* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Spontaneous Aortic Regurgitation and Valvular Cardiomyopathy in
Survey
Document related concepts
Transcript
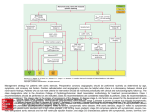
Spontaneous Aortic Regurgitation and Valvular Cardiomyopathy in Mice Georges P. Hajj, Yi Chu, Donald D. Lund, Jason A. Magida, Nathan D. Funk, Robert M. Brooks, Gary L. Baumbach, Kathy A. Zimmerman, Melissa K. Davis, Ramzi N. El Accaoui, Tariq Hameed, Hardik Doshi, BiYi Chen, Leslie A. Leinwand, Long-Sheng Song, Donald D. Heistad,* Robert M. Weiss* Downloaded from http://atvb.ahajournals.org/ by guest on May 14, 2017 Objective—We studied the mechanistic links between fibrocalcific changes in the aortic valve and aortic valve function in mice homozygous for a hypomorphic epidermal growth factor receptor mutation (Wave mice). We also studied myocardial responses to aortic valve dysfunction in Wave mice. Approach and Results—At 1.5 months of age, before development of valve fibrosis and calcification, aortic regurgitation, but not aortic stenosis, was common in Wave mice. Aortic valve fibrosis, profibrotic signaling, calcification, osteogenic markers, lipid deposition, and apoptosis increased dramatically by 6 and 12 months of age in Wave mice. Aortic regurgitation remained prevalent, however, and aortic stenosis was rare, at all ages. Proteoglycan content was abnormally increased in aortic valves of Wave mice at all ages. Treatment with pioglitazone prevented abnormal valve calcification, but did not protect valve function. There was significant left ventricular volume overload, hypertrophy, and fetal gene expression, at all ages in Wave mice with aortic regurgitation. Left ventricular systolic function was normal until 6 months of age in Wave mice, but became impaired by 12 months of age. Myocardial transverse tubules were normal in the presence of left ventricular hypertrophy at 1.5 and 3 months of age, but became disrupted by 12 months of age. Conclusions—We present the first comprehensive phenotypic and molecular characterization of spontaneous aortic regurgitation and volume-overload cardiomyopathy in an experimental model. In Wave mice, fibrocalcific changes are not linked to valve dysfunction and are epiphenomena arising from structurally incompetent myxomatous valves. (Arterioscler Thromb Vasc Biol. 2015;35:1653-1662. DOI: 10.1161/ATVBAHA.115.305729.) Key Words: aortic regurgitation ◼ aortic stenosis ◼ aortic valve disease ◼ cardiomyopathy I n patients with either aortic stenosis (AS) or aortic regurgitation (AR), morbidity and mortality accrue from exhaustion of compensatory mechanisms in the left ventricle (LV).1,2 Several mouse models of AS have been reported,3 and myocardial reponses to pressure-overload have been extensively investigated. Mechanisms of volume-overload heart failure are less completely understood. A recent Scientific Statement from the American Heart Association highlighted the absence of mouse models of valvular regurgitation and suggested that discovery of such a model would be useful for understanding the mechanisms by which chronic LV volume-overload leads to heart failure.4 EGFR-tyrosine kinase (tk) activity.6,7 Consequently, Wave mice develop histological and functional abnormalities in the aortic valve, which are strongly influenced by background strain, findings which have been interpreted as evidence for aortic valve stenosis.7 In the present study, we found that AR, not AS, is the predominant functional abnormality in Wave mice. We tested, and rejected, the hypothesis that valve fibrosis and calcification are temporally linked to progression of aortic valve dysfunction. We reported previously that treatment with pioglitazone, a PPAR-γ (peroxisome proliferator-activated receptor gamma) agonist, attenuated valve calcification and protected aortic valve function in hypercholesterolemic mice.8 In Wave mice, however, although treatment with pioglitazone prevented abnormal valve calcification, it did not protect valve function, findings which do not support a mechanistic link between valve calcification and valve dysfunction in this model. Finally, we report functional, molecular, and See accompanying editorial on page 1554 Epidermal growth factor receptor (EGFR) signaling regulates embryonic formation of semilunar heart valves.5 Inbred mice homozygous for a single-nucleotide substitution mutation in the gene encoding EGFR are known as EgfrWa2/Wa2, or waved-2 (Wave) mice, and have a global 90% reduction in Received on: December 17, 2014; final version accepted on: May 8, 2015. From the Department of Internal Medicine (G.P.H., Y.C., D.D.L., N.D.F., R.M.B., K.A.Z., M.K.D., R.N.E.A., T.H., H.D., B.C., L.-S.S., D.D.H., R.M.W.), Department of Pharmacology (D.D.H.), and Department of Pathology (G.L.B.), Roy J. and Lucille A. Carver College of Medicine, University of Iowa, Iowa City; and Department of Molecular, Cellular, and Developmental Biology (J.A.M., L.A.L., D.D.H.), University of Colorado, Boulder. *These authors contributed equally to this article. The online-only Data Supplement is available with this article at http://atvb.ahajournals.org/lookup/suppl/doi:10.1161/ATVBAHA.115.305729/-/DC1. Correspondence to Robert M. Weiss, MD, Division of Cardiovascular Medicine, University of Iowa Carver College of Medicine, 200 Hawkins Dr, E317A GH, Iowa City, IA 52242. E-mail [email protected]; or Donald D. Heistad, MD, Division of Cardiovascular Medicine, University of Iowa Carver College of Medicine, 200 Hawkins Dr, E11 GH, Iowa City, IA 52242. E-mail [email protected] © 2015 American Heart Association, Inc. Arterioscler Thromb Vasc Biol is available at http://atvb.ahajournals.org 1653 DOI: 10.1161/ATVBAHA.115.305729 1654 Arterioscler Thromb Vasc Biol July 2015 Nonstandard Abbreviations and Acronyms ACS AR AS EGFR-tk LV pSmad-2 TT Wave mice aortic cusp separation aortic regurgitation aortic stenosis epithelial growth factor receptor-tyrosine kinase left ventricle phosphorylated homolog of mothers against decapentaplegic-2 cardiomyocyte transverse tubules EgfrWa2/Wa2 mice cardiomyocyte structural responses to volume-overload in the LV, with eventual progression to heart failure in Wave mice. Materials and Methods Materials and Methods are available in the online-only Data Supplement. Downloaded from http://atvb.ahajournals.org/ by guest on May 14, 2017 Results Morphometry and Metabolism Body mass and blood chemistries were normal in Wave mice (Table I in the online-only Data Supplement). Histological Changes in Aortic Valve Valve collagen levels, assessed using Masson’s Trichrome staining, were normal in Wave mice at 1.5 months of age, but were significantly increased at 6 and 12 months of age (Figure 1A–1C). After treatment with pioglitazone, collagen levels, assessed using Pircrosirius Red staining, remained elevated in Wave mice at 6 months of age. Valve calcification, assessed using Alizarin Red staining, was undetectable in Wave mice and control mice at 1.5 months of age (Figure 1D–1F). In Wave mice, valve calcification was significantly increased, compared with age-matched control mice, at 6 and 12 months of age. After treatment with pioglitazone, valve calcification was significantly reduced in Wave mice, compared with vehicle-treated Wave mice. Lipid deposition, assessed using Oil Red-O staining, was undetectable in Wave mice and control mice at 1.5 months of age. At 6 and 12 months of age, lipid levels were significantly increased in valves from Wave mice compared with control (Figure 1G–1I). After treatment with pioglitazone, lipid levels remained elevated in Wave valves. Levels of proteoglycan in the aortic valve were significantly elevated in Wave mice at 1.5, 6, and 12 months of age (Figure 1J–1L). Figure 1. Histology of aortic valve. A–C, Aortic valve collagen detected by Masson’s Trichrome or Picrosirius Red staining (for pioglitazone-treated [Pio] mice). D–F, Aortic valve calcification, assessed using Alizarin Red staining. G–I, Aortic valve lipid content, detected using Oil Red-O staining. J–L, Proteoglycan, assessed using Movat’s Pentachrome staining (blue-green). % refers to the proportion of valve tissue exhibiting positive staining. Scale bar=500 µm. *P<0.05 vs age-matched control; **P<0.025 vs 6 months wave. Hajj et al Aortic Regurgitation in Mice 1655 Profibrotic Signaling in the Aortic Valve Downloaded from http://atvb.ahajournals.org/ by guest on May 14, 2017 Levels of α-smooth muscle actin, which indicate transdifferentiation of valve interstitial cells from a quiescent state to a profibrotic phenotype, were normal in Wave valves at 1.5 months of age. At 6 and 12 months of age, α-smooth muscle actin levels were significantly elevated in Wave valves (Figure 2A–2C). After treatment with pioglitazone, α-smooth muscle actin levels remained elevated in Wave valves. Levels of the profibrotic signaling molecule, transforming growth factor-β1, were normal in Wave valves at 1.5 months of age, but were significantly elevated at 6 and 12 months of age (Figure 2D–2F). After treatment with pioglitazone, transforming growth factor-β1 levels remained elevated in Wave valves. Phosphorylated homologue of mothers against decapentaplegia-2 (p-Smad2) is a mediator of profibrotic transforming growth factor-β1 signaling. Levels of p-Smad2 were normal in Wave valves at 1.5 months of age, but were significantly elevated at 6 and 12 months of age in Wave mice compared with control mice (Figure 2G–2I). After treatment with pioglitazone, p-Smad2 levels remained elevated in Wave valves. Levels of profibrotic signaling molecules in the aortic valve varied with age and genotype in a pattern that was similar to overall collagen levels in the aortic valve, as shown in Figure 1A–1C. Osteogenic Transdifferentiation in the Aortic Valve Osterix and osteocalcin are procalcific signaling molecules produced by osteoblast-like cells (Figure 3). Osterix and osteocalcin levels were normal in Wave mice at 1.5 months of age. At 6 and 12 months of age, osterix and osteocalcin levels were significantly elevated in Wave mice compared with control mice. After treatment with pioglitazone, osterix and osteocalcin levels in the aortic valve were not significantly different from age-matched control mice. Thus, changes in osterix and osteocalcin with age and genotype were similar to the pattern for overall valve calcification shown in Figure 1D–1F. Proteoglycans in the Aortic Valve Intact versican, a proteoglycan that modulates properties of semilunar heart valves,9,10 was increased in aortic valves from Wave mice at 6 months of age (Figure 4). Cleaved versican, a product of enzymatic breakdown of intact versican, was α Figure 2. Immunostaining for profibrotic signaling molecules in the aortic valve. Examples are shown from mice at 12 months of age. A–C, Transdifferentiation from quiescent valve interstitial cells to profibrotic myofibroblasts, indicated by staining for α-smooth muscle actin (α-SMA). D–F, Staining for transforming growth factor-β1 (TGF-β1), a profibrotic signaling molecule. G–I, Staining for p-Smad2, a mediator of profibrotic TGF-β1 signaling. J–L, Antibody-free negative controls for immunostaining. The image in L is identical to the image in K, except that L was electronically brightened to show the location of valve tissue (V). % refers to the proportion of valve tissue exhibiting positive staining. Autofluorescence (AF) arises from coherently arranged fibers in valve annulus, but not in valve. Scale bar=100 μm. *P<0.05 vs age-matched and treatment-matched control. 1656 Arterioscler Thromb Vasc Biol July 2015 Figure 3. Immunostaining for osteogenic differentiation in the aortic valve. Examples were obtained at 12 months of age. % refers to the proportion of valve tissue exhibiting positive staining. Scale bar=100 μm. *P<0.05 vs age-matched and treatment-matched control. Downloaded from http://atvb.ahajournals.org/ by guest on May 14, 2017 significantly reduced in aortic valves from Wave mice at 6 months of age (Figure 4). Intact and cleaved versican levels remained elevated after treatment with pioglitazone in aortic valves from Wave mice. Expression of ADAMTS5, an enzyme which cleaves versican,9 was decreased in Wave valves (Figure 4). Thus, increases in in tact versican and decreases in cleaved versican are consistent with increased levels of total proteoglycan in Wave valves, shown in Figure 1J–1L. Preliminary studies in a few mice suggest that levels of biglycan, another proteoglycan, were normal in Wave mice (Figure I in the online-only Data Supplement). Expression of ADAMTS1, another proteoglycanolytic enzyme,11 was normal in Wave valves (Figure 4). Thus, changes in versican versus biglycan suggest that changes in proteoglycans homeostasis in the aortic valve are selective for specific proteoglycan moieties. Figure 4. Proteoglycan homeostasis in aortic valve. Histological data were obtained at 6 months of age (N=4). Red stain=intact versican or cleaved versican, respectively (arrows); to-Pro Blue stain=nuclei. Polymerase chain reaction (PCR) data were obtained at 12 months of age (N=6). Scale bar=100 μm. *P<0.05 vs untreated control. Hajj et al Aortic Regurgitation in Mice 1657 Cell Death in the Aortic Valve Expression of activated caspase-3, a marker for programmed cell death, was not increased at 1.5 months in Wave valves (Figure II in the online-only Data Supplement). However, at 6 and 12 months of age, there was a large increase in activated capase-3 levels in Wave mice compared with control mice. Increased apoptosis in Wave mice, at 6 months of age, was confirmed using terminal deoxynucleotidyl transferase dUTP nick end labeling staining (Figure III in the online-only Data Supplement). Pioglitazone prevented increases in activated caspase-3 and terminal deoxynucleotidyl transferase dUTP nick end labeling staining in Wave mice. There was no difference between sexes for any histological parameter in the aortic valve (P=NS for male versus female, data not shown). Aortic Valve Function Downloaded from http://atvb.ahajournals.org/ by guest on May 14, 2017 Representative valve function data are shown in Figure 5. A significant transvalvular gradient was observed, even when AS was not present in the Wave mouse with AR. Aortic cusp separation (ACS) was normal in Wave mice, as a group, at all ages (Figure 6A). In 3 of 55 Wave mice, however, ACS was <0.66 mm, which indicates that those 3 mice had hemodynamically important AS12 (Figure 6B; P=NS versus control for AS prevalence). M-mode echo images only right and noncoronary aortic valve cusps. To address the hypothetical possiblilty that significant stenosis occurs in the left cusp, we performed Anatomic M-mode imaging on 7 additional Wave mice and found that aortic cusp movement was symmetrical (Figure IV in the online-only Data Supplement), supporting the validity of standard M-mode measurements in the larger group of Wave mice. All 3 mice with severe AS also had severe AR with diastolic prolapse of ≥1 valve cusps into the left ventricular outflow