* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Osteopenia – loss of bone mass (used more of a descriptive word)
Survey
Document related concepts
Transcript
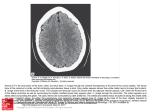
DX Imaging MT Notes 1 of 16 Osteopenia – loss of bone mass (used more of a descriptive word) Lytic bone cancer, osteoporosis Radiolucent – an object that allows x-ray to pass through readily (air is the most radiolucent) Contrast (image) – the number of the shades of gray (kVp controls this and helps when taking images in different areas of the body) Contrast (i.e. orally taken) – radiopaque medium (barium is the metal) Could also do a venogram or ateriogram (blood), angiogram, mylogram (dura mater), airway distribution, digestive system, Differential Absorption – the most radiolucent to most radiopaque things (attenuating properties of an object) Air – most radiolucent Water muscle fat Trabecular or medullar bone Cortical bone Metal – most radiopaque Attentuating technologies – what will help make the best picture in the area that you are taking the picture. Go off of how much of the beam stays in the patient. Beam in less beam out. Tomography, CT, x-ray plain film (pf). Metastasis – primary process that has spread to a distant location (seen in infection, cancer, and soft tissue calcification) Hounsfield Units – CT unit measurement (how much makes it from the sender to the receiver) these are used to decide what number each pixel gets. We will use these to decipher a bone window from a soft tissue window Hematopoiesis - making red blood cells, made in the bone marrow. Older patients will have decreased RBC production capacity and normally have a 1 to 1 ratio. Younger patients have a higher ratio. Red marrow stays the longest at the ends of the long bones. Image based upon mapping protons – MRI, patient emission study. FM radio frequency. Cortical bone = black, because no mobile hydrogen. CSF = black or white, depending on T1 or T2. It all depends on when you listen. When fat is dark fluid is white.(T2) When fluid is dark and fat is white. (T1) Osteoblastic bone activity – bone scan, hot spot – increased blood flow, patient has radioactive material present in them Two types of bone production * These notes are not all inclusive – make sure you read the assigned material and know the cancer chart as gone over in class DX Imaging MT Notes 2 of 16 Intramembranous – one layer at a time with active bone growth out of the endosteum and periosteum. This growth will add diameter to long bones and flat bones except occiput, ribs, and portions of the pelvis. This type of growth never ends Initiated by proliferation of mesenchymal cells about a network of capillaries. Collagen fibers and ground substance join in forming a mesh-like matrix. The cells enlarge and become arranged in layers. Enchondral – the epipheseal plate (growth plate, phisis) normally below the epiphysis. This type of production ends at a point in life. The phisis will show up as a black line on x-ray. Formed around primary ossification centers. Use a non-ossified matrix as a framework. Osteoblasts and osteoclasts form and become imbedded. Cell death is followed by ossification. ZPC - zone of provisional calcification - the most mature layer of the phisis or the least mature layer of the metaphysis Start with mesenchyme, then there is cell death and replacement. From osteoid to completely ossifying. Blood supply comes from the middle first through a nutrient foramen. Next, the ends will get blood supply from the outside. (Before this direct blood supply the blood went through the phisis. Skeleton of the newborn contains primary ossification centers and non-ossified cartilage. FEMUR HEAD - there are 2 growth plates at the head. As the child grows the apophysis and epiphysis grow. The apophysis has muscles and tendons attached to it and is the tubercle at the top of the femur bone. The epiphysis is the femur head and is known as the articular cartilage. Epiphisis - articular cartilage Apophysis - where tendons and ligaments attach. Joint The synovial joints first form as condensations of mesenchyme cavitation, chondrification, synovial differentiation, and finally ossification completing the joint. Growth plate responsible for lengthening Sutures Maxillary sinus - is small when you are young, but builds to make a sharp edge as you get older The mastoid is not developed in the young 5 Regulators of bone 1. Calcium regulators - parathormone, 1,25-dihydroxyvitamin D, calcitonin i. Parathormone 1. Directly acts on renal tubules and makes them more conservative with urine 2. Acts on kidney to activate 1,25 dihydroxyvitamin D * These notes are not all inclusive – make sure you read the assigned material and know the cancer chart as gone over in class DX Imaging MT Notes 2. 