* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download bacterial eye pathogens - UAB School of Optometry
Neonatal infection wikipedia , lookup
Metagenomics wikipedia , lookup
Staphylococcus aureus wikipedia , lookup
Microorganism wikipedia , lookup
Quorum sensing wikipedia , lookup
Horizontal gene transfer wikipedia , lookup
Trimeric autotransporter adhesin wikipedia , lookup
Bioremediation of radioactive waste wikipedia , lookup
Phospholipid-derived fatty acids wikipedia , lookup
Disinfectant wikipedia , lookup
Triclocarban wikipedia , lookup
Marine microorganism wikipedia , lookup
Human microbiota wikipedia , lookup
Bacterial cell structure wikipedia , lookup
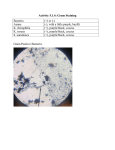
BACTERIAL EYE PATHOGENS Dr. WILLIAM J. BENJAMIN Eye Physiology & Ocular Prosthetics Laboratory University of Alabama at Birmingham School of Optometry Presented at the UAB School of Optometry as Part of MIC 200: MICROBIOLOGY and IMMUNOLOGY O t b 30 & November October N b 3, 3 2008 GRAM (+) POSITIVE COCCI EYE PATHOGENS Ô Ô Ô Ô Ô Staphylococcus aureus & epidermidis Micrococcus species Streptococcus pneumoniae (diplococcus) Streptococcus pyogenese & agalactiae Streptococcus viridans & equisimilus GRAM (+) POSITIVE BACILLI EYE PATHOGENS Ô Ô Ô Ô Ô Bacillus cereus & 4 other species Corynebacterium diphtheriae (w/o phage B) Propionibacterium acnes (Acne) Clostridium perfringens (Gangrene) Listeria monocytogenes GRAM (+) POSITIVE BACILLI EYE PATHOGENS Propionibacterium acnes GRAM (–) NEGATIVE COCCI EYE PATHOGENS Ô Neisseria gonorrhoeae (diplococcus) Ô Neisseria meningitidis Ô Moraxella (Branhamella) catarrhalis GRAM (–) NEGATIVE BACILLI EYE PATHOGENS Ô Ô Ô Ô Ô Ô Pseudomonas aeruginosa Haemophilus influenzae Haemophilus aegyptius (Koch-Weeks Bacilli) Moraxella lacunata (diplobacillus) Proteus species (esp. Proteus mirabilis) Serratia marcescens GRAM (–) NEGATIVE BACILLI EYE PATHOGENS Ô Ô Ô Ô Ô Ô Ô Escherichia coli Klebsiella species Azotobacter species Fusobacterium species Pasteurella species Yersinia species Bacteroides fragilis COCCOBACILLI EYE PATHOGENS Ô Acinetobacter species Ô Brucella species (Brucellosis) Ô Francisella tularensis (Tularemia) * sometimes also, Haemophilus species SPIROCHETE EYE PATHOGENS Ô Treponema pallidum (Syphilis) Ô Borrelia burgdorferi (Lyme Disease) Ô Leptospira interrogans (Leptospirosis) BACTERIAL MECHANISMS TO HEIGHTEN VIRULENCE AND RESISTANCE Ô Ô Ô Ô Ô Ô PHYSIOLOGICAL ADAPTATIONS TO DRUG PENICILLIN RESISTANCE: Beta Lactamase CELL WALL: Most Gram (–), Some Gram (+) CAPSULE or SLIME COAT of Polysaccharide CAPSULE, BIOFILM FORMATION (Exopolysaccharide) COAGULASE: Fibrin Coat / Staph. aureus BACTERIAL MECHANISMS TO HEIGHTEN VIRULENCE AND RESISTANCE Ô Ô Ô Ô Ô Ô FLAGELLA: Some Rods, All Spirochetes PILI (FIMBRIAE): Most