tract (Video SV1 in the online-only Data Supplement; legend for SV1 is included in the onlineonly Data Supplement). The prevalence of moderate or severe AR, assessed using color Doppler echocardiography, was 70%, 81%, and 73% in Wave mice at 1.5, 6, and 12 months of age, respectively, and 0 in control mice (P<0.05 for all ages, Figure 6C). Aortic valve regurgitant fraction, quantitated at 6 months of age using MRI, was 0.34±0.07 for all Wave mice versus 0±0.03 for control mice (P<0.05; Figure 6D). In instances where echocardiography demonstrated moderate or severe AR, MRI confirmed abundant diastolic retrograde flow across the aortic valve (Video SV2 in the online-only Data Supplement; legend for SV2 is included in the online-only Data Supplement), and regurgitant fraction was 0.46±0.06. For all mice without echocardiographic evidence of moderate or severe AR, regurgitant fraction was 0.06±0.03 (P<0.05 versus mice with AR; Figure V in the online-only Data Supplement). Mitral regurgitation, assessed using color Doppler echocardiography, was absent or trivial in all mice. One Wave mouse, which had severe AR, also had mild pulmonic valve regurgitation observed on MRI. Despite the presence of normal ACS, there were substantial systolic pressure gradients across the aortic valve in Wave mice, assessed using invasive hemodynamic measurements (Figures 5H and 6E). The increased transvalvular gradients were associated with increased aortic pulse pressure (Figure 6F), a finding consistent with AR, and not AS. Figure 5. Aortic valve function. A–C, M-mode echocardiograms demonstrating aortic cusp separation (blue-green line). D–F, Color Doppler frames acquired in mid-diastole. Blue jet indicates regurgitant flow across the aortic valve (AoV, white arrow). G–I, Pressure measurements during catheter pullback from left ventricle to aorta, which indicate a significant pressure gradient in the Wave mouse with normal aortic cusp separation (B, E, H). AoW indicates aortic root wall; AR, aortic regurgitation; and AS, aortic stenosis. 1658 Arterioscler Thromb Vasc Biol July 2015 A B D C E Downloaded from http://atvb.ahajournals.org/ by guest on May 14, 2017 G F H µ Figure 6. Aortic valve function. A–C, Echocardiographic findings. D, MRI findings at 6 months. E and F, Invasive hemodynamic findings. G, Correlation between left ventricle (LV) stroke volume and aortic valve peak gradient. H, Lack of correlation between aortic cusp separation and peak aortic valve gradient. ACS indicates aortic cusp separation; Ao, aorta; AoV, aortic valve; AR, aortic regurgitation; AS, aortic stenosis; and LV SV, left ventricular stroke volume. *P<0.05 vs age-matched and treatment-matched control. In mice without AS, there was a remarkable quadratic relationship between left ventricular stroke volume and transvalvular systolic gradient (Figure 6G). Because the magnitude of increased LV stroke volume is determined by severity of AR, the correlation between stroke volume and systolic gradient implies that the gradient is produced by AR. Indeed, there was no correlation between ACS and transvalvular gradient (Figure 6H). Although treatment with pioglitazone prevented abnormal valve calcification, pioglitazone had no effect on ACS or prevalence of moderate or severe AR (Figure 6A and 6C). Proximal Aorta Aortic diameters measured using echocardiography at the level of the sinuses of Valsalva and at the level of the proximal ascending aorta were increased in Wave mice versus control mice at all ages (Figure VIA and VIB in the onlineonly Data Supplement). Aortic enlargement was present at 1.5 months of age in Wave mice, even when AR was absent, which suggests genotype-related abnormalities in the aortic wall. Saccular or fusiform aneurysmal dilatation of the aortic root was not observed in any mouse. Increased expression of the proinflammatory injury response mediator Smad3, a transforming growth factor-β1 response element, has been linked to increased incidence of aortic aneurysm in humans.13 We found that expression of Smad3 and also the anti-inflammatory mediator, Smad7, were not significantly increased in aorta of Wave mice (Figure VIC and VID in the online-only Data Supplement). Ventricular Size and Systolic Function There was significant LV chamber enlargement, consistent with volume overload, in Wave mice with AR at 1.5, 6, and 12 months of age (Figure 7A). After treatment with pioglitazone, LV end-diastolic volume remained elevated in Wave mice. LV stroke volume was significantly increased in Wave mice at 1.5, 6, and 12 months of age (Figure 7B). At 1.5 months of age, end-diastolic volume and stroke volume were Hajj et al Aortic Regurgitation in Mice 1659 Downloaded from http://atvb.ahajournals.org/ by guest on May 14, 2017 not increased in the 30% of Wave mice that did not have AR (P=NS versus control, data not shown). After treatment with pioglitazone, LV stroke volume remained elevated in Wave mice. LV mass, indexed to body mass, was elevated in Wave mice at 1.5, 6, and 12 months of age (Figure 7C). After treatment with pioglitazone, LV mass remained elevated in Wave mice. LV ejection fraction was normal in Wave mice at 1.5 and 6 months of age, but was significantly decreased by 12 months of age (Figure 7D). In Wave mice with AR, LV mass, LV enddiastolic volume, and LV ejection fraction were similar in males versus females at 6 months of age. By 12 months of age, there was a trend toward greater LV dilation and lower LV ejection fraction in females. The trend did not achieve statistical significance, however, possibly because of greater variance at later stages of disease (P=NS for male versus female, for each age, data not shown.) Right ventricle ejection fraction, quantitated at 6 months of age using MRI, was significantly decreased in Wave mice versus control (Figure 7E). In summary, LV volumes and mass were increased in Wave mice at all ages, including the youngest age when valve collagen, calcification, and lipid levels were normal (Figure 1). LV systolic function was normal, despite high prevalence of moderate or severe AR, at 1.5 and 6 months of age, but was abnormal at 12 months of age. Myocardial Gene Expression At 1.5 months of age, expression of fetal genes14 was not increased in myocardium of Wave mice, with the exception of brain-type natriuretic peptide (Figure VII in the online-only Data Supplement). When Wave mice with AR were analyzed separately, however, expression of skeletal muscle-type actin A Organization of Myocardial Transverse Tubules To examine structural changes in individual cardiomyocytes in this model of valvular volume overload cardiomyopathy, we focused on transverse tubules (TT). At 1.5 and 3 months of age, when Wave mice demonstrated LV hypertrophy and normal LV systolic function, TT organization was normal in Wave mice (Figure 8). At 12 months of age, when both LV hypertrophy and systolic dysfunction were present in Wave mice, TT organization was significantly disrupted. Discussion For the first time, we provide comprehensive functional, histological, and molecular characterization of spontaneous valvular volume overload cardiomyopathy in a mouse model. Aortic valve dysfunction occurs in the presence of excess proteoglycans, including versican, in valve cusps, but precedes fibrosis, calcification, apoptosis, and lipid deposition in the valve. Treatment with pioglitazone prevents abnormal calcification and apoptosis in the aortic valve in Wave mice, but does not protect aortic valve function. Over time, LV volume B C E and atrial natriuretic peptide were also increased (Figure VIII in the online-only Data Supplement). Abnormal expression of several genes persisted or progressed during the course of disease (Figure VII in the onlineonly Data Supplement). By 6 months of age, myocardial expression of β-myosin heavy chain, myocyte-enriched calcineurin-interacting protein-1.4, collagen-1, and collagen-3 was significantly increased in Wave mice. At 12 months of age, fibrosis was histologically evident in myocardium from Wave mice. There was no difference between sexes for myocardial gene expression in Wave mice (P=NS for male versus female, data not shown). D Figure 7. Ventricular structure and function. A–D, Echocardiography. For wave mice, data are shown only for mice with moderate or severe aortic regurgitation. E, RVEF, assessed by MRI, at 6 months of age. EDV indicates end-diastolic volume; EF, ejection fraction; LV, left ventricular; RV, right ventricular; and SV, stroke volume. *P<0.05 vs age-matched and treatment-matched control. 