* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download ERYTHEMA MULTIFORME MAJOR: CASE REPORT AND REVIEW
Survey
Document related concepts
Transcript
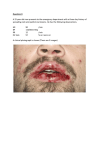
Sathawane et. al : Erythema Multiforme Major : Case Report and Review ERYTHEMA MULTIFORME MAJOR: CASE REPORT AND REVIEW OF LITERATURE Dr. R. S. SATHAWANE1, Dr. SAMIKSHA TRIPATHI2, Dr. ABHIJEET DEOGHARE3 1. PROFESSOR, HEAD OF DEPARTMENT, Department of Oral Medicine and Radiology 2. POST GRADUATE STUDENT, Department of Oral Medicine and Radiology 3. READER, Department of Oral Medicine and Radiology CHHATTISGARH DENTAL COLLEGE AND RESEARCH INSTITUTE, RAJNANDGAON (C.G.), INDIA. ADDRESS FOR CORRESPONDENCE Dr. Samiksha Tripathi, D/o Chandra Kant Tripathi, Manager, Ultratech Cement, QTR No.- 3064, Grasim Vihar, Rawan, Dist - Baloda Bazar, Chhattisgarh. Pincode – 493196. Email id – [email protected] Phone no. – +919009904195, +919826725406 ABSTRACT Erythema multiforme is an acute mucocutaneous disorder that occurs with varying degrees of blistering and ulceration. We report a case of major erythema multiforme managed with systemic steroids. A 45-year-old male had cutaneous target lesions and ulcerative lesions throughout the oral cavity and lips, which had been diagnosed as erythema multiforme major. This episode was related to neither drug intake nor herpetic infection, which suggests that the erythema multiforme was of idiopathic origin. This hypothesis was supported by negative serology for herpes simplex virus. Excisional biopsy of an intact bulla was performed and the diagnosis was confirmed as erythema multiforme major. The patient was treated with Prednisolone in a tapering dose for 2 months to control and completely cure the disease. Key-words: Erythema multiforme, Immune disorder, Target lesion. INTRODUCTION Erythema multiforme (EM) is a rare, acute immune-mediated mucocutaneous disorder, a widespread hypersensitivity reaction, caused by the appearance of cytotoxic T lymphocytes in the epithelium that induce apoptosis in keratinocytes, leading to satellite cell necrosis.1 Despite being frequently caused by, or at least associated with, infection or drug therapy, the pathogenic mechanism of EM stays vague, and as a result there are no evidence-based, reliably effective therapies. Oral manifestations may occur independently or precede cutaneous involvement.2 The present article discusses a case of 45-year old male who was clinically and histopathologically diagnosed as erythema multiforme and reviews aspects of EM as relevance to dental practice. CASE HISTORY A 45-year old male patient presented to the outpatient department of our institute with complains of painful oral ulceration and hemorrhagic crusts on the lips. History revealed that complaints started around 2 months back. International Journal of Innovations in Dental Sciences / December 2016 / Vol 1 / Issue 1 13 Sathawane et. al : Erythema Multiforme Major : Case Report and Review Initially there was erythema in the oral cavity and over lips, due to which patient experienced burning and pain during mastication. Pain was gradual in onset, moderate to severe in intensity, continuous in duration, aching type. There was no history of referred/radiating pain. Soon vesicles and ulcers appeared at these sites. Vesicles first appeared on lips, buccal mucosa bilaterally, followed by hard palate and then onto tongue and upper and lower labial mucosa. Vesicles ruptured to form encrustations over lips. History of itching and burning sensation present in the perioral region. Also history of dysphonia, odynophagia and dysarthria was present. No history of any concomitant symptoms associated with pain nor febrile episode was present. There was no history of any drug intake before the onset of these lesions. History of similar lesions starting primarily in the hands, legs & then moving centripetally toward the trunk, neck, inguinal, genital area and on external nares and near inner canthus of right eye 1 ½ months back. No history of