3. 4. 5. 3 of 16 3. Goes to skeleton and weakens the bonds within the boney matrix, this allows the osteoclasts liberate or withdraw more calcium per unit time. (softens bone) ii. 1,25-dihydroxyvitamin D - helps to capture more calcium in digestion iii. Calcitonin - works in opposition to parathormone (decreases calcium in blood stream and allows calcium to be secreted through urine, it also inhibits the production of 1,25-dihydroxyvitamin D Maturation Hormones - glucocorticoids, insulin, thyroxin, androgen, estrogen, ad growth hormone i. Estrogen - if this is too high the lady will go through premature maturation and can cause a person to be shorter than normal, since there is a premature closure of the growth plate ii. Growth hormone - responsible for the lengthening of the bone 1. Acromegaly - frontal bone, hands can still grow iii. Androgen & Estrogen - control growth plate Growth factors - somatomedin, epidermal growth factor, plateletderived growth factor Somatomedin - major regulator in bone regulation i. Local factors - prostoglandinE2, interleukins Ions-calcium and phosphate i. Calcium phosphate exist in a 2-1 ration and is responsible for the building and breaking down of bone Normal changes in the maturing skeleton pseudotumor of the growth pelvis…really a growth center You must know basic x-ray anatomy - handout given on what is testable (outline) The use of radiology in your practice Documentation is the frame of mind that Dr. Kuhn would like you to have. There is some risk around radiology. There is absorption of the x-ray in the body. From this there is risk. First get to know them, find out what their goal is and possibly where I can help. New patient information form o OPPQRST - this provides an easy way to learn a lot. This will provide information that will make a difference, and if you can put it into a conversation that is where you become very good at this. Orthopedic exam, Neurologic exam, and chiropractic specific exam Having the above will give you the Differential Diagnosis - possible (probability), you are taught this at Logan and this is so you get a fast and usually accurate diagnosis We are in a cost containment health care system * These notes are not all inclusive – make sure you read the assigned material and know the cancer chart as gone over in class DX Imaging MT Notes 4 of 16 Overall Meet the NP, OPPQRST, Past medical history, family history, local information, diff. Diagnosis, testing strategy, rule in or rule out diagnosis, treat, look for results or changes Imaging is used for documentation and additional testing past the physical exam of the patient Another time to take a X-ray If there is a trauma you would not immediately x-ray, there are some other things to look for, but usually a x-ray may still be warranted. A patient may request the x-ray too Who owns the film? The patient does not own it. The doctor owns the film, unless a business has an agreement with the doctor. If you let it out of your hands and you have to bring it up for some reason and cannot, you are the one in trouble. The patient owns the information….that's what they pay for, which is usually 2 bills o Technical o Service X-ray report - where you document findings on the x-ray o There should be some order to it all. o Heading Stationary - this includes header of business name, location, and how to get in communication and who actually read the film Patient information - name or identification, age of patient, date of x-ray taken *optional* - Technique - kVp/MAS used Views - which ones did you use to get to the conclusion o Body / Finding Use descriptive language (the femoral acetabular joint….) for the picture you see Impression - DJD of the hip Differential Diagnosis - possibility or probability o Recommendation What you think the doctor could do to resolve the problem Possible resolutions for what is present in the patient o How do we use this report or what is it used for? Report of findings What is happening with the patient? Insurance coverage The patient may want to read or see this 3rd party payers Lawyers Research * These notes are not all inclusive – make sure you read the assigned material and know the cancer chart as gone over in class DX Imaging MT Notes o 5 of 16 This report can be used to replace a lost film. It is the only legal way. Any licensed health care professional can do a report. Every x-ray should have a report, and the report is needed if you plan to bill for it. Why would you want to read your own films? o If you read your own you can treat now. Convenience or make money? Why send the films out? o So you do not miss something o So the