* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Adopting caries risk assessment in all practice environments
Forensic epidemiology wikipedia , lookup
Prenatal testing wikipedia , lookup
Patient safety wikipedia , lookup
Maternal health wikipedia , lookup
Race and health wikipedia , lookup
Epidemiology of metabolic syndrome wikipedia , lookup
Epidemiology wikipedia , lookup
Diseases of poverty wikipedia , lookup
Adherence (medicine) wikipedia , lookup
Focal infection theory wikipedia , lookup
Fluoride therapy wikipedia , lookup
Dentistry throughout the world wikipedia , lookup
Dental degree wikipedia , lookup
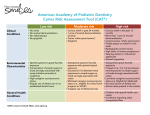
Adopting caries risk assessment in all practice environments Claire Mills, BS ¢ Piyush Patel, DDS Caries management by risk assessment (CAMBRA) is an evidence-based model intended to provide dentists with a protocol for diagnosis, treatment, and prevention of caries by assessing and addressing a patient’s overall oral health. The aim of this review was to examine the literature on CAMBRA to determine its efficacy. Clinical studies demonstrate that the CAMBRA approach is an effective concept that is both predictive of dental caries development and accurate in outlining appropriate treatment options and preventive strategies that can reduce the morbidity of this common disease process across all patient demographics. Received: March 26, 2015 Accepted: June 8, 2015 D ental caries is a complex multifactorial disease that cannot be controlled by reactive treatments such as restorations or extractions alone. Evaluating each individual’s risk for dental caries via caries risk assessment (CRA) and developing an individualized, evidence-based treatment plan allows identification of at-risk patients, thus preventing future disease.1 Clinical studies have indicated that caries management by risk assessment (CAMBRA) is both predictive of dental caries development and accurate in outlining appropriate treatment options and preventive strategies for patients of all demographics.2,3 The use of CAMBRA is not limited to general dentists; dental specialists and healthcare providers can incorporate caries management into their practices at minimal financial cost. Most patients who utilize the treatment options offered by CAMBRA will see long-term positive outcomes.3 One of the most expensive—yet preventable—healthcare problems facing the United States today is dental caries.4 Dental caries is an infectious transmissible disease process caused by a complex cariogenic biofilm, which, in the presence of a susceptible oral environment, results in demineralization and eventual cavitation of hard dental tissue.4 According to the American Dental Association Health Policy Resources Center, dental emergency department (ED) visits cost the US healthcare system approximately $2 billion annually.5 This is primarily because the number of dental patients presenting to the ED has risen greatly, from 1.1 million in 2000 to 2.1 million in 2010, which is proportionally greater than the growth of the US population.5,6 Approximately 42% of these dental ED visits were a direct result of dental caries.5 Emergency department treatment for dental caries is primarily limited to prescriptions for pain medicine and antibiotics.7 One of the main reasons cited as to why people with dental caries present at the ED is that they are either unaware of preventive measures to stop dental caries or have not implemented these practices into their lifestyle.5 Because ED treatment often does not address the actual source of caries, the disease worsens, and patients may require extensive treatment in the future. Infections requiring hospital stays and oral surgery as a consequence of untreated caries are still a common problem in hospitals (Fig 1).5,6 Caries prevalence Dental caries is a severe problem facing most people in the world. Data from the World Health Organization in 2012 revealed that 60%-90% of schoolchildren and nearly 100% of adults worldwide had dental caries.8 Additionally, 30% of adults 65-74 years of age had no teeth at all.8 This indicates a clear trend that, as people age, caries rates and cavity severity will increase, resulting in many cases that will necessitate either extraction or extensive restoration of affected teeth. 