* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Indications for PFT
Compartmental models in epidemiology wikipedia , lookup
Nutrition transition wikipedia , lookup
Eradication of infectious diseases wikipedia , lookup
Epidemiology wikipedia , lookup
Computer-aided diagnosis wikipedia , lookup
Diseases of poverty wikipedia , lookup
Transmission (medicine) wikipedia , lookup
Public health genomics wikipedia , lookup
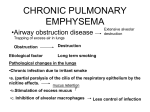
Indications for PFT RET 2414 Pulmonary Function Testing Module 1.0 Indications For PFT Learning Objectives Categorize PFTs according to specific purposes Identify at least one indication for spirometry, lung volumes, and diffusing capacity List one obstructive and one restrictive pulmonary disorder Name at least two disease in which air trapping may occur Relate pulmonary history to indications for performing pulmonary function tests Pulmonary Function Testing Purpose for PFT Identify and quantify pulmonary impairments Pulmonary Function Testing Tests can be divided into categories Airway Function Lung Volumes and Gas Distribution Diffusing Capacity Blood Gas and Exchange Tests Cardiopulmonary Exercise Tests Airway Function Tests Spirometry (meaning the measuring of breath) is the most common of the Pulmonary Function Tests (PFTs). It measures lung function, specifically the direct measurement of the amount (volume) and/or speed (flow) of air that can be inhaled and exhaled. Airway Function Tests Spirometry Vital Capacity (VC) Airway Function Tests Spirometry Forced Vital Capacity (FVC) Airway Function Tests Spirometry Flow – Volume Loop (FVL) AKA; MEFV Curve Airway Function Tests Spirometry Flow – Volume Loop (FVL) AKA; MEFV Curve Airway Function Tests FVC and/or FVL Pre/Post Bronchodilator Pre/Post Bronchochallenge Methacholine Histamine Exercise Airway Function Tests Spirometry Maximum Voluntary Ventilation (MVV) Airway Function Tests Maximal Inspiratory (MIP) Expiratory Pressure (MEP) Airway Resistance (Raw) Compliance (CL) Indications for Spirometry Detect the presence of lung disease Spirometry is recommended as the “Gold Standard” for diagnosis of obstructive lung disease by: National Lung Health Education Program National Heart, Lung and Blood Institute (NLHEP) (NHLBI) World Health Organization (WHO) Indications for Spirometry BOX 1-2 Diagnose the presence or absence of lung disease Quantify the extent of known disease on lung function Measure the effects of occupational or environmental exposure Determine beneficial or negative effects of therapy Indications for Spirometry BOX 1-2 Assess risk for surgical procedures Evaluate disability or impairment Epidemiologic or clinical research involving lung health or disease Lung Volumes Determination of lung volume Includes the VC (spirometry) and its subdivisions, along with the FRC (indirect spirometry) – from these TLC and other lung volumes can be determined Lung Volumes Functional Residual Capacity (FRC) Nitrogen Washout Helium Dilution Thoracic Gas Volumes Indications for Lung Volume Tests Box 1-3 Diagnose or assess the severity of restrictive lung disease Differentiate between obstructive and restrictive disease patterns Assess the response to therapy Make preoperative assessment of patients with compromised lung function Indications for Lung Volume Tests Box 1-3 Determine or evaluate disability Assess gas trapping by comparison of plethysmographic lung volumes with gas dilution lung volumes Standardize other lung functions (i.e., specific conductance) Ventilation Minute Ventilation Alveolar Ventilation Dead Space Distribution of Ventilation Multiple – Breath N2 He Equilibration Single – Breath Techniques Diffusing Capacity (DLco) Diffusing Capacity (DLco) Single – Breath (Breath Hold) Steady – State Other Techniques Indications for Diffusing Capacity Box 1-4 Evaluate or follow the progress of parenchymal lung disease Evaluate pulmonary involvement in systemic disease Evaluate