* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Perfusion characteristics of late radiation injury of parotid glands
Backscatter X-ray wikipedia , lookup
Proton therapy wikipedia , lookup
Medical imaging wikipedia , lookup
Nuclear medicine wikipedia , lookup
Neutron capture therapy of cancer wikipedia , lookup
Industrial radiography wikipedia , lookup
Radiation therapy wikipedia , lookup
Radiosurgery wikipedia , lookup
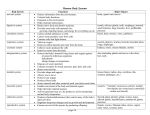
Radiation burn wikipedia , lookup
Eur Radiol (2009) 19: 94–102 DOI 10.1007/s00330-008-1104-9 HEAD AN D NECK Chun-Jung Juan Cheng-Yu Chen Yee-Min Jen Hua-Shan Liu Yi-Jui Liu Chun-Jen Hsueh Chao-Ying Wang Yu-Ching Chou Yao-Te Chai Guo-Shu Huang Hsiao-Wen Chung Perfusion characteristics of late radiation injury of parotid glands: quantitative evaluation with dynamic contrast-enhanced MRI Received: 11 December 2007 Revised: 28 May 2008 Accepted: 5 June 2008 Published online: 26 July 2008 # European Society of Radiology 2008 Y.-J. Liu Department of Automatic Control Engineering, Feng Chia University, Taichung, Taiwan C.-J. Juan . C.-Y. Chen . H.-S. Liu . C.-J. Hsueh . C.-Y. Wang . G.-S. Huang . H.-W. Chung Department of Radiology, Tri-Service General Hospital and National Defense Medical Center, Taipei, Taiwan, Republic of China Y.-M. Jen Department of Radiation Oncology, Tri-Service General Hospital and National Defense Medical Center, Taipei, Taiwan, Republic of China H.-S. Liu . C.-Y. Wang . H.-W. Chung (*) Department of Electrical Engineering, National Taiwan University, No. 1, Sec. 4, Roosevelt Road, Taipei, Taiwan, 10764, Republic of China e-mail: [email protected] Tel.: +886-2-33663628 Y.-C. Chou School of Public Health, National Defense Medical Center, Taipei, Taiwan Y.-T. Chai Section of General Surgery, Department of Surgery, Hualien Armed Forces General Hospital, Hualien, Taiwan Abstract We aimed to quantitatively investigate the alteration of parotid perfusion after irradiation using dynamic contrast-enhanced magnetic resonance imaging (DCE-MRI) based on a two-compartment tracer kinetic model. This study enrolled 19 patients (53.2±14.9 years) treated by head and neck radiotherapy and 19 age-relevant and sex-matched subjects as a control group. Perfusion parameters (Kel, k21 and A) of parotid glands were analyzed based on the Brix model from T1-weighted DCE-MRI. Suitability of Introduction Parotid glands are highly radiosensitive. Occurring within 24 h after irradiation, early radiation injuries of the parotid glands are known as acute radiation parotitis, manifesting fever, dry mouth, pain, swelling and tenderness clinically [1]. Late radiation injuries of the parotid glands usually the Brix model was evaluated via Monte Carlo simulation for the goodness-of-fit. Analysis of nonlinear goodness-of-fit showed that the Brix model is appropriate in evaluating the parotid perfusion (R2 =0.938±0.050). The irradiated parotid glands showed significantly lower Kel (P<0.0005) and k21(P<0.05) and consequently significantly higher value of peak enhancement (P<0.0005) and time-topeak (P<0.0005) compared with nonirradiated ones, suggestive of gradual and prolonged accumulation and delayed wash-out of contrast agent due to increased extracellular extravascular space and decreased vascular permeability in the irradiated glands. Linear regression analysis showed dose-dependent perfusion changes of the irradiated parotid glands. We conclude that quantitative DCE-MRI is a potential tool in investigating parotid gland perfusion changes after radiotherapy. Keywords Radiation injury . Parotid glands . Magnetic resonance imaging . Perfusion present as transient or permanent xerostomia, which further increases the risk for developing dental caries, compromises the oral mucosal integrity, and results in oral pain, loss of taste, difficulty with swallowing and chewing, sleep disorders and worse quality of life [2]. Sialometric studies disclose reduction of salivary flow in the acute setting [3] as well as in the late stage [3, 4] after head and neck 95 radiation. On histopathological studies, acute radiation injuries present as swelling, degeneration and necrosis of acinar cells [5], while late radiation injuries further demonstrate loss of acinar cells, dilatation