uncommon type (see Fig. 91.10). Atrioventricular reciprocating tachycardia using a rapidly conducting accessory AV pathway is twice as common in men than in women. Concealed accessory pathways are about half as common as overt anterogradely conducting accessory pathways (ventricular preexcitation). The mean age at onset of the first attack of tachycardia in patients with overt or concealed accessory pathways is 10 years younger than that in patients with AVNRT.20 11/24/2006 1:29:05 PM 19 4 8 chapter 91 Other Findings Helpful in Making the Distinction Between the Different Types of Supraventricular Tachyarrhythmia Effect of Carotid Sinus Massage As shown in Table 91.2, carotid sinus massage (CSM) may induce changes during SVT that are helpful in differentiating between the different types. Before CSM is applied, severe narrowing of the carotid arteries should be excluded by checking pulsations and the absence of carotid bruits. While recording the ECG, pressure should be applied on the carotid bulb beneath the angle of the jaw, gradually increasing the pressure, which should last no longer than 5 seconds. The elderly, especially, may be very sensitive to CSM with a long period of asystole after termination of the tachycardia. CMT with “fast” AP CMT with “slow” AP FIGURE 91.11. Schematic representation of a circus movement tachycardia using a “concealed” fast-conducting (left) or slowconducting (right) accessory AV pathway. The corresponding ECGs during tachycardia with their characteristic RP/PR ratio are shown in Figure 91.12. A B 94135 I Mode of Initiation of Supraventricular Tachyarrhythmia Initiation of an SVT by a single atrial premature beat during sinus rhythm after marked prolongation of the PR interval suggests the presence of dual AV nodal pathways and AVNRT as the mechanism of the arrhythmia (Figs. 91.13 and 91.14). In contrast, initiation of an SVT during sinus rhythm without prolongation of the PR interval suggests an AVRT using an accessory pathway for ventriculoatrial conduction (Fig. 91.15). Initiation of an SVT by a single ventricular premature beat argues in favor of an AVRT (Fig. 91.16). II III aVR aVL aVF V1 TABLE 91.2. Findings on carotid sinus massage in different types of supraventricular tachyarrhythmias Tachycardia Effect of carotid sinus massage Sinus tachycardia Atrial tachycardia Paroxysmal form Gradual and temporary slowing in heart rate V2 Incessant form V3 V4 Atrial flutter V5 Atrial fibrillation V6 FIGURE 91.12. Two types of circus movement tachycardias. Circus movement tachycardia due to rapid (A) and slow conducting (B) accessory pathway (AP). The rapidly conducting AP (A) is associated with a short RP, the slow conducting AP (B) with a long RP. The P waves are relatively narrow, inverted in the inferior leads and positive in leads aVR and aVL, suggesting a septal or paraseptal location. CAR091.indd 1948 AVNRT AVRT (CMT) Temporary slowing in ventricular rate because of increase in AV block Cessation of tachycardia No effect Temporary slowing in ventricular rate because of increase in AV block No effect Temporary slowing in ventricular rate because of increase in AV block Transformation into atrial fibrillation No effect Temporary slowing in ventricular rate because of increase in AV block No effect Cessation of tachycardia No effect Cessation of tachycardia No effect AVNRT, atrioventricular nodal reciprocating tachycardia; AVRT, atrioventricular reciprocating tachycardia; CMT, circus movement tachycardia. 11/24/2006 1:29:05 PM 19 4 9 s u p r av e n t r i c u l a r t a c h y c a r d i a s A B C 92426/1 I atrium s f II AVN III His aVR aVL aVF PR 160 PR 240 PR 360 atrial echo SR APC APC common AVNT FIGURE 91.13. Initiation of an AVNRT by an atrial premature complex (APC) during sinus rhythm (SR). (A) During sinus rhythm, the atrial impulse reaches the bundle of His by way of the most rapidly conducting (the fast f) pathway. (B) An APC is conducted to the bundle of His by way of the most rapidly conducting (the fast f) pathway. This results in sudden prolongation of the PR interval compared with sinus rhythm. (C) An even earlier APC with slower conduction in the slow pathway is able to reenter the fast pathway and to initiate the common form of AVNRT. 