1660 Arterioscler Thromb Vasc Biol July 2015 Downloaded from http://atvb.ahajournals.org/ by guest on May 14, 2017 Figure 8. T-tubule organization in myocardium. At 1.5 months of ageand at 3 months of age, when left ventricular hypertrophy is already present in Wave mice, T-tubules are regularly spaced and oriented perpendicular to myocyte long-axes in Wave myocardium (arrow). By 12 months of age, when left ventricular systolic dysfunction occurs in Wave mice, T-tubules have become disorganized. TTpower is a statistical convention used to quantify the level of organization of T-tubules.11 Sample sizes for WT and Wave mice at the 3 ages are 3,3; 2,3; and 4,8. Ten confocal micrographs were analyzed for each mouse. Scale bar=50 μm. *P<0.05 vs control. overload is associated with increased expression of fetal myocardial genes, progressive impairment of LV systolic function, myocyte TT disruption, and myocardial fibrosis. Others have reported fibrosis, calcification, and elevated transvalvular gradients in aortic valves of Wave mice and have interpreted the results as indicative of calcific AS.7 We provide multiple lines of evidence, which indicate that AS is rare in Wave mice and that AR predominates. ACS is normal in Wave mice, as a group, at all ages. Color Doppler and 2D echocardiography clearly depict AR and increased LV stroke volume, respectively, in Wave mice. MRI demonstrates abundant retrograde diastolic flow across the aortic valve and regurgitant volumes, which confirm the presence of moderate or severe AR in Wave mice. Systolic gradients across the aortic valve, assessed using invasive hemodynamic methods, follow a predictable quadratic relationship to LV stroke volume, which indicates that increased flow across the valve, not stenosis, accounts for elevated valve gradients in the vast majority of mice. Excluding 3 of 55 Wave mice in which echocardiography identified significant AS, there was no correlation between aortic valve pressure gradients and systolic ACS. LV-to-aorta pressure gradients were higher in Wave mice than those typically observed in humans with pure AR. We speculate that this apparent disparity arises because normal LV systolic function is relatively hyperdynamic in mice (EF≈0.80) compared with humans (EF≈0.55). Our findings are unique because aortic valve fibrosis, profibrotic signaling, valve calcification, osteogenic transformation, and increased transvalvular pressure gradients are all features of acquired aortic valve stenosis in mice and humans and together are often proffered as pathognomonic evidence for the disease. Indeed the levels of fibrocalcific changes in Wave mice actually exceed those previously reported in aortic stensosis-prone mice.15 Our findings in Wave mice, however, support the conclusion that abundant valve calcification and fibrosis alone are not sufficient to cause prevalent hemodynamically important AS in mice. Others have observed, anecdotally, spontaneous AR in mice, putatively in the presence of AS.5,16,17 However, the prevalence, quantitative severity, structural mechanism, and the impact of spontaneous chronic AR on ventricular morphology, function, myocyte structure, and gene expression have not previously been reported. Mechanisms of Valve Dysfunction In the present study, we identify myxomatous structural incompetence and consequent diastolic prolapse of valve cusps as major mechanisms of AR in Wave mice. Those findings are common in humans with isolated AR.18 Deficiency of proteoglycan breakdown occurs postnatally in Wave mice, a novel finding of the present study. Despite significant increases in polymeric intact versican, levels of Hajj et al Aortic Regurgitation in Mice 1661 cleaved versican are reduced in Wave mice at 6 months of age. Expression of ADAMTS5, an enzyme known to cleave versican,9 was reduced in Wave mice. Expression of the gene encoding versican core protein was not increased, further supporting a post-transcriptional mechanism for proteoglycan excess in Wave valves. Preliminary findings indicate that biglycan, another valve proteoglycan, was not increased in Wave valves. Together, the findings indicate that proteoglycan remodeling is selectively dysregulated in postnatal Wave mice. The findings may have translational implications because the presence of postnatal proteoglycan dysregulation suggests a potential therapeutic target. Lipid Deposition Downloaded from http://atvb.ahajournals.org/ by guest on May 14, 2017 Prior studies have demonstrated electrostatic affinity of tissue proteoglycans for circulating lipoprotein particles, a putative early stage of atherosclerotic lesion formation.19 We speculate that the persistent excess of proteoglycans in the aortic valve in Wave mice may bind blood pool lipoprotein particles by similar interactions, resulting in lipid deposition in Wave valves. That speculation is supported by the observation that lipid deposition was almost exclusively observed in Wave aortic valve cusps and their attachment sites, where proteoglycans are abundant, but not in valve annulus or myocardium (Figure 1H). The finding may have clinical relevance because lipid deposition is an early finding in humans with aortic valve disease.20 Valvular Cardiomyopathy in Wave Mice Changes in LV morphology and function, paired with changes in myocardial gene expression and TT organization, reflect a longitudinal pattern of adaptation, then decompensation, in the presence of volume overload in Wave mice. In rats with traumatic acute AR, increased expression of some fetal genes and collagen isoforms occurs early and persists essentially unchanged for months.21 Our findings in Wave mice with spontaneous chronic AR differ somewhat in that increased expression of fetal genes is progressive over 12 months, and myocardial expression of collagen-1,3 is normal during the early period of LV compensation in the presence of volume overload. Our findings thus dissociate upregulation of myocardial collagen isoform expression from volume overload per se, a novel finding. Cardiomyocyte TT critically regulate excitation–contraction coupling by facilitating Ca2+ release from sarcoplasmic reticulum. TT disruption exacerbates disease progression from hypertrophy to heart failure.22 Strategies designed to inhibit or reverse the process of TT disruption can attenuate the transition to left ventricular systolic dysfunction.23 In experimental left ventricular pressure-overload hypertrophy, TT disruption occurs before the