of intercalated ducts, fibrosis and atrophy of parotid lobules [4, 5]. The functional impairment and morphological damage of the parotid glands can persist as long as 24 months after the irradiation [3]. Furthermore, the severity of acinar loss has been positively correlated with the radiation dose in the late stage. The parotid glands recover well without residual damage after low-dose irradiation (2.5 Gy). A radiation dose of 7.5 Gy [5] and 20 Gy [6] leads to slight loss and marked reduction (50% in number) of acinar cells, respectively. When the radiation dose reaches as high as 45 Gy, only 10% of acini survive [6, 7]. Although the severity of xerostomia can be assessed by the Radiation Therapy Oncology Group (RTOG) criteria [8] or by measuring the salivary flow, for example using the Saxon’s test [9], these clinical observations do not depict any morphological or physiological change of the irradiated parotid glands. On the other hand, histopathological study has a major disadvantage in its invasiveness, which makes it an impractical tool to quantify the radiation injuries of human parotid glands. Under this situation, imaging studies unavoidably play an important role for in vivo and noninvasive investigation of the morphological and physiological changes of the irradiated parotid glands. Contrastenhanced computed tomography (CT) and MR studies have been used worldwide for diagnosing and monitoring the response of treatment for head and neck cancer by providing satisfactory morphological information of the head and neck structures. The irradiated parotid glands appear swollen on both CT and MR and show high T2 signal on MR images at an early stage and later become smaller and exhibit low T1 and T2 signal [10]. Following intravenous administration of contrast medium, the irradiated parotid glands often show strong enhancement on CT and MR images [11–13] before visually perceivable volume reduction [13, 14]. These qualitative contrast-enhanced imaging features are suggestive of alterations in parotid perfusion characteristics after radiotherapy. In other words, it seems plausible that the parameters of perfusion characteristics could be used as quantitative indices of radiation-induced injury of parotid glands. Dynamic contrast-enhanced magnetic resonance imaging (DCE-MRI) has the capability to exploit tissue perfusion properties [15–18] via quantitative analysis using appropriate tracer kinetics models [19]. To the best of our knowledge, the perfusion characteristics of the irradiated parotid glands using DCE-MRI have not been documented. Therefore, in this preliminary study we applied DCE-MRI to investigate the perfusion changes of the parotid glands following irradiation. Specifically, we hypothesized that the perfusion alterations due to irradiation are dosage dependent and that the physiological mechanism causing the difference in perfusion alterations could be explored using quantitative analysis. By applying DCE-MRI, the physiological changes of the irradiated parotid glands can be further assessed without additional injection of contrast agent compared to the conventional contrast-enhanced MRI. Materials and methods Subjects From January 2006 to April 2006, 19 subjects who had undergone radiotherapy (radiotherapy group) and 19 agerelevant and sex-matched subjects who had not experienced radiotherapy (control group) received perfusion-weighted head and neck MR imaging with contrast administration in our hospital. These subjects all gave written informed consent before the MR examinations. The clinical indications for contrast-enhanced MR investigation in these patients included clinically suspicious malignancy and post-treatment follow-up of previously known head and neck malignancy. The radiotherapy group consisted of 16 men and 3 women (aged 53.2±14.9 years) who had received radiation therapy for head and neck cancer before the MR study. The radiation dose delivered to the head and neck tumors was 68.5±4.6 Gy using intensity-modulated radiation therapy (IMRT) in 14 cases and 3D conformal radiotherapy (3DCRT) in 2 cases. The mean total cumulative dose to the parotid glands was 36.0±15.9 Gy. The details of clinical data, including the gender, age, primary tumor site, the time interval after