* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Dr. Sadeghi
Maternal physiological changes in pregnancy wikipedia , lookup
Dental emergency wikipedia , lookup
Prenatal development wikipedia , lookup
Prenatal testing wikipedia , lookup
Breech birth wikipedia , lookup
Women's medicine in antiquity wikipedia , lookup
Fetal origins hypothesis wikipedia , lookup
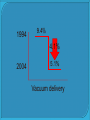
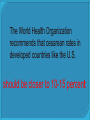
by :Dr sadeghi Jun 7, 2010 The physiologic process sufficiently frequent, strong uterine contractions thinning and dilation of the cervix permitting passage of the fetus from the uterus through the birth canal. Friedman divided labor into three stages : First stage: time from the onset of labor until complete cervical dilatation Second stage: time from complete cervical dilatation to expulsion of the fetus Third stage: time from expulsion of the fetus to expulsion of the placenta latent phases The first stage active phases the latent phase: regular contractions mild infrequent contractions gradual change in cervical dilation (usually <1 cm per hour) Increase effacement. the average duration of latent phase in nulliparous and multiparous women is 6.4and 4.8 hours 1st stage of labor – mostly visceral Dilation of the cervix and distention of the lower uterine segment Dull, aching and poorly localized Slow conducting, visceral C fibers, enter spinal cord at T10 to L1 2nd stage of labor – mostly somatic • Distention of the pelvic floor, vagina and perineum • Sharp, severe and well localized • Rapidly conducting A-delta fibers, enter spinal cord at S2 to S4 T10 L1 S2 S4 Primarily dilation of the cervix Small component from uterine muscle stimulation of the mechanoreceptor Visceral pain Only amputation of a digit exceeded the pain of labor Sensory words: sharp, cramping, aching, throbbing, stabbing, tight Sensory nerves from uterus and cervix:T10-L1 Pass through par cervical region Accompany the sympathetic fibers To the white ramie communicants Dorsal horn, laminae V Referred pain Fetus descends through the birth canal Stretching and tearing of fascia, skin, subcutaneous tissue, and other somatic structures Somatic pain Anterior primary divisions of sacral nerves, S2-S4 Pudendal nerve provides total pain relief to the mother without adversely affecting the labour process unwanted side effects in the mother or baby. freely available labor pains can be a very real downside to a vaginal delivery. Since labor pains can extend over a long period of time, it can be a harrowingly difficult and painful time for a woman. Safe Maternal Health and Safe Motherhood Programmed vaginal delivery represents the safest route for the fetus and newborn in the first and subsequent pregnancies There are many different techniques, both regional and non-regional to provide labour analgesia. Non-regional techniques are the most frequently employed methods for labour analgesia. Meperidine (pethidine) is the most frequently used opioid for labour analgesia. Its limited efficacy and side effects are well documented. Inhalation of nitrous oxide relieves labour pain to a significant degree . Epidural analgesia, CSA , PCEA ,when compared with other methods, provides superior analgesia for labour. Boundaries of epidural space Superior - the foramen magnum Inferior - the sacral hiatus and sacrococcygeal membrane Anterior - the posterior longitudinal lig. Posterior - periosteum of laminae of the vertebrae and the lig. flavum Lateral - periosteum of the pedicles and intervertebral foraminae Epidural space contains: • Dural sac and nerve roots • Blood vessels and lymphatics • Connective and fatty tissue Epidural analgesia is a commonly employed technique of providing pain relief during labor. The number of parturient given intrapartume epidural analgesia is reported to be over 50 percent at many institutions in the .United States Safe (for both mother and fetus) Easy and painless placement Fast onset, easy administration, tight control Effective analgesia (for both stage I and II) Reliable extension for indicated procedures Minimal side effects (for both mother and fetus) No adverse effects on labor progress Minimal complications High patient satisfaction overall Epidural Contraindications: 1. patient refusal 2. maternal hemorrhage 3. coagulopathy 4. fever>38.5`c TABLE Complications of Epidural Analgesia Immediate Hypotension (systolic blood pressure <100 mm Hg or a decrease of 25 percent below preblock average Urinary retention) Local