* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Aging Q3 Med Use and Safety Detailing Sheet2 - 86 KB
Survey
Document related concepts
Effects of long-term benzodiazepine use wikipedia , lookup
Prescription costs wikipedia , lookup
Neuropharmacology wikipedia , lookup
Psychopharmacology wikipedia , lookup
Pharmacokinetics wikipedia , lookup
Electronic prescribing wikipedia , lookup
Polysubstance dependence wikipedia , lookup
Drug interaction wikipedia , lookup
Intravenous therapy wikipedia , lookup
Theralizumab wikipedia , lookup
Transcript
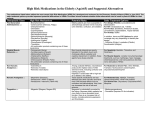
Medication Use and Safety in the Elderly Americans aged 65 and over consumer 30% of all prescriptions and 40% of all OTC medications. They are at higher risk for adverse drug events, drug-drug interactions, and therapeutic duplication. Medication Use and Patient Safety ***** Challenges of Prescribing for Older Adults • Multiple chronic medical problems • Multiple medications and prescribers • Different metabolism and responses • Adherence and cost • Supplements, herbals, and OTC drugs Physiologic Changes Associated with Normal Aging • Less Water • More Fat • Less muscle mass • Slowed hepatic metabolism • Decreased renal excretion • Decreased responsiveness and sensitivity of the baroreceptor reflex Dangers of Multiple Medications: “Polypharmacy” • Adverse effects (side effects) • Drug-drug interactions • Duplication of drug therapy • Poor adherence • Cost • Decreased quality of life Adverse Drug Events (ADEs) Adverse symptoms Adverse patient outcomes o Doctor visits or hospitalizations o Falls o Functional decline o Changes in cognition (delirium) o Death ↑ number of medications = ↑ risk of ADEs (even if all the meds are “clinically indicated”) References: 1. Budnitz, DS, et al. (2006) “National Surveillance of Emergency Department Visits for Outpatient Adverse Drug Events.” JAMA 296 (15) 2. Beers, J Am Geriatr Soc. 2012 Funded by DW Reynolds Foundation The most common cause of adverse medication events that result in emergency department use in the elderly: ***** Hypoglycemic agents: Decreased renal clearance leads to drug accumulation and hypoglycemic episodes so ask patients about signs and symptoms of hypoglycemia. Digoxin (Lanoxin): Accumulates in the elderly population can lead to toxicity (nausea, anorexia, vomiting, and rarely yellow vision) Digoxin should be dosed at ≤ 0.125mg/day unless treating atrial arrhythmias. Ask patients about nausea, anorexia, vomiting and, if present, check a digoxin level. Warfarin (Coumadin): Make sure all patients on warfarin are enrolled in pharmaco- therapy clinic. Amiodarone (Cordarone): A major CYP-3A4 inhibitor resulting in multiple drug-drug interactions. Dose reductions are necessary for many medications including: Warfarin- 35-65% dose reduction, Digoxin50% dose reduction and Simvastatin- maximum dose of 20 mg. NSAIDs: Increase incidence of GI bleed, acute renal failure and HTN in the elderly with risk factors for GI bleed: age >75 years, previous GI bleed, concomitant use of warfarin, long term glucocorticoid use, history of PUD. Risk factors warrant therapy with misoprostol or PPI. Herbal products: Not regulated by FDA, many have the potential to be dangerous. Rarely considered by patients as medications and their use is often not discussed with a physician. Garlic and Gingko Biloba: Increase bleeding time St John’s Wort: Increased clearance of medications metabolized through CYP3A4 Chromium, Gingko Biloba, Nettle: Hypoglycemia Know what your patients are taking and evaluate for potential harm. Other agents commonly associated with ED visits and hospitalizations in the elderly: 1 Opioid and non-opioid analagesics Antibiotics ACE Inhibitors/ARBs Antihistamines Decongestants/ remedies AVOID THESE MEDICATIONS IN OLDER PATIENTS WHENEVER POSSIBLE!2 MEDICATIONS Pain Relievers Meperidine (Demerol®) Muscle Relaxants Carisoprodol (Soma®), cyclobenzapine (Flexeril®), metaxalone (Skelaxin®) Antidepressants Tricyclic Antidepressants (TCAs): ie, amitriptyline (Elavil®) Fluoxetine (Prozac®) Sleeping Pills and Antianxiety Medications Benzodiazepines: ie, Alprazolam (Xanax®), lorazepam (Ativan®), zolpidem (Ambien®) Heart Medications Digoxin (Lanoxin®) doses above 0.125 mg Dipyridamole (Persantine®) Methyldopa (Aldomet®) Amiodarone (Cordarone®) Diabetes Medications Glipizide (Glucotrol®), glyburide (Diabeta®), glimiperide (Amaryl®), insulin Stomach and Intestinal Medications Dicyclomine (Bentyl®), hyoscyamine (Levsin®), promethazine (Phenergan®) Antihistamines Chlorpheniramine (Chlor-Trimeton®), diphenhydramine (Benadryl®), hydroxyzine (Vistaril®, Atarax®), cyproheptadine (Periactin®) Constipation Calcium channel blockers REASON THAT USE IS A PROBLEM Not effective oral pain reliever, many disadvantages compared to other narcotics. AVOID IN ELDERLY. Poorly tolerated due to severe anticholinergic SE. Can cause sedation, weakness, BP changes, several anticholinergic SE. Long half-life leading to prolonged CNS stimulation, sleep disturbance, anxiety. Increased sensitivity in the elderly. Should use lowest dose possible if used. Decreased renal clearance may lead to toxicity; nausea, anorexia. May cause orthostatic hypotension May cause bradycardia and exacerbate depression in the elderly. Increased risk of QT prolongation and Torsades Decreased renal clearance may result in prolonged hypoglycemia. Monitor closely. Can cause sedation, weakness, BP changes, several anticholinergic SE. Can cause sedation, weakness, BP changes, several anticholinergic SE. Avoid if possible. Safer alternatives are available for cough and cold. Worsen constipation Cognitive impairment Anticholinergics, antispasmodics, muscle relaxants Parkinson’s disease Metoclopramide (Reglan®) Antipsychotics Bladder outflow obstruction Anticholinergics, antihistamines, antispasmodics Syncope/Falls Tricyclic antidepressants Benzodiazepines Concern due to CNS-altering effects Due to cholinergice/antidopaminergic activity Increased urinary retention Increased risk for falls; ataxia; impaired psychomotor function