radiotherapy (called RT-to-MR interval in this paper), initial and current grade of dry mouth, and radiation dose to either parotid gland of the radiotherapy group are listed in Table 1. The control group was comprised of 16 men and 3 women (aged 49.4±16.7 years) who had not received radiation therapy, including 7 cases with negative results and 12 cases with fresh head and neck malignancy in areas other than the parotid glands (nasopharyngeal carcinoma in 4, buccal cancer in 3, oral tongue cancer in 3, palatine tonsil cancer in 1 and thyroid cancer in 1). Because of the use of parotid-sparing radiotherapy techniques (IMRT and 3DCRT), the parotid glands on either side received different radiation doses according to the specific location of the primary head and neck malignancy. Hence, the glands in each subject were treated as two different glands in our study. Clinical assessment of dry mouth Clinically, the severity of dry mouth was assessed and classified by a radiation oncologist (Y.M.J.) based on the RTOG scoring criteria [8]: Grade 0 represented no symptom of dry mouth; grade 1 described slight dryness of mouth with good response on stimulation; grade 2 portrayed moderate dryness with poor response on stimulation; grade 3 stood for complete dryness with no response on stimulation; grade 4 characterized necrosis of the salivary glands. The total of 19 patients (38 glands) was further classified as low-grade dry 96 Table 1 Clinical data of the radiotherapy group No. 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 Gender M M M M M F M M M F M M M M M M M F M Age (years) 54 53 74 59 45 50 34 27 56 53 64 53 74 62 57 24 34 71 68 Tumor site NP OP HP HP NP NP Oral NP Sinus NP Oral HP NP OP NP NP NP NP NP RT-to-MR interval (month) 7 13 10 2 36 37 2 23 4 3 24 2 16 26 20 43 13 17 25 Dry mouth grade (RTOG criteria) RT dosage (Gy) Initial Current Right Left 2 2 3 2 1 1 2 2 1 2 1 2 2 2 2 2 2 2 2 2 1 3 2 0 1 2 0 1 1 1 1 1 2 2 0 1 2 2 39.4 41.7 44.3 46.0 21.4 24.3 37.9 30.0 0.7 61.6 45.6 39.1 65.1 31.0 54.2 53.8 32.1 40.8 36.5 40.2 40.7 38.2 42.7 22.4 20.5 43.8 24.6 1.5 51.9 48.1 35.0 39.5 71.3 48.3 30.5 29.2 37.6 37.3 Gender (M: male; F: female), tumor site (NP: nasopharynx; OP: oropharynx; HP: hypopharynx). Eight of 19 patients showed downgrading of dry mouth at the time of MR study, while 11 remained unchanged mouth subgroup (grade 0 and grade 1) and high-grade dry mouth subgroup (grade 2 to grade 4). Dynamic MR image acquisition Axial dynamic contrast-enhanced perfusion-weighted MR images were obtained on a 1.5-T MR system (ECLIPSE, Philips Medical System, Cleveland, OH) using a multi-slice 2D T1-weighted fast spin-echo sequence with a field-ofview of 230 mm, matrix of 256×256, slice thickness of 5 mm, slice number of 6 and TR/TE of 372/12. A total of 20 dynamic phases at an interval of 10.4 s were acquired with a total data acquisition time of 208 s. A 20-G catheter was inserted into the antecubital vein before MRI. GadoliniumDTPA was manually injected as a bolus over a period of 3 s with the standard dose of 0.1 mmol/kg of patient weight. The RT-to-MR interval between the completion of radiotherapy and DCE-MRI study was 17±12.7 months. using Matlab (MathWorks, Natick, MA). Regions of interest (ROIs) were manually drawn on the parotid gland. All imaging processing, ROI drawing and data analysis were performed by C.J.J., who is a neuroradiologist with 6 years’ experience in head and neck imaging interpretation and has obtained a Ph.D. in electrical engineering. The signal-time data (SIt) were first normalized to be converted to concentration-time data (Ct) based on the following relationship [16, 17]: Ct / The MR image data were digitally transferred to a personal computer from the MR operating console and then processed by software developed in-house (by C.J.J.) (1) where SI0 is the baseline signal intensity of the parotid glands before contrast administration. The concentration time data were fitted, by means of a non-linear least square curve fitting algorithm, to the two-compartment Brix pharmacokinetic model [19] as shown in Eq. (2). Ct ¼ Data analysis SIt SI0 SI0 A eKelt ek21t k21 Kel (2) where A is an amplitude scaling constant for the concentration-time curve of the plasma, which is determined by