Gram (–) Rods CYST FORMATION: Azotobacter species SPORE FORMATION: Bacillus species BACTERICINS CYTOTOXINS: Fibroblasts, Epithelial Cells Leukocidins BACTERIAL MECHANISMS TO HEIGHTEN VIRULENCE AND RESISTANCE Ô ENDOTOXINS: Within Cell Walls of Gram (–) Ô EXOTOXINS: Clostridium botulinum & tetani Ô PROTEASES and LIPASES Collagenase Sphingomyelinase “IgA IgA -ase ase” Elastase Phospholipidase Streptokinase Hemolysin Lecithinase Hyaluronidase Catalase Esterase Fibrinolysin HOW BACTERIA BECOME RESISTANT TO ANTIBACTERIALS Ô CELL WALL and MEMBRANE ALTERATIONS Mutations Decrease Drug Transport Ô PRODUCE ENZYMES TO INACTIVATE DRUG Split Molecule or Add Groups Ô RIBOSOMAL ALTERATIONS Decrease Drug Binding at 30S Ribosome Ô INCREASE BIOFILM PRODUCTION HOW BACTERIA BECOME RESISTANT TO ANTIBACTERIALS Ô DNA / RNA RELATED ALTERATIONS Reduce Binding To Polymerase, Gyrase Ô METABOLIC PATHWAY ALTERATIONS Key Metabolites Obtained Thru Diff Path Ô SPREAD OF VIRULENT PROPERTIES Plasmid Exchange Between Bacteria Ô INCREASED PURULENCE: PABA in Purulence a Contraindication to Sulfonamides HOW ANTIBACTERIALS WORK Ô INHIBIT CELL WALL SYNTHESIS Cell Lysis or Alters Cell Shape Iron Acquisition Proteins in Cell Wall Electron Transport System in Cell Wall EXAMPLES: Penicillins Penicillins, Cephalosporins Bacitracin, Vancomycin Ô INHIBIT DNA / RNA SYNTHESIS Bind DNA Polymerase or DNA Gyrase EXAMPLE: Rifamycin HOW ANTIBACTERIALS WORK Ô INHIBIT CELL MEMBRANE FUNCTION Leakage of Cell Contents Intracellular Build-up of Toxic Byproducts “Starve” Cell of Nutrients, Metabolites EXAMPLE: Polymixins Ô INHIBIT PROTEIN SYNTHESIS At the Ribosome (30S) Blocks tRNA from Forming Properly EXAMPLE: Aminoglycosides CULTURING OF BACTERIA FROM THE CONJUNCTIVA AND EYELIDS CULTURING OF BACTERIA FROM THE CONJUNCTIVA AND EYELIDS Staphylococcus aureus CULTURING OF BACTERIA FROM THE CONJUNCTIVA AND EYELIDS Ô Ô Ô Ô STERILE SALINE; NO ANESTHETIC DACRON SOAKED IN CALCIUM ALGINATE DACRON OR COTTON TIP APPLICATORS SWAB INNER LID MARGIN Lower Preferred, but ….. Ô STREAK MARKED AGAR PLATE & DISPOSE Ô SWAB PALP CONJ & C-d-S Lower Preferred, but ….. Ô STREAK MARKED AGAR PLATE & DISPOSE CULTURING OF BACTERIA FROM THE CONJUNCTIVA AND EYELIDS CULTURING OF BACTERIA FROM THE CONJUNCTIVA AND EYELIDS CULTURING OF BACTERIA FROM THE CONJUNCTIVA AND EYELIDS Ô INCUBATE AT 35 DEGREES FOR 24-48 Hrs. OR SEND TO MICRO LABORATORY Ô DO NOT WAIT TO START ANTIBIOTICS Ô KEY AGAR PLATES FOR THE O.D. OFFICE Blood Agar: Use for Everything Chocolate Agar: If Suspect Neisseria, etc. Sabouraud’s Sabouraud s Agar: Fungi; 25 Deg, Deg 2-10 Days Ô CULTURE TRANSPORT PACKS: Not Good, but sometimes necessary CULTURING OF BACTERIA FROM THE CONJUNCTIVA AND EYELIDS Ô OCULAR PATHOGENS REQUIRING CHOCOLATE AGAR + CO2 Neisseria