onset of LV systolic dysfunction,22 suggesting that TT disruption is an inherent component of myocyte remodeling in response to hemodynamic stress. In Wave mice, however, TT organization was preserved in the presence of volume-overload hypertrophy for a period of at least 3 months and did not become disrupted until the development of contractile dysfunction. Wave mice at 1.5 and 3 months of age demonstrated similar severity of LV hypertrophy (≈50%) to that reported previously in pressure-overload.22 Thus, we report a new finding with fundamental mechanistic importance: unlike pressure-overload LV hypertrophy, TT disruption is not an inherent feature of left ventricular hypertrophy induced by volume overload hemodynamic stress, but occurs during the transition to heart failure in Wave mice with AR. Future studies, using techniques which overcome the limited resolution of light microscopy,24 may reveal disturbances within individual TT that occur in volume-overload left ventricular hypertrophy and heart failure. EGFR-tk signaling is trophic for LV myocardium, as overexpression produces cardiomyocyte enlargement and increased LV mass,25 whereas EGFR-tk deficiency results in LV wall thinning and decreased contractility.26 EGFR-tk activity is decreased ≈90% in Wave mice. We found neither wall thinning nor impaired LV contractility in young Wave mice. The findings indicate that residual EGFR-tk activity in Wave mice is sufficient to prevent overt cardiomyopathy in the absence of volume overload. Our findings of LV hypertrophy in Wave mice at all ages, and preserved LV contractility until older age, argue strongly against a predominant effect of myocardial Wave genotype. Nevertheless, EGFR deficiency may modulate some aspects of LV responses to volume overload, possibly blunting the hypertrophic response. Limitations The most obvious histological abnormality in young Wave mice is overabundance of proteoglycan in valve tissue, a finding which is common in patients with AR. We provide evidence for temporal association between proteoglycan excess and valve dysfunction, but cannot conclusively determine whether this association indicates causality or is an epiphenomenon arising from other, as yet uncharacterized, abnormalities of valve matrix. A previous study indicated that valve abnormalities ascribed to EGFR-tk deficiency, including proteoglycan overabundance, are strongly influenced by background strain in mice,7 suggesting the possibility of modifiers of valve homeostasis that could serve as therapeutic targets. Conclusions There are several novel findings in this study which challenge current paradigms of fibrocalcific aortic valve disease. Valve fibrosis, calcification, lipid accumulation, and apoptosis are common features of AS in humans and mice and are putative targets for therapeutic intervention. Here we report that, even when those features are present, AS is uncommon in Wave mice, ≤12 months of age. Treatment with pioglitazone prevented valve calcification in Wave mice, but did not protect valve function, confirming further the dissociation between valve calcification and valve function. We speculate that fibrocalcific changes in the aortic valve reflect a response to injury arising from mechanical stresses on structurally incompetent valve cusps. Our findings reinforce the importance of comprehensive characterization of aortic valve function in vivo, when assessing the therapeutic efficacy of interventions designed to protect or improve valve function. Because phenotypic mechanisms of AR in Wave mice resemble those observed frequently in humans, a targeted search for abnormalities of EGFR-tk signaling in humans with isolated AR may be warranted. 1662 Arterioscler Thromb Vasc Biol July 2015 Acknowledgments We thank Stephanie Troyer, Wendy Meyers, and Teresa Ruggle for assistance with preparation of the article, the University of Iowa Central Microscopy Research Facility for use of equipment, Katherine S. Walters for assistance with microscopy, and Thomas Gerhold for assistance with the mouse colony. We also thank Loretha Myers and Jennifer Habashi, Johns Hopkins University School of Medicine, for helpful suggestions regarding p-Smad2 immunostaining. Sources of Funding These studies were supported by grants HL62984, HL090905, ODO019941, and RR 026293 from the National Institutes of Health. Disclosures None. References Downloaded from http://atvb.ahajournals.org/ by guest on May 14, 2017 1. Carabello BA. Introduction to aortic stenosis. Circ Res. 2013;113:179– 185. doi: 10.1161/CIRCRESAHA.113.300156. 2.Lindman BR, Bonow RO, Otto CM. Current management of calcific aortic stenosis. Circ Res. 2013;113:223–237. doi: 10.1161/ CIRCRESAHA.111.300084. 3.Weiss RM, Miller JD, Heistad DD. Fibrocalcific aortic valve disease: opportunity to understand disease mechanisms using mouse models. Circ Res. 2013;113:209–222. doi: 10.1161/CIRCRESAHA.113.300153. 4.Houser SR, Margulies KB, Murphy AM, Spinale FG, Francis GS, Prabhu SD, Rockman HA, Kass DA, Molkentin JD, Sussman MA, Koch WJ, Koch W; American Heart Association Council on Basic Cardiovascular Sciences, Council on Clinical Cardiology, and Council on Functional Genomics and Translational Biology. Animal models of heart failure: a scientific statement from the American Heart Association. Circ Res. 2012;111:131–150. doi: 10.1161/ RES.0b013e3182582523. 5. Chen B, Bronson RT, Klaman LD, Hampton TG, Wang JF, Green PJ, Magnuson T, Douglas PS, Morgan JP, Neel BG. Mice mutant for Egfr and Shp2 have defective cardiac semilunar valvulogenesis. Nat Genet. 2000;24:296–299. doi: 10.1038/73528. 6. Luetteke NC, Phillips HK, Qiu TH, Copeland NG, Earp HS, Jenkins NA, Lee DC. The mouse waved-2 phenotype results from a point mutation in the EGF receptor tyrosine kinase. Genes Dev. 1994;8:399–413. 7. Barrick CJ, Roberts RB, Rojas M, Rajamannan NM, Suitt CB, O’Brien KD, Smyth SS, Threadgill DW. Reduced EGFR causes abnormal valvular differentiation leading to calcific aortic stenosis and left ventricular hypertrophy in C57BL/6J but not 129S1/SvImJ mice. Am J Physiol Heart Circ Physiol. 2009;297:H65–H75. doi: 10.1152/ajpheart.00866.2008. 8. Chu Y, Lund DD, Weiss RM, Brooks RM, Doshi H, Hajj GP, Sigmund CD, Heistad DD. Pioglitazone attenuates valvular calcification induced by hypercholesterolemia. Arterioscler Thromb Vasc Biol. 2013;33:523–532. doi: 10.1161/ATVBAHA.112.300794. 9. Dupuis LE, Osinska H, Weinstein MB, Hinton RB, Kern CB. Insufficient versican cleavage and Smad2 phosphorylation results in bicuspid aortic and pulmonary valves. J Mol Cell Cardiol. 2013;60:50–59. doi: 10.1016/j. yjmcc.2013.03.010. 10.Wilson CL, Gough PJ, Chang CA, Chan CK, Frey JM, Liu Y, Braun KR, Chin MT, Wight TN, Raines EW. Endothelial deletion of ADAM17 in mice results in defective remodeling of the semilunar valves and cardiac dysfunction in adults. Mech Dev. 2013;130:272–289. doi: 10.1016/j. mod.2013.01.001. 11. Fu Y, Nagy JA, Brown LF, Shih SC, Johnson PY, Chan CK, Dvorak HF, Wight TN. Proteolytic cleavage of versican and involvement of ADAMTS-1 in VEGF-A/VPF-induced pathological angiogenesis. J Histochem Cytochem. 2011;59:463–473. doi: 10.1369/0022155411401748. 12.Weiss RM, Ohashi M, Miller JD, Young SG, Heistad DD. Calcific aortic valve stenosis in old hypercholesterolemic mice. Circulation. 2006;114:2065–2069. doi: 10.1161/CIRCULATIONAHA.106.634139. 13. van de Laar IM, Oldenburg RA, Pals G, et al. Mutations in SMAD3 cause a syndromic form of aortic aneurysms and dissections with early-onset osteoarthritis. Nat Genet. 