factors including the injected dose of contrast agent, the 97 blood volume of the parotid gland and so forth [16, 17]. Kel is an elimination transfer rate constant that describes the excretion of contrast agent through the kidneys, and k21 is a transfer rate constant that describes the return of contrast agent from the extracellular extravascular space (EES) of parotid tissue to the plasma compartment. Goodness-of-fit was assessed by R2 values used in nonlinear curve fitting [20]. Following curve fitting, the analytical concentrationtime relationship was used to derive three indices: The peak enhancement (Cmax) was defined as the maximal value of contrast agent concentration, the time-to-peak (Tmax) was defined as the time duration to reach Cmax, and the slope of the wash-in phase was defined as Cmax/Tmax. Error assessment Possible error due to the finite temporal resolution of 10.4 s in the estimation of perfusion parameters was assessed using Monte Carlo simulation at different levels of additive noise. For this purpose, an analytical Gd-DTPA concentration-time curve obtained from one healthy subject was first taken as the true reference curve, with the values of the perfusion parameters recorded. The reference curve was then sampled at the interval of 10.4 s. Subsequently, Gaussian white noise was added to the concentration-time data at ten different signal-to-noise ratio (SNR) levels ranging from 5 to 50, with each SNR level containing 1,000 sets of random noise. Nonlinear least-square-error fitting to the Brix model was performed on these simulated data to derive three perfusion parameters (A, k21, Kel), with errors expressed as percentage deviation from the true values. enhancement and time-to-peak. Fisher exact test was used to test the dependence between the two categorical variables (radiotherapy or not vs. gender distributions; perfusion parameters vs. radiation doses between two glands in the same patient). For these analyses, a P value<0.05 was considered as statistically significant. Results Good curve fitting of the concentration-time data was achieved in all subjects. The R2 values were 0.951±0.053 in the radiotherapy group and 0.925±0.044 in the control group, respectively, suggesting that the use of the Brix model is appropriate in curve-fitting the parotid perfusion data. For the image acquisition protocol used in our study, SNR of the concentration enhancement time curve was at the level of about 30 in all subjects, corresponding to imprecision of −0.93±7.84%, −1.25±9.44% and 5.14± 29.16% for A, Kel and k21, respectively. Among all perfusion parameters, k21 was most susceptible to noise and carried the largest error range. The radiotherapy group did not differ from the control group regarding the age (P=0.25) or gender (P=1). The binary logistic regression analysis demonstrated a statistically significant relationship between the radiation dose and the peak enhancement (P=0.009; odds ratio=7.84), the amplitude scaling constant A (P=0.005; odds ratio=7.84) and the kel (P=0.002; odds ratio=30), within the same subjects. Correlation between the perfusion parameters and radiation dose (and RT-MR interval) Statistical analysis Linear regression analysis was performed to evaluate the correlation between the changes of perfusion parameters and radiation doses, and the correlation between the changes of perfusion parameters and the RT-to-MR interval. Difference in perfusion parameters among the dry mouth subgroups, as well as other group comparisons, was examined using Student’s t test. Since multiple hypotheses were tested simultaneously regarding changes in the perfusion parameters derived from DCE-MRI, Bonferroni correction was used when assessing possible statistical significance, i.e., a P value < 0.05/3=0.017 was considered as statistically significant. Binary logistic regression analysis was executed to investigate the dependence of the perfusion changes on the radiation doses between the two parotid glands in the same patient. The parotid gland was coded as 1 for the higher radiation dose and 0 for lower radiation dose. The perfusion changes were coded as 1 for lower k21 and Kel and higher value for peak enhancement and time-to-peak, and were coded as 0 for higher k21 and Kel and lower