99574 V1 V2 V3 V4 V5 I V6 920391 400 ms FIGURE 91.15. Initiation of a SVT during sinus rhythm. Note that an acceleration in rate during sinus rhythm is followed by a tachycardia with a narrow QRS complex. The RP interval exceeds the PR interval during tachycardia with negative P waves in leads II, III, V2 to V6. These fi ndings indicate the presence of a circus movement tachycardia using a slowly conducting accessory pathway for ventriculoatrial conduction. II III aVR aVL aVF V1 AV node V2 Acc P V3 His V4 V5 VPB V6 A 400 ms FIGURE 91.14. Clinical example of initiation of the common form of AV nodal tachycardia. After two sinus beats that are conducted to the ventricle, an APC is conducted to the ventricle, with marked PR prolongation indicating conduction over the slow AV nodal pathway. This is followed by perpetuation of reentry in the AV node and AVNRT. Six precordial leads were recorded simultaneously. CAR091.indd 1949 B FIGURE 91.16. (A) During sinus rhythm a circus movement tachycardia, using an accessory AV pathway, can easily be initiated by a single ventricular premature beat (VPB) because the VPB fi nds the distal conduction system refractory and is retrogradely conducted to the atrium over the accessory pathway (ACC P). (B) In contrast, because of refractoriness of the distal conduction system, a VPB cannot get to the AV node to initiate AV nodal reentry. 11/24/2006 1:29:06 PM 19 5 0 chapter 91 96536 I II III aVR AV node aVL aVF Acc P V1 His V2 V3 VPB A V4 B FIGURE 91.17. Differences for a ventricular premature beat (VPB) to get into the tachycardia circuit (and to terminate tachycardia) in AVNRT and in a circus movement tachycardia using an accessory pathway for ventriculoatrial conduction. The VPB in AVNRT will be blocked distal to the reentry circuit (B), whereas the VPB easily invades the reentry circuit during circus movement tachycardia (A). V5 V6 960829 400 ms FIGURE 91.18. Example of electrical alternans of the QRS complex during a circus movement tachycardia using a “concealed” accessory AV pathway. Note that QRS alternation is best seen in leads II, V3, and V4. Mode of Termination of Supraventricular Tachyarrhythmia As shown in Figure 91.17, it is extremely unlikely for an AVNRT to be terminated by a single ventricular premature beat. However, this is quite common in an AVRT. Electrical Alternans of the QRS Complex Alternating changes in the QRS complex during a narrow QRS tachycardia are highly suggestive for an AVRT.21 QRS alternation as a clue to an AVRT can be used only when it is present more than 5 seconds after the start of the tachycardia. Changes in QRS configuration are common at the start of SVT because the sudden acceleration in ventricular rate leads to different degrees of changes in refractoriness and conduction velocity in the conduction system. In patients with AVRT and a narrow QRS, the incidence of electrical alternans increases with increasing heart rate during tachycardia. An example of electrical alternans is shown in Figure 91.18. FIGURE 91.19. Increase in the length of the reentry circuit when bundle branch block develops during circus movement tachycardia using an accessory pathway that is on the same side as the bundle branch block. (A) There is a right-sided accessory pathway. (B) The tachycardia circuit is confi ned to the AV node. When right bundle branch block develops in the patient with a right-sided accessory pathway, the circuit becomes longer and the tachycardia rate slows; compare V1 before and after right bundle branch block on the left. In contrast (B), nothing happens to the tachycardia rate when bundle branch block develops during AVNRT (measurements are in milliseconds). CAR091.indd 1950 11/24/2006 1:29:07 PM 19 51 s u p r av e n t r i c u l a r t a c h y c a r d i a s I 84041 II III V1 effects from antiarrhythmic drugs clearly diminish the quality of life. Supraventricular tachyarrhythmias can sometimes be fatal or may lead to serious cardiac impairment when (1) life-threatening trauma occurs during syncope, (2) SVT precipitates acute pulmonary edema (in patients with severe systolic or diastolic dysfunction), (3) thromboembolism occurs, or (4) incessant SVT leads to a dilated cardiomyopathy. Symptoms during SVT, frequency of recurrences, length of episodes, and the presence or absence of additional heart disease determine the type of treatment. V4 Steps in diagnosis of narrow QRS tachycardia (QRS <0.12 sec) V6 400 ms FIGURE 91.20. The presence of a slower heart rate during SVT in a case of left bundle branch block. As explained in Figure 91.20, this indicates a circus movement tachycardia using an accessory AV pathway on the same side as the blocked bundle branch. In this example, therefore, the accessory pathway is between the left atrium and the left ventricle. 1. 