anesthetic induced convulsions Local anesthetic induced cardiac arrest Delayed Postural puncture headache Transient backache Epidural abscess or meningitis Permanent neurologic deficit .Very rare--* The most common complications occurring with epidural analgesia are maternal hypotension and postural puncture headache STRATEGIES TO MINIMIZE MATERNAL MOTOR BLOCK — Decreasing the intensity of motor block may be achieved by administering lower concentrations of local anesthetics by either the epidural or spinal route. Low concentrations of some local anesthetics (eg, bupivacaine) Analgesic adjuvant (fentanyl, sufentanil, epinephrine) are often co-administered with local anesthetics to offset the decreased analgesic intensity resulting from the reduction of local anesthetic dose. The opioids do not produce any motor block, and thus are ideally suited adjuvant for labor analgesia. The rate of operative vaginal delivery fell 45 percent, from 9.4 percent of live births in 1994 to Vacuum deliveries comprised 5.2 percent in 200 4.1 percent of all live births in 2004, whereas forceps deliveries dropped dramatically, from 5.5 percent of births in 1989 to 1.1 percent in 2004 Training in forceps use also has decreased, with one study showing that only one half of graduating obstetrics and gynecology residents surveyed felt comfortable performing forceps deliveries in their practice 1994 2004 Operative vaginal delivery 1994 9.4% 4.1% 2004 5.1% Vacuum delivery 1989 5.5% 4.4% 2004 1.1% forceps INDICATIONS FOR OPERATIVE VAGINAL DELIVERY Prolonged second stage of labor nulliparousi Without more than 2hours With regional more than3 hours multiparious Without With regional regional more more than 2 than 1 hours hours immediate potential fetal compromise Shortening for maternal benefit vacuum Vacuum vaginal delivery A.Cephalo hematomas B. subgaleal hematomas When the c-section rate reached its peak in 1988, it came under closer scrutiny. Critics expressed alarm at the frequency of a procedure that places the mother at risk for infections, hemorrhage and other .complications The World Health Organization recommends that the caesarean section rate should not be higher than 10% to 15% Moreover, caesarean delivery 1. high maternal complication 2. neonatal complication rates 3. increased health-care costs Vaginal delivery Faster recovery rate Decreased risk for respiratory distress syndrome in babies Faster bonding with baby and ability to breastfeed immediately Less risk and more safe option in most cases Lower cost and shorter hospital stay More involvement during the birth process The World Health Organization recommends that cesarean rates in developed countries like the U.S. . should be closer to 10-15 percent WHO recommends that the rate of Caesarean sections should not exceed 15% in any country. However, in recent years the rate has risen to a record level of 46% in China and to levels of 25% and above in many Asian countries, Latin America, and the USA Caesarean section is associated : risks of post-operative adhesion incision hernias wound infections Server blood loss Increasing the anesthesia risk a placenta accrete The risk of potentially life-threatening condition, is only 0.13% after two Caesarean sections but increases to 2.13% after four and then to 6.74% after six or more surgeries Among developing countries, Brazil has one of the highest rates of caesarean sections in the world. In the public health network, the rate reaches 35%, while in private hospitals the rate approaches 80% A caesarean is a life threatening medical procedure that is obviously ultimately decided upon by a .doctor or several doctors Cesarean section Risks associated with anesthesia use Increased risk of infection Risk of bowel or bladder injury resulting from surgery Risk for air or amniotic embolism Risk of uncontrolled bleeding Risk to fetus of respiratory distress syndrome Increased risk of placenta previa or uterine abruption in future pregnancies Risks for recurrent cesarean sections Which one is better for choose ? vaginal delivery or cesarean section women choosing primary elective cesarean delivery will have a higher incidence of maternal morbidity, including hemorrhage,infection, and venous thromboembolism. Maternal mortality, while a rare event in developed nations, is 2 to 3 times higher in elective cesarean delivery than in vaginal delivery, although there are no large studies of maternal mortality risk for primary elective cesarean delivery. vaginal