66 GENERAL DENTISTRY July/August 2016 A B Fig 1. Odontogenic infection in a 50-year-old woman who presented to a hospital in Atlanta, Georgia, with a history of recurrent pain from her mandibular right first molar. A. Panoramic radiograph at the time of presentation. B. The carious lesion associated with the first molar had progressed to an infection requiring extensive treatment and hospitalization. Data from the National Institutes of Health revealed that the percentage of people with dental caries increases from 21% of children (6-11 years) to 59% of adolescents (12-19 years) to 92% of adults (20-64 years) to 93% of seniors (65 years and older).9 The severity of dental caries also worsens as people grow older.5 The number of decayed, missing, and filled teeth (DMFT) measures, on average, how many teeth are affected by dental caries. In the United States, the DMFT per person in permanent teeth starts at 0.19 in children aged 6-11 years.9 The number then rises to 2.55 in adolescents. Young adults (20-34 years) have a DMFT of 6.16, which increases to 10.91 in older adults (35-49 years). People 50-64 years of age have a DMFT of 15.05, and those aged 65 years and older have an average DMFT of 17.96.9 Across all age groups, approximately 21.75% of people have untreated dental caries.9 Untreated dental caries never improves; it only worsens over time, causing patients severe pain and discomfort. These data illustrate not only that more people experience dental caries as they age but also that (on average) significantly more teeth are affected.9 Dental caries is also a severe problem in other developed countries. In the United Kingdom, the Child Dental Health Survey is commissioned every 10 years to determine the caries rates in children. Results from the 2013 survey indicated that 46% of 8 year olds had experienced dental caries.10 Similarly, in Norway, results from a study conducted in 2004 indicated that 12-year-old children experienced a dental caries rate of 59.8%, compared to 52.2% in the same age group in 2002.11 Data from emerging and developing countries also illustrate that dental caries is a severe health problem. Data from China in 2008 indicated that individuals aged 5-74 years had a 100% caries rate.11 In India, the caries rates were 53.8% for 12-year-old children, 80.2% for adults (35-44 years), and 85.0% for seniors (65-74 years).11 A 2006 study of Russian military personnel showed that 100% had dental caries.11 While more research is needed in these nations to accurately establish a trend between age and dental caries rate, the high percentages of those with dental caries in isolated age groups illustrates the severity of the problem in older people. The startlingly high numbers from these emerging and developing countries may illustrate a positive trend between a country’s industrialization and caries rates. As nations become developed, many people leave rural farming life for urban labor, resulting in negative changes in diet, lifestyle, and health.11 Fig 2. White-spot lesions located at the cervical aspects of the posterior teeth. Caries development A common misunderstanding in the general public regarding cavities is the assumption that dental caries and cavities are synonymous. Cavities are the end result of dental caries. Many species of bacteria contribute to dental caries, including streptococci (Streptococcus salivarius, Streptococcus sanguis, and Streptococcus sobrinus), lactobacilli (Lactobacillus acidophilus and Lactobacillus casei), and actinomycetes (Actinomyces viscosus and Actinomyces naeslundii). The dominant organisms of dental caries, however, are Streptococcus mutans (MS) and Lactobacillus acidophilus (LB), which are both acidogenic (acid producing) and aciduric (able to live in low pH environments).4 Streptococcus mutans is considered to be the most harmful bacteria in cases of dental caries, due to its ability to metabolize sucrose more effectively than other bacteria, a regulatory system that stimulates the conversion of dietary carbohydrates to acid, and its ability to survive long periods of sugar starvation.12 Streptococcus mutans metabolizes fermentable carbohydrates and creates organic acids—such as lactic, acetic, formic, and propionic acids—as by-products.4 These acids diffuse into the tooth, and, when they reach a susceptible site on a crystal surface, calcium and phosphate are dissolved into the surrounding aqueous phase. If caries is left untreated, the end result will be a cavity.4 The earliest clinical sign that dental caries is in progress is known as the white-spot lesion, a subsurface noncavitated carious lesion (Fig 2). In the initial stages, demineralization can only be seen at the electron microscopic level. As demineralization progresses, the mineral loss advances deeper into the enamel or exposed dentin until it can be detected