* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Additional Precautions
Compartmental models in epidemiology wikipedia , lookup
Focal infection theory wikipedia , lookup
Medical ethics wikipedia , lookup
Rhetoric of health and medicine wikipedia , lookup
Marburg virus disease wikipedia , lookup
Adherence (medicine) wikipedia , lookup
Electronic prescribing wikipedia , lookup
Patient safety wikipedia , lookup
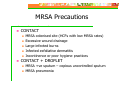
Patient advocacy wikipedia , lookup
Additional Precautions A Guide for Health Care Workers MRSA Staphylococcus aureus (or staph) are bacteria that are found on the skin and in the nose of people. Staph are usually harmless, but they can sometimes cause infection and serious illness. Some strains of staph have become resistant to the antibiotic methicillin and to other antibiotics. Infections caused by methicillinresistant Staphylococcus aureus (MRSA) are hard to treat, as most antibiotics will not kill the bacteria. Methicillin Resistant Staph aureus Amplified by the use of broad-spectrum antibiotics Currently more common in hospitals than in the wider community – is increasing in community May colonise patients and sometimes HCWs Do not appear to be more virulent than antibioticsensitive strains More difficult to treat if infection occurs Colonisation verses Infection Colonisation – the presence of microorganisms without sign of infection The deposition and harmful multiplication of m/o in tissues or on the surfaces of the body, followed by signs and symptoms of clinical illness Increased Morbidity and Mortality MRSA Surgical site infections Infected vascular and orthopaedic prostheses Septicaemia Pneumonia Risk Factors for MRSA Patients most at risk of getting MRSA are those who have: presence of vascular access devices health problems such as diabetes low immunity broken skin from wounds recent surgery; and dermatitis Occurrence of MRSA Colonisation precedes infection, colonisation depends on: Length of stay Nutritional status Severity of underlying disease Presence of invasive devices Recurrent or recent AB treatment Presence of wounds Transmission of MRSA Patient to patient VIA hands of HCWs Direct patient care Handling contaminated materials/equipment INADEQUATE HAND HYGIENE Basic Infection Control In 1996, the National Health and Medical Research Council (NHMRC) adopted the terms ‘standard precautions’ and ‘additional precautions’. These precautions are based on the modes of transmission of infectious agents, to define appropriate work practices. This two tiered approach should provide a high level of protection to patients, HCWs and others. Use of Standard Precautions – For ALL Patients Minimises the risk of cross-infection from: HCW to patient. Patient to HCW. Patient to patient. To be used for all patients regardless of infectious status or perceived risk. Standard Precautions Work practices required for a basic level of infection control Hand hygiene Personal protective equipment Appropriate handling of sharps and waste Appropriate reprocessing of reusable items Use of aseptic technique Use of environmental controls Additional Precautions Additional precautions are based on method of transmission Necessary for infections spread via airborne or droplet transmission AND May be indicated for patients with certain highly transmissible or epidemiological important microorganisms transmitted by direct or indirect contact – e.g. MRSA, VRE MRSA Transmission MRSA can be transmitted via: Contact Droplet – direct/indirect Direct Contact Transfer of microorganisms as a result of direct physical contact between an infected or colonised individual and a susceptible host. (Body surface to body surface) Indirect Contact Involves passive transfer of microorganisms to a susceptible host via an intermediate object, such as contaminated hands that are not washed between patients, or contaminated instruments or other inanimate objects. Droplet Transmission A form of contact transmission Droplet transmission refers to large droplets, > 5 um, generated from the respiratory tract or the source patient coughing or sneezing, or during procedures such as suctioning or bronchoscopy (Large droplets do not remain suspended in the air) MRSA - Additional Precautions Contact precautions or Contact + Droplet precautions Extent of Precautions Depends on: 1. Vulnerability of the patient population 2. Endemicity of MRSA in health care facility Where MRSA rates are relatively low there may be more stringent precautions used than when MRSA is endemic in an organisation MRSA Precautions