2nd degree AV block? (spontaneous or after CSM) no yes Atrial rate >250/min Slowing in Heart Rate During Tachycardia when Bundle Branch Block Develops Figures 91.19 and 91.20 illustrate the importance of careful measurements of the rate of tachycardia when bundle branch block develops and disappears during SVT. As shown in Figure 91.20, a slowing in tachycardia rate during bundle branch block indicates the presence of an AVRT using an accessory AV pathway for ventriculoatrial conduction inserting into the free wall of the ventricle on the same side as the blocked bundle branch.18,19 Atrial flutter Atrial T 2. yes AVRT P wave location? 3. PR > RP P in R AVRT with fast AP AVNRT Most patients with SVT have a normal life expectancy, but their quality of life is often poor.22 The uncertainty of when SVT may occur leads to social isolation. During SVT, symptoms such as palpitations, dizziness, syncope, chest pain, and dyspnea; the need to seek hospital treatment; the feeling of prolonged tiredness after an episode of SVT; and the side CAR091.indd 1951 PR < RP uncommon AVNRT Atrial T AVRT P axis (frontal plane) 4a. inferior-superior Atrial T AVRT septal AP other Atrial T AVRT (right or left AP) P axis (horizontal plane) 4b. right Treatment of Supraventricular Tachyarrhythmia AVNRT with 2:1 block QRS alternation? no The Practical Approach to Diagnosis A stepwise approach is advised for analyzing the 12-lead ECG during SVT (Fig. 91.21). The steps include the relation between atrial and ventricular events during SVT, the presence or absence of electrical alternans and the location and configuration of the P wave. If that analysis does not facilitate a definitive diagnosis, an electrophysiologic study is indicated, especially when the tachycardia is symptomatic, leading to myocardial dysfunction, or because its frequent occurrence is annoying and socially incapacitating for the patient. ≤250/min left left right AVRT with right-sided AP AVRT with left-sided AP Atrial T Atrial T FIGURE 91.21. Four steps to be taken when analyzing the 12-lead ECG of a regular SVT. As shown, information should be obtained about the relation between atrial and ventricular events during SVT [spontaneously and after carotid sinus massage (CSM)] followed by a look for electrical alternans of the QRS complex. Thereafter, the location of the P wave in relation to the QRS complex and the polarity of the P wave in the frontal and horizontal plane should be studied. 11/24/2006 1:29:07 PM 19 5 2 chapter Vagal maneuvers (Valsalva, CSM, submerging the face in cold water, etc.) can terminate SVT when they are applied early after the start of the SVT, indicating that the patient should be informed not only how but also when to perform them. In-hospital adenosine IV is the drug of choice in most cases of SVT, unless the patient has a history of bronchospasm. Verapamil and diltiazem IV should be avoided in patients using beta-blockers. Atrial flutter can pharmacologically best be terminated by ibutilide IV. It is important to stress that patients with atrial flutter have a similar risk of thromboembolic events as patients with atrial fibrillation, indicating the necessity of adequate anticoagulation, also in relation to cardioversion attempts.23,24 As discussed in the recent guidelines for the management of patients with supraventricular arrhythmias,25 antiarrhythmic drugs can be prescribed when the SVT is relatively well tolerated, both for termination and prevention of recurrences. As shown by Alboni et al.,26 in selected patients, SVT can be safely terminated out-of-hospital by a self-administered antiarrhythmic drug. However, chronic antiarrhythmic drug treatment, because of side effects, often impairs the patient’s quality of life more than the arrhythmia itself. Therefore, cure from SVT by catheter ablation is increasingly used. It is efficacious and safe in the hands of the experienced ablator.27 Obviously, as indicated in Chapter 102, an electrophysiologic study is required when catheter ablation of the site of origin or part of the tachycardia pathway is considered. Summary Supraventricular tachycardias are common and their significance may vary from being a nuisance to life-threatening. Usually, the 12-lead ECG facilitates a correct diagnosis of the type of arrhythmia. The mode of treatment depends on the type of arrhythmia, its incidence and severity, and the presence or absence of additional heart disease that plays a role in tolerance and risks. In most supraventricular tachycardias, definitive cure is possible by way of catheter ablation of the focus of the arrhythmia or by interrupting the arrhythmia circuit (see Chapter 102). References 1. Bar FW, Brugada P, Dassen WRM, Wellens HJJ. Differential diagnosis of tachycardia with narrow QRS complex. Am J Cardiol 1984;54:555. 