previous episodes of ulcerations elsewhere in the body. Patient went to a private medical practitioner, got medicated and was referred to the college for further needful treatment. On clinical examination, dark brown and red colored encrustations were present on lips. Lips were edematous and erythema was present around encrustations (Fig. 1). Bleeding ulcers and localized areas of erythema were present on hard palate, buccal mucosa, tongue and gingivae (Fig. 2). None of the lymph nodes were palpable. Diagnostically significant finding was the presence of multiple target lesions on the trunk (Fig. 3). Nikolsky's sign was negative. Other systemic examination was normal. Clinically, diagnosis of erythema multiforme was made. Routine hematological investigations were within normal range. Biopsy from the lesion on histopathological examination (H&E and PAS stain) revealed intercellular edema, sub-basilar separation of epithelium from underlying connective tissue along with degeneration of basal cells at few places and connective tissue showing numerous bundles of collagen fibres, fibroblast, muscle tissue and blood vessels surrounded by dense chronic inflammatory cells (Fig. 4). Oral prednisolone at the dose of 20 mg twice daily was started along with local application of potent steroid - Clobetasol ointment thrice daily. Also oral supplementations were prescribed, to improve the overall condition of the patient. Within 15 days, there was decrease in the severity of the mucosal and skin lesions and prednisolone was tapered over next 15 days and stopped after further tapering till all lesions healed. Mouthwashes consisting of local anesthetics and antiseptics were added for symptomatic treatment. Complete hematological investigations were routinely done during the course of treatment which were within normal limits. In addition, no oral or skin lesions developed during the 2 months of treatment, the patient is still under follow-up and the disease is currently under control (Fig. 5). DISCUSSION Erythema multiforme (EM) is an acute, usually self-limiting, immune-mediated, blistering, ulcerative condition affecting the skin and/or mucous membranes, including the oral cavity.2,3,4 EM has been classified into a number of variants, mainly minor and major forms (Table 1).2,3. International Journal of Innovations in Dental Sciences / December 2016 / Vol 1 / Issue 1 14 Sathawane et. al : Erythema Multiforme Major : Case Report and Review Type of Erythema multiforme EM Minor (EMm) EM Major (EMM) Characteristic features Skin lesions Involves less than 10% of the body surface area Mucosal lesions Uncommon Most commonly oral mucosa Ocasionally EMm that only affects the oral mucosa may arise Skin lesions Involves less than 10% of the body surface area but more severe than EMm Mucosal lesions Involves two or more mucous membranes with more variable skin involvement. Oral lesions are usually widespread and severe ` EM arises as a result of immune-complex mechanisms involving antigen-antibody reactions that target small blood vessels in the skin or mucosa. In approximately, 90% of cases, the precipitating event relates to infection, with the herpes simplex virus (HSV) playing a Once in a while it may be associated with prodromal symptoms, which typically occur 7 to 14 days before development of cutaneous lesion. The classic skin lesion of EM is a target or iris lesion or bull’s eye distributed symmetrically on the extremities and trunk and characterized by concentric erythematous rings separated by rings of near normal color with lesion size ranging from 2 to 20 mm with central area of necrosis or crusting. Less commonly macules, papules or plaques are manifested. Complete recovery from an EM attack typically occurs within 1 to 4 weeks, with transient hypo/hyperpigmentation.3,6 Oral mucosal lesions occur in more than 70% of EM cases.3 The lesions show considerable variability in the appearance, ranging from diffuse oral erythema, to multifocal superficial ulcerations, thus the term