patient gets the best care possible. Accuracy in reading films o 660 participants in this sampling o 21 different standardize cases o Different types of practices, yet the same 71% accuracy is the top and Chiropractic Radiologists is that type of person 51% for General Medical Radiologist 28% Chiropractic Students 5.75% Medical Students What is the patient’s best interest? What type of liability is out there? General practice Specialist 3 types of people to interpret films D.C. only (level of liability is as a radiologist) Specialist only (level of liability is as a general practitioner) D.C. and specialist (level of liability is as a radiologist) Anatomy can be used as a match part for the Exam Basic rules for interpretation Plain films are a 2 dimensional gray scale image of a 3 dimensional anatomical structure 4 basic densities Metal Air Water Bone * These notes are not all inclusive – make sure you read the assigned material and know the cancer chart as gone over in class DX Imaging MT Notes 6 of 16 Rule of thumb for radiographs: minimum of 2 views that are offset by 90 degrees for any body part ABCS search patterns AP view of open mouth This is the most used recent film series Atlanto-occiptal joint, lateral masses of C-1, odontoid process, C2, atlantoaxial joint, dens, pedicle (attachment site of the posterior element), Lateral Cervical - important assessment of this Cervical Oblique - taken to see the foramen o Neuronal foramina, apophyseal joints, intervertebral disc space, Anterior or posterior oblique possible Anterior and posterior for cervical and do lumbar in positioning Cervical Oblique o LPO - looking at right foramen of the cervicals (left posterior oblique) 15 degrees cephalid tube tilt o LAO - looking at right foramen of cervicals (left anterior oblique) 15 degrees caudal tube tilt Posterior Anterior Chest o The bigger the kyphosis the more we will superimpose ribs on top of each other o Check for the ribs. Once you think you found the 1st rib, check for any other ribs above that. o Also look for ribs superimposed under clavicle AP lumbar o Body, pedicle, o o Parallel ileum tells all Scotty is always looking to the right LAO Normal Wrist (this could be on Comp Boards II) o Some lovers tri positions that they can't handle (start at thumb) o Scaphoid, lunate, triquetrum, pisiform, trapezium (at the base of the thumb), trapezoid, capitate, hamate Possible Questions Which of the following is true regarding chamberlain's line? Dot on hard palate and back of foramen magnum Very good if you have tomography available * These notes are not all inclusive – make sure you read the assigned material and know the cancer chart as gone over in class DX Imaging MT Notes 7 of 16 It is harder to draw than McGreggor's line McGreggors line - uses back of hard palate and you are looking for a sliver of bone that divides the oropharynx and nasopharynx to the base of the occiput. Never found an author that is not concerned about the odontoid being over 10cm above McGreggors line. Which of the following is true with regard to Hadley's "S" curve? Done on lumber films May be used for AP and oblique views Some fill in the blank, short answer. MC, 4-5 hard ones, on the TEST coming soon. Seven Categories of bone disease (VICTANE) ***** V - (Vascular) Hematologic I - Infections C - congenital T - Trauma A - Arthritis N - Neoplasm (tumor) E - Endocrine, metabolic, nutritional Predictor Variables (7.3 or 7.4) Analysis of the lesion Skeletal location Position within bone Site of origin Metaphyseal - tumor (do to slow blood flow) & infection Shape If round this is a bad thing Size Margination Sharply marginated lesion ( this usually means the thing is benign Cortical integrity Behavior of the lesion Pain? Pattern? Matrix Does it turn fibrous Periosteal response Periosteal lifting - in adult…not good Soft tissue changes Broad, displacement of muscle, sub periosteal bleed May lead to look at joints in RA * These notes are not all inclusive – make sure you read the assigned material and know the cancer chart as gone over in class DX Imaging MT Notes 8 of 16 Joint Changes Preliminary Analysis Clinical data: age, sex, race, history Reiter’s syndrome - 50:1, Men:Women Number of lesions Symmetry of lesions Systems involved Supplementary analysis Other radiologic procedures Laboratory examination Biopsy Osteolytic, osteoblastic, or both Osteolytic Geographic lesion Solitary, greater than 1 cm, sharp margin Permeative lesion - pinhole destruction Multiple, lass than 1mm, imperceptible transition Motheaten lesion Multiple, 2-5mm, ragged margins and coalescence (merge borders) Osteoblastic behavior Diffuse lesion Localized lesion KNOW THE CHART ON AGES and CANCER (7.5) p695 