CONTACT MRSA colonised site (HCFs with low MRSA rates) Excessive wound drainage Large infected burns Infected exfoliative dermatitis Incontinence or poor hygiene practices CONTACT + DROPLET MRSA +ve sputum – copious uncontrolled sputum MRSA pneumonia Additional Precautions (Contact Precautions) Single room if possible, with ensuite Cohort with like condition if necessary Clean, non sterile gown and gloves when entering the room Remove gloves and gown (mask), wash hands before leaving patient room Additional Precautions Use dedicated patient equipment – clean and disinfect before reuse Use disposable equipment wherever possible Instruments and equipment used for dressing changes should not be transferred from patient to patient but should remain by the patients bedside – tapes, non sterile scissors etc. Additional Precautions Patient to leave the room for essential procedures only Maintain precautions during transport Notify area receiving patient Visitors should talk to nursing staff before entering the room Keep visitors to a minimum Droplet Precautions (In addition to contact precautions) Use surgical mask when entering room if patient has colonised/infected respiratory secretions Teach patient to cover nose and mouth when coughing or sneezing Transport of patients – surgical mask to be worn by patient Environmental Contamination Consider the surfaces and furniture within the room contaminated as well as patient After gown/glove/mask removal and handwashing, ensure that hands do not touch potentially contaminated environmental surfaces or items in the patient's room to avoid transfer of microorganisms to other patients or environments. Environmental Cleaning: Wear appropriate PPE – gown, gloves +/- mask Daily routine cleaning of room using dedicated equipment and neutral detergent Pay particular attention to frequently touched surfaces and horizontal surfaces Call bells, door knobs, bed rails, bedside tables and lockers, sinks, surfaces close to patient Terminal cleaning after patient discharge Crockery and Cutlery: No special precautions are needed for dishes, glasses, cups, or eating utensils. The combination of hot water and detergents used in hospital dishwashers is sufficient to decontaminate dishes, glasses, cups, and eating utensils. Handling Linen: Handle with a minimum of agitation All soiled linen should be handled in the same way for all patients Place soiled linen directly into linen skip at point of generation — avoid carrying soiled linen to prevent contamination of uniform. Linen Contd: Roll or fold heavily soiled linen to contain heaviest soil in centre of bundle – place solid soil, faeces or blood clots into a bed pan or toilet for flushing Linen soiled with blood or body substances should be bagged, transported and stored in leakproof bags. Double bagging of linen is not necessary unless outside of bag is contaminated The laundering of linen must be consistent with Australian Standard AS 4146: Laundry Practice. Waste Disposal: Place all sharps into a sharps container Use gloves and protective clothing when handling clinical and related waste bags and containers Do not over fill containers Never compact by hand Secure lids during transport PLACE WASTE HEAVILY CONTAMINATED WITH WOUND EXUDATE INTO YELLOW INFECTIOUS WASTE BAGS Definition – Clinical Waste Discarded sharps Laboratory and associated waste directly involved in specimen processing Human tissue, including materials or solutions containing or contaminated with blood (including other body fluids removed during surgery, birth and autopsy) Animal tissue or carcasses used in research (Australian and New Zealand Clinical Waste Management Industry Group (ANZCWMIG), “Code of Practice for the Management of Clinical and Related Wastes 2004” ) Clinical Waste Contd: Urine and faeces are not considered clinical waste unless: The specimen of urine or faeces is for laboratory testing The urine or faeces is contaminated with visible blood Removal of Waste and Linen Call environmental services to remove waste and linen as soon as possible Do not leave piled up outside door Refer to your Infection Control Nurse or Infection Control Manual for more details REFERENCES: 1. 2. 3. Department of Health and Ageing: Infection Control Guidelines for the Prevention of Transmission of Infectious Diseases in the Health Care Setting, 2004 NSW Health Department Circlar 9987: Infection Control Policy Health Canada. Infection Control Guidelines Supplement: Routine Practices and Additional Precautions for Preventing the Transmission of Infection in Health Care