visually, radiographically, or by other optical methods, such as laserinduced fluorescence.4 A carious lesion that is noncavitated, especially if it is in the enamel, can be reversed or arrested chemically. Remineralization is a natural repair process for white-spot lesions. Calcium and phosphate, primarily found in saliva (or other topical sources), diffuses into the tooth, and, with the help of fluoride, builds on existing crystal remnants rather than forming new crystals entirely.4 The new crystal surface, fluorapatite, is composed of a veneer of calcium, phosphate, and fluoride (dependent on the amount of fluoride present). The new layer is much more acid resistant due to a lower solubility than the original mineral.4 www.agd.org/generaldentistry 67 Adopting caries risk assessment in all practice environments This process of mineralization is cyclic; for tooth decay to occur, a combination of factors must be present: salivation levels must be insufficient, a high concentration of bacteria must be present, and the patient must be consuming a sufficient amount of carbohydrates.4,13 While cavitated lesions form over long periods of time, several disease indicators exist in order to identify whether caries disease is present. These include visible cavities, radiographic proof of dentin penetration or proximal enamel lesions, white spots on smooth enamel surfaces, and a history of placement of dental restorations in the last 3 years.13 These indicators illustrate that tooth decay either has happened or is rapidly occurring. They can also be indicative of whether future cavities will form. In addition to the aforementioned indications that the disease of caries is present, a concise list of risk factors has been identified to accurately predict whether cavities will form. These include a medium to high concentration of bacteria, visibly heavy plaque build-up on teeth, frequent snacking between daily meals, deep pits and fissures, recreational drug and/or tobacco use, hyposalivation, saliva-reducing factors (such as certain medications), exposed roots, and orthodontic appliances.14 The more risk factors a patient has, the more likely irreversible tooth decay will develop. Disease indicators •White spots •Restorations <3y •Enamel lesions •Cavities/dentin Caries progression Risk factors •Bad bacteria •Absence of saliva •Dietary habits (poor) Protective factors •Saliva and sealants •Antibacterials •Fluoride •Effective diet No caries Fig 3. The caries imbalance. (Adapted from Featherstone JD, Domejean-Orliaquet S, Jenson L, Wolff M, Young DA. Caries risk assessment in practice for age 6 through adult. J Calif Dent Assoc. 2007;35(10):703-707, 710-713.13 Reprinted with permission from the California Dental Association. Copyright © October 2007.) Caries management by risk assessment is an evidence-based model that addresses a patient’s overall oral health as opposed to a restorative/surgical model that only addresses an individual tooth. CAMBRA evaluates the presence of disease indicators and assesses the patient’s risk based on biological, behavioral, and medical history factors. Its purpose is to provide clinicians with a protocol for diagnosis, treatment, and prevention of caries, including nonsurgical means to repair tooth structure.14 After assigning patients to a risk category of low, moderate, high, or extreme risk, a clinician can provide the patient with a personalized plan to halt dental caries. category is based on criteria regarding their own biology and behavior. Ideal salivary flow should be greater than 1 mL/min. Salivary flow can be easily measured by having the patient chew gum and then collecting all saliva produced over 5 minutes in a cup. Measuring this quantity will reveal whether the patient is hyposalivating (0.07-0.99 mL/min, mild hyposalivation; less than 0.05 mL/min, severe hyposalivation).13 After the patient is assigned a risk category based on responses to the questionnaire and the clinician’s judgment, the patient can be given a personalized recommendation letter detailing treatment options. A follow-up letter can also be generated and individualized for each patient. Stock letters that detail treatment recommendations in lay language for each risk category can be made available for distribution within any practice. Assessment factors and indicators Treatment CAMBRA Figure 3 presents the CAMBRA model as a metaphorical seesaw illustrating that, for caries to progress to cavities beyond reversible repair, a clear imbalance must be struck.13 In the cases where there is a progression in caries, protective