obstructive lung disease Indications for Diffusing Capacity Box 1-4 Evaluate cardiovascular diseases Quantify disability associated with interstitial lung disease Evaluate pulmonary hemorrhage, polycythemia, or left-to-right shunts Blood Gases and Gas Exchange Blood Gases and Gas Exchange Blood Gas Analysis and Oximetry Shunt Study Blood Gases and Gas Exchange Pulse Oximetry and Capnography Indications for Blood Gas Analysis Box 1-5 Evaluate the adequacy of lung function Determine the need for supplemental oxygen Monitor ventilatory support Indications for Blood Gas Analysis Box 1-5 Document the severity or progression of know pulmonary disease Provide data to correct or corroborate other pulmonary function measurement Cardiopulmonary Exercise Test Indications for Exercise Testing Box 1-6 Determine the level of cardiorespiratory fitness Document or diagnose exercise limitations as a result of fatigue, dyspnea, or pain, Cardiovascular / Pulmonary Disease Indications for Exercise Testing Box 1-6 Evaluate adequacy of arterial oxygenation oxyhemoglobin saturation Assess preoperative risk Lung resection or reduction Indications for Exercise Testing Box 1-6 Assess disability Occupational lung disease Evaluate therapeutic interventions such as heart or lung transplant Patterns of Impaired Pulmonary Function Sometimes, patients display patterns during pulmonary function testing that are consistent with a specific diagnosis Obstructive Airway Diseases Simple definition: “Airflow into and out of the lungs is reduced” Obstructive Airway Diseases Chronic Obstructive Pulmonary Disease (COPD) Long-standing airway obstruction caused by: Cystic Fibrosis Bronchitis Asthma Bronchiectasis Emphysema “CBABE” Obstructive Airway Diseases COPD Characterized by: Dyspnea at rest or with exertion Productive cough Obstructive Airway Diseases Emphysema “air trapping” Primarily caused by cigarette smoking! Genetic defect; absence of α-antitrypsin Chronic exposure to environmental pollutants Obstructive Airway Diseases Emphysema Dyspnea at rest or with exertion Productive cough Under weight Barrel-chested Use of accessory muscles Obstructive Airway Diseases Emphysema Purse-lip breathing Breath sounds are distant or absent Chest X-Ray Flattened diaphragms Increased air spaces Obstructive Airway Diseases Emphysema Airway obstruction Spirometry FEV1 is reduced Air trapping Lung Volumes Hyperinflation of FRC Obstructive Airway Diseases Emphysema (cont) Gas exchange abnormalities Diffusing Capacity (DLco) Blood Gases Reduced Hypoxemia/Hypercapnia Possible O2 Desaturation with Exertion Exercise Testing Obstructive Airway Diseases Chronic Bronchitis “Excessive mucus production, with a productive cough on most days, for at least 3 months for 2 years or more.” Obstructive Airway Diseases Chronic Bronchitis Primarily caused by cigarette smoking! Chronic exposure to environmental pollutants Obstructive Airway Diseases Chronic Bronchitis Chronic cough – “smoker’s cough” Dyspnea, particularly with exertion Chest X-Ray Congested airways Enlarged heart w/prominent pulmonary vessels Diaphragms normal or flattened Edema of lower extremities Obstructive Airway Diseases Chronic Bronchitis (cont) Airway obstruction Spirometry FEV1 is reduced Dlco Usually reduced May have a preserved (normal) Dlco, which is helpful to distinguish it from emphysema Obstructive Airway Diseases Chronic Bronchitis (cont) Gas exchange abnormalities Blood Gases Hypoxemia, Hypercapnia in advanced cases Polycythemia Cyanosis Obstructive Airway Diseases Bronchiectasis Pathologic dilatation of the bronchi, resulting from destruction of the bronchial wall by severe, repeated infections. Obstructive Airway Diseases Bronchiectasis Common in Cystic Fibrosis (CF), as well as following bronchial obstruction by a tumor or foreign body. When entire bronchial tree is involved, it is assumed that the disease is inherited. Obstructive Airway Diseases Bronchiectasis Dyspnea Very