* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Post Cataract Surgery Filamentary Keratitis Abstract Text
Survey
Document related concepts
Transcript
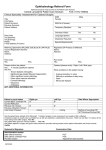
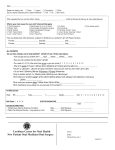
Cynthia Brown Post Cataract Surgery Filamentary Keratitis Abstract Text: Introduction: Case Report of unilateral filamentary keratitis after cataract surgery. Methods: Treatment included hourly non-preserved artificial tears with weekly follow-ups. Results: Resolved after four weeks. Conclusions: Treating dryness before ocular surgery reduces symptoms after surgery. I. Case History: Caucasian, 64 year old male. Chief complaint was an irritated left eye with foreign body sensation, redness, and photophobia. Ocular history included full time glasses wearer and cataract surgery in the left eye 4 months ago. Medical history includes hypertension, high cholesterol, chronic obstructive pulmonary disease, and sleep apnea. No current ocular medications. Systemic medications included Aspirin, Ventolin HFA, Symbicort, Atorvastatin, Furosemide, Losartan, Amlopidine, Omeprazole, Clopidogrel, Allegra, multivitamin, and Carvedilol. II. Pertinent Findings: 20/40 visual acuity OS, upper lid dermatochalasis OU, 2+ circumlimbal injection OS, watery discharge OS, 3 mucous clumps that stained with fluorescein on superior and central cornea OS, trace cells in anterior chamber OS, posterior chamber intraocular lens was clear and central OS III. Differential diagnosis: Primary-Filamentary Keratitis. Others include corneal/conjunctival foreign body, keratoconjunctivitis sicca, bacterial or viral keratoconjunctivitis, and allergic conjunctivitis. IV. Diagnosis and Discussion:Filamentary Keratitis is often caused by aqueous deficient dry eye, corneal trauma due to post-corneal surgery (refractive surgery, corneal graft, cataract surgery) or erosions, and superior limbic keratoconjunctivitis. Symptoms include foreign body sensation, watery discharge, and redness. The condition can be chronic and recurrent. It is characterized by strands or clumps of epithelial cells and mucus that are attached to the cornea. V. Treatment and Management:Treatment includes non-preserved artificial tears, filament removal, anti-inflammatory drops, mucolytic agents, punctual plugs, and bandage contact lenses. With this patient, non-preserved artificial tears were used 2-4 times per hour for the first 3 weeks of treatment and improvement in signs and symptoms was seen with every week follow up. VI. Conclusion: Patient education on the time required to treat the disorder and the chronic and reoccurring nature of this condition is important. Treating the underlying condition is neccessary for resolution and prevention of reoccurrence. Acknowledging dryness symptoms and providing pre-surgical dry eye treatment can help prevent serious dry eye symptoms after surgery.