gonorrhoeae* Haemophilus sp. Moraxella lacunata * Other Neisseria also grow better this way Ô CULTURE TRANSPORT PACKS: Not Good, y but sometimes necessary CULTURING OF BACTERIA FROM THE CONJUNCTIVA AND EYELIDS CULTURING OF BACTERIA FROM THE CONJUNCTIVA AND EYELIDS CULTURING OF BACTERIA FROM THE CONJUNCTIVA, AND EYELIDS CULTURING OF BACTERIA FROM THE CONJUNCTIVA AND EYELIDS CULTURING OF BACTERIA FROM CORNEAL ULCERS Ô STERILE SALINE; ANESTHETIC REQUIRED Ô KIMURA SPATULA but not CYTOBRUSH Ô DACRON SOAKED IN CALCIUM ALGINATE Ô DACRON OR COTTON TIP APPLICATORS Ô SCRAPE CENTER AND LEADING MARGIN CORNEAL PATHOGENS WITH SPECIAL AFFINITY FOR CORNEAL EPITHELIUM Ô Streptococcus pneumoniae Prefers Corneal Epithelial Cells in general Be sure to scrape the “leading edge” Ô Pseudomonas aeruginosa Prefers Basal Corneal Epithelial Cells Be sure to scrape the center at bottom Ô Staphylococcus aureus CULTURING OF BACTERIA FROM CORNEAL ULCERS Ô STREAK AGAR PLATE Ô DISPOSE OR FLAME: Be sure to let cool Ô INCUBATION AT 35 DEGREES FOR 24-48 Hr. OR SEND TO MICRO LABORATORY Ô 50% of Microbial Ulcers WON’T WON T GROW OUT CULTURING OF BACTERIA FROM CORNEAL ULCERS Ô 50% of Microbial Ulcers WON’T GROW OUT Ô Therefore, many attempts are “Culture-Negative” CULTURING OF BACTERIA FROM CORNEAL ULCERS Ô 50% of Microbial Ulcers WON’T GROW OUT Ô Ulcers should not be called “Sterile” CULTURING OF BACTERIA FROM CORNEAL ULCERS Ô 50% of Microbial Ulcers WON’T GROW OUT Ô Such an Ulcer is a “Culture-Negative Ulcer” but is not necessarily a “Sterile Sterile Ulcer” Ulcer CULTURING OF BACTERIA FROM CORNEAL ULCERS Culture-Negative Macular Keratitis turned Ulcer Started on Tobramycin Ophthalmic Drops every 2 hours as dual Macular Keratitis with Anterior Chamber Reaction Intensified to dual Ulcers overnight with greater ACR and Corneal Edema, VA ↓ Fortified Tobramycin and F tifi d Vancomycin Fortified V i alternating every half hour CULTURING OF BACTERIA: The Hospital Micro Laboratory CULTURING OF BACTERIA: The Hospital Micro Laboratory IDENTIFICATION OF BACTERIA FROM CULTURES Ô GRAM STAIN FOR (+) or (–), CELL MORPHOL. Ô DIFF QUIK or GIEMSA STAIN SMEARS FOR HOST INFLAMMATORY CELLS Ô COLONY MORPHOLOGY, COLOR, ODOR, AFTER GROWTH ON AGAR PLATES Ô IF GRAM (+) COCCI, GO TO CATALASE TEST Micro Labs do same same, automated automated, quicker Ô IF GRAM (–) BACILLI, GO TO STRIP TESTS Micro Labs do same, automated, quicker IDENTIFICATION OF BACTERIA FROM CULTURES IDENTIFICATION OF BACTERIA FROM CULTURES Ô GRAM STAIN FOR (+) or (–), CELL MORPHOL. Ô DIFF QUIK or GIEMSA STAIN SMEARS FOR HOST INFLAMMATORY CELLS Ô COLONY MORPHOLOGY, COLOR, ODOR, AFTER GROWTH ON AGAR PLATES Ô IF GRAM (+) COCCI, GO TO CATALASE TEST Micro Labs do same same, automated automated, quicker Ô IF GRAM (–) BACILLI, GO TO STRIP TESTS Micro