2011;43:121–126. 14.Buttrick PM, Kaplan M, Leinwand LA, Scheuer J. Alterations in gene expression in the rat heart after chronic pathological and physiological loads. J Mol Cell Cardiol. 1994;26:61–67. doi: 10.1006/jmcc.1994.1008. 15. Miller JD, Weiss RM, Serrano KM, Brooks RM II, Berry CJ, Zimmerman K, Young SG, Heistad DD. Lowering plasma cholesterol levels halts progression of aortic valve disease in mice. Circulation. 2009;119:2693– 2701. doi: 10.1161/CIRCULATIONAHA.108.834614. 16.Aikawa E, Nahrendorf M, Sosnovik D, Lok VM, Jaffer FA, Aikawa M, Weissleder R. Multimodality molecular imaging identifies proteolytic and osteogenic activities in early aortic valve disease. Circulation. 2007;115:377–386. doi: 10.1161/CIRCULATIONAHA.106.654913. 17. Kokubo H, Miyagawa-Tomita S, Nakashima Y, Kume T, Yoshizumi M, Nakanishi T, Saga Y. Hesr2 knockout mice develop aortic valve disease with advancing age. Arterioscler Thromb Vasc Biol. 2013;33:e84–e92. doi: 10.1161/ATVBAHA.112.300573. 18. Boodhwani M, de Kerchove L, Watremez C, Glineur D, Vanoverschelde JL, Noirhomme P, El Khoury G. Assessment and repair of aortic valve cusp prolapse: implications for valve-sparing procedures. J Thorac Cardiovasc Surg. 2011;141:917–925. doi: 10.1016/j.jtcvs.2010.12.006. 19. Grande-Allen KJ, Osman N, Ballinger ML, Dadlani H, Marasco S, Little PJ. Glycosaminoglycan synthesis and structure as targets for the prevention of calcific aortic valve disease. Cardiovasc Res. 2007;76:19–28. doi: 10.1016/j.cardiores.2007.05.014. 20. Freeman RV, Otto CM. Spectrum of calcific aortic valve disease: pathogenesis, disease progression, and treatment strategies. Circulation. 2005;111:3316–3326. doi: 10.1161/CIRCULATIONAHA.104.486738. 21. Champetier S, Bojmehrani A, Beaudoin J, Lachance D, Plante E, Roussel E, Couet J, Arsenault M. Gene profiling of left ventricle eccentric hypertrophy in aortic regurgitation in rats: rationale for targeting the beta-adrenergic and renin-angiotensin systems. Am J Physiol Heart Circ Physiol. 2009;296:H669–H677. doi: 10.1152/ajpheart.01046.2008. 22.Guo A, Zhang C, Wei S, Chen B, Song LS. Emerging mechanisms of T-tubule remodelling in heart failure. Cardiovasc Res. 2013;98:204–215. doi: 10.1093/cvr/cvt020. 23. Guo A, Zhang X, Iyer VR, Chen B, Zhang C, Kutschke WJ, Weiss RM, Franzini-Armstrong C, Song LS. Overexpression of junctophilin-2 does not enhance baseline function but attenuates heart failure development after cardiac stress. Proc Natl Acad Sci U S A. 2014;111:12240–12245. doi: 10.1073/pnas.1412729111. 24.Ibrahim M, Navaratnarajah M, Siedlecka U, Rao C, Dias P, Moshkov AV, Gorelik J, Yacoub MH, Terracciano CM. Mechanical unloading reverses transverse tubule remodelling and normalizes local Ca(2+)induced Ca(2+)release in a rodent model of heart failure. Eur J Heart Fail. 2012;14:571–580. doi: 10.1093/eurjhf/hfs038. 25. Sysa-Shah P, Xu Y, Guo X, Belmonte F, Kang B, Bedja D, Pin S, Tsuchiya N, Gabrielson K. Cardiac-specific over-expression of epidermal growth factor receptor 2 (ErbB2) induces pro-survival pathways and hypertrophic cardiomyopathy in mice. PLoS One. 2012;7:e42805. doi: 10.1371/journal.pone.0042805. 26. Crone SA, Zhao YY, Fan L, Gu Y, Minamisawa S, Liu Y, Peterson KL, Chen J, Kahn R, Condorelli G, Ross J Jr, Chien KR, Lee KF. ErbB2 is essential in the prevention of dilated cardiomyopathy. Nat Med. 2002;8:459–465. doi: 10.1038/nm0502-459. Significance We provide the first comprehensive functional, histological, and molecular characterization of spontaneous valvular volume overload cardiomyopathy in a clinically relevant mouse model. Valve dysfunction is mechanistically dissociated from profound fibrocalcific changes in the aortic valve in Wave mice. Cardiomyocyte remodeling in this model of volume-overload left ventricular hypertrophy differs fundamentally from previously observed remodeling in pressure-overload hypertrophy.The findings reinforce the importance of comprehensive characterization of aortic valve function in vivo when assessing the therapeutic efficacy of interventions designed to ameliorate fibrocalcific changes in the aortic valve. Downloaded from http://atvb.ahajournals.org/ by guest on May 14, 2017 Spontaneous Aortic Regurgitation and Valvular Cardiomyopathy in Mice Georges P. Hajj, Yi Chu, Donald D. Lund, Jason A. Magida, Nathan D. Funk, Robert M. Brooks, Gary L. Baumbach, Kathy A. Zimmerman, Melissa K. Davis, Ramzi N. El Accaoui, Tariq Hameed, Hardik Doshi, BiYi Chen, Leslie A. Leinwand, Long-Sheng Song, Donald D. Heistad and Robert M. Weiss Arterioscler Thromb Vasc Biol. 2015;35:1653-1662; originally published online May 21, 2015; doi: 10.1161/ATVBAHA.115.305729 Arteriosclerosis, Thrombosis, and Vascular Biology is published by the American Heart Association, 7272 Greenville Avenue, Dallas, TX 75231 Copyright © 2015 American Heart Association, Inc. All rights reserved. Print ISSN: 1079-5642. Online ISSN: 1524-4636 The online version of this article, along with updated information and services, is located on the World Wide Web at: http://atvb.ahajournals.org/content/35/7/1653 Data Supplement (unedited) at: http://atvb.ahajournals.org/content/suppl/2015/05/21/ATVBAHA.115.305729.DC1 Permissions: Requests for permissions to reproduce figures, tables, or portions of articles originally published in Arteriosclerosis, Thrombosis, and Vascular Biology can be obtained via RightsLink, a service of the Copyright Clearance Center, not the Editorial Office. Once the online version of the published article for which permission is being requested is located, click Request Permissions in the middle column of the Web page under Services. Further information about this process is available in the Permissions and Rights Question and Answer document. Reprints: Information about reprints can be found online at: http://www.lww.com/reprints Subscriptions: Information about subscribing to Arteriosclerosis, Thrombosis, and Vascular Biology is online at: http://atvb.ahajournals.org//subscriptions/ Supplemental Table I. Blood Chemistry and Body Mass. Tchol (mg/dl) Ca++ (mg/dl) Phosphorus (mg/dl) Body Mass(g) 1.5 month Control 73 ± 7 9.2 ± 0.1 7.7 + 0.4 20 + 1 Wave 73 ± 3 9.2 ± 0.2 7.3 + 0.3 18 + 1 Control 55 ± 4 6.1 ± 0.1 9.5 ± 0.5 28 + 1 Wave 66 ± 6 6.1 ± 0.1 9.9 ± 1.1 26 + 1 Control 59 ± 8 6.4 ± 0.1 8.1 ± 0.2 33 + 2 Wave 61 ±12 6.4 ± 0.1 9.1 ± 0.7 30 + 2 Control 56 ± 4 6.1 ± 0.1 NM 34 + 2 Wave 73 ± 7 6.1 ± 0.1 NM 32 + 1 6 month 6 month + pio 12 month N = 3 for 1.5 month-old, 9 or 10 for 6 month-old, 3 or 4 for Pio-treated, and 7 or 12 month-old Control and Wave mice, respectively. Tchol total cholesterol, Ca++ calcium, NM not measured. p = NS for Wave vs. Control for all values. Wave Biglycan Immunofluorescence * % Positive Staining Control N= 2 3 3 4 Supplemental Figure I. Biglycan in aortic valve. Histologic data were obtained at 6 months of age. Red stain = biglycan immunofluorescence; to-Pro Blue stain = nuclei. Scale bar = 100 μm. *p < 0.05 vs. Control. Control Wave * Activated Caspase-3 20 * ** 0 Age (mo.) N= 1.5 6 8,12 9,12 6+Pio 3,4 12 11,7 Supplemental Figure II. Immunostaining for the pro-apoptotic marker activated caspase-3 in the aortic valve. *p < 0.05 vs. age-matched Control; **p < 0.025 vs. 6 mo Wave. Scale bar = 100 μm. Wave Control Apoptosis Supplemental Figure III. Valve cell turnover. Total valve tissue area, summed over three histologic slides from analogous anatomic locations in each of 4 mice per group, was about twofold higher in Wave vs. Control. Cell density was not different