factors are insufficient, risk factors are present, and disease indicators confirm damage has been done. In order to assign patients to a risk level, a group of experts from the California Dental Association (CDA) developed CRA forms, which are subdivided into categories based on risk factors, protective factors, and disease indicators.2,14-16 These forms are commonly known as CDA CRA forms. Disease indicators automatically put the patient into a high or extreme risk category because visible dental damage can be seen. Additionally, if the patient says yes to any of the disease indicators, a bacterial culture should be taken to better evaluate risk factors.13 Simpleto-use products that can be used in-office to determine bacterial counts (MS and LB) are readily available to any practitioner. Risk evaluation forms are available from multiple sources. Figure 4 presents a CDA CRA form for patients aged 6 years and older.13 Children aged 0-5 years are assigned a risk category based on criteria related to the biology and behavior of both the mother and child.16 For patients 6 years and older, the assigned risk 68 GENERAL DENTISTRY July/August 2016 Recommended treatments for patients aged 6 years and older in each risk category are detailed in the Table.15 One strategy is the use of xylitol, a naturally occurring, diabetic-safe, low-calorie sugar that MS are unable to metabolize.17 The bacteria are unable to process xylitol, resulting in starvation similar to that which occurs when sucrose is removed from the diet. Xylitol also prevents MS from colonizing the mouth, as it inhibits attachment to teeth. Because xylitol gums and mints stimulate salivary flow, the buffering capacity and remineralization ability of saliva are drawn in as well. The consequential neutral pH environment favors nonacidogenic bacteria.17 Xylitol-containing gums, mints, candy, and cookies have been clinically shown to decrease caries, reverse carious lesions, and stop vertical transmission of bacteria from mother to child.17 To achieve positive effects, approximately 6-10 g of xylitol per day is recommended.17 Two other antibacterial solutions exist as well. Chlorhexidine (CHX) and 1% iodine treatment have been shown to reduce MS.17 Chlorhexidine attaches to bacteria over a period of 4-12 hours and works by attacking the cell walls, making it effective against a broad spectrum of microorganisms.17 However, LB counts are not affected as significantly by CHX as are MS counts.17 Alternatively, 1% iodine treatment has been Patient name:____________________________________ Chart No.:_____________________ Date:_____________________________ Assessment date:__________________________________ Is this (please check) Baseline or Recall Disease indicators (Any one Yes signifies likely “high risk” and to do a bacteria test**) Yes = Circle Yes = Circle Yes = Circle Visible cavities or radiographic penetration of the dentin Yes Radiographic approximal enamel lesions (not in dentin) Yes White spots on smooth surfaces Yes Restorations in last 3 years Yes Risk factors (biological predisposing factors) MS and LB both medium or high (by culture**) Yes Visible heavy plaque on teeth Yes Frequent snack (> 3× daily between meals) Yes Deep pits and fissures Yes Recreational drug use Yes Inadequate saliva flow by observation or measurement (**if measured, note the flow rate below) Yes Saliva-reducing factors (medications/radiation/systemic) Yes Exposed roots Yes Orthodontic appliances Yes Protective factors Lives/work/school fluoridated community Yes Fluoride toothpaste at least once daily Yes Fluoride toothpaste at least 2× daily Yes Fluoride mouthrinse (0.05% NaF) daily Yes 5000-ppm fluoride toothpaste daily Yes Fluoride varnish in last 6 months Yes Office fluoride, topical, in last 6 months Yes Chlorhexidine prescribed/used 1 week each of last 6 months Yes Xylitol gum/lozenges 4× daily last 6 months Yes Calcium and phosphate paste during last 6 months Yes Adequate saliva flow (> 1 mL/min stimulated) Yes ** Bacteria/saliva test results: MS:________ LB:_______ Flow rate:________ mL/min Date:________ Visualize caries balance (use circled indicators/factors above) Extreme risk = high risk + severe salivary gland hypofunction Caries risk assessment (please check) Extreme High Moderate Low Dentist signature:_______________________________________________________________ Date:_____________________________ Fig 4. California Dental Association Caries Risk Assessment (CDA CRA) form for ages 6 years through adulthood. LB, lactobacilli; MS, mutans streptococci; NaF, sodium fluoride. (Adapted from Featherstone JD, Domejean-Orliaquet S, Jenson L, Wolff M, Young DA. Caries risk assessment in practice for age 6 through adult. J Calif Dent Assoc. 