Labs do same, automated, quicker IDENTIFICATION OF BACTERIA FROM CULTURES Serratia marcescens IDENTIFICATION OF BACTERIA FROM CULTURES Pseudomonas aeruginosa IDENTIFICATION OF BACTERIA FROM CULTURES Ô GRAM STAIN FOR (+) or (–), CELL MORPHOL. Ô DIFF QUIK or GIEMSA STAIN SMEARS FOR HOST INFLAMMATORY CELLS Ô COLONY MORPHOLOGY, COLOR, ODOR, AFTER GROWTH ON AGAR PLATES Ô IF GRAM (+) COCCI, GO TO CATALASE TEST Micro Labs do same same, automated automated, quicker Ô IF GRAM (–) BACILLI, GO TO STRIP TESTS Micro Labs do same, automated, quicker IDENTIFICATION OF BACTERIA FROM CULTURES: GRAM (+) COCCI IDENTIFICATION OF BACTERIA FROM CULTURES: GRAM (–) RODS IDENTIFICATION OF BACTERIA FROM CULTURES: AUTOMATION IDENTIFICATION OF BACTERIA FROM CULTURES: ANAEROBES IDENTIFICATION OF BACTERIA FROM CULTURES Ô IF GRAM (+) BACILLI, SEND TO EXPERT Ô IF GRAM (–) COCCI, MUST BE Neisseriarelated BUT SEND TO EXPERT ANYWAY Ô IF COCCOBACILLI, SEND TO EXPERT Micro Labs do these last three categories by hand, plus any strange Gram (+) Cocci and Gram (–) Bacilli IDENTIFICATION OF BACTERIA FROM CULTURES QuadFerm Test for Neisseriarelated organisms ID OF GRAM (+) COCCI ((continued … ) ID OF GRAM (+) COCCI ( … continued) IDENTIFICATION OF GRAM (+) COCCI Ô CATALASE TEST Catalase (+) = Staphylococcus species Catalase (–) = Streptococcus species Ô COAGULASE TEST / MANNITOL FERMENT. Coagulase (+) ( ) = Staphylococcus aureus Coagulase (–) = Staphylococcus epidermidis, et al IDENTIFICATION OF GRAM (+) COCCI Mannitol fermentation = Coagulase test (+) and (–) IDENTIFICATION OF GRAM (+) COCCI Ô GAMMA (NO) HEMOLYSIS (Nonhemolytic) Group D Streptococcus sp. (Enterococci) Ô BETA (COMPLETE) HEMOLYSIS A DISC (Bacitracin) Sensitive (+) p A: Streptococcus p pyogenes py g Group A DISC (Bacitracin) Insensitive (–) Non Group A, Beta Hemolytic Strept. species (Streptococcus agalactiae) Ô A Disc = Bacitracin IDENTIFICATION OF GRAM (+) COCCI Streptococcus pyogenes (Strong ß hemolysis hemolysis, A disc sensitive) IDENTIFICATION OF GRAM (+) COCCI Streptococcus agalactiae (Weak ß hemolysis, A disc insensitive) ID OF GRAM (+) COCCI: Strong vs. Weak ß Hemolysis CAMP Test: Staph. aureus, Strept. agalactiae, & Strept. pyogenes IDENTIFICATION OF GRAM (+) COCCI Ô ALPHA (INCOMPLETE) HEMOLYSIS P DISC (Optochin) Sensitive (+) Streptococcus pneumoniae P DISC (Optochin) Insensitive (–) ( ) Streptococcus viridans or Group D Ô P Disc = optochin = ethyl hydrochloride IDENTIFICATION OF GRAM (+) COCCI Streptococcus pneumoniae (α hemolysis, hemolysis P disc sensitive) IDENTIFICATION OF GRAM (+) COCCI and GRAM (–) BACILLI Ô AUTOMATED IDENTIFICATION IDENTIFICATION OF GRAM (+) COCCI and GRAM (–) BACILLI Ô AUTOMATED IDENTIFICATION BACTERIAL SUSCEPTIBILITY TO ANTI-BACTERIALS DISC DIFFUSION METHOD Ô LARGE QUANTITY OF