* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download ANTIBIOTIC REVOLUTION
Marine microorganism wikipedia , lookup
History of virology wikipedia , lookup
Neglected tropical diseases wikipedia , lookup
Antimicrobial copper-alloy touch surfaces wikipedia , lookup
Gastroenteritis wikipedia , lookup
Human microbiota wikipedia , lookup
Transmission (medicine) wikipedia , lookup
Disinfectant wikipedia , lookup
Antibiotics wikipedia , lookup
Infection control wikipedia , lookup
Traveler's diarrhea wikipedia , lookup
Bacterial morphological plasticity wikipedia , lookup
Urinary tract infection wikipedia , lookup
Antimicrobial surface wikipedia , lookup
Neonatal infection wikipedia , lookup
Triclocarban wikipedia , lookup
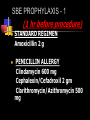
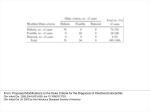
Trends of usage of antimicrobial agents in dental practice on the basis of prescription analysis Oral cavity organisms more than 400 species Aerobic as well as anaerobic Anerobic 10 – 100 times more Spirochetes, Candida, viral To deal with Dental Caries Dentoalveolar abscess, pulp infection, periapical abscess Gingivitis Periodontitis – pericoronitis, periodontal abscess, osteomyelitis, peri-implantitis Deep fascial infection Indications for Chemotherapeutic Agents Orodental Infections To prevent other infections – bacterial endocarditis To prevent postoperative infection Improve healing Aims of study To get general idea of prescribing trends Comparing the trends in institutional practice and private practice To analyze the prescriptions in order to determine The rationale - indications, adequacy of dosage, and duration of treatment The adequacy for prophylaxis The attention given to contraindications and precautions Period of study: 01/01/05–06/30/05: 6 months Material: OPD antimicrobial Prescriptions Data collected from – TEACHING INSTITUTES: 03 PRIVATE CLINICS: 30 ¤ SPECIALISTS: 10 ¤ GDP: 20 (General Dental Practitioners) INSTITUTES Prescriptions VPDC, Sangli 1805 TKDC, Kolhapur 910 GMC, Miraj 903 Total PRIVATE CLINICS Specialists 1235 GDP 2740 Total 3618 Total 3975 TOTAL 7593 TEACHING INSTITUTES DRUG 1 Penicillins 222 Pen + clavulanate 2 3 Total ( %) 120 419 761 (21%) 215 52 137 404 (11.16%) Cephalosporin 52 16 37 105 (2.9%) Quinolone 237 135 123 495 (13.68%) Quino + metro/T 820 475 95 1390 (38.4%) Macrolide 118 63 45 226 (6.24%) Sulfa/cotrimoxazole 95 19 22 136 (3.7%) Tetra 37 20 5 62 (1.71%) Clindamycin 9 10 20 39 (1.07%) PRIVATE CLINICS DRUG Penicillins Pen+ clavulanate Cephalosporin Quinolone Quino + metro/T Macrolide Sulfa/cotrim Tetra Clindamycin SPE 75 77 95 97 805 34 16 8 28 GDP 247 260 67 164 1661 230 62 44 5 TOTAL 322 337 162 261 2466 264 78 52 33 (%) (8.10%) (8.47%) (4.07%) (6.56%) (62.3%) (6.64%) (1.96%) (1.3%) (0.83%) TRENDS – Institutes Vs Private DRUG Penicillins Pen+clavulanate Cephalosporin Quinolone Quino+metro/T Macrolide Sulfa/cotrim Tetra Clindamycin INSTI 761 404 105 495 1390 226 136 62 39 PRI 322 337 162 261 2466 264 78 52 33 TOTAL (%) 1083 (14.4%) 741 (9.83%) 267 (3.54%) 756 (10%) 3856 (51.2%) 490 (6.5%) 214 (2.84%) 114 (1.51%) 72 (0.95%) Trends INSTITUTES PRIVATE TOTAL Quinolone + 38.41% metronidazole/T Penicillins 21% 62.3% 51.18% 8.10% 14.37% Quinolone alone 13.68% 6.56% 10.03% Penicillin + clavulanate Macrolides 11.16% 8.47% 9.83% 6.24% 6.64% 6.5% Other remarkable observations CIPRO IN CHILDREN Ciprofloxacin ( up to 5 years): 1.3% Ciprofloxacin ( 5-10 years): 2.7% Ciprofloxacin ( > 10 years): 3% Inadequate frequency of admn Amoxicillin: 