delivery A normal fetal heart rate is between 110 and 160 beats per minute. Hypertension (systolic blood pressure ≥ 140 mmHg or diastolic blood pressure ≥ 90 mmHg) is one of the two criteria for preeclampsia (the other is proteinuria, a random urine protein determination of 30 mg/dL or 1+ on dipstick). Hypothermia in the immediate newborn period increases oxygen consumption and metabolic demands and is independently associated with increased mortality; therefore, maintaining body heat is an important initial step in caring for the newborn Drying the newborn is crucial, as it significantly reduces heat loss. There are several additional ways to keep the infant warm after drying: swaddling in warm towels/blankets, "skin to skin" contact with mother, placement in a warm (36.5ºC) isolette, raising the environmental (room) temperature, and clothing. The Apgar score assesses neonatal heart rate, respiratory effort, muscle tone, reflex irritability, and color. Assign Apgar scores at one and five minutes after birth (show calculator). About 90 percent of neonates have Apgar scores of 7 to 10, and generally require no special intervention. Catheter manipulation Additional volume of local anesthetic Patient’s position manipulation Replacement of the epidural catheter A single shot spinal anesthesia Continuous spinal anesthesia Combined spinal-epidural anesthesia Placement of an additional epidural catheter Supplementation with intravenous medications Conditions for a cesarean section: There are several conditions which may make having a baby by cesarean section more likely. These include, but are not limited to, the following: previous cesarean section fetal distress abnormal a delivery presentation (i.e., breech, shoulder, face) labor that fails to progress or does not progress normally placental complications (i.e., placenta previa, in which the placenta blocks the cervix and presents the risk of becoming detached prematurely from the fetus) Regional Analgesia Regional analgesia tends to be the most effective method of pain relief during labor and causes few side effects. Epidural analgesia, spinal blocks, and combined spinal–epidural blocks are all types of regional analgesia that are used to decrease labor pain. Epidural Analgesia. Epidural analgesia, sometimes called an epidural block, causes some loss of feeling in the lower areas of your body, yet you remain awake and alert. An epidural block may be given soon after your contractions start, or later as your labor progresses. An epidural block with more or stronger medications (anesthetics, not analgesics) can be used for a cesarean delivery or if vaginal birth requires the help of forceps or vacuum extraction. Your doctors will work with you to determine the proper time to give the epidural. Lumbar epidural analgesia provides complete pain relief for eighty-five percent and partial relief in a further twelve percent of labouring women. Only three percent have no relief at all (Crawford JS, 1979). A continuous infusion maybe started early in the first stage and can be continued for anaesthesia if a caesarean section is required. well-trained anaesthesiologist with an interest in obstetric analgesia is needed to provide an epidural analgesia service. Ideally, a twentyfour hour obstetric analgesia service should be in operation. The labouring woman should have had an informed discussion about the procedure, benefits and risks of epidural analgesia in the prenatal period. The epidural catheter should be inserted early in labour when the patient is more co-operative and the Epidural analgesia, also called an epidural block, numbs the lower area of a woman's body, and allows her to remain awake and alert. A spinal block, usually given only once during labor, works right away but for only an hour or two. A combined spinal-epidural block, sometimes called the 'walking epidural,' works immediately and allows pain relief drugs to be given throughout labor. Advantages of the Epidural A pain free labor! Rapid pain relief Medications can be increased or decreased based on your comfort level-without additional injections No groggy feeling or cloudy-headed side effects Disadvantages of the Epidural A common side effect is a drop in mom's blood pressure (repositioning or medications are used to correct this) Fewer than 10 percent of women report itching all over their body Labor time may increase by approximately an hour You will need to be connected to an IV and monitor- and if you are mobile, need