BACTERIUM NEEDED Ô PLACE IN THIOGLYCOLLATE BROTH, MIX Ô STANDARDIZED MUELLER-HINTON AGAR MH+5% MH 5% Sheep Blood for Strept. pneumo. MH Chocolated for Neisseria, Moraxella, & Haemophilus species Ô STREAK EVENLY OVER ENTIRE SURFACE Ô PLACE SET OF DISCS WITH DIFF AGENTS BACTERIAL SUSCEPTIBILITY TO ANTI-BACTERIALS DISC DIFFUSION METHOD Ô Ô Ô Ô INCUBATE 24 Hrs. AT 35 DEGREES DIAMETERS OF INHIBITORY ZONES IN mm COMPARE DIAM’s TO STANDARD CHART THIS PROCEDURE HAS BEEN AUTOMATED, COMPUTERIZED FOR Mueller Hinton Agar Mueller-Hinton BACTERIAL SUSCEPTIBILITY TO ANTI-BACTERIALS DISC DIFFUSION METHOD Anti-bacterials for Gram (+) BACTERIAL SUSCEPTIBILITY TO ANTI-BACTERIALS DISC DIFFUSION METHOD Anti-bacterials for Gram (–) BACTERIAL SUSCEPTIBILITY TO ANTI-BACTERIALS DISC DIFFUSION METHOD Anti-bacterials A ib i l for f Streptococcus pneumoniae BACTERIAL SUSCEPTIBILITY TO ANTI-BACTERIALS SERIAL DILUTION METHOD Ô TEST TUBES WITH BROTH & AGENT Ô AGENT IN DIMINISHING CONCENTRATION Ô LOWEST CONC. TO DENY VISIBLE GROWTH Minimum Inhibitory Concentration (MIC) Ô LOWEST CONC. TO KILL 99.9% INOCULUM Minimum Bactericidal Concentration (MBC) BACTERIAL SUSCEPTIBILITY TO ANTI-BACTERIALS SERIAL DILUTION METHOD Ô AUTOMATED SERIAL DILUTION vs. LIMITED AGENTS COMBINED WITH ID OF GRAM (+) and ((–)) BACTERIAL SUSCEPTIBILITY TO ANTI-BACTERIALS EPSILOMETER METHOD Ô LARGE QUANTITY OF BACTERIUM NEEDED Ô MIX IN THIOGLYCOLATE BROTH Ô STANDARDIZED MUELLER-HINTON AGAR MH+5% MH 5% Sheep Blood for Strept. pneumo. MH Chocolated for Neisseria, Moraxella, & Haemophilus species Ô STREAK EVENLY OVER ENTIRE SURFACE BACTERIAL SUSCEPTIBILITY TO ANTI-BACTERIALS EPSILOMETER METHOD Ô PLACE SET OF “E TEST” STRIPS WITH DIFF. ANTIMICROBIAL AGENTS Ô EACH AGENT IN DIMINISHING CONCENTRATION ALONG E TEST STRIP Ô INCUBATE 24 Hrs. AT 35 DEGREES Ô ASSESS INHIBITION FOR MINIMUM INHIBITORY CONCENTRATION (MIC) BACTERIAL SUSCEPTIBILITY TO ANTI-BACTERIALS EPSILOMETER METHOD BACTERIAL SUSCEPTIBILITY TO ANTI-BACTERIALS EPSILOMETER METHOD BACTERIAL SUSCEPTIBILITY TO ANTI-BACTERIALS EPSILOMETER METHOD CLINICAL PEARLS ABOUT BACTERIAL SUSCEPTIBLITY Ô BACTERIA IN EYE MAY ALTER PHYSIOLOGICALLY AFTER TREATMENT IS BEGUN Ô GROWTH ON AGAR PLATE in vitro MAY BE DIFFERENT THAN BACTERIA in vivo Ô SUSCEPTIBILITY TESTS MAY NOT INDICATE SUSCEPTIBILITY OF BACTERIA IN EYE Ô ANTIBACTERIALS MUST BE USED FULL 10 to 14 DAYS TO KILL RESISTANT STRAINS Ô DON’T “TAPER OFF” ANTIBACTERIALS CLINICAL PEARLS ABOUT BACTERIAL SUSCEPTIBLITY Ô SAVE THE NEW, MORE POTENT ANTIBACTERIALS UNTIL THEY ARE NECESSARY? Ô CLINICAL DILEMMA: The Flouroquinolones Ciprofloxacin (Alcon Ciloxan) Cipro 38.9% Ofloxacin (Allergan Ocuflox) Floxacin 0.8% Norfloxacin (Merck Chibroxin) Noroxin ~0% Levofloxacin (Santen Quixin) Levaquin 40.9% Gatifloxacin (Allergan