250 mg bid: 16.7% Ampicillin: 250 mg bid: 15% Timing of treatment/prophylaxis Inadequate duration: 19.4% Ciprofloxacin single dose, Amoxicillin 2 days, Ampicillin 2 days Antibiotic started after the procedure: 61.3% ORO DENTAL INFECTIONS Periapical/Periodontal Abscess Acute Suppurative pulpitis/Toxic cellulitis. Salivary Gland Sepsis/Sinusitis Post Surgical/Post Traumatic. Oro-antral/Oro-nasal Fistula. Ludwig’s angina/Purulent osteitis Pericoronitis/Mucositis/Pemphigus SPECTRUM PEN G/ PEN V AMPI/ AMOXY MACROLIDE ORODENTAL INFECTIONS CLINDA CEPHA Prophylaxis (Prevention) 1. 2. 3. 4. Bacterial Endocarditis. Prosthetic Joint Infections. Immuno-Compromised Hosts. Procedures and others. SBE PROPHYLAXIS RECOMMENDED Extractions, Periodontal procedures Prophylactic cleaning Implant placement, Re-implantation Endodontic Instrumentation/Surgery beyond root apex, Placement or removal of orthodontic bands Intraligamentary LA SBE PROPHYLAXIS - 1 (1 hr before procedure) STANDARD REGIMEN Amoxicillin 2 g PENICILLIN ALLERGY Clindamycin 600 mg Cephalexin/Cefadroxil 2 gm Clarithromycin/Azithromycin 500 mg SBE PROPHYLAXIS - 2 30 mins before procedure) Failure to take P/O Ampicillin 2 gm IM/IV Penicillin allergy & Failure to take P/O Clindamycin 600 mg IV Cefazolin 1 gm IM/IV PREFER CIDAL AGENT, SUSCEPTIBILITY NARROWEST SPECTRUM CORRECT DOSING AND ADEQUATE DURATION OF TREATMENT Inferences 1. 2. 3. Most commonly prescribed antimicrobials were quinolones in combination with metronidazole and tinidazole (51% ). Amongst the quinolones, ciprofloxacin and ofloxacin were the quinolones chosen by 95% of the prescribers. Quinolones – ciprofloxacin, ofloxacin were prescribed alone by 10% prescribers. 4. Inadequacy of the frequency of administration was found in 15-17% prescriptions. 5. Inadequate duration of treatment was observed in 19.4% prescriptions. 6. First generation quinolones were prescribed to the children in the range of 1-3% of the prescriptions given for quinolones. 7. The antimicrobial agent was started AFTER THE PROCEDURE in about 61% cases. BIBLIOGRAPHY 1. Sudha P et al: Journal of Indian society of Pedodontics and preventive dentistry 23-2 (2005) 74-79 2. Studervant et al: JIDA 64 (1993) 389-392 3. Damle et al: Community dental oral epidemiol:22 (1994) 62-63 4. Dajani et al: Prevention of bact endocarditis recommendations by AHA: JAMA: 277-1997-1794-1801 5. Oral health and morbidity - implications of oral infections on the elderly - Jukka H. Meurman, Piia Hämäläinen GerodontologyVol. 23 Issue 1 Page 3 March 2006 5. Lin LJ, Chiu GK, Corbet EF. Are periodontal diseases risk factors for certain systemic disorders-what matters to medical practitioners? Hong Kong Med J. 2003;9:31-37. 6. Loesche WJ. Association of the oral flora with important medical diseases. Curr Opin Periodontol. 1997;4:21-28. 7. 1989 World Workshop in Clinical Periodontics. Ann Periodontol. 1999;4:1-112. 1999 International Workshop for a Classification of Periodontal Diseases and Conditions. Papers. Ann Periodontol. 1999;4:1-112. 8. Evaldson G, Heimdahl A, Kager L, Nord CE. The normal human anaerobic microflora. Scand J Infect Dis Suppl. 1982;35:9-15. 9. Heimdahl A, von Konow L, Satoh T, Nord CE. Clinical appearance of orofacial infections of odontogenic origin in relation to microbiological findings. J Clin Microbiol. 1985;22:299-302. 10. Brook I, Frazier EH, Gher ME. Aerobic and anaerobic microbiology of periapical abscess. Oral Microbiol Immunol. 1991;6:123-125. 