Aggressive vs. Benign Aggressive Primary vs. Secondary/metastasis Primary Larger size Monostotic Cortical destruction Spiculated (sunburst) periosteal rxns also…(solid, codmans, laminated) Motheaten or permeative Imperceptible margins Soft tissue Mass Some matrix Secondary Larger size Polystotic Cortical destruction NO periosteal rxns Motheaten or permeative Imperceptible margins No matrix * These notes are not all inclusive – make sure you read the assigned material and know the cancer chart as gone over in class DX Imaging MT Notes 9 of 16 Benign Discovered early usually Found incidentally usually Smaller size Monostotic None, solid, laminated, codmans (all types of periosteal rxns) Geographic lesion Sharp Margins Thick Matrix Age, Size, Monostotic (one place), Polystotic (multiple places), Cortical destruction, periosteal rxns (Solid, Laminated, Spiculated, Codman's), Destruction (geographic, motheaten, permeative), Margins (sharp, imperceptible), Matrix, Soft tissue mass, Joint space Infections - do not respect anything, go through everything, effects joint space Tumor - will respect some things and usually does not affect joint space Panorex View a piece of film that has been curved This used to only be found in the ER Plain Film strengths Availability Relatively low cost Well known usage's Entry level diagnostic tool Search for contraindications to further imaging Quick assessment of gross osseous and soft tissue integrity Plain film weakness Ionizing radiation Just be present that you are putting radiation into someone's body Relatively poor resolution (50% of bone must not be present to show on the plain film as a loss of bone) Poor spatial localization Soft tissues generally not seen Frequently fail to document fractures, even under ideal conditions Plain Film study may be limited by: Poor patient positioning Patient motion This is with any radiographic tech Incomplete series * These notes are not all inclusive – make sure you read the assigned material and know the cancer chart as gone over in class DX Imaging MT Notes 10 of 16 Trauma patients, the elderly may not be able to cooperate during the exam C1-C2 region tough to evaluate C6-C7 region also tough to evaluate Lower lumbars are also hard to shoot through Weak chemistry and additional errors can cause problems Plain film proper use Introductory study Can evaluate intervertebral foramen well Use to rule out contraindications for advanced imaging Metal present…no MRI Not good for central canal stenosis Tomography - this type of film is missing some of the anatomy that should normally be present. Linear Circular Elliptical Hypocycloidal Trispiral 9.5 is centimeters above the table (this number is on the lower corner of the Tomography. This was not a CT though. Myelography Air was the 1st contrast agent used This caused headaches if the air got into the brain. Other materials include poppy seed oil, pantopaque Slow movement, thick oils. However, not soluble in water so all of it had to be removed after study was completed. In the 1940's water soluble products (very toxic) 1970 metrizamide non-ionic, water soluble, in use today Arachnoiditis was a common effect of the very toxic products Complications Arachnoiditis Infections - if the inject site does not get better , then infection is a probable cause Arterial bleeding Headache is the most common complication - due to puncture of the dura and getting blood into the CSF If they are getting a CT myelogram, make sure they take someone to go with them. Image production Utilizes ionizing radiation Depends on displacement of contrast * These notes are not all inclusive – make sure you read the assigned material and know the cancer chart as gone over in class DX Imaging MT Notes 11 of 16 Differential absorption Image Capture Video, plain film, Proper use of myelography If CT or MR are not available Patient who cannot undergo MRI because of time, size, claustrophobia, other contraindications (metal) May be used in conjunction with CT CT myelogram When injecting the fluid you would want to put it in the lumbar L4 or so to avoid the conus medularis Most sensitive in finding the true positive in disc herniation Myelography Weakness Ionizing Radiation Relatively Poor Resolution Soft Tissues Not Well Seen High Rate of False Negatives Potential Complications from Contrast Film Bone Scan Use a phosphate compound of some kind (phosphate is integral to bone formation and destruction Osteoblastic activity is detected with this study The hottest spots will be at the growth plates and at the sites of fracture repair, fracture can be hot for up to 18 months Whole body dose even if a regional bone scan Phases of bone scan Radionuclide - providing a dose that is using