between Wave and Control. Apoptosis (TUNEL, arrow, red staining) was significantly increased in Wave vs. Control. Mitosis (immunostaining for pHH3, red) was present in < 0.1% of valve cells in all samples analyzed ( p = NS, group data not shown). Mitosis was abundant in the positive control sample from spleen. Data are shown for mice at 6 months of age. *p < 0.05 vs. Control. **p < 0.025 vs. Wave. Scale bar = 100 μm. Positive Control Mitosis * 0.3 6000 3000 0 Control Wave TUNEL Positive Nuclei (%) Total Nuclei/mm2) * % Positive Nuclei Valve Tissue Area (mm2) 0 12 6 ** 0 Control Wave Control Control + Pio Wave Wave + Pio Supplemental Figure IV. Symmetry of systolic aortic valve cusp separation. A: schematic of standard M-mode and Anatomical M-mode imaging of the aortic valve. B: representative images from a single Wave mouse. C: R-NC vs. L-NC cusp separation in a group of Wave mice (N = 7). D: L-NC cusp separation is normal in Wave mice, but is reduced in aortic stenosis-prone Reversa mice16 (N = 5). E: agreement between L-NC separation and R-NC separation in individual mice. LV left ventricle, Ao aorta, R right cusp, L left cusp, NC noncoronary cusp, *p < 0.05 vs. Control. Regurgitant Fraction (MRI) * 0.4 0.2 0 < Mild Mod-Severe Aortic Regurgitation Score (Echo) Supplemental Figure V. Aortic regurgitation assessed by MRI and echocardiography. < Mild, N = 18; Moderate or Severe, N = 8. Data were obtained at 6 and 12 mo. of age. *p < 0.05 vs. < Mild. A. Sinus of Valsalva (mm) * * B. Ascending Aorta (mm) * * * * Age (mo.) N= C. 14 6 0 8 27 27 5 20 11 Age (mo.) D. Smad3 mRNA in Aorta 1 Smad7 mRNA in Aorta 1.5 1 0.5 0.5 0 0 Control Wave Con Pio Wave Pio Control Wave Con Pio Wave Pio Supplemental Figure VI. Aorta. A,B: aortic dimensions, assessed by echocardiography. N = 14, 27, 7, 11 for 1.5 mo., 6 mo., Wave + Pio, and 12 mo., respectively. C,D: Smad3 or Smad7 expression as a fraction of Control (Con), in aortas from mice at 6 months of age (N = 6 each). Pio pioglitazone-treated; *p < 0.05 vs. age-matched and treatment-matched Control. MCIP-1.4 C W Supplemental Figure VII. Gene expression and collagen in myocardium. Sk skeletal muscle isoform, ANP atrial natriuretic peptide, BNP brain-type natriuretic β-MyHC beta-myosin heavy chain, Col collagen, MCIP myocytepeptide, enriched calcineurin-interacting protein-1.4. Expression levels are normalized to values for Control mice at each age; N = 7 – 11 for each group. C Masson’s Trichrome staining for collagen in Control myocardium at age 12 mo., W Masson’s Trichrome staining for collagen in Wave myocardium at age 12 mo. Calibration bar = 100µm. *p < 0.05 vs. Control. † p < 0.05 vs. Wave at 1.5 mo. * N= 7 4 * 7 Supplemental Figure VIII. Effects of genotype and aortic regurgitation (AR) upon myocardial gene expression at 1.5 months of age. *p < 0.05 vs. Control. AoV LV Ao SoV LA Key to Supplemental Video SV1. Parasternal long-axis 2D echocardiogram in mid-diastole from a Wave mouse with a myxomatous aortic valve (AoV, red arrows) and cusp prolapse (white arrows). The movie also shows restricted systolic motion of the aortic valve. LV left ventricle, LA left atrium, SoV sinus of Valsalva, Ao proximal ascending aorta. Ao RA LA RV LV PM Key to Supplemental Video SV2. Middiastole cine-MRI frame from a Wave mouse, showing severe aortic regurgitation (arrows). Ao aorta, LV left ventricle, RV right ventricle, LA left atrium, RA right atrium, PM papillary muscle. ATVB/2015/305729DR1 Final 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 32 33 34 35 36 37 38 39 40 41 42 43 44 45 46 47 48 49 50 51 Materials and Methods All studies were approved by the Institutional Animal Care and Use Committee at the University of Iowa (PHS Animal Welfare Assurance #A3021-01). Experimental strategy. EgfrWa2/+ (Control) and littermate EgfrWa2/Wa2 (Wave) mice bred on a C57/BL6 background were maintained on normal chow diet (Harlan Teklad 7004 Rodent Diet). Echocardiograms were performed on surviving mice at 1.5, 6, and 12 months of age. Cardiac magnetic resonance imaging (MRI) was performed on a subset of mice from each group at 6 months of age. Cardiac catheterization was performed on subsets of mice from each group at 6 or 12 months of age. Following completion of imaging and catheterization studies, mice were euthanized (pentobarbital, 150 mg/kg intraperitoneal injection), at age 1.5, 6, or 12 months, and tissue was collected for subsequent histological analysis. Pharmacologic intervention. In a previous study, we found that administration of the PPAR-γ agonist pioglitazone attenuated aortic valve calcification and protected aortic valve function in hypercholesterolemic mice.1 We hypothesized that pioglitazone would attenuate aortic valve calcification and protect valve function in normocholesterolemic Wave mice. Therefore, 16 mice (7 Control and 9 Wave mice) were treated with pioglitazone (20 mg/kg per day in chow) from 1 to 6 months of age, then euthanized. Echocardiography. Midazolam (0.15 mg, subcutaneous) was used to produce light conscious sedation. Parasternal long- and short-axis views were obtained using high-frequency echocardiography (Vevo 2100®, VisualSonics, Toronto, Canada) to assess aortic valve function and aortic root dimensions. LV mass, volumes, and systolic function were assessed using the bi-plane area-length method, previously validated in our laboratory.2 M-mode images were then acquired in order to measure systolic aortic valve orifice dimension as previously described.3 Anatomical M-mode imaging was accomplished by redirection of the cursor superimposed on a short-axis 2D image of the aortic valve, as shown in Supplemental Figure IV. Color Doppler was used in a parasternal long-axis plane to determine the presence of aortic regurgitation. Echocardiographic severity of AR was graded by measuring length of the maximum diastolic regurgitant jet, and dividing by the end-diastolic long-axis length of the LV. Trace or mild AR was recorded when jet length was < 25% of LV length, moderate: 25 – 50%, severe: > 50%. Cardiac MRI. Mice were deeply sedated with midazolam (8 mg/kg, subcutaneous) and morphine (4 mg/kg, subcutaneous), a regimen that produces only modest depression of heart rate and left ventricular contractility, and MRI was performed using an Innova® 4.7T instrument (Varian, Palo Alto, CA) as described previously.4 The presence and qualitative severity of aortic regurgitation were assessed by observing dephasing of the blood signal in the left ventricular outflow tract during early diastole. Regurgitant fraction was then calculated as the difference between left and right ventricular (RV) stroke volumes divided by LV stroke volume. Invasive hemodynamic measurements. Immediately prior to euthanasia, the peak aortic valve gradient was measured. Mice were anesthetized using ketamine/acepromazine (87.5/12.5 mg/kg, intraperitoneal). A 1.4F microtransducer-tipped catheter (Millar, Houston, TX) was inserted into the right common carotid artery and advanced retrograde into the LV. Pressure was then continuously recorded as the catheter tip was pulled back into the ascending aorta. Aortic valve peak systolic gradient was calculated as the difference between peak LV pressure and peak aortic pressure. Aortic pulse pressure was calculated as the difference between systolic and diastolic aortic pressures. Valve histology. Tissue was frozen in optimal cutting temperature compound (OCT, 10.24% polyvinyl alcohol 4.26% polyethylene glycol 85.5% non-reactive ingredients). Sections, 