to move with your equipment A small percentage of women, usually first time moms, will spike a Advantages Advantages of epidural anesthesia during childbirth These are the main advantages of having an epidural during childbirth: It provides complete pain relief without making you feel confused or drowsy. It can be topped up if you need surgery (a Caesarean). A low-dose (mobile) epidural will allow you to feel your contractions. It immediately calms the baby if your labor pains were previously causing stress. It can allow you to have a rest, giving you more energy for An epidural delivers continuous pain relief to the lower part of your body while allowing you to remain fully conscious. Medication is delivered through a catheter, a very thin, flexible, hollow tube that's inserted into the epidural space just outside the membrane that surrounds your spine. Since the effect of the medication is localized, you'll be awake and alert during labor and birth. And, because you're painfree, you can rest if you want (or even sleep!) as your cervix dilates. As a result, you may have more energy when it comes time to push. You have to stay in an awkward position for ten to 15 minutes while the epidural is put in, and then wait another five to 20 minutes before the medication takes full effect. This may seem like a minor inconvenience, though, when the tradeoff is hours of pain relief. Conclusions In 2002, the American College of Obstetricians and Gynecologists and the American Society of Anesthesiologists issued a joint statement indicating that a woman's request for pain relief is sufficient medical indication for its use. Our opinion is that epidural analgesia is a safe, widely used, effective means of pain relief during labor and From 1985 to present use of epidural analgesia for labor has increased from 10% to over 50% of laboring women in the U.S. Advances include low dose epidurals, “walking” epidurals, PCEA, and CSE Early: increased doses of LA = increased SE PDPH 7-10% OB/GYN perspective 1054 nulliparous women were randomized into 3 groups to receive either a traditional epid (0.25% BUP), a low-dose CSE, or a low-dose infusion epid Increased rate of normal vaginal delivery with CSE and low-dose infusion Decreased Increased rate of instrumental vaginal delivery rate of CS with traditional epidural Epidural initiated: 8 ml 0.25% BUP 0.125% BUP PCA: 4 ml basal, 4 ml bolus, Lockout 20 min, 16 ml/hr max CIEA: 12 ml/hr infusion The • • • • • • • Is ideal labor analgesic: Rapid onset Long duration Easy to administer No side effects on mother No side effects on baby Allow ambulation, unrestricted expulsive efforts No effect on length of labor or mode of delivery CSE the ideal labor analgesic? Rapid onset of analgesia Reliable, fewer failed, or patchy blocks Effective sacral analgesia in advanced labor Less motor block Better Aids epidural localization in difficult backs Faster Side patient satisfaction cervical dilation in early nulliparas effects are acceptably low A retrospective analysis in a large academic medical center involving near 20 thousand patients found incidences of overall failure, IV epid cath, wet tap, inadequate epid analgesia and cath replacement were all lower in patients receiving CSE Sacral analgesia is difficult to obtain with conventional epidural, CSE is good at providing it CSE is an obvious choice in advanced labor Several studies have found better patient satisfaction scores with CSE vs. conventional epid. Others have found no difference, but none have found better satisfaction with conventional epid analgesia No randomized trial has yet appeared CSE has been associated with improved chances of adequate analgesia in parturient with scoliosis or other causes of a difficult back Patients progress rapidly through labor One explanation for an apparent increase in FHR abnormalities occurring after CSE is this rapid progress 2 large randomized trials have confirmed an increase in the spontaneous vaginal delivery rate with CSE vs. conventional epid analgesia As is the case with epidural analgesia, the CS rate is not increased with CSE PDPH Fetal bradycardia/FHR changes Pruritus Infection Neurotrauma Other side effects PDPH • Rate ~ 1% • CSE technique might actually decrease the incidence of dural puncture with the epid needle by allowing the anesthesiologist to confirm an equivocal loss of resistance by passage of a pencil point spinal needle rather than advancing the large bore epid needle futher Fetal bradycardia/ FHR