productive cough Purulent, foul smelling sputum Hemoptysis is common Obstructive Airway Diseases Bronchiectasis Frequent pulmonary infections Right-sided heart failure when advanced Appear chronically ill - under weight Chest X-Ray / CT Scan Airway Dilation Obstructive Airway Diseases Bronchiectasis (cont) Airway obstruction Spirometry Lung Volumes FEV1 is reduced Hyperinflation Gas exchange abnormalities Blood Gases Hypoxemia, Hypercapnia in advanced cases Obstructive Airway Diseases Asthma (Hypereactive Airway Disease) Reversible airway obstruction. Obstruction is characterized by inflammation of the mucosal lining of the airways, bronchospasm, and increased airway secretions. Obstructive Airway Diseases Asthma (Hypereactive Airway Disease) Triggers; agents or events that cause an asthmatic episode Allergic agents Nonallergic agents Pollens, animal dander, house dust mites, molds Viral infections, exercise, cold air, air pollutants, drugs, food additives, emotional upset Occupational exposure Toluene 2,4-diisocyanate (TDI), cotton or wood dusts, grain, metal salts, insecticides Obstructive Airway Diseases Asthma (cont) Airway obstruction During Attacks Peak Flow (PEF) is reduced, also used to track response to bronchodilators Blood Gases Hypoxemia During Diagnosis Airway Resistance (Raw) Spirometry, Pre/Post Bronchodilator Bronchial Provocation if airways appear normal Obstructive Airway Diseases Cystic Fibrosis An inherited disease that primarily affects the mucus-producing apparatus of the lungs and pancreas. Obstructive Airway Diseases Cystic Fibrosis Airway obstruction Spirometry FEV1 used to monitor the progression of the disease Pulmonary function studies are routinely used to assess lung function following transplantation Obstructive Airway Diseases Upper or Large Airway Obstruction (Upper: nose, mouth, pharynx) (Large: Trachea, mainstem bronchi) Increased work of breathing Spirometry Flow-Volume Loop Restrictive Lung Disease Characterized by: Reduction in lung volumes (Vital Capacity (VC) and Total Lung Capacity (TLC) are both reduced below the lower limits of normal. Restrictive Lung Disease Any process that interferes with the bellows action of the lungs or chest wall can cause restriction. Restrictive Lung Disease Idiopathic Pulmonary Fibrosis Characterized by alveolar wall inflammation resulting in fibrosis. Vascular changes are usually associated with pulmonary hypertension. Restrictive Lung Disease Idiopathic Pulmonary Fibrosis IPF often follows Treatment with bleomycin, cyclophosphamide, methotrexate or amiodarone Autoimmune diseases Rheumatoid arthritis, systemic lupus erythematousus (SLE), scleroderma Restrictive Lung Disease Idiopathic Pulmonary Fibrosis Increasing exertional dyspnea Pulmonary hypertension Vascular changes Chest X-Ray Infiltrates are visible Honeycombing pattern when advanced Restrictive Lung Disease Idiopathic Pulmonary Fibrosis Spirometry Reduced VC Lung Volumes Reduced TLC Restrictive Lung Disease Idiopathic Pulmonary Fibrosis Gas exchange abnormalities Reduced DLco Blood Gases Hypoxemia; worsens with exertion Lung compliance Reduced Restrictive Lung Disease Pneumoconiosis Lung impairment caused by inhalation of dusts. Silicosis – Silica dust Asbestosis – Asbestos fibers Coal Worker’s Pneumoconiosis – Coal dust Restrictive Lung Disease Pneumoconiosis (cont) Spirometry Lung Volumes Reduced VC Reduced TLC Gas exchange abnormalities Decreased Diffusing Capacity (DLco) Blood Gases Hypoxemia Restrictive Lung Disease Sarcoidosis Granulomatous disease that affects multiple organ systems. The granuloma found in sarcoidosis is composed of macrophages, epithelioid cells, and other inflammatory cells. Restrictive Lung Disease Sarcoidosis Fatigue Muscle weakness Fever Weight loss Dyspnea and cough Chest X-Ray Enlargement of hilar and mediastinal lymph nodes Interstitial infiltrates Restrictive Lung Disease Sarcoidosis Spirometry Lung Volumes Reduced VC Normal Flow