value for peak The peak enhanced T1-weighted images and percent signal enhancement-time curves of the irradiated and controlled parotid glands were demonstrated (Fig. 1). The correlations between the radiation doses and changes in perfusion parameters and between the RT-to-MR interval after radiation and changes in perfusion parameters assessed by linear regression are shown in Table 2. The scatter plots of perfusion parameters (peak enhancement, time-to-peak and Kel) versus radiation dose were illustrated (Fig. 2). While the radiation doses positively correlated with the peak enhancement (P=0.009; R=0.418), time-to-peak (P=0.0017; R= 0.491) and negatively correlated with the Kel (P=0.0008; R= 0.521) significantly, the RT-to-MR interval did not correlate with the perfusion parameters significantly except marginally for the k21 (P=0.011; R=0.407). Effect of dry mouth on the perfusion parameters With regard to the severity of dry mouth at the time of MR study, the low-grade dry mouth subgroup consisted of 11 98 Fig. 1 Peak-enhanced T1weighted images of irradiated (a) and control (b) parotid glands and their corresponding signal enhancement-time curves (c). Note the prominent enhancement in (a). Each of the signal enhancement-time curves represents the average value within one encircled region-ofinterest from a single subject, rather than the group average patients (3 cases in grade 0; 8 cases in grade 1), while the high-grade dry mouth subgroup consisted of 8 patients (7 cases in grade 2; 1 case in grade 3). The low-grade subgroup did not differ from the high-grade subgroup in Kel (0.0011±0.0010 s−1 vs. 0.0009±0.0009 s−1; P=0.54), k21 (0.082±0.035 s−1 vs. 0.062±0.035 s−1; P=0.09), peak enhancement (80.0±35.1% vs. 62.7±33.2%; P=0.13), time-to-peak (77.3±40.7 s vs. 101.3±56.2 s; P=0.16) and the amplitude scaling constant A (0.072±0.058 vs. 0.038± 0.029; P=0.02), but had statistically significantly higher value for the wash-in slope (1.08±0.34%/s vs. 0.70±0.40%/s; P=0.005). When comparing with the control group, the Table 2 Correlation between the radiation doses (and RT-to-MR interval) and perfusion parameters using linear correlation regression (y=y0+ax) Radiation dose (Gy) RT-to-MR interval (months) PE TTP k21 Kel PE TTP k21 Kel Correlation coefficient (R) y0 a P value 0.418 0.491 0.165 0.521 0.298 0.012 0.407 0.136 34.23 24.54 0.090 0.0022 86.67 88.15 0.0092 0.0008 1.01 1.65 −0.0904 −3.3×10−5 −0.82 −0.046 0.0004 9.9×10−6 0.0090* 0.0017* 0.32 0.0008* 0.069 0.943 0.011* 0.41 PE (peak enhancement); TTP (time-to-peak); * denotes a significant difference between the paired subgroups 99 low-grade subgroup had significantly lower Kel (P<0.005), insignificant changes in the amplitude scaling constant A (P<0.05) and consequently higher values for peak enhancement (P<0.005) with insignificant difference in time to peak (P<0.05). Likewise, the high-grade subgroup had significantly lower Kel (P<0.005), but not k21 (P<0.05), and consequently higher values for time to peak (P<0.01), but not higher for peak enhancement (P<0.05) than the control group. Effect of radiation on the perfusion parameters compared with control The radiotherapy group had significantly lower Kel (0.0010± 0.0009 s−1 vs. 0.0023±0.0011 s−1; P<0.0005) and k21 (0.073±0.036 s−1 vs. 0.102±0.088 s−1; P<0.05) than the control group (Fig. 3). The amplitude scaling constant A was higher in the radiotherapy group (0.057±0.051 vs. 0.041±0.034), but not significantly (P=0.26). Alterations in these perfusion parameters resulted in significantly higher values for the peak enhancement (72.7±34.9% vs. 38.7±13.1%; P<0.0005) and time-to-peak (87.4±48.6 s vs. 54.7±32.0 s; P<0.0005) consistent with the common observation of increased signal enhancement with contrast administration, with insignificant changes in the wash-in slope (0.92±0.41%/s) vs. 0.96±0.78%/s; P=0.45). Fig. 2 Scatter plots of peak enhancement (a), time-to-peak (b) and Kel (c) versus radiation dose. The dashed lines represent the 95% confidence bands, while the dotted lines represent the 95% prediction bands Fig. 3 Perfusion parameters of irradiated and non-irradiated parotid glands. The scales and units on the vertical axes are: ×10−1 for A, ×10−1 sec−1 for k21, ×10−3 sec−1 for Kel, ×1%. sec−1 for