2. Josephson ME, Wellens HJJ. Differential diagnosis of supraventricular tachycardia. Cardiol Clin 1990;8:411. 3. Wellens HJJ, Conover MB. The ECG in Emergency Decision Making, 2nd ed. Philadelphia: WB Saunders, 2005. 4. Orejarena LA, Vidaillet H, DeStefano F, et al. Paroxysmal supraventricular tachycardia in the general population. J Am Coll Cardiol 1998;31:150. 5. Wellens HJJ, Brugada P. Mechanisms of supraventricular tachycardia. Am J Cardiol 1988;62:10. CAR091.indd 1952 91 6. Shinbane JS, Wood MA, Jensen DN, et al. Tachycardia-induced cardiomyopathy: a review of animal models and clinical studies. J Am Coll Cardiol 1997;29:709. 7. Saoudi N, Cosio F, Waldo A, et al. A classification of atrial flutter and regular atrial tachycardia according to electrophysiological mechanisms and anatomical basis. Eur Heart J 2003; 22:1162. 8. Olgin JE, Kalman JM, Fitzpatrick A, et al. Role of right atrial endocardial structures as barriers to conduction during human type I atrial flutter. Activation and entrainment mapping guided by intracardiac echocardiography. Circulation 1995;92: 1839. 9. Cosio FG, Goicolea A, Lopez-Gil M, et al. Catheter ablation of atrial flutter circuits. Pacing Clin Electrophysiol 1993; 16:637. 10. Granada J, Uribe W, Chyou PH, et al. Incidence and predictors of atrial flutter in the general population. J Am Coll Cardiol 2000;36:2242. 11. Bochoeyer A, Yang Y, Chang J, et al. Surface electrocardiographic characteristics of right and left atrial flutter. Circulation 2003;108:60. 12. Denes P, Wu D, Dhingra RC, et al. Demonstration of dual AV nodal pathways in patients with paroxysmal supraventricular tachycardia. Circulation 1973;48:549. 13. Mazgalev TN, Ho SY, Anderson RH. Anatomic-electrophysiological correlations concerning the pathways for atrioventricular conduction. Circulation 2001;103:2660. 14. Torrecilla EG, Farre J, Villacastin JP. AV nodal re-entry tachycardia: Clinical and electrophysiological characteristics. In: Farre J, Moro C, eds. Cardiac Arrhythmias: Foundations and Therapeutic Options. Barcelona: Edos, 1992:163. 15. Wellens HJJ. Electrical Stimulation of the Heart in the Study and Treatment of Tachycardias. Baltimore: University Park Press, 1971. 16. Wellens HJJ, Durrer D. The role of an accessory pathway in reciprocal tachycardia. Circulation 1975;52:58. 17. Durrer D, Roos JP. Epicardial excitation of the ventricles in a patient with Wolff-Parkinson-White syndrome (type B). Circulation 1976;35:15. 18. Coumel P, Attuel P. Reciprocating tachycardia in overt and latent pre-excitation: Influence of functional bundle branch block on the rate of tachycardia. Eur J Cardiol 1974; 1:423. 19. Wellens HJJ, Brugada P, Farre J, et al. Diagnosis and treatment of concealed accessory pathways in patients suffering from paroxysmal AV junctional tachycardia. In: Rosenbaum MB, Elizari MV, eds. Frontiers of Cardiac Electrophysiology. The Hague: Martinus Nijhoff, 1983:773. 20. Rodriguez LM, De Chillou C, Schlapfer J, et al. Age at onset and gender of patients with different types of supraventricular tachycardias. Am J Cardiol 1992;70:1213. 21. Green M, Heddle B, Dassen W, et al. The value of QRS alternation in diagnosing the site of origin of narrow QRS supraventricular tachycardia. Circulation 1983;68:368. 22. Wood KA, Drew BJ, Scheinman MM. Frequency of disabling symptoms in supraventricular tachycardia. Am J Cardiol 1997; 79:145. 23. Irani WN, Grayburn PA, Afridi I. Prevalence of thrombus, spontaneous echo contrast and atrial stunning in patients undergoing cardioversion of atrial flutter. A prospective study using transesophageal echocardiography. Circulation 1997; 95:962. 24. Corrado G, Sgalambro A, Mantero A, et al. Thromboembolic risk in atrial flutter. The FLASIEC (Flutter Atriale Societa Italiana di Ecografia Cardiovascolare): multicentre study. Eur Heart J 2001;22:104. 11/24/2006 1:29:08 PM s u p r av e n t r i c u l a r t a c h y c a r d i a s 25. Blomstrom-Lundquist C, Scheinman MM, Aliot EM, et al. ACC/ AHA/ESC guidelines for the management of patients with supraventricular arrhythmias. J Am Coll Cardiol 2003;42:1493. 26. Alboni P, Tomasi C, Menozzi C, et al. Efficacy and safety of out of-hospital self administered single-dose oral drug treat- CAR091.indd 1953 19 5 3 ment in the management of infrequent well-tolerated paroxysmal supraventricular tachycardia. J Am Coll Cardiol 2001; 37:548. 27. Morady F. Catheter ablation of supraventricular arrhythmias: state of the art. Pacing Clin Electrophysiol 2004;27:125. 11/24/2006 1:29:08 PM CAR091.indd 1954 11/24/2006 1:29:08 PM