Rates Reduced TLC Gas exchange abnormalities Decreased Diffusing Capacity (DLco) when advanced Blood Gases Normal or hypoxemia Diseases of Chest Wall and Pleura Disorders involving the chest wall or pleura of the lungs result in restrictive patterns on pulmonary function testing. Diseases of Chest Wall and Pleura Kyphoscoliosis Abnormal curvature of the spine both anteriorly (kyphosis) and lateraly (scoliosis). Diseases of Chest Wall and Pleura Kyphoscoliosis Spirometry Lung Volumes Reduced VC Reduced TLC Gas exchange abnormalities Decreased Diffusing Capacity (DLco) Blood Gases (Hypoxemia / Hypercapnia) Diseases of Chest Wall and Pleura Obesity Increased mass of the thorax and abdomen interferes with the bellows action of the chest wall, as well as excursion of the diaphragm. Diseases of Chest Wall and Pleura Obesity Spirometry Reduced VC Normal Flow Rates Lung Volumes Reduced TLC Diseases of Chest Wall and Pleura Obesity Gas exchange abnormalities Decreased Diffusing Capacity (DLco) Blood Gases Hypoxemia / Hypercapnia Polycythemia Pulmonary Hypertension Cor pulmonale Diseases of Chest Wall and Pleura Pleurisy and Pleural Effusion Pleurisy is characterized by deposition of a fibrous exudate on the pleural surface – often associated with pneumonia or cancer. May precede the development of pleural effusion. Diseases of Chest Wall and Pleura Pleurisy and Pleural Effusion Plural effusion is an abnormal accumulation of fluid in the pleural space. Diseases of Chest Wall and Pleura Pleurisy and Pleural Effusion Spirometry Reduced VC because of volume loss Difficulty performing because of pain Lung Volumes Reduced TLC because of volume loss Diseases of Chest Wall and Pleura Pleurisy and Pleural Effusion Gas exchange abnormalities DLco – Difficulty performing due to pain Blood Gases Large effusions may cause changes Neuromuscular Disorders Disease that affect the spinal cord, peripheral nerves, neuromuscular junctions, and the respiratory muscles can all cause a restrictive pattern of pulmonary function. Neuromuscular Disorders Diaphragmatic paralysis Amyotrophic Lateral Sclerosis (ALS, Lou Gehrig’s disease) Guillain – Barre’ syndrome Myasthenia gravis Neuromuscular Disorders Spirometry Reduced VC Lung Volumes Reduced TLC Neuromuscular Disorders Gas exchange abnormalities Blood Gases Hypoxemia if involvement is severe Respiratory alkalosis from hyperventilation Inspiratory Pressures MIP - Reduced Congestive Heart Failure Often caused by left ventricular failure, but may also be associated with cardiomyopathy, congenital heart defects, or left-to-right shunts. In each case, fluid backs up in the lungs. Congestive Heart Failure Spirometry Reduced VC Lung Volumes Reduced TLC Congestive Heart Failure Gas exchange abnormalities DLco is reduced Blood Gases Hypoxemia Lung Compliance Reduced Lung Transplantation Lung transplantation has been used for patients with CF, primary pulmonary hypertension, and COPD. Lung Transplantation Pulmonary function testing is used to both assess potential transplant candidates and follow them postoperatively. Preliminaries to Patient Testing Patient Preparation Withholding Medications Smoking Cessation Bronchodilator held 4-6 hours prior to test Should be ceased 24 hours prior to test Eating should be limited Preliminaries to Patient Testing Physical Measurements Age Height (arm span if unable to stand) Weight Gender Race or Ethnic Origin Preliminaries to Patient Testing Physical Assessment Breathing Patterns Breath Sounds Respiratory Symptoms Preliminaries to Patient Testing Pulmonary History Age, gender, height, weight, race Current Dx. or reason for test Family History (immediate family: mother, father, brother, or sister) Tuberculosis Emphysema Chronic Bronchitis Asthma Hay fever or allergies Cancer Other lung disorders Preliminaries to Patient Testing Pulmonary History Personal History Tuberculosis Emphysema Chronic Bronchitis Asthma Recurrent lung infection Pneumonia or