slope, and % for peak enhancement, sec for time-to-peak, respectively. Data are presented as mean + SD with P<0.05 (*) and P<0.0005 (**) being statistically significantly different as compared to the control group 100 Discussion Radiation injuries of the parotid glands include functional impairment, structural changes and physiological alterations. Clinically, the functional impairment of the irradiated parotid glands could be evaluated either by assessing the severity of xerostomia using RTOG scoring criteria [8] or by measuring the salivary flow [9]. However, the reduction of salivary flow and the symptom of xerostomia are attributed to dysfunction of the parotid and submandibular glands and therefore are not specific for the parotid gland injury alone. Although histopathological analysis provides a standard tool to characterize the microstructural damage of the irradiated parotid glands, it is not beneficial clinically owing to the invasiveness of biopsy, which might potentially endanger the facial nerves. Alternatively, the structural changes of the irradiated parotid glands could be investigated by cross-sectional imaging studies, such as CT and MR imaging. Prior CT studies have demonstrated increased enhancement of the irradiated parotid glands after intravenous contrast injection [11–13], implying that the parotid perfusion might alter after irradiation. Two assumptions have been made to explain the post-irradiated enhancement of parotid glands: One is that the radiation results in changes of vascular permeability; the other attributes the enhancement to the increase of EES secondary to acinar loss [12, 13]. The results from our dynamic MR imaging study show that the increased peak enhancement following contrast administration is predominantly determined by the significant alterations of Kel (the elimination transfer rate constant describing the wash-out of contrast agents) and k21, (the transfer rate constant describing the wash-in of contrast agents). The statistically significant decrease in the Kel is consistent with a continuous build up of Gd-DTPA from the blood vessels to the EES and its prolonged wash out, an outcome likely to originate from the increase of EES secondary to acinar loss under radiation exposure. On the other hand, the significantly lower k21 is suggestive of a decrease of permeability and slower exchange of GdDTPA between the plasma and EES, leading to significantly prolonged time-to-peak and contrast stasis in the EES. In other words, the decrease of vascular permeability and the increase of EES together explain how the postirradiated parotid glands enhancement is seen on conventional CT and MR images [11–13]. Moreover, the radiation dosage received by the parotid glands plays an important role in the perfusion change of post-irradiated parotid glands. Linear regression analysis reveals that the radiation doses are positively correlated with the peak enhancement (P=0.009, R=0.418) and timeto-peak (P=0.0017, R=0.491) and are negatively correlated with the Kel (P=0.0008, R=0.521) with statistical significance. The dose-dependent perfusion changes are consistent with results from literature reports investigating the functional loss of salivary glands using either direct measurement of salivary flow [3, 21] or 11C-methionine on positron emission tomography (PET) [22]. In particular, the PET study shows that the net metabolic clearance of 11Cmethionine correlates positively with the salivary flow, both of which reduce with increased radiation dose. The dose-dependent perfusion changes of Kel, suggesting increase of EES, are also consistent with the histopathological observations of acinar loss in animal studies, showing dose-dependent acinar loss [23, 24]. Regarding the relationship between the severity of dry mouth and the changes of perfusion parameters, our results show that both the low-grade subgroup (grade 0 and 1) and high-grade subgroup (grade 2 and 3) have significantly lower Kel (P<0.005) than the control group, again suggestive of an increase in EES secondary to acinar loss. Since the symptom of dry mouth is partly attributed to the functional impairment of the submandibular glands, which is beyond the scope of the current preliminary study, we suggest not