* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Peptic Ulcer Disease
Survey
Document related concepts
Transcript
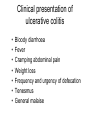
Miscellaneous Topics in Gastroenterology Waseem Hamoudi M.D Consultant Internal Medicine Gastroenterology & Hepatology • Peptic Ulcer Disease. • Inflammatory Bowel Disease. • Acute diarrhea. Peptic Ulcer Disease • Peptic ulcerations are excavated defects (holes) in the gastrointestinal mucosa that result when epithelial cells succumb to the caustic effects of acid and pepsin in the lumen. • Peptic ulcer disease commonly used term to refer to ulcerations of the stomach, duodenum, or both, that is caused by acidpeptic injury. • Histological, ulcers are necrotic mucosal defects that extend through the muscularis mucosa and into the submucosa or deeper layers. • More superficial necrotic defects are named erosions. History • In the early part of the 20th century, stress and diet were considered to be the pathogenetic factors for PUD, so treatment was with bed rest and diet. • 1950, clinicians had focused their attention on the pathogenetic role of gastric acid, so antacid therapy had become the treatment of choice. • 1970, histamine H2 receptor antagonists became available, and acid suppression with antisecretory therapy was the treatment of choice for UD. • 1980, proton pump inhibitors (PPI) were discovered, with more potent acid suppression and higher rates of ulcer healing. • Using alone antisecretory drugs, will have recurrence within one year in most patients • H. pylori was discovered in April 1982 by two Australian physicians, Dr. Barry Marshall and Dr. Robbin Warren. • In 1983 the two doctors proposed that the bacterium is the cause of peptic (duodenal and gastric) ulcers. • Dr. Marshall even went so far as to inoculate himself with the bacterium to prove his point. • it soon became apparent just how widespread and serious the H. pylori threat is. • Researches confirm that over 90 per cent of people with peptic ulcers are infected with the bacterium. • In 1987 the Sydney gastroenterologist Thomas Borody invented the first triple therapy for the treatment of duodenal ulcers. Causes • • • United Kingdome Duodenal ulcer Gastric ulcer( Benign) • • • • • Esophagitis Mallory-Weiss tear Gastroesophageal varices Gastritis or gastric erosions Tumors United states Peptic ulcer disease Gastroesophageal varices Angiomas Mallory-Weiss tear Tumors Erosions Dieulafoy's lesion Jordan (Al Bashir Hospital) • • • • • • • • • • • Duodenal ulcer Esophageal varices Erosive gastritis/duodenitis Esophagitis Gastric ulcer Gastric and duodenal ulcers Esophageal ulcer Anastomotic ulcer Mallory-Weiss tear Esophageal tumor Gastric tumor Waseem H. et al. Upper G.I Bleeding in Jordan- Retrospective statistical analysis 1996-2000 41.90% 16.07% 14.09% 8.64% 5.87% 3.60% 3.25% 2.26% 1.55% 1.41% 1.27% • Peptic Ulcer Disease. • Inflammatory Bowel Disease. • Acute diarrhea. Main types of inflammatory bowel disease (IBD) • Ulcerative colitis • Crohn’s disease Endoscopic features of ulcerative colitis (reproduced with permission, Schiller et al, 1986) Anatomical location of ulcerative colitis Intestinal complications of ulcerative colitis • • • • • • Fibrosis Shortening of the colon Bleeding Stricture Bowel perforation Toxic megacolon Systemic complications of ulcerative colitis • • • • • • • Arthritis Iritis Erythema nodosum Pyoderma gangrenosum Sclerosing cholangitis Aphthous stomatitis Thromboembolic disorders Clinical presentation of ulcerative colitis • • • • • • • Bloody diarrhoea Fever Cramping abdominal pain Weight loss Frequency and urgency of defecation Tenesmus General malaise Endoscopic appearance of Crohn’s disease (reproduced with permission, Schiller et al, 1986) Anatomical location of Crohn’s disease Clinical presentation of Crohn’s disease • • • • • • • • Diarrhoea Abdominal pain Bleeding Pyrexia Weight loss Fistulae Perianal disease General malaise Intestinal complications of Crohn’s disease • • • • • Fistulae Abscesses Adhesions Strictures