a carrier molecule to the place that you are looking at. In this case it is the bone. You inject this into a vein, starting the vascular phase. It will then start going into the bone after it goes through the heart and into the arteries. Anywhere there is osteoblastic activity this is laid down. Lytic Cancers will show up as a hot spot When a hot spot there is positive osteoblastic activity Computerized Tomography Technical Aspects Ionizing radiation Image based on absorption differentials Computer generated pictures Hounsfield Unit (the color that the pixel takes) Pixels (surface) * These notes are not all inclusive – make sure you read the assigned material and know the cancer chart as gone over in class DX Imaging MT Notes 12 of 16 Voxel (true representation of the anatomy) Volume Averaging Slice Thickness Scout Films (first film shot to determine thickness) 16 shades of grey in the CT scan CT Strengths Widely Available Improved Visualization of Soft Tissues Can Provide three dimensional Imaging Image Manipulation possible May be combined with myelography Accurately measure a variety of structures CT Weakness Higher cost Ionizing radiation Intracranial artifacts Artifacts secondary to metallic Dose is a consideration CT Proper use Very good axial images Some application in the neurology work up Excellent bone detail Although MR imaging is fast becoming the dominant modality for cross sectional musculoskeletal imaging, the availability, speed, and versatility of CT continue to make it a mainstay in emergency NMS imaging. When a plain film isn't enough, CT can often delineate additional findings that lead to the correct diagnosis and triage Helical CT SPECT / Pet Scan Single photon emission computerized tomography (SPECT) This makes layers out of a bone scan image Positron emission tomography (PET) MRI Technical Aspects Magnetic Resonance Imaging Technologies developed from nuclear resonance which is used to Evaluate Chemical Composition of Laboratory Samples Raymond Damadin First produced a Full body MR image in 1976 Radiofrequency (RF) coils Placed on or near the area of interest Used to excite target tissue * These notes are not all inclusive – make sure you read the assigned material and know the cancer chart as gone over in class DX Imaging MT Notes 13 of 16 Also receives information regarding Hydrogen Nuclei Relaxation There are different kinds for each body part. They are expensive too. Image Production Hydrogen is a charged particle representing 80% of all the atoms in the body Hydrogen behaves like a small bar magnet They are randomly orientated and their charges cancel out The MR scanner can spatially locate hydrogen within the body In the strong magnetic field of the MR Unit, the hydrogen molecules tend to align with (or less often against) the field Dr. Kuhn does not really see any issues with using MR, but does not agree totally that there is no risk. There is no such thing as a free lunch. The hydrogen molecules are not held static, but are induced to demonstrate precession (wobble) They are aligned with the magnetic field A strict linear relationship between the MR magnetic field The larmor equation forms the foundation for MR imaging Resonance Energy must be added to the system RF identical to the larmor frequency is pulsed into the patient. This is the concept of resonance. This causes the aligned hydrogen atoms to precess in phase. The RF pulse is turned off and the "excited" hydrogen atoms undergo "relaxation". This release of excess energy is in the form of RF and specialized antenna (surface coils) receive the input. Tremendous computer power is now brought to bear and an image is reconstructed. Imaging techniques The appearance of the image on an MR study is directly related to the signaling hydrogen. High signal intensity appears bright and Dark areas represent areas of low signal intensity. Intensity of the signal is determined by the quantity of mobile hydrogens and two magnetic relaxation times. T1 and T2 Manipulating the repetition of administered RF pulses (repetition times, TR) And collection of the emitted RF signal (echo time TE) This is how we recognize the difference between T1 and T2 MR pulsing sequences T1 = Short TR and Short TE T2 = Long TR and Long TE Proton = Long TR and Short TE T1 protocols utilized TR's of 200-600 milliseconds approximately TE's lasting approximately 25 milliseconds T2 images are very time consuming protocols and have long TR's and long TE's * These notes are not all inclusive – make sure you read the assigned material and know the cancer chart as gone over in class DX Imaging MT Notes 14 of 16 Hybrid images have been developed to take advantages of T2 type images with greater economy of