over-interpreting the relationship between the severity of dry mouth and the parotid perfusion unless both parotid and submandibular glands are investigated together. One unique feature of our study is the quantification of parotid perfusion parameters that, to the best of our knowledge, has not been investigated before. While contrast-enhanced dynamic MR imaging has been previously applied to the parotid glands for the purpose of tumor differentiation [15, 18, 25], these approaches remain qualitative. A quantitative investigation using curve fitting to an appropriate model provides the important advantage that the underlying changes can be examined physiologically and that the influence of noise or finite sampling interval could be minimized. Certainly, sufficient SNR of the concentration time curves during image acquisition and proper choice of the perfusion model are two prerequisites for the validity of a quantitative study. In our case, good curve fitting of the concentration-time data could be achieved in all subjects with high R2 values (0.938±0.050), indicating appropriateness of the Brix model for use in the parotid glands. Analysis of the fitting errors at routine SNR (about 30 in our study) also gives satisfactory estimation accuracy for the perfusion parameters. Therefore, the effectiveness of the quantitative approach as shown in our study may shed light on the future use of DCE-MRI as a reliable tool to monitor the perfusion changes of the irradiated parotid glands and, for example, the value of radioprotection in new radiotherapy techniques or medications. One might question that a temporal resolution of 10.4 s seems insufficient in sampling the rapid wash-in kinetics, leading to a relatively large error range of k21 (±29%) in spite of good curve fitting. It could be remedied by using a gradient echo sequence with a short TR (about 11 ms) or using the parallel imaging technique, both allowing higher temporal resolution by shortening the image acquisition time. Nevertheless, the k21 already distinguished the radiotherapy group from the control group significantly in our study. 101 A prior study suggests that regeneration of acinar cells might occur after irradiation [23]; thus, the RT-to-MR interval may itself be a factor that needs to be controlled before ruling out the possibility of perfusion changes due to acinar regeneration. In our study, the possible relationship between the RT-to-MR interval and the perfusion changes were examined by linear regression analysis, showing that the RT-to-MR interval does not correlate with the perfusion parameters except only marginally for the k21 (P=0.011; R=0.407). The lack of strong correlation partly supports our hypothesis that the perfusion changes in parotid glands are more likely due to irradiation dosage. The broad RT-to-MR interval in our preliminary retrospective study, however, does not allow us to further characterize the perfusion changes related to the acinar regeneration. To answer this question, a prospective time-course study performed before radiotherapy and shortly and longer after radiotherapy would be required, which is currently under planning at our institute. In conclusion, our study shows that quantitative analysis of DCE-MRI with the Brix model is a potential tool investigating the perfusion characteristics of the parotid glands after radiotherapy. The dose-dependent change of perfusion parameters, including Kel, peak enhancement and time to peak, suggests that the persistent accumulation and delayed wash-out of the contrast agent at late stage of radiation injury reflects the increase of the EES of parotid glands. Acknowledgment The authors express gratitude to Miss Shih-I Tsao for MR data archiving and reference preparation. References 1. Cairncross JG, Salmon J, Kim JH, Posner JB (1980) Acute parotitis and hyperamylasemia following wholebrain radiation therapy. Ann Neurol 7:385–387 2. de Castro GJ, Federico MH (2006) Evaluation, prevention and management of radiotherapy-induced xerostomia in head and neck cancer patients. Curr Opin Oncol 18:266–270 3. Jen YM, Lin YC, Wang YB, Wu DM (2006) Dramatic and prolonged decrease of whole salivary secretion in nasopharyngeal carcinoma patients treated with radiotherapy. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 101:322–327 4. Li J, Shan Z, Ou G et al (2005) Structural and functional characteristics of irradiation damage to parotid glands in the miniature pig. Int J Radiat Oncol Biol Phys 62:1510–1516 5. Stephens L, King G, Peters L, Ang K, Schultheiss T, Jardine J (1986) Acute and late radiation injury in rhesus monkey parotid glands. Evidence of interphase cell death. Am J Pathol 124:469–478 6. Henriksson R, Frojd O, Gustafsson H et al (1994) Increase in mast cells and hyaluronic acid correlates to radiationinduced damage and loss of serous acinar cells in salivary glands: the parotid and submandibular glands differ in radiation sensitivity. Br J Cancer 69:320–326 7. Lotz S, Caselitz J, Tschakert H, Rehpenning W, Seifert G (1990) Radioprotection of minipig salivary glands by orciprenaline-carbachol. An ultrastructural and semiquantitative light microscopic study. Virchows Arch A Pathol Anat Histopathol 417:119–128 8. Cox JD, Stetz J, Pajak TF (1995) Toxicity criteria of the Radiation Therapy Oncology Group (RTOG) and the European Organization for Research and Treatment of Cancer (EORTC). Int J Radiat Oncol Biol Phys 31:1341– 1346 9. Kohler PF, Winter ME (1985) A quantitative test for xerostomia. The Saxon test, an oral equivalent of the Schirmer test. Arthritis Rheum 28:1128–1132 10. Shah GV (2004) MR imaging of salivary glands. Neuroimaging Clin N Am 14:777–808 11. Tartaglino LM, Rao VM, Markiewicz DA (1994) Imaging of radiation changes in the head and neck. Semin Roentgenol 29:81–91 12. Bronstein AD, Nyberg DA, Schwartz AN, Shuman WP, Griffin BR (1987) Increased salivary gland density on contrast-enhanced CT after head and neck radiation. AJR Am J Roentgenol 149:1259–1263 13. Rabin BM, Meyer JR, Berlin JW, Marymount MH, Palka PS, Russell EJ (1996) Radiation-induced changes in the central nervous system and head and neck. Radiographics 16:1055–1072 14. Nomayr A, Lell M, Sweeney R, Bautz W, Lukas P (2001) MRI appearance of radiation-induced changes of normal cervical tissues. Eur Radiol 11:1807– 1817 15. Yabuuchi H, Fukuya T, Tajima T, Hachitanda Y, Tomita K, Koga M (2003) Salivary gland tumors: diagnostic value of gadolinium-enhanced dynamic MR imaging with histopathologic correlation. Radiology 226:345– 354 16. Buckley DL, Kerslake RW, Blackband SJ, Horsman A (1994) Quantitative analysis of multi-slice Gd-DTPA enhanced dynamic MR images using an automated simplex minimization procedure. Magn Reson Med 32:646–651 17. Larsson HB, Stubgaard M, Frederiksen JL, Jensen M, Henriksen O, Paulson OB (1990) Quantitation of blood-brain barrier defect by magnetic resonance imaging and gadolinium-DTPA in patients with multiple sclerosis and brain tumors. Magn Reson Med 16:117–131 18. Ikeda M, Motoori K, Hanazawa T et al (2004) Warthin tumor of the parotid gland: diagnostic value of MR imaging with histopathologic correlation. AJNR Am J Neuroradiol 25:1256–1262 19. Brix G, Semmler W, Port R, Schad LR, Layer G, Lorenz WJ (1991) Pharmacokinetic parameters in CNS Gd-DTPA enhanced MR imaging. J Comput Assist Tomogr 15:621–628 20. Bates D, Watts D (1988) Nonlinear regression analysis and its applications: Wiley:33–66 21. Munter MW, Karger CP, Hoffner SG et al (2004) Evaluation of salivary gland function after treatment of head-andneck tumors with intensity-modulated radiotherapy by quantitative pertechnetate scintigraphy. Int J Radiat Oncol Biol Phys 58:175–184 102 22. Buus S, Grau C, Munk OL, Bender D, Jensen K, Keiding S (2004) 11Cmethionine PET, a novel method for measuring regional salivary gland function after radiotherapy of head and neck cancer. Radiother Oncol 73:289– 296 23. Gustafsson H, Franzen L, Henriksson R (1995) Regeneration of parotid acinar cells after high radiation doses. A morphological study in rat. Acta Oncol 34:193–197 24. Radfar L, Sirois D (2003) Structural and functional injury in minipig salivary glands following fractionated exposure to 70 Gy of ionizing radiation an animal model for human radiationinduced salivary gland injury. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 96:267–274 25. Suenaga S, Indo H, Noikura T (2001) Diagnostic value of dynamic magnetic resonance imaging for salivary gland diseases: a preliminary study. Dentomaxillofac Radiol 30:314–318