2007;35(10):703-707, 710-713.13 Reprinted with permission from the California Dental Association. Copyright © October 2007.) used to combat gram-positive and gram-negative bacteria, fungi, mycobacteria, viruses, and protozoans. This treatment can be used effectively against MS and LB in the mouth.17 Clinical studies illustrate that a 1% iodine treatment applied topically is very effective in children, but there is limited evidence that it is effective for adults.17 Healthy patients are able to produce sufficient saliva such that remineralization of carious lesions can occur with the help of calcium and phosphate. Saliva acts protectively in that it lubricates the mouth, buffers the pH of the mouth, and acts as an antimicrobial.17 However, many adults suffer from hyposalivation and thus are unable to stop the demineralization process. www.agd.org/generaldentistry 69 Adopting caries risk assessment in all practice environments Table. Caries management by risk assessment: clinical guidelines for patients 6 years of age and older. a Risk level Frequency of radiographs Frequency of caries recall examinations Antimicrobials Saliva test (saliva flow (chlorhexidine and and bacterial culture) xylitol) Low risk Bitewing radiographs every 24-36 mo Every 6-12 mo to reevaluate caries risk May be done as a baseline reference for new patients Per saliva test if done OTC fluoridecontaining toothpaste twice daily, after breakfast and at bedtime. Optional: NaF varnish if excessive root exposure or sensitivity Moderate risk Bitewing radiographs every 18-24 mo Every 4-6 mo to reevaluate caries risk May be done as a baseline reference for new patients or if there is suspicion of high bacterial challenge and to assess efficacy and patient cooperation Per saliva test if done Xylitol (6-10 g/d) gum or candies: 2 tabs of gum or 2 candies 4 times daily OTC fluoridecontaining toothpaste twice daily plus 0.05% NaF rinse daily Initially, 1-2 applications of NaF varnish; 1 application at 4- to 6-mo recall High risk Bitewing radiographs every 6-18 mo or until no cavitated lesions are evident Every 3-4 mo to reevaluate caries risk and apply fluoride varnish Saliva flow test and bacterial culture initially and at every caries recall appointment to assess efficacy and patient cooperation Chlorhexidine gluconate, 0.12%: 10-mL rinse for 1 min daily for 1 wk each month Xylitol (6-10 g/d) gum or candies: 2 tabs of gum or 2 candies 4 times daily 1.1% NaF toothpaste twice daily Initially, 1-3 applications of NaF varnish; 1 application at 3- to 4-mo recall Extreme risk Bitewing radiographs every 6 mo or until no cavitated lesions are evident Every 3 mo to reevaluate caries risk and apply fluoride varnish Saliva flow test and bacterial culture initially and at every caries recall appointment to assess efficacy and patient cooperation Chlorhexidine gluconate, 0.12%: 10-mL rinse for 1 min daily for 1 wk each month Xylitol (6-10 g/day) gum or candies: 2 tabs of gum or 2 candies 4 times daily 1.1% NaF toothpaste twice daily Initially, 1-3 applications of NaF varnish; 1 application at 3- to 4-mo recall Fluoride a Adapted from Jenson L, Budenz AW, Featherstone JD, Ramos-Gomez FJ, Spolsky VW, Young DA. Clinical protocols for caries management by risk assessment. J Calif Dent Assoc. 2007;35(30):714-723.15 Reprinted with permission from the California Dental Association. Copyright © October 2007. Abbreviations: ICDAS, International Caries Detection and Assessment System; NaF, sodium fluoride; OTC, over-the-counter. Irradiation, many medications, and systemic diseases can reduce the flow of saliva.17 It has been reported that 80% of the most commonly prescribed medications cause xerostomia.17 To combat the body’s inability to buffer the pH in the mouth as a result of hyposalivation, toothpastes with sodium bicarbonate are recommended.17 Additionally, a solution of water and sodium bicarbonate (2 tsp per 12-16 oz of water) can be used as a neutralizing rinse throughout the day. These treatments have been shown to reduce demineralization and inhibit colonization by MS.17 After bacteria and the pH of the mouth are stabilized, remineralization is necessary to prevent cavitation and reverse any demineralization. To maximize remineralization, fluoride treatment should be used for all patients, regardless of age or risk. Fluoride inhibits plaque, halts demineralization, speeds remineralization, and, when combined