pleurisy Allergies or hay fever Chest injury Chest surgery Preliminaries to Patient Testing Occupation What was your occupation? How long did you work there? Have you ever worked in … Mine, quarry, foundry? Near gases or fumes? Dusty environment? Preliminaries to Patient Testing Smoking Habits Have you ever smoked the following: Cigarettes (how many per day?) Cigars (how many per day?) Pipe (how many bowls per day?) How many years? Do you still smoke? Do you live with a smoker? Preliminaries to Patient Testing Cough Do you ever cough? In the morning? At night? Blood? Phlegm? (when, color, volume) Preliminaries to Patient Testing Dyspnea Do you get short of breath at the following times: At rest? On exertion? At night? Preliminaries to Patient Testing Patient Disposition Dyspneic Wheezing Coughing Cyanotic Apprehensive Cooperative Preliminaries to Patient Testing Current Medications Heart, lung, or blood pressure? Last taken? Test Performance Patient Instruction Many tests are effort dependent Instruction & coaching very important Demonstration a must Test Performance Patient Instruction Encouragement during test Suboptimal effort results in poor reproducibility Documentation of effort important Practice / Review Which of the following are indications for performing spirometry? I. Assess the risk of lung resection II. Determine the response to bronchodilator therapy III. Assess the severity of restrictive lung disease IV. Quantify the extent of COPD a. I and IV b. II and III c. I, II, and IV d. II, III, and IV Practice / Review Which of the following symptoms is an indication for performing spirometry? A. Headache B. Shortness of breath C. Chest pain D. Daytime sleepiness Practice / Review Which of the following tests would be indicated to assess the severity of a restrictive lung disease? A. Blood gas analysis B. Simple spirometry C. Lung volume determination D. Cardiopulmonary exercise test Practice / Review Which of the following tests would be indicated in the evaluation of a patient exposed to dust including asbestos? A. Shunt study B. DLco C. Methacholine challenge D. Airway Resistance Practice / Review A 17-year old female complains of chest tightness and cough after soccer practice. These symptoms are most consistent with which of the following? A. Emphysema B. Congestive heart failure C. Asthma D. Cystic fibrosis Practice / Review Which of the following diseases often results in an obstructive pattern when simple spirometry is performed? A. Sarcoidosis B. Idiopathic pulmonary fibrosis C. Pleurisy D. Chronic bronchitis Practice / Review Lung volumes measured by closed – circuit He dilution may be expected to show a reduced FRC in which of the following? A. Emphysema B. Asthma C. Pulmonary fibrosis D. Upper airway obstruction Practice / Review Which of the following should a pulmonary function technologist do before performing spirometry? a. b. c. d. Limit feedback to the patient to limit placebo effect Explain the physiologic basis of the test Demonstrate how to correctly perform the test maneuver Explain the exact number of efforts that will be required for the test Practice / Review Pulmonary function testing is usually contraindicated in which of the following conditions? A. Untreated pneumothorax B. Congestive heart failure C. Cyanosis D. Tuberculosis Practice / Review In which of the following diseases is air-trapping likely to occur? A. Acute exacerbation of asthma B. Sarcoidosis C. Asbestosis D. Emphysema E. B & C F. A & D Practice / Review Which of the following correctly describes appropriate physical measurements before pulmonary function testing? I. Actual body weight should be used to calculate predicted values II. Standing height should be measured when the patient is barefoot III. Arm span should be used instead of height for a patient with kyphosis IV. Age should be recorded to the nearest decade (10 years) a. I only b. II and III c. I, II, and IV d. I, II, III, and IV