Zymar) Tequin 8.3% Moxifloxacin (Alcon Vigamox) Avelox 10 10.8% 8% Ô FOLLOW THE EXAMPLE OF TOBRAMYCIN? Ô USE TOPICALS NOT USED SYSTEMICALLY Systemic use creates resistant strains CLINICAL PEARLS ABOUT BACTERIAL SUSCEPTIBLITY Ô Farhi & Kowalski (2007) Tested 1161 Conj’itis Isolates vs. 11 Antibacterials DRUG SUSCEPTIBILITY COST Moxifloxacin 86% $73.38 Ofloxacin 86% $46.75 Ciprofloxacin 84% $49.18 Gatifloxacin % 84% $70.38 $ Sulfacetamide 84% $13.11 PolyTrim 80% $22.18 Gentamicin 74% $14 68 $14.68 Bacitracin 70% $10.82 Tobramycin 68% $15.13 Erythromycin 62% $11.17 CLINICAL PEARLS ABOUT BACTERIAL SUSCEPTIBLITY ÔSodium sulfacetamide, a bacteriostatic agent, with 84% in vitro coverage of all isolates, and an average cost of $13.11, appeared to be most cost-effective cost effective for empirical coverage of bacterial conjunctivitis. ÔThe fluoroquinolones, although more expensive and of recent introduction introduction, gave only similar coverage coverage. ÔPERHAPS RESISTANCE FADED AWAY AFTER 20 YEARS OF DISUSE FOR SODIUM SULFACETAMIDE! Will there be a 20-year recycling effort? MICROORGANISMS THAT CAN INFECT (PENETRATE ?) THE INTACT CORNEA Ô Ô Ô Ô Ô Neisseria gonorrhoeae Streptococcus pneumoniae Corynebacterium diphtheriae (+ other sp.) Haemophilus sp. sp (H. (H aegyptius, aegyptius H. H influenzae) Listeria sp. ( L. monocytogenes) BACTERIA THAT CAUSE MAJORITY OF CONJUNCTIVITIS IN CHILDREN Ô Streptococcus pneumoniae (< 5 years old) Ô Haemophilus aegyptius (< 5 years old) Ô Staphylococcus aureus (> 5 years old) INSTANCES WHEN MICRO LAB STUDIES ARE MANDATORY Ô Ô Ô Ô Ô Ô Ô NEONATAL CONJUNCTIVITIS HYPERACUTE CONJUNCTIVITIS MEMBRANEOUS CONJUNCTIVITIS CORNEAL ULCERS not obviously Herpetic POSTOPERATIVE EYE INFECTIONS SEVERE LONG-STANDING LONG STANDING CONJUNCTIVITIS SUSPECTED FUNGAL EYE INFECTION MICROORGANISMS CAUSING CONJUNCTIVAL MEMBRANES or PSEUDOMEMBRANES Ô Ô Ô Ô Ô Ô Ô Neisseria gonorrhoeae Streptococcus pneumoniae Corynebacterium diphtheriae Streptococcus species Adenovirus Herpes simplex virus Chlamydia trachomatis BACILLUS CEREUS BACILLUS CEREUS Ô Ô Ô Ô Ô Ô Ô UBIQUITOUS; SPORE FORMING G(+) Rod EXOTOXIN: Highly Virulent Pathogen PENETRATING EYE TRAUMA METASTATIC INFECTION OF DRUG ADDICT POST-TRAUMATIC ENDOPHTHALMITIS CORNEAL RING ABCESS WITHIN 24 Hrs. EYE IS BLIND WITHIN 72 Hrs. OF INFECTION NEISSERIA GONORRHOEAE NEISSERIA GONORRHOEAE Ô Ô Ô Ô Ô Ô Ô Ô G(–) COFFEE BEAN SHAPED DIPLOCOCCUS OPHTHALMIA NEONATORUM YOUNG, SEXUALLY ACTIVE ADULTS ATTACKS MUCOSAL EPITHELIUM ACUTE COPIOUSLY PURULENT CONJ’ITIS CAN PENETRATE INTACT CORNEAL EPITH. UNTREAT: CORN. ULCER, PERFORATION REQUIRES CHOCOLATE AGAR + CO2 NEISSERIA GONORRHOEAE Ô Ô Ô Ô Ô IgA -ase, OUTER MEMBRANE ADHESINS PILI (FIMBRIAE) IRON ACQUISITION PROTEIN IN CELL WALL QUICKLY KILLED BY HEAT, HEAT