with calcium and phosphate, forms a hard fluorapatite coating on top of demineralized tooth crystals.17 70 GENERAL DENTISTRY July/August 2016 Fluoride can be employed as a topical agent such as in toothpaste or a varnish. Fluoride toothpaste in concentrations of 1000-1100 ppm should be used twice per day in a pea-sized amount.17 Patients in high and extreme caries risk categories (especially those with root sensitivity or who are hyposalivating) should use 1.1% sodium fluoride (NaF) toothpaste (5000 ppm).17 Additionally, all at-risk patients should use over-the-counter 0.05% NaF mouthrinses twice per day for 30-60 seconds to stop demineralization and stimulate remineralization. Fluoride varnishes can be applied at intervals that depend on the patient’s risk.18 Varnishes are effective because they adhere well to tooth surfaces even in the presence of saliva and provide a high concentration of fluoride (5% NaF), improving the rate and degree of remineralization.17 The use of fluoride varnish, especially at 4-month intervals, has been shown to be efficacious for those individuals with a moderate or greater risk.18 Fluoride varnish can be applied easily outside a dental office pH Control Calcium phosphate topical supplements between 2 categories, the patient was assigned to the higher category. The presence of any disease indicator automatically placed the patient in the high-risk category. Additionally, if any disease indicator was combined with dry mouth, the patient was automatically deemed to be at extreme risk for dental caries.2 Results of the 6-year study confirmed that the CDA CRA form is a valid tool for assigning patients to appropriate risk categories.2 All of the disease indicators and pathological risk factors on the CDA CRA form showed a statistically significant (odds ratio greater than 1) positive relationship to the presence of cavitation or penetration into dentin. Those patients deemed at high or extreme risk of dental caries had developed caries at follow-up. Conversely, 76% of those deemed to be at low risk returned with no new cavities.2 All of the results illustrated that the CDA CRA form was predictive of dental caries. According to another clinical study conducted at the University of California, San Francisco, from 2010 to 2012, caries risk assessment—including aggressive preventive treatment and minimal restorations—resulted in a reduced caries increment compared to that found in adults who did not use this approach.3 CAMBRA intervention led to a statistically significant reduction in caries risk and MS bacteria. Additionally, placing restorations in the control group did not significantly reduce MS bacteria counts or change the risk of caries.3 Sealants (resin-based or glass ionomer) Not required Not required Optional: for excessive root exposure or sensitivity Optional Not required Not required Optional: for excessive root exposure or sensitivity As per ICDAS sealant protocol Not required Optional Apply calcium phosphate paste several times daily As per ICDAS sealant protocol Conclusion setting, as no special equipment is needed; however, this task must be carried out in accordance with the rules and regulations of local practice acts. Dental caries is a burden on patients, clinicians, and hospitals. Severe odontogenic infections requiring inpatient and even intensive care unit stays are familiar challenges to every oral and maxillofacial surgeon and are often the result of untreated carious lesions. Many patients admitted to hospitals for severe odontogenic infections had previously been treated by an outside dentist or physician who employed either a targeted restorative treatment or an antibiotic prescription.19 These types of treatment are not sufficient. Dental caries is a complex disease that requires aggressive preventive treatment. CAMBRA is an evidence-based preventive method that provides an effective measure of which risk factors are out of balance and which protective factors can restore balance. Protective factors are needed to both arrest carious lesions and inhibit further formation.13 Any healthcare provider can easily adopt a caries risk assessment such as CAMBRA for every patient encounter. Early implementation of preventive strategies can reduce the morbidity of this common disease process. Success of the CAMBRA model Author information Acid-neutralizing rinse as needed if mouth feels dry, after snacking, at bedtime, and after breakfast Required Apply calcium phosphate paste twice daily As per ICDAS sealant protocol Clinical studies have shown that CAMBRA accurately