11. Brook I, Hunter V, Walker RI. Synergistic effect of Bacteroides, Clostridium, Fusobacterium, anaerobic cocci, and aerobic bacteria on mortality and induction of subcutaneous abscesses in mice. J Infect Dis. 1984;149:924-928. 12. Namavar F, Verweij-van Vught AMJJ, Vel WAC, Bal M, MacLaren DM. Polymorphonuclear leukocyte chemotaxis by mixed anaerobic and aerobic bacteria. J Med Microbiol. 1984;18:167?172. 13. Namavar F, Verweij AMJJ, Bal M, Martijn van Steenbergen TJ, de Graaf J, MacLaren DM. Effect of anaerobic bacteria on killing of Proteus mirabilis by human polymorphonuclear leukocytes. Infect Immun. 1983;40:930-935. 14. Gibbons RJ, MacDonald JB. Hemin and vitamin K compounds as required factors for the cultivation of certain strains of Bacteroides melaninogenicus. J Bacteriol.1960;80:164-170. 15. Mouton, C., Hammond PG, Slots J, Genco RJ. Serum antibodies to oral Bacteroides asaccharolyticus (Bacteroides gingivalis): relationship to age and periodontal disease. Infect Immun. 1981;31:182-192. 16. Slots J. Microbial analysis in supportive periodontal treatment. Periodontol. 2000;12:56-59. 17. Gronbaek Frandsen EV. Bacterial degradation of immunoglobulin A1 in relation to periodontal diseases. APMIS Suppl. 1999.87:1-54. 18. Duerden BI. Virulence factors in anaerobes. Clin Infect Dis. 1994;Suppl 4:S253-S259. 19. Brook I. The role of beta-lactamase-producing bacteria in the persistence of streptococcal tonsillar infection. Rev Infect Dis. 1984;6:601-607. 20. Roos K, Grahn E, Holn SE. Evaluation of beta-lactamase activity and microbial interference in treatment failures of acute streptococcal tonsillitis. Scand J Infect Dis. 1986;18:313-319. 21. Brook I, Gober AE. Emergence of beta-lactamase-producing aerobic and anaerobic bacteria in the oropharynx of children following penicillin chemotherapy. Clin Pediatr. 1984:23:338341. 22. Tuner K, Nord, CE. Emergence of beta-lactamase producing microorganisms in the tonsils during penicillin treatment. Eur J Clin Microbiol. 1986;5:399-404. 23. Brook I, Gober A. Prophylaxis with amoxicillin or sulfisoxazole for otitis media: effect on the recovery of penicillin-resistant bacteria from children. Clin Infect Dis. 1996;22:143-145. 24. Brook I, Gober AE. Monthly changes in the rate of recovery of penicillin-resistant organisms from children. Pediatr Infect Dis J. 1997;16:255-257. 25. Brook I, Douma M. Antimicrobial Therapy Guide for the Dentist. Newtown, Pa: Handbooks in Health Care Co.; 2003. 26. Stanford Guide to Antimicrobial Therapy. 33rd ed. Vermont: Antimicrobial Therapy, Inc; 2002. 27. Ehrenfeld M. Clindamycin in the treatment of dental infections. In: Zumbrano D, ed. Clindamycin in the Treatment of Human Infections. 2nd ed. Kalamazoo, Mich: Pharmacia and Upjohn; 1997. 28. Bartlett JG. Clinical practice. Antibiotic-associated diarrhea. N Engl J Med. 2002;346:334-339. 29. Conrads G. DNA probes and primers in dental practice. Clin Infect Dis. 2002;1(Suppl 1):S72-S77. 30. Craig WA. Pharmacokinetic/pharmacodynamic parameters: rationale for antibacterial dosing of mice and men. Clin Infect Dis. 1998;26:1-12. 31. Longman LP, Preston AJ, Martin MV, Wilson NH. Endodontics in the adult patient: the role of antibiotics. J Dent. 2000;28:539-548. 32. Isla A, Canut A, Gascon AR, et al. Pharmacokinetic/pharmacodynamic (PK/PD) analysis of antimicrobial treatment of orofacial odontogenic infections. Clin Pharm. 2003.





























![Jones Handouts [Compatibility Mode]](http://s1.studyres.com/store/data/004198564_1-64893a1a1dcde6f69f39c96314d64c08-150x150.png)