DRYING, DRYING SUN MUTATED VERSIONS HAVE RESISTANCE: Beta Lactamase Production Altered Cell Wall Structure Ô CONJ. MEMBRANE or PSEUDOMEMBRANE HAEMOPHILUS AEGYPTIUS (Koch-Weeks Bacillus) Ô Ô Ô Ô Ô Ô Ô G(–) ROD, SUBSPECIES OF H. influenzae RARELY CAUSES SYSTEMIC ILLNESS ACUTE CONJ’ITIS WITH BRIEF INCUBATION MOST COMMON IN WARM MONTHS, MONTHS SOUTH MUCOPURULENT DISCHARGE; Kids < 5 yrs INFERIOR LIMBUS ULCERATIONS SOME SCARRING OF INFERIOR CORNEA HAEMOPHILUS AEGYPTIUS (Koch-Weeks Bacillus) Ô Ô Ô Ô Ô Ô PILI (FIMBRIAE) ENDOTOXIN CAPSULE GROWTH ENHANCED AROUND Staph. Staph sp. sp CAN INFECT INTACT CORNEAL EPITHELIUM REQUIRES CHOCOLATE AGAR + CO2 MORAXELLA LACUNATA MORAXELLA LACUNATA Ô Ô Ô Ô Ô Ô G(–) DIPLOBACILLUS with PILI (FIMBRIAE) ANGULAR BLEPHAROCONJ’ITIS (Temporal) CORNEAL ULCERATION with HYPOPYON RARE IN YOUNG CHILDREN MUST NOW DIFFERENTIATE FROM Staph. REQUIRES CHOCOLATE AGAR + CO2 STREPTOCOCCUS PNEUMONIAE STREPTOCOCCUS PNEUMONIAE Ô Ô Ô Ô Ô Ô G(+) DIPLOCOCCUS with PILI (FIMBRIAE) OPHTHALMIA NEONATORUM ADULT DACRYOCYSTITIS ACUTE CATARRHAL CONJ’ITIS; CONJ ITIS; Kids < 5 yrs CORNEAL ULCERATIONS with HYPOPYON SHOWS PREFERENTIAL ADHERENCE TO CORNEAL EPITHELIAL CELLS Ô CONJ. MEMBRANE or PSEUDOMEMBRANE STREPTOCOCCUS PNEUMONIAE Ô Ô Ô Ô Ô Ô Ô WELL ORGANIZED CAPSULE (SLIME COAT) BIOFILM (GLYCOCALYX) IgA -ase Fibrinolysin Hyaluronidase Streptokinase Hemolysin Leukocidin PNEUMOLYSIN: Inhibit Chemotaxis of PMNs CAN INFECT INTACT CORNEAL EPITHELIUM PSEUDOMONAS AERUGINOSA PSEUDOMONAS AERUGINOSA Ô Ô Ô Ô Ô Ô Ô Ô UBIQUITOUS G(–) ROD MOST VIRULENT CORNEAL PATHOGEN CAN NOT PENETRATE INTACT EPITHELIUM CORNEAL ULCERATIONS AND KERATITIS CAN PERFORATE CORNEA IN 24 Hrs. CAN FEED ON FLUORESCEIN IN SOLUTION CAN FEED ON CAMPHOR, NAPHTHALENE CAN GROW IN DISTILLED WATER PSEUDOMONAS AERUGINOSA Ô Ô Ô Ô Ô Ô Ô PILI (FIMBRIAE); BIOFILM POLAR FLAGELLUM Endotoxin Elastase Proteases Exotoxins Phosphatase Collagenase HEMOLYSIN: Unusual for a Gram (–) BLUE-GREEN BLUE GREEN PURULENCE from BG PYACIN SHOWS PREFERENTIAL ADHERENCE TO BASAL CORNEAL EPITHELIAL CELLS STAPHYLOCOCCUS AUREUS STAPHYLOCOCCUS AUREUS Ô Ô Ô Ô Ô Ô Ô G(+) COCCI, NORMAL OCULAR FLORA COMMON & CHRONIC EYELID INFECTIONS HORDEOLUM: Nearly always the cause ACUTE & CHRONIC CONJ’ITIS; CONJ ITIS; Kids > 5 yrs KERATITIS AND OCCASIONAL ULCERATION POST-OPERATIVE POST OPERATIVE ENDOPHTHALMITIS MEIBOMIAN GLAND DYSFUNCTION: Most common, with Propionibacterium acnes STAPHYLOCOCCUS AUREUS Ô CELL WALL BINDING PROTEIN BINDS TO CORN EPITHELIAL SURFACE FIBRONECTIN CORN. Ô Catalase Wax Esterase Hemolysin Ô Coagulase Cholesterol Esterase Ô Exotoxins Cytotoxins Leukocidins Ô Hyaluronidase Ô GROWS SLOWLY EVEN AT 5 DEGREES AND CAN CONTAMINATE REFRIDGERATED SOLN STREPT. VIRIDANS STAPH EPIDERMIDIS STAPH. LINE-UP: CAN YOU IDENTIFY THE PERPETRATOR ?