Obstruction Perianal complications of Crohn’s disease Systemic complications of Crohn’s disease • Arthritis • Gallstones • Malabsorption – Lactase deficiency – Vitamin B12 deficiency • Renal stone formation Differences in clinical presentation between ulcerative colitis and Crohn’s disease Ulcerative colitis Crohn’s disease * *** *** ** * * *** * Blood *** * Mucus * ** Pus * ** Symptoms Pain General malaise Fever Diarrhoea Stools The number of * symbols indicates the frequency with which each symptom is present Pathological and anatomical features distinguishing ulcerative colitis from Crohn’s disease Ulcerative colitis Crohn’s disease Distal Segmental, proximal Always 50% of cases Normal thickness Thickened Rare Common Superficial layers All layers Superficial Deep Denuded Cobblestones Granulomas 0–4% 50–70% Lymphocytic infiltration Rare Always Fistulae Rare Common Localisation Rectum affected Intestinal wall Adhesions Inflammation Ulcerations Mucous membrane Geographical distribution of IBD (reproduced with permission, the AGA Teaching Project, 1992) Aetiological theories of IBD • • • • • • Genetic Smoking Dietary Infection Immunological Psychological? Pharmacological treatment of IBD • 5-ASA-containing compounds – mesalazine Pentasa® Asacol® Claversal®/Mesasal®/Salofalk® – sulphasalazine Salazopyrin® – olsalazine Dipentum® • Corticosteroids • Immunosuppressants Treatment: indications for surgery • • • • • Perforation Toxic dilatation Massive haemorrhage Chronic ill-health Risk of cancer • Peptic Ulcer Disease. • Inflammatory Bowel Disease. • Acute diarrhea. • Normally 10 liters enter the duodenum daily, of which 1 liter is absorbed by the small intestine. • Colon resorbs most of the remaining fluid with only 100 ml fluids lose in the stool. • Medical definition of diarrhea: a stool weight more than 250 g/day. • Practical definition: increased stool frequency more than 3 times/day or liquidity. • There are 2 types of diarrhea: acute diarrhea (less than 3 weeks) and chronic diarrhea (more than 3 weeks). Acute diarrhea • Acute diarrhea: acute onset of diarrhea and present for less than 3 weeks • Mostly caused by infectious agents, bacterial toxins (ingested preformed in food or produced in gut) and drugs. • Similar recent illness in family members suggests an infectious etiology. Non-inflammatory diarrhea • Fever absent. • Stool without blood or fecal leucocytes. • Watery stool with peri-umbilical cramps, bloating, nausea and vomiting (small bowel enteritis) caused by either a toxin or other a toxin producing toxin or other agents that disrupt the normal absorption and secretory process in the small intestine. How do we recognize noninflammatory diarrhea? By examining the absence of the leucocytes in the stool What are the causes of Noninflammatory diarrhea? • • • • Viral: Norwalk virus, Rotavirus. Protozoa: Giardia lamblia, Cryptosporidium. Bacterial: Preformed entero-toxins: Staphylococcus aureus, Bacillus cereus, and Clostridium perfringens. • Intra-intestinal enterotoxin production: E. coli (enteropathogen) and Vibrio cholera. • New medication. • Fecal impaction. Inflammatory diarrhea • Presence of fever and bloody diarrhea (dysentery) indicates colonic damage caused by invasion (shigellosis, salmonellosis, yersinia and amibiasis) or a toxin (C.difficile, E. coli 0157:H7). • Colonic diarrhea is a small amount diarrhea in volume (< 1l/day) and associated with left lower quadrant cramps, urgency and tenesmus. • Fecal leucocytes are present in infections with invasive organisms. How do we recognize inflammatory diarrhea? By examining the presence of the leucocytes in the stool What are the causes of inflammatory diarrhea? • Viral: Cytomegalovirus. • Bacterial: 1. Cytotoxin production: E. coli 0157:H7 (enterohemorhagic), Vibrio parahemolyticcus and Clostridium difficile. 2. Mucosal invasion: Shigella, Salmonella, enteroinvasive E. coli, aeromonas and Yersinia. 3.Bacterial proctitis: Chlamydia, N. gonorrhea. • Protozoa: E. histolytica. • Other: Ischemic colitis, I.B.D. and radiation colitis.