10-microns thick, were obtained from proximal, mid, and distal aortic valve from each mouse. Slides were stained with Alizarin Red, Masson’s Trichrome or Picrosirius Red, or Oil Red-O to quantitate the amount of calcium, collagen and lipid, respectively, as described previously.1 Movat’s pentachrome stain was used to quantitate proteoglycan content in the aortic valve. ATVB/2015/305729DR1 Final 52 53 54 55 56 57 58 59 60 61 62 63 64 65 66 67 68 69 70 71 72 73 74 75 76 77 78 79 80 81 82 83 84 85 86 87 88 89 90 91 92 93 94 95 96 97 98 99 100 101 102 Immunofluorescence was used to quantitate levels of α-SMA, TGF-β1, p-Smad2, osterix, osteocalcin, intact versican, cleaved versican, biglycan, p-HH3, and activated caspase3. The method for discriminating between true immunofluorescence in the valve vs. autofluorescence in the valve annulus is shown in Supplemental Materials and Methods Figure IB below. Confirmatory quantitation of apoptosis in the aortic valve was performed using terminal deoxynucleotidyl transferase dUTP nick end labeling (TUNEL, In Situ Cell Death detection Kit®, Roche). The percentage of valve exhibiting positive staining was reported as “% positive”. Gene expression in aortic valve and proximal aorta. Aortic roots from individual mice (6 Control mice and 6 Wave mice, at 12 + 1 months of age) were frozen in OCT, after which the aortic valve was dissected free from supporting structures, under microscopic guidance, and transferred to Trizol reagent. RNA was prepared using RNeasy mini kit (Qiagen). Complementary DNA was generated using MMLV reverse transcriptase with random hexamers. ADAMTS1, ADAMTS5, biglycan, and versican mRNA levels were each measured in a well along with a β-actin reference standard, using qRT-PCR FAM and VIC fluors, respectively (TaqMan®, Integrated DNA Technologies, Coralville, IA). RNA from the ascending aorta was isolated at 6 months of age with Trizol reagent, followed by separation with RNeasy minicolumn(Quiagen). Smad3 and Smad7 mRNA levels were measured as described above. Sources for primers are shown in Supplemental Materials and Methods Table 1 below. Myocardial gene expression. RNA was isolated with Trizol reagent from the left ventricle of 7-11 mice, and cDNA was generated using Superscript-III reverse transcriptase and random hexamers. Transcript levels were measured with SYBR Green and Bio-Rad CFX96 Real-Time system. Expression of genes of interest was normalized to 18S rRNA. The primer sequences utilized to interrogate myocardial gene expression are shown in Supplemental Materials and Methods Table 2 below. T-tubule imaging in myocardium. The structure and organization of cardiomyocyte ttubules were assessed using methods previously described in rats.5 Briefly, whole hearts were removed, then perfused retrograde at room temperature for 30 minutes with Ca2+-free Tyrode’s solution via Langendorff apparatus. The membrane-binding lipophilic marker, MM 4-64 (AAT BioQuest, CA) was added to perfusate for 30 minutes. T-tubules were imaged in intact hearts using a confocal microscope (LSM 510, Zeiss, Germany) at 63x magnification. Left ventricular T-tubule organization was reported as TTpower, in each of 10 confocal micrographs from each mouse, using software designed for this purpose.5 Lower values for TTpower indicate disruption of T-tubule organization. Blood chemistries. Total plasma cholesterol and inorganic phosphorus were measured with a spectrophotometer using the reagent sets (C7510 and P7516, respectively, Pointe Scientific, Inc., Canton, MI). Plasma calcium was determined spectrophotomically using C503 reagent set (Teco Diagnostics, Anaheim, CA). Statistical analysis. All continuous variables are reported as mean ± standard error. Group data for continuous variables were compared between Wave vs. age-matched Control mice, using Student’s t-test. Presence or absence of a discrete condition (severe aortic stenosis or moderate/severe AR) was compared between groups using z-testing.6 Data reporting the effect of pioglitazone treatment upon valve calcification, where N < 4, were first subject to Mann-Whitney Rank Sum testing in order to confirm that data conformed sufficiently to a normal distribution.6 Statistical significance was set at p < 0.05, except where a group of data were utilized in two discrete comparison, in which case Bonferroni correction was utilized to set statistical significance at p < 0.025. ATVB/2015/305729DR1 Final 103 104 105 106 107 108 109 110 111 112 113 114 115 116 117 118 119 120 121 122 123 124 125 126 127 128 129 130 131 132 133 134 135 136 137 138 139 140 141 142 143 144 145 146 147 148 149 150 151 152 References 1. Chu Y, Lund DD, Weiss RM, Brooks RM, Doshi H, Hajj GP, Sigmund CD, Heistad DD. Pioglitazone attenuates valvular calcification induced by hypercholesterolemia. Arterioscler Thromb Vasc Biol. 2013;33:523-532. 2. Hill, J.A., Mohsen, K, Kutschke, W., Davisson,R., Zimmerman, K., Wang, Z., Kerber, R.E., and Weiss, R.M.: Cardiac hypertrophy is not a required compensatory response to short-term pressure overload. Circulation. 2000;101:2854-2862. 3. Weiss RM, Lund DD, Chu Y, Brooks RM, Zimmerman KA, Accaoui RE, Davis MK, Hajj GP, Zimmerman MB, Heistad DD. Osteoprotegerin inhibits aortic valve calcification and preserves valve function in hypercholesterolemic mice. PloS One. 2013;8:e65201. 4. Berry CJ, Thedens DR, Light-McGroary K, Miller JD, Kutschke W, Zimmerman KA, Weiss RM. Effects of deep sedation or general anesthesia on cardiac function in mice undergoing cardiovascular magnetic resonance. J Cardiovasc Magnet Reson. 2009;11:16. 5. Wei S, Guo A, Chen B, Kutschke W, Xie YP, Zimmerman K, Weiss RM, Anderson ME, Cheng H, Song LS. T-tubule remodeling during transition from hypertrophy to heart failure. Circ Res. 2010;107:520-31. 6. Glantz SA. Primer of Biostatistics. 2012; McGraw-Hill, New York. ATVB/2015/305729DR1 Final 153 154 155 Methods and Materials Table 1. Primers and probes for assessment of gene expression in the aortic valve and proximal aorta. 156 Gene TaqMan Primers/probe 157 ADAMTS1 Mm.PT.58.29991678/FAM Integrated DNA Technologies* 158 ADAMTS5 Mm.PT.58.28649059/FAM Integrated DNA Technologies 159 Biglycan Mm.PT.58.6381330/FAM 160 Versican Mm.PT.58.13796540/FAM Integrated DNA Technologies 161 Smad3 Mm.PT.56a.10139890/FAM Integrated DNA Technologies 162 Smad7 Mm.PT.56a.6640883/FAM Integrated DNA Technologies 163 Beta-actin 4352341E/VIC Applied Biosystems** 164 GAPDH 4352339E/VIC Applied Biosystems 165 166 167 168 169 170 171 172 173 174 175 176 177 178 179 180 181 182 183 Source Integrated DNA Technologies *Coralville, IA; **Carlsbad, CA ATVB/2015/305729DR1 Final 184 Materials and Methods Table 2. Primer sequences for myocardial gene expression. 185 (18S-fwd) CTTTCGCTCTGGTCCGTCTT; (18S-rev) CTTTCGCTCTGGTCCGTCTT, 186 (α-MyHC-fwd) CCTGTCCAGCAGAAAGAGC, 187 (α-MyHC-rev)CAGGCAAAGTCAAGCATTCATATTTATTGTG, 188 (β-MyHC-fwd) CAGGACACCAGCGCCCA, 189 (bMyHC-rev) CCCTTGGAGCTGGGTAGCAC, 190 (Anp-fwd) AGGAGAAGATGCCGGTAGAAGA, 191 (Anp-rev) GCTTCCTCAGTCTGCTCACTCA, 192 (Bnp-fwd) AAGGTGCTGTCCCAGATG, 193 (Bnp-rev) TTGGTCCTTCAAGAGCTGTC, 194 (Sk actin-fwd) CGACATCAGGAAGGACCTGTATGCC, 195 (Sk actin-rev) AGCCTCGTCGTACTCCTGCTTGG, 196 (Mcip1.4-fwd) AGCTCCCTGATTGCTTGTGT, 197 (Mcip1.4-rev) TGGAAGGTGGTGTCCTTGT, 198 (Col1a1-fwd) AATGGCACGGCTGTGTGCGA, 199 (Col1a1-rev) AACGGGTCCCCTTGGGCCTT, 200 (Col3a1-fwd) TGGCACAGCAGTCCAACGTA, 201 (Col3a1-rev) TGACATGGTTCTGGCTTCCA, 202 (Serca-fwd) TGTAAGTGGCCAGATTGCTC, 203 (Serca-rev) CCTAAACAACTGAAGTTAGG. 204 205