time MRI strengths Superior resolution Superior tissue contrast Images soft tissue very well Non contrast enhancement in the spinal canal Axial images OK Coronal, sagittal, etc. Images are superior MRA can produce Non contrast visualization of major and minor vessels Measurements may be accomplished MR reports on the physiology as well as anatomy Not reliant on attenuation of ionizing radiation No known harmful effects Cheat Sheet handed out. MT known what is MR or CT Final and next TRI known T1 T2 and so forth Fat bright on T1 and not really available on T2 Nucleus pulposes is blank on T1 Air is black on both Cortical bone will be black on T1 and T2 THE STUFF ABOVE IS SOME STUFF FROM THE CHART, BUT DO NOT MEMORIZE THE CHART. MRI Contraindications Pace makers - not that it is made of ferris metal, but can it operate under the magnetic field Ear implants Miscellaneous implanted electronic devices - insulin pumps Cerebrovascular clips Machine shop workers Claustrophobia Orthopedic implants (distorts Gaussian field) MRI contrast Non-iodinated: adverse reactions very rare Magnetic contrast agents Gadolinium is the most common agent Works as a T1 shortening agent which causes tissue containing gadolinium to appear bright on T1 Very useful in cases of CNS Tumor Multiple sclerosis Disc herniation vs. Scar tissue * These notes are not all inclusive – make sure you read the assigned material and know the cancer chart as gone over in class DX Imaging MT Notes 15 of 16 Fasting imaging protocols in MRI IMPROVE o Until recently the utility of MR in trauma has been limited by cost, availability, and the data acquisition time o Rapid imaging is now more available and these units are increasingly being located near the ER. Improved software and hardware threaten to alter current practices despite the stranglehold of insurers o 1.5 Tesla magnet is considered the minimum o More widely accepted in extremity trauma o Many authors believe that MR should be used with more regularity in the acutely injured spine ST injury more likely to be identified o Any case presenting with neurological signs should be examined by MR This is the best use for MR Know that MRA is for head injury and vascular stuff MRA (Magnetic Resonance Angiogram) NO contrast HUGE ADVANTAGE fMRI (functional MRI) Blood Oxygenated Level Dependent (BOLD) imaging Physiologic Processes may be observed Cortical activation Look at how the brain responds to stimulation Retinoptic organization of the visual cortex Saw how the back of the cortex lights up when using the eyes Cerebral basis for language Mapping of the motor cortex Memory Study psychiatric disorders fMRI advantages over PET scan Lack ionizing radiation Less expensive Widely available Studies can be frequently repeated ABC's of Quality Control Anatomy - is the entire region depicted on the radiograph Bone - search for signs of patient motion and evaluate technique Cartilage - reminds us to look into the various joint spaces which may become obscured by positioning errors Arthritis, lines, joint spaces Soft tissues - helps evaluate technique and signs of injury or pathology * These notes are not all inclusive – make sure you read the assigned material and know the cancer chart as gone over in class DX Imaging MT Notes 16 of 16 Collection of blood, tumors ABC's of interpretation Anatomy - look closely at the vertebrae subinventory Bone - cortical and trabeculae destruction Cartilage - decreased joint space, arthritis Soft tissue - looking for things that are obliterated or mass objects such as cancer Know background thinking of where X ray will fit into your practice. Could I use X-ray to help determine the diagnosis What view do we use to look at IVF's = oblique view 1. Which of the following imaging modalities allows for manipulation of the image to enhance or suppress bone detail using the information stored on a computer disc? 2. Which of the following is a feature of benign lesions? 3. Which of the following is true regarding hadley's S curve? 4. Which is most likely to be associated with lesions in multiple areas 5. Which imaging modalities uses the patient as the emitter? a. Photons - bone scan b. Protons - MRI 6. 3D imaging best done in the coronal plane - MRI 7. CT - best for bone and taken in sagittal position 8. Bone scan - infection, fracture, pathology (osteoblastic activity) 9. How do you tell MRI from CT? Look at the cortex of bone Slide Exam is timed and in the first hour NO QUESTIONS 25 questions 15 MC 10 Fill in the blank X-ray anatomy, structure, types, lines and what they mean Written Exam 4th hour Tuesday * These notes are not all inclusive – make sure you read the assigned material and know the cancer chart as gone over in class