multiforme. Initially, vesicles or bullae may be present, which rupture causing hemorrhagic crustations. Any area of the mouth may be involved, with buccal mucosa, palate, and tongue being most frequently affected. In most cases, lip lesions show hemorrhagic crustations. There may be mild to severe oral and perioral pain that may interfere with functional activities like speech, eating, swallowing and fluid intake, debilitating the health of the patient. Intraoral and perioral lesions heal without scarring.6 The diagnosis of EM is chiefly based on the history and clinical presentation, as histopathologic features and laboratory predominant role in 70% to 80% of cases.5 Other triggering factors may include medications, especially sulfonamides, NSAIDS, penicillins, and investigations are nonspecific.2,3,4 anticonvulsants.3 lack of evidence2 EMm may respond to topical corticosteroids. Patients with EMM ought to be Corticosteroids are the most commonly used drugs in the management of EM, regardless of International Journal of Innovations in Dental Sciences / December 2016 / Vol 1 / Issue 1 15 Sathawane et. al : Erythema Multiforme Major : Case Report and Review treated with systemic corticosteroids (prednisolone 0.5–1.0 mg/kg/day tapered over 7– 10 days) or azathioprine, or both or other immunomodulatory medications such as cyclophosphamide, dapsone, cyclosporine, levamisole, thalidomide or interferon-a.7 Cyclosporine given intermittently may control recurrent EM.8 . Fig. 1: Ulcers and hemorrhagic crusts on the lower lip during the first episode of EM Fig. 2: Bleeding ulcers and localized areas of erythema on buccal mucosa, hard palate, gingivae and tongue International Journal of Innovations in Dental Sciences / December 2016 / Vol 1 / Issue 1 16 Sathawane et. al : Erythema Multiforme Major : Case Report and Review Fig. 3: Characteristic target lesions seen on the trunk, back, extremities Fig. 4: Microphotograph (H&E, 10x) showing histopathological features suggestive of EM International Journal of Innovations in Dental Sciences / December 2016 / Vol 1 / Issue 1 17 Sathawane et. al : Erythema Multiforme Major : Case Report and Review 4. Osterne, Brito, Pacheco et al. Management of Erythema Multiforme Associated with Recurrent Herpes Infection: A Case Report. www.cda-adc.ca/jcda • October 2009, Vol. 75, No. 8. 5. Fig. 5: Intra-oral and Extra-oral post steroid therapy photographs of the patient, showing almost completely healed lesions ACKNOWLEDGEMENT We acknowledge the help and guidance from Dr. Shivmurthy, Professor and Head, Department of Oral and Maxillofacial Surgery and Dr. Gandhi, Head of Department of General Surgery, Chhattisgarh Dental College and Research Institute, Rajnandgaon (C.G.). REFERENCES 1. Siegel MA, Balciunas BA. Oral presentation and management of vesiculobullous disorders. Semin Dermatol 1994; 13:78–86. 2. Parvinderjit S. Kohli, Jasbir Kaur. Erythema Multiforme-Oral Variant: Case Report and Review of Literature. Indian J Otolaryngol Head Neck Surg 2011 63(Suppl 1):S9–S12; DOI 10.1007/s12070-011-0169. Watanabe R, Watanab H, Sotozono C, et al. Clinical factors differentiating erythema multiforme majus from Stevens-Johnson syndrome (SJS)/toxic epidermal necrolysis (TEN). Eur J Dermatol 2011; 21(6):889-94. 6. Williams PM, Conklin RJ. Erythema multiforme: a review and contrast from Stevens- Johnson syndrome/toxic epidermal necrolysis. Dent Clin North Am 2005; 49(1):67-76. 7. Stewart MG, Duncan III NO, Franklin DJ et al. Head and neck manifestations of erythema multiforme in children. Otolaryngol Head Neck Surg 1994; 111:236–242. 8. Schofield JK, Tatnall FM, Leigh IM. Recurrent erythema multiforme: clinical features and treatment in a large series of patients. Br J Dermatol 1993; 128:542–545. 3. Samim Firoozeh, Zed Christopher, Williams Michele P.Erythema multiforme-A review of Epidemiology, Pathogenesis, Clinical Features, and Treatment. Dent Clin N Am 57 (2013) 583-596. International Journal of Innovations in Dental Sciences / December 2016 / Vol 1 / Issue 1 18