assigns patients to risk categories, predicts how likely a patient in a certain risk category is to develop dental caries, and, if recommended treatments are followed, reverses and inhibits progression of damage from dental caries.2,3 One study reviewing the success of the CDA CRA form and CAMBRA protocols for patients older than 6 years was conducted from 2003 to 2009.2 Dental students and faculty at the University of California, San Francisco, were trained to perform an overall caries risk assessment by evaluating the patient’s yes or no answers to the CDA CRA form and making a clinical judgment as to which category best fit the patient. If it was found that the patient fell Ms Mills is a research assistant, Lombaert Lab, University of Michigan, School of Dentistry, Ann Arbor. Dr Patel is in private practice, Dunwoody, Georgia. References 1. California Dental Association Foundation. Caries Management by Risk Assessment (CAMBRA). http://www.cdafoundation.org/education/cambra. Accessed April 11, 2016. 2. Doméjean S, White JM, Featherstone JD. Validation of the CDA CAMBRA caries risk assessment—a six-year retrospective study. J Calif Dent Assoc. 2011;39(10):709-715. 3. Featherstone JD, White JM, Hoover CI, et al. A randomized clinical trial of anticaries therapies targeted according to risk assessment (caries management by risk assessment). Caries Res. 2012;46(2):118-129. 4. Featherstone JD. Dental caries: a dynamic disease process. Aust Dent J. 2008;53(3):286-291. www.agd.org/generaldentistry 71 Adopting caries risk assessment in all practice environments 5. American Dental Association. ADA: Dental-Related ER Visits Rising in the US [press release]. July 2, 2013. http://www.ada.org/en/press-room/news-releases/2013-archive/july/ada-dental-related-er-visits-rising-in-the-us. Accessed April 11, 2016. 6. US Census Bureau. Population Distribution and Change: 2000 to 2010. 2010 Census Briefs. March 2011. http://www.census.gov/prod/cen2010/briefs/c2010br-01.pdf. Accessed April 11, 2016. 7. McCormick AP, Abubaker AO, Laskin KM, Gonzales MS, Garland S. Reducing the burden of dental patients on the busy hospital emergency department. J Oral Maxillofac Surg. 2013; 71(3):475-478. 8. World Health Organization. Oral Health. Fact sheet No. 318. April 2012. http://www.who.int/ mediacentre/factsheets/fs318/en/. Accessed April 11, 2016. 9. National Institutes of Health, National Institute of Dental and Craniofacial Research. Dental Caries (Tooth Decay). Updated May 28, 2014. http://www.nidcr.nih.gov/datastatistics/finddatabytopic/dentalcaries/. Accessed April 11, 2016. 10. Department of Health, Health & Social Care Information Centre. Child Dental Health Survey 2013, England, Wales and Northern Ireland. March 19, 2015. http://www.hscic.gov.uk/catalogue/PUB17137. Accessed April 28, 2016. 11. Bagramian RA, Garcia-Godoy F, Volpe AR. The global increase in dental caries. A pending public health crisis. Am J Dent. 2009;22(1):3-8. 12. Pottinger P, Reller LB, Ryan KJ. Pathogenic bacteria. In: Ryan KJ, Ray CG, eds. Sherris Medical Microbiology. 6th ed. New York: McGraw-Hill Education; 2014:687-694. 13. Featherstone JD, Domejean-Orliaquet S, Jenson L, Wolff M, Young DA. Caries risk assessment in practice for age 6 through adult. J Calif Dent Assoc. 2007;35(10):703-707, 710-713. 14. Young DA, Featherstone JD, Roth JR, et al. Caries management by risk assessment: implementation guidelines. J Calif Dent Assoc. 2007;35(11):799-805. 15. Jenson L, Budenz AW, Featherstone JD, Ramos-Gomez FJ, Spolsky VW, Young DA. Clinical protocols for caries management by risk assessment. J Calif Dent Assoc. 2007;35(30):714723. 16. Ramos-Gomez F, Ng MW. Into the future: keeping healthy teeth caries free: pediatric CAMBRA protocols. J Calif Dent Assoc. 2011;39(10):723-733. 17. Spolsky VW, Black BP, Jenson L. Products—old, new, and emerging. J Calif Dent Assoc. 2007; 35(10):724-737. 18. Association of State and Territorial Dental Directors Fluorides Committee. Fluoride Varnish: An Evidenced-Based Approach [research brief]. September 2007. http://www.astdd.org/ docs/Sept2007FINALFlvarnishpaper.pdf. Accessed April 11, 2016. 19. Appelblatt R, Krutoy J, Karlis V. Associated factors involved in presentation and care of severe odontogenic infections. J Oral Maxillofac Surg. 2014;72(9 Suppl):e37. Published with permission of the Academy of General Dentistry. © Copyright 2016 by the Academy of General Dentistry. All rights reserved. For printed and electronic reprints of this article for distribution, please contact [email protected]. 72 GENERAL DENTISTRY July/August 2016