changes • Incidence of 11-30% • Meta - analysis of 24 randomized trials including over 3,500 patients comparing CSE to conventional epid analgesia found no difference in the rate of FHR changes but an increase in the risk of bradycardia • Usually a reduction in uterine activity (decreasing or interrupting oxytocin administration, or short acting tocolytic administration), raising maternal BP, position change, or simply patience will resolve the problem • The meta – analysis showed no difference in the rate of CS due to bradycardia or for all indications, and neonatal Apgar scores were equivalent Pruritus • 3-95% of patients • Effect is time limited, peak at 30min and largely resolved within 1hr • Prophylactic Ondansetron • Patient satisfaction remains high Numerous studies of varying quality Bradycardia more frequent Management: LUD, fluids, oxygen, treat BP if applicable, IV or SL NTG has been shown to be effective in treating fetal bradycardia associated with uterine hyperactivity However, there is no data demonstrating an increased risk of CS due to CSE CSE: No 2.5mg BUP + 25mcg fentanyl test dose Infusion started Inhalation of nitrous oxide relieves labour pain to a significant degree . Epidural analgesia, CSA , PCEA ,when compared with other methods, provides superior analgesia for labour. well-trained anaesthesiologist with an interest in obstetric analgesia is needed to provide an epidural analgesia service. Ideally, a twenty-four hour obstetric analgesia service should be in operation. The labouring woman should have had an informed discussion about the procedure, benefits and risks of epidural analgesia in the prenatal period. The epidural catheter should be inserted early in labour when the patient is more co-operative and the epidural veins are not dilated. An epidural delivers continuous pain relief to the lower part of your body while allowing you to remain fully conscious. Medication is delivered through a catheter, a very thin, flexible, hollow tube that's inserted into the epidural space just outside the membrane that surrounds your spine. When the parturient think that is no way for their problem they have to choose cesarean section and never think about vaginal delivery Can It we help them or not? is one of the most our responsibility as anesthetists Water birth is an option chosen by some women for pain relief during labor Why do some women consider caesarean delivery more advantageous and more in keeping with the 21st century? Caesarean section or vaginal birth? What difference does it make? A caesarean is a modern way to have a baby, involving the use of technology. Modern technology features highly in our daily lives. We are at ease with it and find it reassuring. The latest and most up-to-date technological equipment is much prized and sought after in all areas of our lives . A caesarean is a medical operation. Birth is currently seen a For epidural catheterization, the tip of a specialized needle (eg, 17 or 18 gauge) is positioned within the epidural space. A thin catheter (eg, 19 or 20 gauge) is then threaded through the needle, and the needle is withdrawn. The catheter is secured to the skin of the parturient ’s back with an adhesive dressing. Intermittent epidural bolus dosing was the standard technique used for providing labor analgesia Continuous infusion of analgesics into the epidural space avoids the peaks and valleys of intermittent administration and results in a smoother analgesic experience for the parturient with fewer provider interventions. Continuous infusion of analgesics into the epidural space avoids the peaks and valleys of intermittent administration and results in a smoother analgesic experience for the parturient with fewer provider interventions. The phrase "walking epidural" is a generic description of any neuraxial analgesic technique that preserves motor function in a parturient. However, for various reasons 34 to 85 percent of women do not actually ambulate during labor The addition of opioids to neuraxial analgesia, namely to provide pain relief while avoiding opioid side effects in the mother and neonate new mode of analgesia is sterile water injection placed just underneath the skin in the most painful spots during labor. A control trial in Iran of 0.5mL injections was conducted with normal saline which revealed a statistical superiority with water over saline From my daughter for preparing these slides From my husband for his supporting Form you dear audience for your attention